Abstract
Knee alignment after total knee arthroplasty (TKA) is essential for implant survival. Several studies on accelerometer-based navigation systems have given controversial results, with or without improvement in knee alignment. The aim was to evaluate the accuracy of an accelerometer-based navigation system for tibial resection during total knee arthroplasty. Twenty TKAs performed with an accelerometer-based navigation system were included in this prospective–comparative study. They were matched (on age, body mass index, and preoperative mechanical axis of the lower limb) in a 2:1 ratio with TKA performed with a conventional technique. The objective of this study was to determine the accuracy of the Perseus System for making the tibial cut on TKA. The primary endpoint was the tibial mechanical angle (TMA) measured on radiographic images at two months postoperatively. Secondary endpoints were the tibial slope and the mechanical axis of the lower limb (HKA angle, Hip-Knee-Ankle). The mean TMA in the accelerometer group was 87.6 ± 2.1° versus 89.1 ± 1.6° in the control group (p < 0.01). The tibial slope in the accelerometer group was 90.0 ± 1.9° versus 89.9 ± 1.3° in the control group (not significant). The mean HKA was 177.7 ± 1.8° in the accelerometer group and 177.5 ± 2.2° in the control group (not significant). This accelerometer-based navigation system during TKA did not improve the accuracy of the tibial cut compared to the conventional technique, but it restored the tibial slope.
1. Introduction
Despite much progress in implant design, surgical techniques and early rehabilitation, a significant proportion of patients remain unsatisfied with total knee arthroplasty (TKA). The implant positioning in the three planes of space during total knee arthroplasty (TKA) is crucial to obtain satisfying functional outcomes, few revisions, and a high survival rate [1,2]. New or “modern” concepts about the alignment are a current question in the improvement of TKA outcomes. However, regardless of the type of alignment (mechanical, kinematic, limited kinematic), the accuracy of the tibia and femur cuts is still crucial.
This is especially important for kinematic alignment. A 3° error in component alignment has serious consequences if the target alignment is already in varus or valgus.
A previous study has shown that TKA performed with extramedullary guides has a correct coronal alignment (more or less 3° around neutral mechanical axis) in only 70 to 80% of cases [3]. Recently, new technologies have been developed to improve the accuracy, reliability, and reproducibility of knee arthroplasty implantation, such as personalized cutting guides [4], computer-assisted navigation [5], or navigation with robotic assistance [6,7,8]. Accelerometer-based sensor navigation has also emerged, using an independent mass-spring system that measures linear acceleration in all three space planes. Accelerometer-based navigation is a portable surgical navigation system that does not use a large computer console for TKA (Figure 1). The first validation study about this system was in 2011 (cadaveric study) [9]. Accelerometer-bases navigation is a hand-held, sterile device used within the operative field to determine the resection planes of distal femoral and proximal tibial cut, analyzing the hip rotation center and the femoral mechanical axis. These wireless, imageless systems collect data intraoperatively and display the data directly on pods attached to the femoral and tibial resection guides. These systems guide resection angles in the coronal and sagittal planes, and also can confirm alignment accuracy of cuts after resection. Unlike other assistive technologies, this system does not need intra-bone captors or preoperative 3D imaging. All these navigation technologies aim to make prosthetic positioning more accurate in usual situations by choosing angular values for bone cuts, but also to be able to bypass obstacles to conventional techniques (bone callus, extra-articular deformity, intramedullary material).
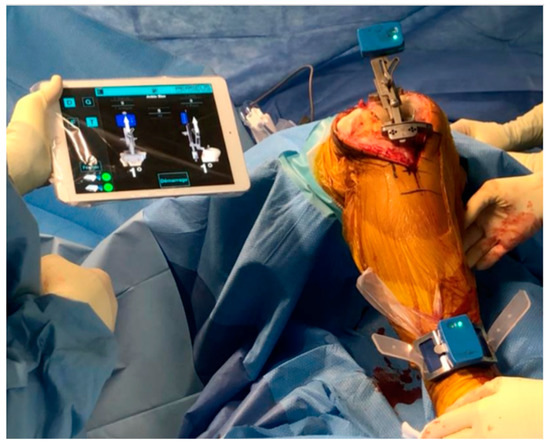
Figure 1.
Navigation setup with software and sensors.
