Abstract
Several innovations have been introduced in recent years to improve total knee arthroplasty (TKA). Robotic-assisted surgery is gaining popularity for more precise implant placement while minimizing soft tissue injury. The main concerns are increased cost, operative time, and a significant learning curve. This systematic review aims to analyze the surgical time learning curve, implant placement accuracy, and complications related to robotic-assisted TKA (raTKA). A systematic literature review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The research was conducted up to September 2022 in four databases (PubMed/MEDLINE, Embase, Scopus, and the Cochrane Database of Systematic Reviews), with the following key terms: “robotic-assisted”, “total knee arthroplasty”, “robotic”, “TKA”, “learning”, and “TKR”. The methodology quality of the studies was assessed using the Methodological Index for Non-Randomized Studies (MINORS) criteria. This systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO), ID: CRD42022354797, in August 2022. Fifteen clinical studies that analyzed the raTKA learning curve of 29 surgeons and 2300 raTKAs were included in the systematic review. Fourteen surgeons reported the presence of an inflection point during the learning curve. Few studies have reported the learning curve of raTKA regarding lower limb alignment, component position, and intraoperative and postoperative complications. The main finding of this systematic review is that the procedure number required to reach the learning plateau is about 14.9 cases. Furthermore, an average decrease in surgical time of 23.9 min was described between the initial and proficiency phases; the average surgical time in the two phases was 98.8 min and 74.4 min, respectively. No learning curve was observed for implant placement and lower limb alignment because the implants were correctly placed from the first raTKAs. No significant complication rates were reported during the raTKA learning curve.
Keywords:
TKA; total knee arthroplasty; knee replacement; orthopedic; robotic; robotic-assisted; raTKA; learning; curve; limb alignment 1. Introduction
Total knee arthroplasty (TKA) is a safe and successful surgical procedure for end-stage knee osteoarthritis treatment [1,2]. More than half a million surgeries are performed annually in the United States, and epidemiological studies predict a more than 650% increase by 2030 [3]. Despite high long-term survival of more than 90% after ten years, about 20% of patients are dissatisfied with their surgeries [1,2,3,4].
In recent years, several innovations have been introduced into clinical practice to improve TKA outcomes, such as upgraded materials, minimally invasive surgery, innovative TKA alignment, computer-assisted surgery (CAS), intraoperative navigation, augmented reality, and robotic-assisted (ra) surgery [5,6,7,8,9,10,11]. Ra surgery has fascinated many since its beginnings around 1980. Ra procedures allow surgeons to perform complex operations with greater precision, flexibility, and control than conventional techniques and have become a staple in operating rooms worldwide. In recent decades, considerable technological advances have made robotics applications possible in multiple surgery fields, including orthopedics [12]. Robotic-assisted TKA (raTKA) has gained popularity, and its use is steadily growing [13,14]. Despite its theoretical advantages, raTKA raises some concerns, such as increased cost and operative time, absence of long-term follow-up studies, and a significant learning curve to refine the technique [8,14]. A not-yet well-defined learning curve is one of the major concerns of surgeons approaching raTKA [15]. The learning curve has a key role in training surgeons by allowing improved performance, accuracy, and reduced surgical time [16]. It is characterized by three phases: a rapid improvement through the first cases, a successive modest but steady improvement achieved with increased experience, and finally, a plateau phase where additional experience does not influence improvement. The “inflection point” is defined as the number (n) of procedures required to achieve proficiency in each stage of the surgical procedure [16,17]. Identifying the learning curve of raTKA has several clinical applications for patient safety, surgeon training, and cost-effectiveness.
The primary purpose of this systematic review is to analyze the surgical time learning curve of raTKA. The secondary aims are to investigate the learning curve associated with implant placement accuracy and complications related to raTKAs.
