Optimizing the Outcome of Anti-Myeloma Treatment with Daratumumab
Abstract
:1. Introduction
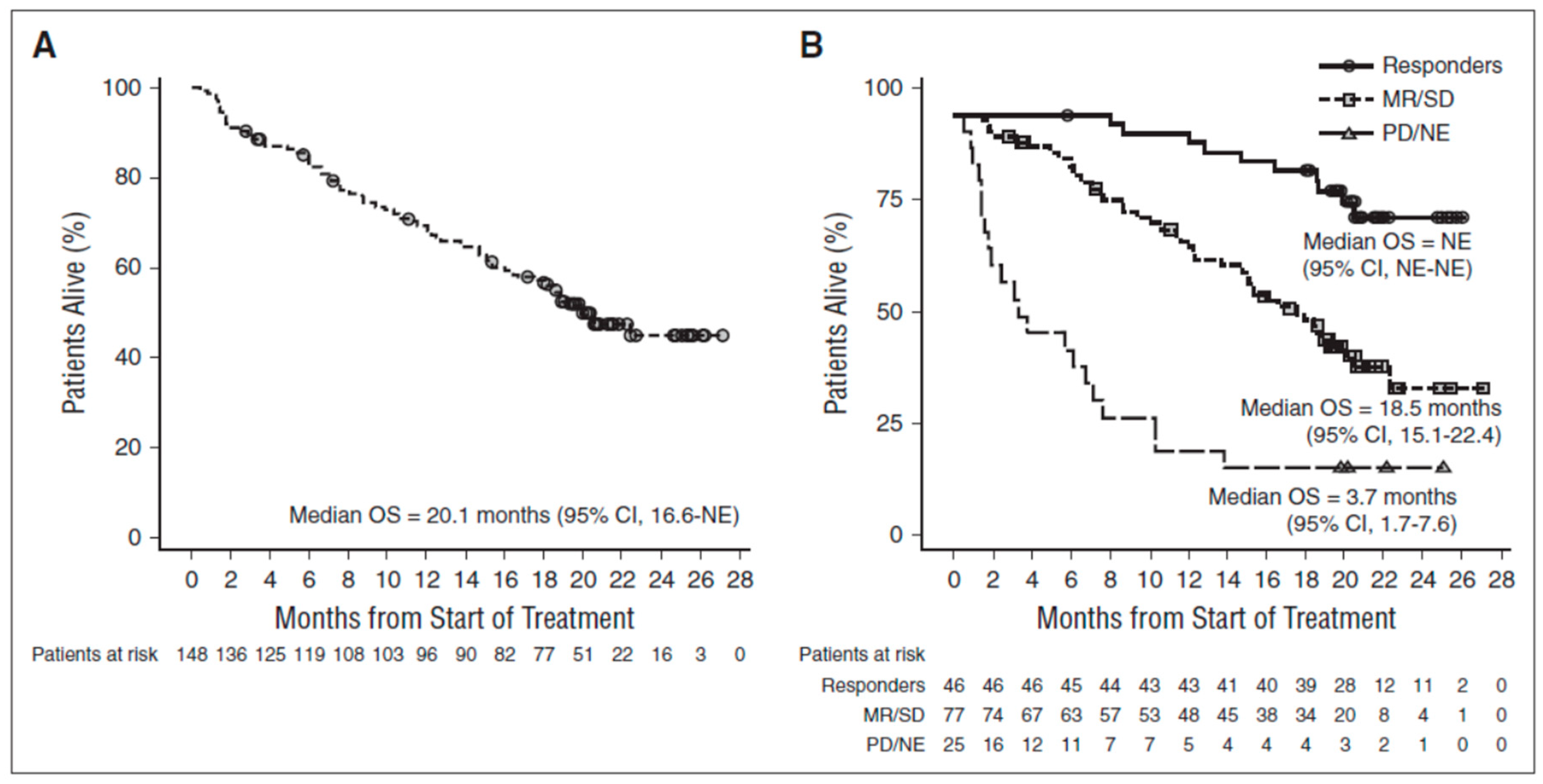
2. Challenging a Dogma with Daratumumab
3. Prolonging Survival without a Response
4. The Dubious Concept of High CD38 Expression Being Beneficial
5. Treat Early
6. Supportive Treatment
7. Use the Best Treatment Upfront
8. Duration of Therapy
9. Anti-Myeloma Therapy with Daratumumab: Re-Treatment or Continuous Therapy?
10. Frailty as an Issue
11. Anti-Myeloma Therapy as a Two-Step Process
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CDC | Complement Mediated Cytotoxicity |
| ADCC | Antibody Dependent Cellular Cytotoxicity |
| ADCP | Antibody Dependent Cellular Phagocytosis |
| PFS | Progression Free Survival |
| OS | Overall Survival |
| CR | Complete Response |
| sCR | Stringent Complete Response |
| PR | Partial Response |
References
- Bahlis, N.J.; Dimopoulos, M.A.; White, D.J.; Benboubker, L. Daratumumab plus lenalidomide and dexamethasone in relapsed/refractory multiple myeloma: Extended follow-up of POLLUX, a randomized, open-label, phase 3 study. Leukemia 2020, 34, 1875–1884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szabo, A.G.; Iversen, K.F.; Moller, S.; Plesner, T. The Clinical Course of Multiple Myeloma in the Era of Novel Agents: A Retrospective, Singe-Center, Real-World Study. Clin. Hematol. Int. 2019, 1, 220–228. [Google Scholar]
- Lokhorst, H.M.; Plesner, T.; Laubach, J.P.; Haji, H. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N. Engl. J. Med. 2015, 373, 1207–1219. [Google Scholar] [CrossRef] [PubMed]
- Lonial, S.; Weiss, B.M.; Usmani, S.Z.; Sanghal, S. Daratumumab monotherapy in patients with treatment-refractory multiple myeloma (SIRIUS): An open-label, randomised, phase 2 trial. Lancet 2016, 387, 1551–1560. [Google Scholar] [CrossRef]
- Kumar, S.K.; Lee, J.H.; Lahuerta, J.J. Risk of progression and survival in multiple myeloma relapsing after therapy with IMiDs and bortezomib: A multicenter international myeloma working group study. Leukemia 2012, 26, 149–157. [Google Scholar] [CrossRef] [Green Version]
- Usmani, S.Z.; Weiss, B.M.; Plesner, T.; Bahlis, N.J. Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood 2016, 128, 34–44. [Google Scholar] [CrossRef]
- Nijhof, I.S.; Casneuf, T.; Van Velzen, J. CD38 expression and complement inhibitors affect response and resistance to daratumumab therapy in myeloma. Blood 2016, 128, 959–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Overdijk, M.B.; Verploegen, S.; Bögels, M.; van Egmond, M. Antibody-mediated phagocytosis contributes to the anti-tumor activity of the therapeutic antibody daratumumab in lymphoma and multiple myeloma. MAbs 2015, 7, 311–320. [Google Scholar] [CrossRef]
- Horenstein, A.L.; Bracci, C.; Morandi, F.; Malavasi, F. CD38 in Adenosinergic Pathways and Metabolic Re-programming in Human Multiple Myeloma Cells: In-tandem Insights From Basic Science to Therapy. Front. Immunol. 2019, 10, 760. [Google Scholar] [CrossRef]