Computer-assisted navigation has already proved its benefits in these particular situations. Still, its usefulness in first-line surgery remains debated because of its questionable clinical benefits and high cost [5,10]. Accelerometer navigation has the advantage of low cost, small size, and the lack of intraosseous sensors as conventional navigation systems. This navigation system has been described with an accuracy equivalent to or superior to standard mechanical instrumentation [11]. Different models of accelerometers exist with a precision that seems to be demonstrated [12,13,14,15,16,17]. However, some systems’ accuracy, like Perseus, has not yet been evaluated. The objective of this study was to assess the accuracy of the Perseus System for making the tibial cut on TKA to determine if this technique is safe and accurate. The hypothesis was that the accuracy of accelerometer-based navigation is non-inferior to mechanical conventional instrumentation for tibial cut.
2. Materials and Methods
2.1. Study Design
This is a prospective, comparative, single-centre study. The inclusion criteria were a primary TKA for medial femorotibial osteoarthritis without previous osteotomy. The exclusion criteria were a revision of TKA, lateral femorotibial osteoarthritis or isolated patellofemoral osteoarthritis, and previous osteotomy surgery. The accelerometer-based navigation system was used according to the system’s availability and systematically when a patient can be included. The patients in the accelerometer group were operated on with the Perseus system for the tibial cut and the conventional ancillary for the femoral cuts. Twenty patients (20 TKA) were included in this study group. Patients in the accelerometer group were matched 2:1 on age, body mass index (BMI), and preoperative deformity (HKA angle: Hip Knee Ankle angle) with previous primary TKA to form the control group. The patients in the control group were operated on with conventional ancillary for all the cuts. Forty patients (40 TKA) were included in this control group. Demographic data are presented in Table 1. There was no significant difference between the two groups. The average age was 70 years-old in both groups. BMI was 30.4 and 30.2, there was 50% and 45% of females in the Perseus and Control group respectively. Pre-operative HKA was 172.5° in the Perseus group and 173.1 in the Control group. Patients were included between 2020 and 2021. The mean follow-up was 12 months. No patients were lost to follow-up.

Table 1.
Pre-operative characteristics.
The same single primary prosthesis was used for all patients: a postero-stabilized TKA with a third condyle, rotational tibial plateau, and with patellar resurfacing (HLS Kneetec, CORIN®, Tampa, FL, USA). All surgeries were performed with a thigh root tourniquet inflated to 300 mmHg. All implants were cemented with high viscosity cement. A trans-quadricipital medial approach was used for all patients. No femoral rotation was applied; the distal femoral cut was made with a 7° valgus intramedullary guide.
The tibial cut was performed in the control group using a mechanical instrumentation device with intra-medullary and extra-medullary guides. In the accelerometer group, the tibial cut was performed with an accelerometer-based navigation system, the Perseus system (ORTHOKEY®, Næstved, Denmark). This system was based on sensors connected via Bluetooth to a tablet available on the operating field in sterile packaging. Two sensors (single-use, sterile-packed) per surgery were required, one on the cutting guide and the other attached to the ankle with a dedicated elastic band (Figure 1). The targets recorded on the software were a mechanical alignment with a tibial cut at 90° of the tibial mechanical axis in the frontal plane and with a slope of 90°. The calibration and the acquisition of the good positioning of the cutting guide were obtained by two series of knee movements in the sagittal and frontal planes. After adjusting the cutting guide in the frontal plane (Varus/Valgus) and the sagittal plane (tibial slope) according to the indications on the software, the cutting guide was fixed with dedicated pins. To confirm the position of the cutting guide before the tibial cut, we performed two acquisitions (Figure 2). Once the tibial cut was made using the accelerometer sensors, the rest of the surgical technique was similar to the control group. All patients had a patellar resurfacing, using an on-lay symmetrical spherical dome-shaped polyethylene patellar button. The patellar resurfacing cut was performed such that a minimal thickness of 14 mm of patellar bone remained. A lateral release was performed to improve patellar tracking in cases of patellar subluxation during flexion. A vacuum drain was used only in case an early curative anticoagulation was necessary.