2. Materials and Methods
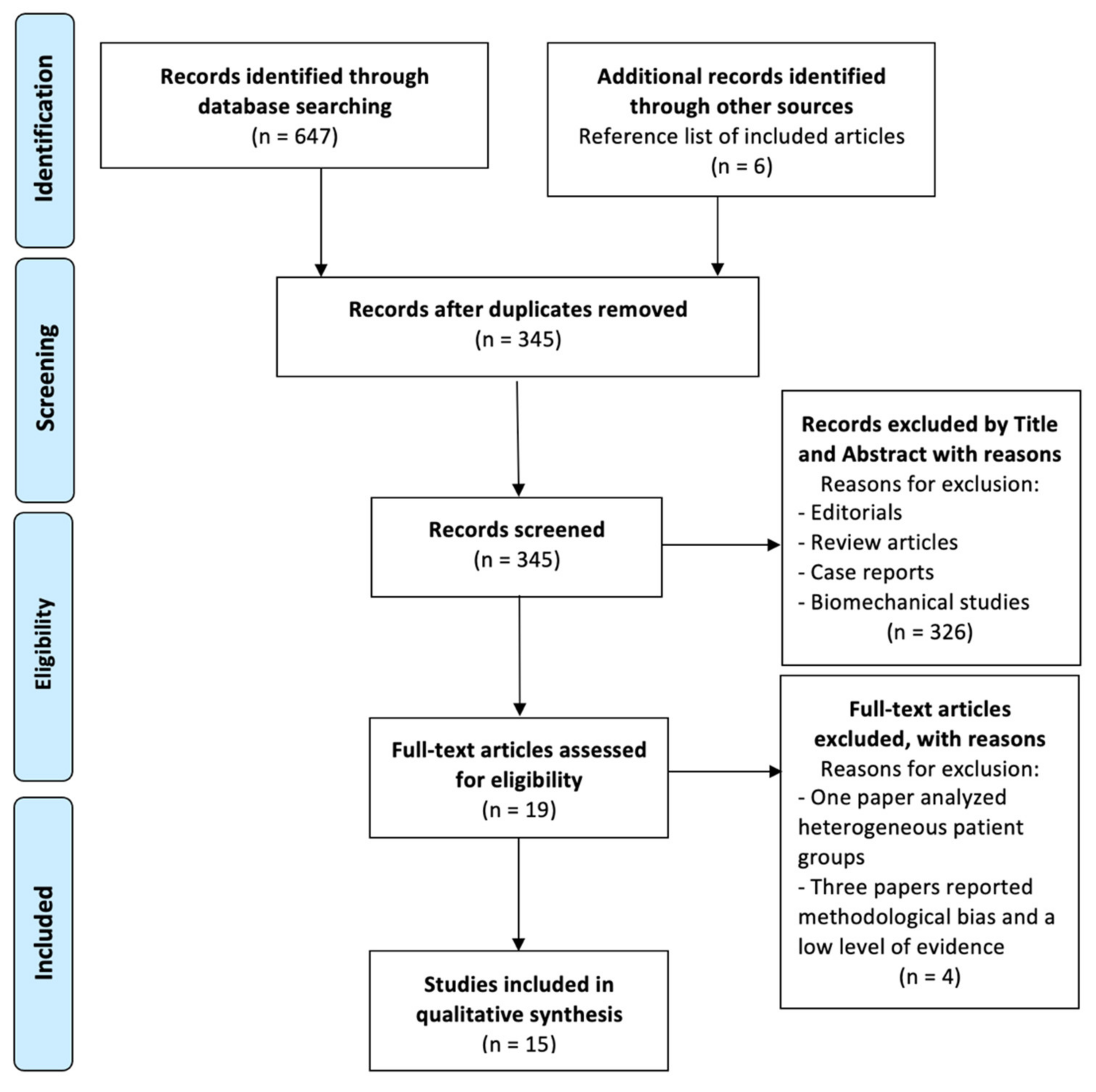
A systematic literature review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18]. The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO), ID: CRD42022354797, in August 2022 [19,20].
2.1. Study Design and Search Strategy
Literature research in four databases (PubMed/MEDLINE, Embase, Scopus, and the Cochrane Database of Systematic Reviews) was performed until September 2022. The research was focused on studies dealing with the learning curve of raTKA. The following key terms were used in association with the Boolean operators “AND” and “OR”: “robotic-assisted”, “total-knee-arthroplasty”, “robotic”, “TKA”, “learning”, and “TKR”.
2.2. Study Screening
The initial database search resulted in 647 studies. Two independent reviewers screened the titles and abstracts of the studies identified through the comprehensive literature analysis (GC and FB). Duplicate articles were removed. The full text was reviewed in case of title/abstract analysis discrepancies. In case of discrepancies, a third author (FG) was consulted. After applying the inclusion and exclusion criteria, 15 clinical studies [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35] investigating the learning curve in robotic-assisted total knee arthroplasty were included in this systematic review. Furthermore, a cross-reference check for the inclusion of possibly relevant studies was performed. The PRISMA flowchart is shown in Figure 1.

Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Flowchart of studies included in this systematic review.
2.3. Inclusion and Exclusion Criteria
Clinical studies on raTKA that respected the following criteria were included: studies on human subjects with levels of evidence (LoE) from 1 to 4 as defined by the Oxford Centre for Evidence-Based Medicine 2011 and clinical studies written in English. No publication time restrictions were established. Preclinical studies, book chapters, editorials, reviews, technical reports, and abstracts of scientific meetings were excluded.
2.4. Data Extraction and Collection
Two different reviewers (GC and FB) independently collected data from included studies in a template with the following characteristics: demographics data, data on the operative time learning curve, implant accuracy, and complications.
2.5. Quality Assessment
The articles were analyzed using the Levels of Evidence (LoE) defined by the Oxford Centre for Evidence-Based Medicine 2011. Articles were graded from I to V, where LoE I indicates the best study design [36]. The methodological quality of the included studies was evaluated by two authors using the Methodological Index for Non-Randomized Studies (MINORS) criteria. A third author resolved cases of disagreement [37,38].
3. Results
Based on the analysis of the included studies, it was found that there were two LoE II studies [26,27,28,29,30,31,32,33], six LoE III studies [21,24,25,27,34,35], and seven LoE IV studies [22,23,24,25,26,27,28,32]. The mean MINORS score for non-comparative studies was 9.3 (range 6–12) and 15.5 for comparative studies (range 14–17) (Table 1).

Table 1.
Main demographic characteristics and surgical data.
3.1. Demographic Characteristics and Surgical Data
This study analyzed the raTKA learning curve of 29 surgeons (surgeons’ competencies are listed in Table 1). A total of 2300 raTKAs were included in the final analysis. The mean age of the treated patients was 67.1 (64.2–71) years, 50.7% were women, and the mean BMI was 30.3 (26.1–33.5) kg/m2. Nine studies used MAKO (Stryker, n: 839 raTKA) [21,22,28,29,30,32,33,34,35], four studies used NAVIO (Smith & Nephew, n: 264 raTKA) [24,25,27,31], one study used Think Surgical (Think Surgical Robot, n:108 raTKA) [26], and one study used ROSA (Zimmer, n: 90 raTKA) [23]. Triathlon (Stryker, n: 1347 RATKA) was the most widely used TKA [21,22,29,30,32,33], followed by Legion (Smith & Nephew, n: 147 RATKA) [24,31], Journey II (Smith & Nephew, n: 117 RATKA) [25,27], Persona (Zimmer, n: 90 RATKA) [26], and Corin (Unity Knee, n: 107 RATKA) [26]. Implants were not specified in three studies (n: 492 RATKA) [28,34,35]. Fourteen studies reported the surgeon’s experience [21,22,23,24,25,26,27,28,29,30,31,32,34,35]. There were nine fellowship-trained surgeons (31%), six “high-volume” (>200 TKA per year) surgeons (20.7%), four surgeons with no previous computer- or robot-assisted TKA experience (13.8%), two surgeons with previous computer- or robot-assisted TKA experience (6.9%), one medium-volume (100–200 TKA per year) surgeon (3.5%), and one low-volume (<100 TKA per year) surgeon (3.5%). In five cases, the surgeon’s experience was not reported (17.3%). The main demographic and surgical characteristics are reported in Table 1.
3.2. Surgical Time
Fourteen surgeons reported the presence of an inflection point during the learning curve. The mean inflection point was observed after 14.9 cases (5–43 cases). Two studies [22,34] reported that the inflection point was reached within the first 200 cases [22] and within the first 40 cases [34]. Five studies reported average surgical times between the learning and proficiency phases [23,24,25,29,33]. Three studies reported that the average surgical time was 98.3 min for the learning phase and 74.4 min for the proficiency phase. Seven studies compared the average surgical time between the first and last cases of raTKA [22,23,24,27,28,34,35]. In all but one case, the average surgical time for the first cases was significantly longer than that of the subsequent cases. The only exception was reported by one of the two surgeons in the study by Ali et al. [28]. They reported no improvement in the average surgical time between the first and last cases of raTKA. Five studies reported a statistically superior average surgical time for the first cases of raTKA patients compared to the average surgical time of manual TKA (mTKA) [24,29,32,34,35]. The surgical time results are reported in Table 2.

Table 2.
Learning curve and surgical time of raTKA.