- Ghose, J.; Viola, D.; Terrazas, C. Daratumumab induces CD38 internalization and impairs myeloma cell adhesion. Oncoimmunology 2018, 7, e1486948. [Google Scholar] [CrossRef] [Green Version]
- Marlein, C.R.; Piddock, R.E.; Mistry, J.J.; Auger, M.J. CD38-driven mitochondrial trafficking promotes bioenergetic plasticity in multiple myeloma. Cancer Res. 2019, 79, 2285–2297. [Google Scholar] [CrossRef] [Green Version]
- Chatterjee, S.; Daenthanasanmak, A.; Chakraborty, P.; Paulos, C.M. CD38-NAD + Axis Regulates Immunotherapeutic Anti-Tumor T Cell Response. Cell Metab. 2018, 27, 85–100.e8. [Google Scholar] [CrossRef] [Green Version]
- Stocker, N.; Gaugler, B.; Ricard, L. Daratumumab prevents programmed death ligand-1 expression on antigen-presenting cells in de novo multiple myeloma. Cancer Med. 2020, 9, 2077–2084. [Google Scholar] [CrossRef]
- Krejcik, J.; Casneuf, T.; Nijhof, I.S. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood 2016, 128, 384–394. [Google Scholar] [CrossRef] [Green Version]
- Nijhof, I.S.; Groen, R.W.J.; Lokhorst, H.M. Upregulation of CD38 expression on multiple myeloma cells by all-trans retinoic acid improves the efficacy of daratumumab. Leukemia 2015, 29, 2039–2049. [Google Scholar] [CrossRef]
- García-Guerrero, E.; Gogishvili, T.; Danhof, S.; Einsele, H. Panobinostat induces CD38 upregulation and augments the antimyeloma efficacy of daratumumab. Blood. 2017, 129, 3386–3388. [Google Scholar] [CrossRef]
- Facon, T.; Kumar, S.; Plesner, T. Daratumumab plus lenalidomide and dexamethasone for untreated Myeloma. N. Engl. J. Med. 2019, 380, 2104–2115. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Oriol, A.; Nahi, H.; San-Miguel, J.; Bahlis, N.J.; Usmani, S.Z.; Rabin, N.; Orlowski, R.Z.; Komarnicki, M.; Suzuki, K.; et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N. Engl. J. Med. 2016, 375, 1319–1331. [Google Scholar] [CrossRef] [Green Version]
- Patel, K.K.; Giri, S.; Parker, T.L.; Bar, N.; Neparidze, N.; Huntington, S.F. Cost-Effectiveness of First-Line Versus Second-Line Use of Daratumumab in Older, Transplant-Ineligible Patients With Multiple Myeloma. J. Clin. Oncol. 2021, 375, 1319–1331. [Google Scholar]
- Vacca, A.; Melaccio, A.; Sportelli, A.; Solimando, A.G.; Dammacco, F.; Ria, R. Subcutaneous immunoglobulins in patients with multiple myeloma and secondary hypogammaglobulinemia: A randomized trial. Clin. Immunol. 2018, 191, 110–115. [Google Scholar] [CrossRef]
- Chapel, H.; Lee, M.; Hargreaves, R.; Pamphilon, D.; Prentice, A. Randomised trial of intravenous immunoglobulin as prophylaxis against infection in plateau-phase multiple myeloma. Lancet 1994, 343, 1059–1063. [Google Scholar] [CrossRef]