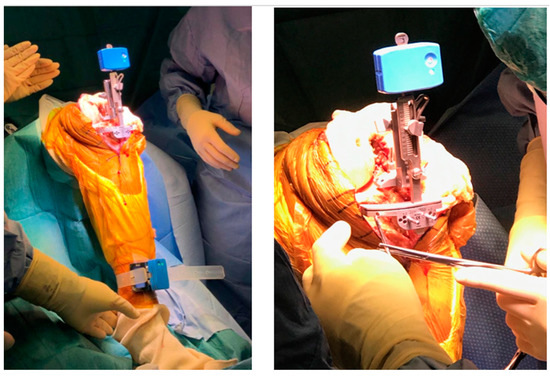
Figure 2.
Cutting guide adjustment, before guide fixation then tibial cut.
2.2. Data Assessment
All patients received the same perioperative management. Full weight-bearing with an early rehabilitation was performed for all patients. Clinical and radiological follow-up was conducted at 2 months and then 12 months post-operatively. The radiological assessment included weight-bearing anteroposterior and lateral views, axial view of the patellae at 30° of flexion, and standing long-leg radiographs. We measured the Hip Knee Ankle (HKA) angle, the mechanical femoral and tibial axis, and the tibial slope. The complications and revisions were recorded at the last follow-up. All measurements were performed by the same independent and blinded surgeon observer using the scale provided by the radiological software (Centricity Universal Viewer, version 6.0 SP10.2, GE Healthcare, 540 West Northwest Highway, Barrington, IL 60010, USA). Our primary endpoint was the tibial mechanical angle (TMA), representing the alignment of the tibial component in the frontal plane. Secondary endpoints were the tibial slope (sagittal tibial alignment) and the overall mechanical axis of the lower limb (HKA angle). We also measured the femoral mechanical angle (FMA) as an indicator because it influences the HKA but does not correlate with the tibial cutting technique being tested. We also reported the proportion of “outliers” for each angular value measured. Data were classified as “outliers” if they were beyond 3° of the targets (HKA: 180°, TMA: 90°, tibial slope: 90°, FMA: 90°).
2.3. Statistical Analysis
Continuous variables were averaged and reported with standard deviations. Quantitative variables were analyzed with Student’s t-test and qualitative data using χ2. We had planned to include 120 patients matched in the same 2:1 ratio, the mid-inclusion interim analysis found a difference between the two groups in favor of the mechanical ancillary so we stopped the inclusions. The value of p < 0.05 was defined as the statistical threshold. Statistical analysis was performed using R software version 3.6.1 (R Development Core Team, Vienna, Austria).
3. Results
The postoperative radiological measurements are presented in Table 2. For the primary endpoint, the mean TMA in the Perseus group was 87.6 ± 2.1° versus 89.1 ± 1.6° in the control group (p < 0.01) (Figure 3). The tibial slope in the Perseus group was 90.0 ± 1.9° versus 89.9 ± 1.3° in the control group (not significant). The mean HKA was 177.7 ± 1.8° and 177.5 ± 2.2° in the Perseus and control groups, respectively (not significant). The comparison of the FMA did not show any significant difference. The study of outliers did not reveal any statistically significant difference and found, respectively, in the Perseus and control groups 15% and 7.5% for TMA, 10% and 5% for tibial slope, 15% and 25% for HKA, and 5 and 7.5% for FMA (not significant). There were no complications or revisions at the last follow-up in both groups.

Table 2.
Post-operative results.
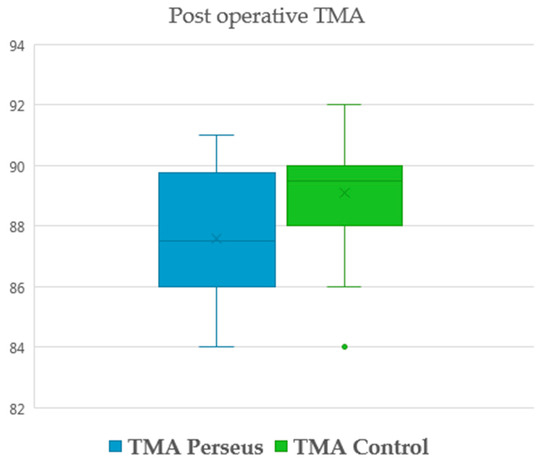
Figure 3.
TMA comparison chart.