3.3. Lower Limb Alignment
Four articles found that the learning curve was not associated with implant position [25,26,29,33]. Schopper et al. found a high percentage of outliers in mTKA compared to raTKA after reaching the inflection point [21]. The difference between intraoperative and postoperative measurements was reported in three studies [21,25,29]. One study reported no difference between the two measurements [21]. One study reported that medial proximal tibial angle (MPTA), lateral distal femoral angle (LDFA), and hip–knee–ankle angle (HKA) differed significantly between intraoperative and postoperative measurements [25]. Finally, one study reported that the mean postoperative HKA was 1.2° more valgus than that measured intraoperatively [29]. Three studies reported differences in lower limb alignment between raTKA and mTKA [24,32,33]. Two articles reported significantly better lower limb alignment in the raTKA cohort [24,33]. In contrast, one study reported no difference in lower limb alignment between raTKA and mTKA [32]. The incidence of outliers (mispositioning greater than 3° from planned positioning) was reported by six studies [21,24,25,26,31,32]. Two studies [21,32] did not report any outliers in their cohorts of patients undergoing raTKA. One study [24] reported that the outlier rate was lower in raTKA than in mTKA. One study [26] reported a higher outlier rate in raTKA than in mTKA. Three studies reported the incidence of postoperative outliers between raTKA and mTKA [25,26,31]. The lower limb alignment characteristics are reported in Table 3.

Table 3.
Lower limb alignment characteristics regarding implant position, intraoperative and postoperative measurements, coronal and sagittal alignment, and outliers.
3.4. Complications
One study reported that one complication was observed during the learning phase (one knee arthrofibrosis). Instead, three complications during the proficiency phase (one knee arthrofibrosis, one deep vein thrombosis, and one surgical site infection) [23]. Three studies reported at least one complication related to raTKA [26,29,33]. Four studies reported no complications related to raTKA [23,27,30,32]. Four studies reported complications not related to raTKA [21,23,28,31]. The most frequently reported complication was reduced postoperative range of motion due to knee arthrofibrosis. The reported complications are summarized in Table 4.

Table 4.
Learning/Proficiency phase and complications related and not related to raTKA.
4. Discussion
The use of raTKA is steadily increasing in everyday surgical practice leading to several advantages, such as the reduction of radiographic outliers and risks of iatrogenic soft tissue injuries [14]. Nevertheless, these advantages must be related to higher costs, increased surgical time, and a long learning curve [8,14]. This systematic review aims to evaluate data on the raTKA learning curve in three different areas: surgical time, lower limb alignment, and complications. The main findings of this paper are focused on surgical time. In most cases, the inflection point was recorded between the first 5 and 20 cases, regardless of the surgeon’s experience. The first and last cases reported a significant reduction in surgical time [22,23,24,25,26,27,28]. Additionally, few studies report the raTKA learning curve regarding lower limb alignment, component position, and intraoperative and postoperative complications [21,23,24].
The main finding of this systematic review is that the inflection points in raTKA range from 5 to 43 cases, with a mean of 14.9 cases. In addition, an average decrease in surgical time of 23.9 min was described between the initial and proficiency phases; the average surgical time in the two phases was 98.8 min and 74.4 min, respectively [21,22,23,24,25,26,27]. Schopper et al., in their study, reported that an experienced surgeon could flatten the learning curve, suggesting that companies should provide surgical support from trained personnel during initial cases [21]. Surgical time may be considered an evaluation index of the learning process for surgical procedures. Multiple factors, such as familiarity with displays, landmark registration, and resection techniques, were related to surgical time procedures [38,39,40]. Several studies included in this review reported improved surgical time in the latter cases compared with the first cases [22,23,24,25,26,27,28]. Patel et al. reported that the average surgical time improved significantly between the first and last 50 cases [22].
Similarly, Vanlommel et al. [23] and Bell et al. [27] reported a statistically significant reduction in surgical time in their respective studies. Ali et al. [28] reported a significant improvement in surgical time for only one of the two surgeons involved in their research. Controversially, the results compare the average intervention time of raTKA and mTKA. Thiegwittapown et al. [24] and Naziri et al. [32] reported that the overall time of raTKA was significantly higher than mTKA. On reaching the inflection point, the average surgical time did not differ between mTKA and raTKA [24,29,35]. Thiegeittaporn et al. [24] observed no difference in the mean surgical time for the last ten raTKA and mTKA cases. Similarly, no surgical time differences were reported both either Ali et al. [28] or Vermue et al. [32] in the last cases of raTKA compared to mTKA.
