1. Introduction
Coffin–Siris syndrome (CSS) is a multisystem congenital anomaly caused by mutations in genes of the BRG1- and BRM-associated factor complexes, including
ARID1A,
ARID1B,
ARID2,
DPF2,
SMARCA4,
SMARCB1,
SMARCC2,
SMARCE1,
SOX11, and
SOX4. [
1,
2,
3].
Recent discoveries have underlined the importance of the BAF complex in human neuronal development and cancer occurrence (three especially well-studied complex assemblies are esBAF, npBAF, and nBAF), whereby mutations in their subunit genes and related genes are implicated in several nonverbal ID (intellectual disability) syndromes such as CSS, autism spectrum disorder, and schizophrenia, as well as in cancers/cancer predisposing syndromes [
4,
5].
In 1970, Coffin and Siris were the first ones to describe three girls with similar phenotypic traits and manifestations, including severe intellectual disability and developmental delay, growth retardation, lax joints, and absent or hypoplastic fifth distal phalanges and nails [
6]. Other findings included a coarse facial appearance, feeding difficulties, frequent infections, and cardiac/neurological/gastrointestinal/genitourinary anomalies [
7].
The typical features of Coffin–Siris syndrome result from the involvement of ectodermal tissues. Abnormal or delayed dentition is also reported frequently [
2,
8].
Fewer than 200 individuals with molecularly confirmed Coffin–Siris syndrome have been reported, indicating and underlining that the diagnosis is rare and difficult. It has to be considered that these numbers are likely underestimated, since not all individuals may have sought medical attention.
In addition, the identification of a pathogenic variant in
ARID1B in some members of a large cohort with intellectual disability suggests that the prevalence of pathogenic variants in genes associated with CSS (and of subtle phenotypic features of CSS) may be higher than is currently appreciated among those with intellectual disability [
2,
9].
The penetrance for Coffin–Siris syndrome appears to be complete.
More females than males with CSS were reported in the literature prior to 2001 [
6]. In cases of molecularly confirmed CSS, the male–female ratios are similar [
10,
11]. No evidence exists for X-linked dominant, sex-limited, or mitochondrial inheritance [
2].
Individuals with Coffin–Siris syndrome have a distinct appearance, with overall typically coarse facial features. In early childhood, individuals with CSS usually have a round face with thick and arched eyebrows, a short nose with a bulbous tip, and anteverted nostrils, a long philtrum, a small mouth, and micro-retrognathia. Adults tend to have a broad nasal bridge without anteverted nostrils, a broad philtrum, a large tongue, and prognathism [
12].
Common findings include a wide mouth and thick lips. The palate is generally highly arched and a cleft palate is occasionally present. Another common feature is abnormal ears, either in shape or position. Less frequent findings are ptosis, a short philtrum, and macroglossia [
13].
Because of micrognathia, macroglossia, hypotonia, and lax joints, dental and orthodontic management can be challenging in these children, as well as communication because of their IDs. Dentists should be aware that proper motivation and psychological support for the patients and their families are essential to achieve a functional and aesthetical dentition and occlusion [
7,
14].
The most common and significant oral health problems in these patients are gingival and periodontal diseases, which usually lead to the loss of permanent anterior teeth in their young adulthood. Some factors can contribute to such evolution, including malocclusion, bruxism, conical-shaped tooth roots, and an abnormal host response because of a compromised immune system [
14].
This article describes the treatment of a patient affected by CSS through orthognathic surgery and pre- and post-surgical orthodontic treatment.
The patient showed a problematic condition with a significant malocclusion characterised by mandibular prognathism, an extremely narrow palate, an anterior reverse bite, and a right and left crossbite.
This, combined with the facial dysmorphism typical of CSS, caused significant social, functional, and aesthetic problems that the patient perceived as disturbing, requesting us to solve especially her aesthetic condition during the first visit [
15].
2. Materials and Methods
2.1. Case Presentation
The patient suffering from CSS attended the Orthodontic Department of the Gabriele D‘Annunzio Odontostomatological Clinic in April 2016. The reasons for the visit were a third class malocclusion and an impacted second upper premolar (1.5).