4. Discussion
While most patients undergoing TKA are satisfied with the outcome, about a quarter of the patients remain dissatisfied, to varying degrees, even in the absence of a complication. Several factors may be involved, including inappropriate indications, a lack of preoperative information, and surgical factors such as implant alignment, ligament balance or post-operative complications.
The positioning of the prosthesis is a determining factor in the medium- and long-term results [1,2], which is why technological progress has focused on tools that allow personalized and reproducible positioning. Accelerometers are part of the range of tools available to optimize positioning or at least make it more reproducible. The aim of this study was to evaluate the accuracy of the Perseus System for making the tibial cut on TKA, to determine if this technique is safe and reproducible.
Analysis of the primary endpoint showed that the tibial cut navigated by the Perseus accelerometer had a significant tendency to varus of 1.5° compared with the control group. On the other hand, accelerometer navigation allowed a satisfying restitution of the tibial slope in the sagittal plane, but without being superior to the conventional instrumentation. Accelerometer navigation was not more accurate than conventional instrumentation for the tibial cut in this study.
The studies in the literature are not consistent as to whether accelerometers improve the tibial cut’s accuracy. Several accelerometer systems are available and assessed in the literature. Due to a potential disparity, an independent assessment of every accelerometer system seems more appropriate. Matsumoto et al. and Ueyama et al. respectively found satisfying results with TMA values of 90.1 ± 1.4° and 89.8 ± 1.4° in the accelerometer groups, compared with 89.6 ± 1.3° and 90.1 ± 1.4° in the groups with conventional instrumentation, with no significant difference [18,19], as did Gharaibeh et al. [13]. Several studies reported a valgus deviation of the tibial cut (range from 0.4° to 1.3°) [20,21,22]. Conversely, Iorio et al. and Nam et al. found a varus cut of 0.55 ± 0.43° and 0.77 ± 0.64°, respectively [23,24]. This study also reported a varus deviation of the tibial cut in a population with preoperative varus deformity. This kind of deviation had fewer consequences for the implant survival, theoretically, because this deviation remained inferior to 3° and was in the same deformity as preoperatively. Most studies found no difference in tibial slope from conventional instrumentation [21,22,23]. However, some authors reported a moderate increase in the tibial slope of 0.5° to 1° on average [20,24]. The accelerometer system assessed in this study accurately reproduced the tibial slope with no significant difference from conventional instrumentation.
More than the comparison of mean angle values, the rate of outliers is an interesting indicator of a surgical technique’s reproducibility and reliability. In this study, the mean frontal deviation in the accelerometer group was inferior to the 3° margin of error. These results were similar to those in the literature [13,15,18]. However, the rate of outliers for the frontal axis of the tibial cut was not low (15%). The lack of significant difference between both groups for the outliers’ rate could be secondary to the small size of the groups in this study. The literature seems to be unequivocal on the outliers’ rate with accelerometer navigation, showing a significant reduction of the outliers’ rate [25,26,27], particularly for the mechanical femoral angle (FMA) [18,28]. In a randomized controlled trial involving 100 patients, where 50 were operated on with accelerometer navigation, Minoda et al. found a proportion of outliers of 9% in the accelerometer group vs. 27% in the control group for the TMA, and 31% vs. 49% respectively for the HKA [29]. Ueyama et al. found 3% of outliers with FMA with accelerometer system versus 15% with conventional instrumentation, with no difference with TMA in a retrospective study of 159 TKAs [18]. In addition, Li et al. in a recent systematic review of randomized controlled trials, found less outliers with mechanical alignment (relative risk increase of 38% to be an outlier on HKA with conventional technique) [11]. The improvement in clinical results due to accelerometer navigation has not been demonstrated [12], and the time since the introduction of this technology does not yet allow for sufficient long-term follow-up, where the reduction in the number of outliers could show significant progress in terms of loosening. Budhiparama et al. have described the results of the main studies about accelerometers in a systematic review [12]. Five of nine studies found a better HKA restoration in accelerometer-assisted TKA [13,14,25,30,31], while the other four found no difference between the two procedures (conventional vs. accelerometer-assisted) [18,26,32,33]. More recently, Jagadeesh et al., in a prospective study using 122 TKA, found a good accuracy of accelerometer navigation system for tibial cut, finding a better precision on TMA and HKA angles (89.2 ± 1.7° and 179.2 ± 1.8° in accelerometer-navigation group, and 87.4 ± 1.5° and 177.3 ± 2.8° in conventional technique group) [34]. Regarding femoral component coronal-axis alignment, seven of nine studies found a better precision with accelerometer-based navigation [13,14,18,25,30,31]. Nevertheless, there was no significant difference in sagittal alignment. However, Wood et al. report better results in the short term (mean follow-up time 2.7 months) [35]. There are no specific complications or revisions due to the accelerometer system reported in the literature. Indeed, there are no bone trackers, irradiated exams, or other invasive steps with this kind of system. The accelerometer systems also present an interesting facet in complex cases. Indeed, this system can be helpful when the mechanical ancillary device fails, particularly in the case of extra-articular deformity [36,37], intramedullary obstacle, or kinematic alignment [38].