The robots and the implants used differ, so improvements may be found at different surgery phases [39,41,42,43]. Kayani et al. [33] reported that the most remarkable improvement was observed in robot setup (from 14.8 min to 9.2 min), bone registration (from 15.8 min to 11.5 min), bone preparation (from 15.8 min to 11.1 min), and joint balancing (from 14.3 min to 9 min). In contrast, no significant improvement was observed in surgical steps, such as surgical approach, implant trial, cement implantation, and closure. Conversely, different data were reported by Vanlommel et al. [23] that noted a significant improvement not only in robotic setup (from 8.9 min to 7.3 min), bone registration (from 103 min to 7.5 min), and joint balancing (from 7 min to 4.1 min) but also for implant trialing (from 17.3 min to 13.5 min). At the same time, no significant improvement was noted for the surgical approach and bone preparation phases. Bell et al. [27] reported a “dramatic increase in efficiency” during the review of the intraoperative phase, in which the surgeon reviews the bone cuts suggested by the robot.
Appropriate component placement in TKA has a crucial role in improving clinical outcomes and patient satisfaction [7,13,14]. Inadequate implant positioning leads to increased polyethylene wear due to higher contact forces and inappropriate soft tissue tension, reducing implant survival [3,5,39]. Some authors have hypothesized that implant malalignment may reduce postoperative satisfaction because of proprioception changes [1,44,45]. Based on this systematic review, most studies did not report an evident learning curve for component positioning accuracy [25,26,27,28,29]. In their paper, Schopper et al. [21] observed a significantly high rate of misaligned components during the raTKA learning phase compared to the proficiency phase. Furthermore, the authors found no statistically significant differences between intraoperative measurement and postoperative values [21]. On the contrary, Savov et al. [25] reported a statistically significant difference between intraoperative and postoperative valuation, and Vermue et al. [29] described a mean postoperative HKA of 1.2° more valgus than for intraoperative. Thiengwittayaporn et al. [24] showed improved accuracy for HKA, femoral sagittal inclination, and tibial coronal inclination in raTKA. Kayani et al. [23] reported better accuracy for HKA, femoral coronal and sagittal alignment, tibial coronal and sagittal alignment, and tibial slope in raTKA. In contrast, Naziri et al. [32] found no statistically significant differences between patients undergoing mTKA and raTKA.
The studies included in this systematic review reported complications both related and unrelated to robotic-assisted surgery. Vermue et al. [29] described persistent tibial pain at the pin placement site. Further inspections revealed a tibial diaphyseal stress fracture caused by the registration pin insertion. The fracture healed without complications in eight weeks. Mahure et al. [26] reported the persistence of a pin metal fragment in the distal femur that did not result in further complications. Vanlommel et al. [23] described a case of arthrofibrosis during both the learning and proficiency curve phases. Additional complications not directly related to robotic-assisted surgery, such as patellar tendon rupture, arthrofibrosis, tibial fracture, surgical wound dehiscence, deep vein thrombosis, and pulmonary embolism, are also described in the studies included in this systematic review [21,23,28,31]. Ra surgery could simplify and minimize the instrumentation needed to perform surgical procedures, significantly reducing instrumentation sterilization and storage costs. In addition, the time required to prepare the operating room would be reduced, optimizing room rotation and equipment costs. Finally, robotic instruments could contribute to the surgeons’ training because they provide excellent feedback at the time of use, allow accurate data recording, and offer detailed results analysis at the conclusion of surgery [46].
This systematic review presented some limitations. First, the overall quality of the included studies was low; only two papers had LoE of II, while the other studies had LoEs of III and IV. Second, the surgeons’ experiences were very different across the studies, and there was no correlation between these important data and the learning curve. Finally, many papers divided patients into groups, with heterogeneity in the data, including more straightforward cases at the beginning of the learning curve and more complex prostheses in the last phase. Further studies, with a larger and more homogeneous patient sample and longer follow-up, are needed to implement the results obtained in this systematic review.
5. Conclusions
Robotic-assisted surgery was introduced into clinical practice recently to improve component positioning and soft tissue balance during TKA. A major concern is related to the length of the learning curve. The most important finding of this systematic review is that the inflection point is reached early, after an average of 14.9 cases. Another significant result is the absence of a learning curve for implant placement and lower limb alignment, meaning that component position is correct from the earliest cases of raTKA. Finally, the current literature has not provided statistically significant data on any difference in the type and rate of complications during the learning curve of raTKA.