The patient underwent a comprehensive clinical examination at the age of 26. The patient suffered from CSS and despite her ID, she proved to have good communication skills. Her periodontal condition was good and she had not lost any periodontal support tissue or permanent elements, but her oral hygiene needed to be improved. She was extensively educated and motivated at oral hygiene procedures before, during, and after the treatment. During the whole treatment period, we were strongly supported by her family and therapists who followed her closely at home.
Due to the anterior reverse bite, the patient was unable to chew, speak, and breathe properly. She also had debilitating aesthetic problems because she was deeply ashamed of her smile. Giving this patient a better smile was crucial to motivate her to take care of her oral hygiene, and therefore to prevent her from incurring periodontal and dental problems at a young age.
Furthermore, due to the CSS, the patient had significant retinopathy, which had significantly reduced her vision.
2.2. Clinical Assessment
The patient was 26 years old. The orthodontic examination assessed the following characteristics:
- -
Mesiofacial biotype
- -
Competent lips, prognathic profile
- -
Third molar and canine dental class, both right and left
- -
Anterior crossbite
- -
Negative overjet (approximately −3 mm), increased overbite (approximately +5 mm)
- -
Right and left posterior crossbite
- -
Lower midline left deviation (approximately 3 mm)
- -
Narrow upper arch with diastemas due to the absence of element 15.
2.3. Radiographic Assessment
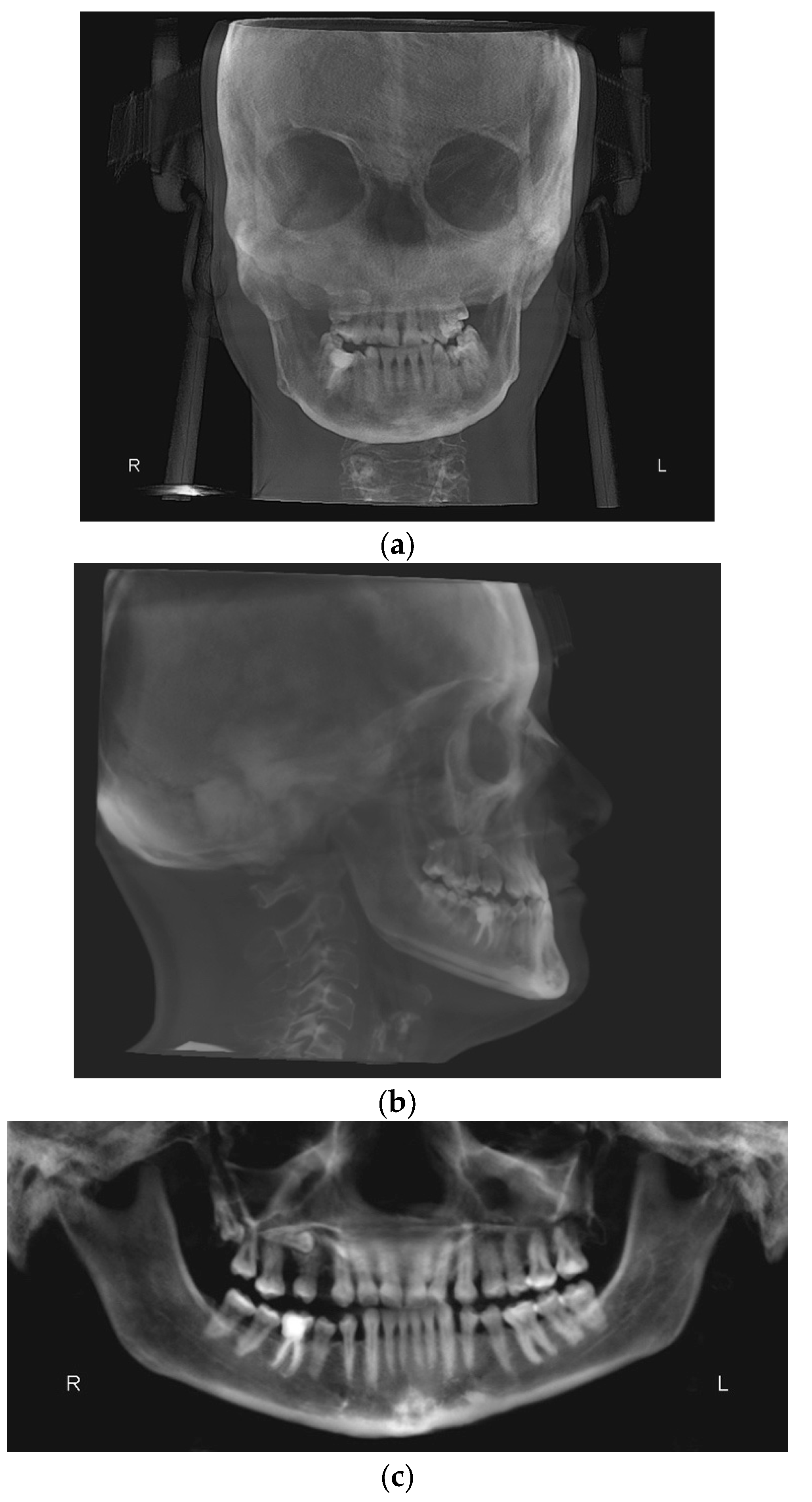
The X-ray examination through cone beam computed tomography (CBCT) [
16] (
Figure 1a–c) was processed with Dolphin Imaging 3D software v. 12.0 (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) [
15] and showed the following:
- -
Third skeletal class
- -
Hyperdivergent skeletal profile
- -
Left lateral deviation of the mandible
- -
Contracted upper arch
- -
Inclusion of 15 in a transverse position, near the apexes of elements 1.4 and 1.6.
Figure 1.
(a): Antero-posterior projection of the CBCT. (b): Lateral–lateral projection of the CBCT. (c): Panoramic projection of the CBCT.
Figure 1.
(a): Antero-posterior projection of the CBCT. (b): Lateral–lateral projection of the CBCT. (c): Panoramic projection of the CBCT.
2.4. Treatment Plan
The treatment plan involved a presurgical orthodontic phase. The aim was to align and level the arches, removing the dental compensations of the third-class malocclusion [
17] (upper incisors proclination and lingual inclination of the lower incisors), mesializing and derotating element 1.4. This phase included the avulsion of the impacted 1.5 [