This study had some limitations. First, only the tibial cut was assessed because the workflow of the conventional technique for the femur starts with the posterior cuts, which drives the distal cuts. Moreover, our study was prospective but with a long inclusion period (one year) due to the current world pandemic, with a sometimes long time between surgeries, which could disrupt the learning curve necessary for using the material under study. However, with the Perseus technology, Bonanzinga et al. reported intra-observer and inter-observer correlation rates of 75% and 90% [39]. Finally, the number of patients was small. Nevertheless, with the significant early difference in the tibial cut’s accuracy, including more patients did not appear appropriate.
This study reported interesting data not yet described concerning this specific accelerometer system.
Future Perspective
A larger-scale, prospective, randomized trial would improve knowledge of the effect of this technology on long-term results, both in terms of quality of life, functional results and implant survival (long-term loosening rate). In addition, accelerometer assistance would allow navigation for the distal femoral cut as well, and the study of the combined precision of the tibial and distal femoral cuts would be relevant. On another side, the evolution towards reusable sensors would be preferable to single-use sensors; however the sterilization of electronic equipment is still difficult to achieve.
5. Conclusions
This accelerometer-based navigation system during TKA did not improve the accuracy of the tibial cut in the coronal plane compared to the conventional technique, but it did restore the tibial slope, and led to a low and comparable rate of radiological outliers. However, by having an accuracy not inferior to the conventional technique, this system can be a real asset for the surgeon and the patient in case of failure of the standard instrumentation without significant additional cost and with a satisfactory accuracy.
Author Contributions
Conceptualization, L.J. and C.B.; methodology, L.J. and C.B.; validation, S.L. and E.S.; formal analysis, L.J.; investigation, L.J.; data curation, L.J.; writing—original draft preparation, L.J.; writing—review and editing, C.B., S.L., E.S.; supervision, S.L. and E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The paper was approved by the Inst. Review Board. Approval to collect the data both retrospectively and prospectively for the study was granted by The Advisory Committee on Research Information Processing in the Field of Health (CCTIRS) approved this study on 24 January 2012 and 9 March 2015 (approval #11-681).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The sensors required for the study were provided free of charge by the CORIN® company.
Conflicts of Interest
L.J., C.B.: declare that they have no conflict of interest. S.L.: Consultant for Stryker, Smith and Nephew, Heraeus, Depuy Synthes. Institutional research support to Lepine and Amplitude. Editorial Board for Journal of Bone and Joint Surgery (Am). E.S.: institutional research support from Corin.