Author Contributions
G.C., F.B., F.G., S.R. and M.C.: designing the work. G.C. and F.B.: acquisition and analysis of the data. G.C.: drafting the work. G.C., F.B., F.G., A.B. and L.S.: revised the work critically for important intellectual content. S.R., A.M. and L.S.: final approval of the version to be published. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| TKA | total knee arthroplasty |
| raTKA | robotic-assisted TKA |
| n | number |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| MINORS | Methodological Index for Non-Randomized Studies |
| LoE | levels of evidence |
| mTKA | manual TKA |
| MPTA | medial proximal tibial angle |
| LDFA | lateral distal femoral angle |
| HKA | hip–knee–ankle angle |
References
- Ayers, D.C.; Yousef, M.; Zheng, H.; Yang, W.; Franklin, P.D. The Prevalence and Predictors of Patient Dissatisfaction 5-years Following Primary Total Knee Arthroplasty. J. Arthroplast. 2022, 37, S121–S128. [Google Scholar] [CrossRef]
- Cacciola, G.; Mancino, F.; De Meo, F.; Di Matteo, V.; Sculco, P.K.; Cavaliere, P.; Maccauro, G.; De Martino, I. Mid-term survivorship and clinical outcomes of the medial stabilized systems in primary total knee arthroplasty: A systematic review. J. Orthop. 2021, 24, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Cacciola, G.; De Martino, I.; De Meo, F. Does the medial pivot knee improve the clinical and radiographic outcome of total knee arthroplasty? A single centre study on two hundred and ninety seven patients. Int. Orthop. 2020, 44, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Quack, V.M.; Kathrein, S.; Rath, B.; Tingart, M.; Lüring, C. Computer-assisted navigation in total knee arthroplasty: A review of literature. Biomed. Tech. 2012, 57, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Risitano, S.; Cacciola, G.; Sabatini, L.; Capella, M.; Bosco, F.; Giustra, F.; Massè, A.; Vaishya, R. Restricted kinematic alignment in primary total knee arthroplasty: A systematic review of radiographic and clinical data. J. Orthop. 2022, 33, 37–43. [Google Scholar] [CrossRef]
- Laverdière, C.; Corban, J.; Khoury, J.; Ge, S.M.; Schupbach, J.; Harvey, E.J.; Reindl, R.; Martineau, P.A. Augmented reality in orthopaedics: A systematic review and a window on future possibilities. Bone Jt. J. 2019, 101-B, 1479–1488. [Google Scholar] [CrossRef]
- Mancino, F.; Rossi, S.; Sangaletti, R.; Lucenti, L.; Terragnoli, F.; Benazzo, F. A new robotically assisted technique can improve outcomes of total knee arthroplasty comparing to an imageless navigation system. Arch. Orthop. Trauma Surg 2022. epub ahead of print. [Google Scholar] [CrossRef]
- Sabatini, L.; Bosco, F.; Barberis, L.; Camazzola, D.; Bistolfi, A.; Risitano, S.; Massè, A.; Indelli, P.F. Kinetic Sensors for Ligament Balance and Kinematic Evaluation in Anatomic Bi-Cruciate Stabilized Total Knee Arthroplasty. Sensors 2021, 21, 5427. [Google Scholar] [CrossRef]
- Bistolfi, A.; Giustra, F.; Bosco, F.; Faccenda, C.; Viotto, M.; Sabatini, L.; Berchialla, P.; Sciannameo, V.; Graziano, E.; Massè, A. Comparable results between crosslinked polyethylene and conventional ultra-high molecular weight polyethylene implanted in total knee arthroplasty: Systematic review and meta-analysis of randomised clinical trials. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3120–3130. [Google Scholar] [CrossRef]
- Bistolfi, A.; Giustra, F.; Bosco, F.; Sabatini, L.; Aprato, A.; Bracco, P.; Bellare, A. Ultra-high molecular weight polyethylene (UHMWPE) for hip and knee arthroplasty: The present and the future. J. Orthop. 2021, 25, 98–106. [Google Scholar] [CrossRef]
- Fujie, M.G.; Zhang, B. State-of-the-art of intelligent minimally invasive surgical robots. Front. Med. 2020, 14, 404–416. [Google Scholar] [CrossRef]