18].
Afterwards, the orthognathic surgery was necessary to obtain anterior and posterior maxillary alignment and to resolve the anterior crossbite, as well as the right and left posterior crossbite [
19].
After surgery, the patient underwent post-surgical orthodontic treatment, to refine the alignment and to avoid surgical relapse [
20].
3. Results
Treatment and Follow-Up
The patient underwent the orthodontic examination in April 2016 and received the diagnosis and the treatment plan in May 2016.
The therapy started in June 2016 with multibracket self-ligating attachments for the upper jaw, Damon prescription, followed by the same approach for the lower jaw in September 2016.
In this syndromic patient, the self-ligating technique proved to be very useful and valid because the check-up and follow-up appointments’ duration was significantly reduced. In fact, the patient was sufficiently cooperative, but she quickly became tired during the sessions.
The pre-surgical orthodontic treatment lasted 3 years. The duration was slightly longer than average [
20] but considering the medical condition of the patient, we believe that the times were appropriate. She missed various check-up appointments because of some ocular problems she was dealing with during the treatment period. Furthermore, several times we had to stop to manage periodontal inflammation and newly motivate the patient to strive for proper oral hygiene. Then, on two occasions the patient lost motivation and she was not completely cooperative for several months. The patient was also treated by a psychologist team for the entire duration of the treatment.
In June 2019, the objectives of the pre-surgical orthodontic treatment were considerably achieved, i.e., the arches were levelled, the teeth were aligned, and the dental compensations of the third skeletal class had been removed. The pre-surgical diagnostic records were sent (
Figure 2a–d) to the maxillofacial team. Kobayashi ligatures were placed all over the teeth to prepare the patient for surgery.
In October 2019, the patient underwent maxillofacial surgery to correct the severe skeletal malocclusion and to relocate the bone bases to the correct location. The combined surgery involved maxillary Le Fort I osteotomy [
21] and mandibular reduction [
22]. Skeletal fixation plates were then used to stabilise the bone segments [
23].
One week later, the post-surgical orthodontic treatment phase started (
Figure 3a–c).
During the post-surgical orthodontic treatment, frequent follow-up examinations were performed to reduce the risk of relapse and to complete the alignment. In this phase, element 1.5 was extracted.