References
- Fang, D.M.; Ritter, M.A.; Davis, K.E. Coronal Alignment in Total Knee Arthroplasty: Just How Important is it? J. Arthroplast. 2009, 24, 39–43. [Google Scholar] [CrossRef]
- Ritter, M.A.; Davis, K.E.; Meding, J.B.; Pierson, J.L.; Berend, M.E.; Malinzak, R.A. The Effect of Alignment and BMI on Failure of Total Knee Replacement. J. Bone Jt. Surg. 2011, 93, 1588–1596. [Google Scholar] [CrossRef] [PubMed]
- Mizu-Uchi, H.; Matsuda, S.; Miura, H.; Okazaki, K.; Akasaki, Y.; Iwamoto, Y. The evaluation of post-operative alignment in total knee replacement using a CT-based navigation system. J. Bone Jt. Surg. 2008, 90, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Lei, K.; Liu, L.; Chen, X.; Feng, Q.; Yang, L.; Guo, L. Navigation and robotics improved alignment compared with PSI and conventional instrument, while clinical outcomes were similar in TKA: A network meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 30, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.W.; Jerabek, S.A. Current Role of Computer Navigation in Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 1989–1993. [Google Scholar] [CrossRef] [PubMed]
- Batailler, C.; Bordes, M.; Lording, T.; Nigues, A.; Servien, E.; Calliess, T.; Lustig, S. Improved sizing with image-based robotic-assisted system compared to image-free and conventional techniques in medial unicompartmental knee arthroplasty. Bone Jt. J. 2021, 103, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Khlopas, A.; Sodhi, N.; Sultan, A.; Chughtai, M.; Molloy, R.M.; Mont, M.A. Robotic Arm–Assisted Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 2002–2006. [Google Scholar] [CrossRef] [PubMed]
- Van der List, J.P.; Chawla, H.; Pearle, A.D. Robotic-assisted knee arthroplasty: An overview. Am. J. Orthop. 2016, 45, 202–211. [Google Scholar] [PubMed]
- Nam, D.; Jerabek, S.A.; Cross, M.B.; Mayman, D.J. Cadaveric analysis of an accelerometer-based portable navigation device for distal femoral cutting block alignment in total knee arthroplasty. Comput. Aided Surg. 2012, 17, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Mathew, K.K.; Marchand, K.B.; Tarazi, J.M.; Salem, H.S.; DeGouveia, W.; Ehiorobo, J.O.; Sodhi, N.; Mont, M.A. Computer-Assisted Navigation in Total Knee Arthroplasty. Surg. Technol. Int. 2020, 36, 323–330. [Google Scholar]
- Li, J.; Zhang, Y.; Gao, X.; Dou, T.; Li, X. Accelerometer-based navigation vs. conventional techniques for total knee arthroplasty (TKA): A systematic review and meta-analysis of randomized controlled trials. Arthroplasty 2022, 4, 35. [Google Scholar] [CrossRef]
- Budhiparama, N.C.; Lumban-Gaol, I.; Ifran, N.N.; Parratte, S.; Nelissen, R. Does Accelerometer-based Navigation Have Any Clinical Benefit Compared with Conventional TKA? A Systematic Review. Clin. Orthop. Relat. Res. 2019, 477, 2017–2029. [Google Scholar] [CrossRef] [PubMed]
- Gharaibeh, M.A.; Solayar, G.N.; Harris, I.A.; Chen, D.B.; MacDessi, S.J. Accelerometer-Based, Portable Navigation (KneeAlign) vs. Conventional Instrumentation for Total Knee Arthroplasty: A Prospective Randomized Comparative Trial. J. Arthroplast. 2017, 32, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Goh, G.S.-H.; Liow, M.H.L.; Tay, D.K.-J.; Lo, N.-N.; Yeo, S.-J.; Tan, M.-H. Accelerometer-Based and Computer-Assisted Navigation in Total Knee Arthroplasty: A Reduction in Mechanical Axis Outliers Does Not Lead to Improvement in Functional Outcomes or Quality of Life When Compared to Conventional Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 379–385. [Google Scholar] [CrossRef]
- Nam, D.; Jerabek, S.A.; Haughom, B.; Cross, M.B.; Reinhardt, K.R.; Mayman, D.J. Radiographic Analysis of a Hand-Held Surgical Navigation System for Tibial Resection in Total Knee Arthroplasty. J. Arthroplast. 2011, 26, 1527–1533. [Google Scholar] [CrossRef]