- Rossi, S.; Sangaletti, R.; Perticarini, L.; Terragnoli, F.; Benazzo, F. High accuracy of a new robotically assisted technique for total knee arthroplasty: An in vivo study. Knee Surg. Sports Traumatol. Arthrosc. 2022, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mancino, F.; Cacciola, G.; Malahias, M.-A.; De Filippis, R.; De Marco, D.; Di Matteo, V.; Gu, A.; Sculco, P.K.; Maccauro, G.; De Martino, I. What are the benefits of robotic-assisted total knee arthroplasty over conventional manual total knee arthroplasty? A systematic review of comparative studies. Orthop. Rev. 2020, 12, 8657. [Google Scholar] [CrossRef] [PubMed]
- Goyal, T.; Choudhury, A.K.; Paul, S.; Das, L.; Gupta, T. The direct anterior approach without traction table: How does it compare with the posterior approach?—A prospective non-randomised trial. J. Clin. Orthop. Trauma 2022, 31, 101924. [Google Scholar] [CrossRef] [PubMed]
- Hopper, A.N.; Jamison, M.H.; Lewis, W.G. Learning curves in surgical practice. Postgrad Med. J. 2007, 83, 777–779. [Google Scholar] [CrossRef] [PubMed]
- Yotsumoto, F.; Sanui, A.; Ito, T.; Miyahara, D.; Yoshikawa, K.; Shigekawa, K.; Noguchi, Y.; Yasunaga, S.; Miyamoto, S. Cumulative Summation Analysis of Learning Curve for Robotic-assisted Hysterectomy in Patients With Gynecologic Tumors. Anticancer Res. 2022, 42, 4111–4117. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef]
- Giai Via, R.; Bosco, F.; Giustra, F.; Lavia, A.D.; Artiaco, S.; Risitano, S.; Giachino, M.; Massè, A. Acute Rockwood type III ACJ dislocation: Conservative vs surgical approach. A systematic review and meta-analysis of current concepts in literature. Injury 2022, 53, 3094–3101. [Google Scholar] [CrossRef]
- Schopper, C.; Proier, P.; Luger, M.; Gotterbarm, T.; Klasan, A. The learning curve in robotic assisted knee arthroplasty is flattened by the presence of a surgeon experienced with robotic assisted surgery. Knee Surg. Sports Traumatol. Arthrosc. 2022. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.; Judd, H.; Harm, R.G.; Nolan, J.R.; Hummel, M.; Spanyer, J. Robotic-assisted total knee arthroplasty: Is there a maximum level of efficiency for the operating surgeon? J Orthop. 2022, 31, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Vanlommel, L.; Neven, E.; Anderson, M.B.; Bruckers, L.; Truijen, J. The initial learning curve for the ROSA® Knee System can be achieved in 6-11 cases for operative time and has similar 90-day complication rates with improved implant alignment compared to manual instrumentation in total knee arthroplasty. J. Exp. Orthop. 2021, 8, 119. [Google Scholar] [CrossRef]
- Thiengwittayaporn, S.; Uthaitas, P.; Senwiruch, C.; Hongku, N.; Tunyasuwanakul, R. Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: A randomized controlled trial. Int. Orthop. 2021, 45, 2851–2858. [Google Scholar] [CrossRef] [PubMed]
- Savov, P.; Tuecking, L.R.; Windhagen, H.; Ehmig, J.; Ettinger, M. Imageless robotic handpiece-assisted total knee arthroplasty: A learning curve analysis of surgical time and alignment accuracy. Arch. Orthop. Trauma Surg. 2021, 141, 2119–2128. [Google Scholar] [CrossRef]
- Mahure, S.A.; Teo, G.M.; Kissin, Y.D.; Stulberg, B.N.; Kreuzer, S.; Long, W.J. Learning curve for active robotic total knee arthroplasty. Knee Surg Sports Traumatol. Arthrosc. 2022, 30, 2666–2676. [Google Scholar] [CrossRef]
- Bell, C.; Grau, L.; Orozco, F.; Ponzio, D.; Post, Z.; Czymek, M.; Ong, A. The successful implementation of the Navio robotic technology required 29 cases. J. Robot Surg. 2022, 16, 495–499. [Google Scholar] [CrossRef]