It was challenging to entirely regain the patient’s collaboration after the surgery because she was scared and demotivated. Her family and therapy team worked for several months to get her to collaborate again. Unfortunately, during this phase, a partial orthodontic relapse was recorded. In fact, the patient did not cooperate enough with the intermaxillary maintenance elastic bands. Furthermore, she had to be constantly re-motivated regarding home oral hygiene procedures.
Since May 2021, the patient has worn cross arch elastics on elements 1.6, 1.4, 2.6, 2.4, and 2.5 to control the high tendency to relapse (
Figure 4).
In August 2022, the post-surgical orthodontic treatment was considered finished, and there was no risk of surgical relapse. We proceeded with the removal of the orthodontic appliances (
Figure 5a–c) and the delivery of the restraints.
4. Discussion
The patient with CSS first visited the D‘Annunzio orthodontics department in April 2016, at the age of 26.
Pre-surgical orthodontic treatment lasted 3 years, and post-surgical orthodontic treatment lasted 1 year.
During the pre-surgical orthodontic treatment, the arches were aligned and levelled, and the dental decompensation was solved. During this phase, a slowdown occurred because the patient had difficulty in understanding the purpose of the “worsening of the malocclusion”. She therefore tended to skip appointments. After the surgery, the post-operative pain worsened and was complicated by poor oral hygiene, resulting in a further slowdown and, unfortunately, also the start of a relapse of the transverse dimension of the upper jaw.
In a rare case report of a patient with CSS of Dr Sahil Mustafa Kidwai et al., a 20-year-old female underwent oral and extraoral examinations. Intraoral examination revealed a missing maxillary lateral incisor, generalised periodontitis, and bifid uvula. The patient had poor oral hygiene and was never cooperative in preserving her oral health. The author found that early professional treatment and daily care at home can mitigate the severity and frequency of oral health issues [
24,
25,
26].
Despite their ID, our patient was cooperative and allowed the operators to perform all the necessary surgical and orthodontic treatment. The duration of the therapy was influenced by the patient’s poor oral hygiene, which required a considerable number of pauses for adequate oral hygiene procedures and motivation. Furthermore, the patient missed numerous follow-up appointments because of the comorbidities of CSS—ocular and dermatological conditions.
Despite this, the operators were satisfied with the result, since the treatment allowed the patient to improve her aesthetic appearance and functional abilities. Furthermore, the patient’s parents were impressed to note that their daughter’s socialisation skills were also improved after the treatment.
Both the family and the psychologists preserved and maintained the patient’s collaboration throughout the treatment, leveraging the aesthetic result of the therapy and the resolution of the jaw deviation. In fact, despite her ID, the patient was perfectly conscious of her syndromic situation and of the functional and aesthetic limitation of her malocclusion.
The outcome cannot be considered perfect since the patient did not want to rehabilitate element 1.5 after the treatment, and a small component of lateral mandibular deviation remained. Moreover, there was a recurrence of the maxillary expansion because the patient lacked cooperation for several months after surgery [
27]. However, these are negligible failures considering the starting condition and the patient’s health condition.
The operators continue to visit the patient every year.
5. Conclusions
It has been interesting for us to describe this case because we think that patients with CSS can be treated with a customised approach and treatment plan.
The treatment lasted longer than average and did not lead to a perfect outcome, but nevertheless, the patient responded well to most of the steps and cooperated to the best of her ability.
Clearly, the patient’s collaboration had to be constantly supervised and re-motivated by her family and all the professional figures who surround her. It was also a challenging, long, and intense process from a psychological standpoint.
Today, the patient no longer has the anterior crossbite, and only a slight left posterior crossbite persists. Moreover, she has an aesthetically acceptable smile and has less concerns about her social life. She is extremely pleased with her new smile and her family reports that after the treatment, they noticed an improvement in her ability to socialise with her peers.
We think that this is of enormous importance, especially in patients with multiple disabilities and comorbidities.
In conclusion, we wanted to document this case, although the result is not “orthodontically” perfect, ultimately to support and send the message that even syndromic patients can be treated if comorbidities and collaboration allow it. The need for more support and collaboration with the family and psychotherapists must be considered, but clinical cases like this can be faced and solved. Obviously, each syndromic patient is a unique case, and the risk–benefit ratio must be correctly assessed for each one.