- Durie, B.G.M.; Hoering, A.; Abidi, M.H.; Rajkumar, S.V.; Epstein, J.; Kahanic, S.P.; Thakuri, M.; Reu, F.; Reynolds, C.M.; Sexton, R.; et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): A randomised, open-label, phase 3 trial. Lancet 2017, 389, 519–527. [Google Scholar] [CrossRef] [Green Version]
- Perrot, A.; Facon, T.; Plesner, T.; Usmani, S.Z.; Kumar, S.; Bahlis, N.J.; Ramasamy, K.; Roussel, M.; Araujo, C.; Jaccard, A.; et al. Faster and sustained improvement in health-related quality of life (HRQoL) for newly diagnosed multiple myeloma (NDMM) patients ineligible for transplant treated with daratumumab, lenalidomide, and dexamethasone (D-Rd) versus Rd alone: MAIA. J. Clin. Oncol. 2019, 37, 8016. [Google Scholar] [CrossRef]
- Paiva, B.; Van Dongen, J.J.M.; Orfao, A. New criteria for response assessment: Role of minimal residual disease in bmultiple myeloma. Blood 2015, 125, 3059–3068. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Clinical Setting | Real World [2] | Pollux Trial [1] |
|---|---|---|
| Number of patients | 303 | 286 |
| Median age (years) | 69 | 65 |
| Age range (years) | 30–90 | 34–89 |
| Prior lines of therapy | 1 | 1 (median) |
| Overall Response Rate % | 59 | 93 |
| Complete Response/Stringent Complete Response | 17 | 57 |
| Progression Free Survival (months) | 10 | 45 |
| Time to Next Treatment (months) | 6 | 51 |
| Impact of CD38 Expression by Myeloma Cells | Mode of Action | Reference |
|---|---|---|
| High expression beneficial | ||
| CDC | [7] | |
| ADCC | [7] | |
| ADCP | [8] | |
| Low expression beneficial | ||
| Inhibition of adenosine production | [9] | |
| Inhibition of adhesion to stroma | [10] | |
| Inhibition of nanotube formation | [11] | |
| Indeterminate but continuous exposure to Daratumumab beneficial | ||
| Enhancement of T-cell mediated cytotoxicity | [12] | |
| Reduced PD-L1 expression by antigen-presenting cells | [13] | |
| Elimination of regulatory T-cells, B-cells and Myeloid cells | [14] |
| Trial Name | MAIA | POLLUX |
|---|---|---|
| Target population | NDMM | RRMM |
| Number of patients | 368 | 286 |
| Follow-up (months) | 28 | 25 |
| Median age (years) | 73 | 65 |
| Median number of prior lines of therapy | 0 | 1 |
| PFS at 30 months | 71% | 60% |
| sCR/CR rate | 48% | 51% |
| MRD negative rate (10−5) | 24% | 26% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plesner, T. Optimizing the Outcome of Anti-Myeloma Treatment with Daratumumab. J. Clin. Med. 2021, 10, 1002. https://doi.org/10.3390/jcm10051002
Plesner T. Optimizing the Outcome of Anti-Myeloma Treatment with Daratumumab. Journal of Clinical Medicine. 2021; 10(5):1002. https://doi.org/10.3390/jcm10051002
Chicago/Turabian StylePlesner, Torben. 2021. "Optimizing the Outcome of Anti-Myeloma Treatment with Daratumumab" Journal of Clinical Medicine 10, no. 5: 1002. https://doi.org/10.3390/jcm10051002
APA StylePlesner, T. (2021). Optimizing the Outcome of Anti-Myeloma Treatment with Daratumumab. Journal of Clinical Medicine, 10(5), 1002. https://doi.org/10.3390/jcm10051002