- Ali, M.; Phillips, D.; Kamson, A.; Nivar, I.; Dahl, R.; Hallock, R. Learning Curve of Robotic-Assisted Total Knee Arthroplasty for Non-Fellowship-Trained Orthopedic Surgeons. Arthroplast. Today 2022, 13, 194–198. [Google Scholar] [CrossRef]
- Vermue, H.; Luyckx, T.; Winnock de Grave, P.; Ryckaert, A.; Cools, A.S.; Himpe, N.; Victor, J. Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 593–602. [Google Scholar] [CrossRef]
- King, C.A.; Jordan, M.; Bradley, A.T.; Wlodarski, C.; Tauchen, A.; Puri, L. Transitioning a Practice to Robotic Total Knee Arthroplasty Is Correlated with Favorable Short-Term Clinical Outcomes-A Single Surgeon Experience. J. Knee Surg. 2022, 35, 78–82. [Google Scholar] [CrossRef]
- Collins, K.; Agius, P.A.; Fraval, A.; Petterwood, J. Initial Experience with the NAVIO Robotic-Assisted Total Knee Replacement-Coronal Alignment Accuracy and the Learning Curve. J. Knee Surg. 2021, 35, 1295–1300. [Google Scholar] [CrossRef] [PubMed]
- Naziri, Q.; Cusson, B.C.; Chaudhri, M.; Shah, N.V.; Sastry, A. Making the transition from traditional to robotic-arm assisted TKA: What to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J. Orthop. 2019, 16, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Huq, S.S.; Tahmassebi, J.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1132–1141. [Google Scholar] [CrossRef] [PubMed]
- Grau, L.; Lingamfelter, M.; Ponzio, D.; Post, Z.; Ong, A.; Le, D.; Orozco, F. Robotic arm assisted total knee arthroplasty workflow optimization, operative times and learning curve. Arthroplast. Today 2019, 5, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Sodhi, N.; Khlopas, A.; Piuzzi, N.S.; Sultan, A.A.; Marchand, R.C.; Malkani, A.L.; Mont, M.A. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J. Knee Surg. 2018, 31, 17–21. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Lopez, I.B.; Benzakour, A.; Mavrogenis, A.; Benzakour, T.; Ahmad, A.; Lemée, J.M. Robotics in spine surgery: Systematic review of literature. Int. Orthop. 2022. epub ahead of print. [Google Scholar] [CrossRef]
- Mancino, F.; Cacciola, G.; Di Matteo, V.; Perna, A.; Proietti, L.; Greenberg, A.; Ma, M.; Sculco, P.K.; Maccauro, G.; De Martino, I. Surgical implications of the hip-spine relationship in total hip arthroplasty. Orthop. Rev. 2020, 12 (Suppl. S1), 8656. [Google Scholar] [CrossRef]
- Mullaji, A.B.; Khalifa, A.A. Is it prime time for robotic-assisted TKAs? A systematic review of current studies. Journal of orthopaedics. J. Orthop. 2022, 34, 31–39. [Google Scholar] [CrossRef]
- Cacciola, G.; De Meo, F.; Cavaliere, P. Mechanical and elution properties of G3 Low Viscosity bone cement loaded up to three antibiotics. J. Orthop. 2018, 15, 1004–1007. [Google Scholar] [CrossRef] [PubMed]
- Kreuzer, S.; Brar, A.; Campanelli, V. Dimensional accuracy of TKA cut surfaces with an active robotic system. Comput. Assist Surg. 2022, 27, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Ueno, J.; Torii, Y.; Umehra, T.; Iinuma, M.; Yoshida, A.; Tomochika, K.; Niki, H.; Akazawa, T. Robotics is useful for less-experienced surgeons in spinal deformity surgery. Eur. J. Orthop. Surg. Traumatol 2022. epub ahead of print. [Google Scholar] [CrossRef]
- Scott, C.E.; Howie, C.R.; MacDonald, D.; Biant, L.C. Predicting dissatisfaction following total knee replacement: A prospective study of 1217 patients. J. Bone Jt. Surg. Br. 2010, 92, 1253–1258. [Google Scholar] [CrossRef] [PubMed]
- Muertizha, M.; Cai, X.; Ji, B.; Aimaiti, A.; Cao, L. Factors contributing to 1-year dissatisfaction after total knee arthroplasty: A nomogram prediction model. J. Orthop. Surg. Res. 2022, 17, 367. [Google Scholar] [CrossRef] [PubMed]
- Parsley, B.S. Robotics in Orthopedics: A Brave New World. J. Arthroplast. 2018, 33, 2355–2357. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).