Author Contributions
Conceptualization, M.M. and F.F.; methodology, M.M. and G.G.; validation, M.M., C.R., M.F. and C.D.P.; formal analysis, M.M. and C.R.; resources, M.M. and F.F.; data curation, C.R., M.M. and C.D.P.; writing, M.M., C.R. and C.D.P.; writing—review and editing, M.M. and G.G.; supervision, M.M. and F.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval (number 23, accept date: 8 November 2018) was obtained by the Independent Ethics Committee of Chieti hospital. The study protocol was drawn following the European Union Good Practice Rules and the Helsinki Declaration. The patient provided written informed consent before the beginning of orthodontic and surgical therapies.
Informed Consent Statement
Informed consent was obtained from the subject involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Wang, X.; Wu, H.; Sun, H.; Wang, L.; Chen, L. ARID2, a Rare Cause of Coffin-Siris Syndrome: A Clinical Description of Two Cases. Front. Pediatr. 2022, 10, 911954. [Google Scholar] [CrossRef] [PubMed]
- Vergano, S.S.; Santen, G.; Wieczorek, D.; Wollnik, B.; Matsumoto, N.; Deardorff, M.A. Coffin-Siris Syndrome Synonym: Fifth Digit Syndrome. In GeneReviews; University of Washington: Seattle, WA, USA, 1993. [Google Scholar] [PubMed]
- Miyake, N.; Tsurusaki, Y.; Matsumoto, N. Numerous BAF complex genes are mutated in Coffin-Siris syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2014, 166, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Kosho, T.; Miyake, N.; Carey, J.C. Coffin-Siris syndrome and related disorders involving components of the BAF (mSWI/SNF) complex: Historical review and recent advances using next generation sequencing. Am. J. Med. Genet. C Semin. Med. Genet. 2014, 166, 241–251. [Google Scholar] [CrossRef]
- Vasko, A.; Drivas, T.G.; Schrier Vergano, S.A. Genotype-Phenotype Correlations in 208 Individuals with Coffin-Siris Syndrome. Genes 2021, 12, 937. [Google Scholar] [CrossRef] [PubMed]
- Fleck, B.J.; Pandya, A.; Vanner, L.; Kerkering, K.; Bodurtha, J. Coffin-Siris syndrome: Review and presentation of new cases from a questionnaire study. Am. J. Med. Genet. 2001, 99, 1. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, A.S.; Akbas, S.; Yalin, M.R.; Ozdemir, E.; Koylu, Z. Successful difficult airway management of a child with Coffin-siris syndrome. Clin. Case Rep. 2017, 5, 1312–1314. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Bielsa, A.; Ruiz-de-Larramendiz, D.R.; Abenia-Usón, P.; Gracia-Cazaña, T.; Gilaberte, Y. Nail dysplasia and digital hypoplasia—Coffin-Siris syndrome. An. Bras. Dermatol. 2024; in press. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, J.; Ekici, A.B.; Endele, S.; Popp, B.; Zweier, C.; Wiesener, A.; Wohlleber, E.; Dufke, A.; Rossier, E.; Petsch, C.; et al. Haploinsufficiency of ARID1B, a member of the SWI/SNF-a chromatin-remodeling complex, is a frequent cause of intellectual disability. Am. J. Hum. Genet. 2012, 90, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Kosho, T.; Okamoto, N. Genotype-phenotype correlation of Coffin-Siris syndrome caused by mutations in SMARCB1, SMARCA4, SMARCE1, and ARID1A. Am. J. Med. Genet. C Semin. Med. Genet. 2014, 166, 262–275. [Google Scholar] [CrossRef] [PubMed]
- Santen, G.W.; Clayton-Smith, J. The ARID1B phenotype: What we have learned so far. Am. J. Med. Genet. C Semin. Med. Genet. 2014, 166, 276–289. [Google Scholar] [CrossRef] [PubMed]
- Kosho, T.; Okamoto, N.; Ohashi, H.; Tsurusaki, Y.; Imai, Y.; Hibi-Ko, Y.; Kawame, H.; Homma, T.; Tanabe, S.; Kato, M.; et al. Clinical correlations of mutations affecting six components of the SWI/SNF complex: Detailed description of 21 patients and a review of the literature. Am. J. Med. Genet. A 2013, 161, 1221–1237. [Google Scholar] [CrossRef] [PubMed]
- Schrier, S.A.; Bodurtha, J.N.; Burton, B.; Chudley, A.E.; Chiong, M.A.D.; D’Avanzo, M.G.; Lynch, S.A.; Musio, A.; Nyazov, D.M.; Sanchez-Lara, P.A.; et al. The Coffin–Siris syndrome: A proposed diagnostic approach and assessment of 15 overlapping cases. Am. J. Med Genet. Part A 2012, 158, 1865–1876. [Google Scholar] [CrossRef] [PubMed]
- Figueira, H.S.; Medina, P.O.; Jesus, G.; Hanan, A.R.A.; Júnior, E.C.S.; Hanan, S.A. Oral findings in Coffin-Siris syndrome: A case report. Rev. Port. Estomatol. Med. Dent. E Cir. Maxilofac. 2021, 62, 42–49. [Google Scholar] [CrossRef]
- Nouri, M.; Hamidiaval, S.; Akbarzadeh Baghban, A.; Basafa, M.; Fahim, M. Efficacy of a Newly Designed Cephalometric Analysis Software for McNamara Analysis in Comparison with Dolphin Software. J. Dent. 2015, 12, 60–69. [Google Scholar]
- Feragalli, B.; Rampado, O.; Abate, C.; Macrì, M.; Festa, F.; Stromei, F.; Caputi, S.; Guglielmi, G. Cone beam computed tomography for dental and maxillofacial imaging: Technique improvement and low-dose protocols. Radiol. Med. 2017, 122, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Almashraqi, A.A.; Khadhi, A.H.; Arishi, K.A.; Alamir, A.A.; Beleges, E.M.; Halboub, E. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: A systematic review. Clin. Oral Investig. 2022, 26, 6443–6455. [Google Scholar] [CrossRef] [PubMed]
- Macrì, M.; D’Albis, G.; D’Albis, V.; Timeo, S.; Festa, F. Augmented Reality-Assisted Surgical Exposure of an Impacted Tooth: A Pilot Study. Appl. Sci. 2023, 13, 11097. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. Orthognathic surgery: A hierarchy of stability. Int. J. Adult Orthod. Orthognath. Surg. 1996, 11, 191–204. [Google Scholar]
- Wolford, L.M. Comprehensive post orthognathic surgery orthodontics: Complications, misconceptions, and management. Oral Maxillofac. Surg. Clin. 2020, 32, 135–151. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, S.M. Le Fort I Osteotomy. In Atlas of the Oral and Maxillofacial Surgery Clinics of North America; Elsevier: Amsterdam, The Netherlands, 2016; Volume 24, pp. 1–13. [Google Scholar]
- Chan, T.C.; Harrigan, R.A.; Ufberg, J.; Vilke, G.M. Mandibular reduction. J. Emerg. Med. 2008, 34, 435–440. [Google Scholar] [CrossRef]
- Ellis, E., III. Rigid skeletal fixation of fractures. J. Oral Maxillofac. Surg. 1993, 51, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, S.; Ahmed, R.; Goel, S.; Atif, A. Coffin Siris Syndrome: A Rare Case Report. Indian J. Res. 2016, 5, 558–559. [Google Scholar] [CrossRef]
- Macrì, M.; Toniato, E.; Murmura, G.; Varvara, G.; Festa, F. Midpalatal suture density as a function of sex and growth-pattern-related variability via CBCT evaluations of 392 adolescents treated with a rapid maxillary expander appliance. Appl. Sci. 2022, 12, 2221. [Google Scholar] [CrossRef]
- Macrì, M.; Rendina, F.; Feragalli, B.; Pegreffi, F.; Festa, F. Prevalence of Ponticulus Posticus and Migraine in 220 Orthodontic Patients: A Cross-Sectional Study. Biology 2023, 12, 471. [Google Scholar] [CrossRef] [PubMed]
- Macrì, M.; Festa, F. Three-dimensional evaluation using CBCT of the mandibular asymmetry and the compensation mechanism in a growing patient: A case report. Front. Public Health 2022, 10, 921413. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).