- Nam, D.; Weeks, K.D.; Reinhardt, K.R.; Nawabi, D.H.; Cross, M.B.; Mayman, D.J. Accelerometer-Based, Portable Navigation vs Imageless, Large-Console Computer-Assisted Navigation in Total Knee Arthroplasty. J. Arthroplast. 2013, 28, 255–261. [Google Scholar] [CrossRef]
- Muccioli, G.M.M.; Alesi, D.; Russo, A.; Presti, M.L.; Sassoli, I.; La Verde, M.; Zaffagnini, S. Intra- and inter-operator reliability assessment of a novel extramedullary accelerometer-based smart cutting guide for total knee arthroplasty: An in vivo study. Int. Orthop. 2022, 47, 83–87. [Google Scholar] [CrossRef]
- Ueyama, H.; Matsui, Y.; Minoda, Y.; Matsuura, M.; Nakamura, H. Using Accelerometer-Based Portable Navigation to Perform Accurate Total Knee Arthroplasty Bone Resection in Asian Patients. Orthopedics 2017, 40, e465–e472. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Fukuta, M.; Mori, N.; Akiyama, H.; Ogawa, H. Comparative Study for Alignment of Extramedullary Guides versus Portable, Accelerometer-Based Navigation in Total Knee Arthroplasty. J. Knee Surg. 2017, 31, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Bugbee, W.D.; Kermanshahi, A.Y.; Munro, M.M.; McCauley, J.C.; Copp, S.N. Accuracy of a hand-held surgical navigation system for tibial resection in total knee arthroplasty. Knee 2014, 21, 1225–1228. [Google Scholar] [CrossRef]
- Fujimoto, E.; Sasashige, Y.; Nakata, K.; Yokota, G.; Omoto, T.; Ochi, M. Technical Considerations and Accuracy Improvement of Accelerometer-Based Portable Computer Navigation for Performing Distal Femoral Resection in Total Knee Arthroplasty. J. Arthroplast. 2016, 32, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.H.; Copp, S.N.; Bugbee, W.D. Accuracy of A Handheld Accelerometer-Based Navigation System for Femoral and Tibial Resection in Total Knee Arthroplasty. J. Arthroplast. 2015, 30, 1906–1910. [Google Scholar] [CrossRef]
- Iorio, R.; Mazza, D.; Drogo, P.; Bolle, G.; Conteduca, F.; Redler, A.; Valeo, L.; Conteduca, J.; Ferretti, A. Clinical and radiographic outcomes of an accelerometer-based system for the tibial resection in total knee arthroplasty. Int. Orthop. 2014, 39, 461–466. [Google Scholar] [CrossRef]
- Nam, D.; Dy, C.J.; Cross, M.B.; Kang, M.N.; Mayman, D.J. Cadaveric results of an accelerometer based, extramedullary navigation system for the tibial resection in total knee arthroplasty. Knee 2011, 19, 617–621. [Google Scholar] [CrossRef]
- Ikawa, T.; Takemura, S.; Kim, M.; Takaoka, K.; Minoda, Y.; Kadoya, Y. Usefulness of an accelerometer-based portable navigation system in total knee arthroplasty. Bone Jt. J. 2017, 99, 1047–1052. [Google Scholar] [CrossRef]
- Kinney, M.C.; Cidambi, K.R.; Severns, D.L.; Gonzales, F.B. Comparison of the iAssist Handheld Guidance System to Conventional Instruments for Mechanical Axis Restoration in Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Li, S.; Wang, K.; Wu, G.; Zhou, J.; Sun, X. Efficacy of Portable Accelerometer-Based Navigation Devices versus Conventional Guides in Total Knee Arthroplasty: A Meta-analysis. J. Knee Surg. 2019, 33, 691–703. [Google Scholar] [CrossRef]
- Shihab, Z.; Clayworth, C.; Nara, N. Handheld, accelerometer-based navigation versus conventional instrumentation in total knee arthroplasty: A meta-analysis. ANZ J. Surg. 2020, 90, 2068–2079. [Google Scholar] [CrossRef] [PubMed]
- Minoda, Y.; Hayakawa, K.; Hagio, K.; Konishi, N.; Tamaki, T.; Iwakiri, K.; The KneeAlign 2 Multicenter RCT Group. Usefulness of an Accelerometer-Based Portable Navigation System for Total Knee Arthroplasty. J. Bone Jt. Surg. 2020, 102, 1993–2000. [Google Scholar] [CrossRef]
- Kawaguchi, K.; Michishita, K.; Manabe, T.; Akasaka, Y.; Higuchi, J. Comparison of an Accelerometer-Based Portable Navigation System, Patient-Specific Instrumentation, and Conventional Instrumentation for Femoral Alignment in Total Knee Arthroplasty. Knee Surg. Relat. Res. 2017, 29, 269–275. [Google Scholar] [CrossRef]
- Liow, M.H.L.; Goh, G.S.-H.; Pang, H.-N.; Tay, D.K.J.; Lo, N.N.; Yeo, S.J. Computer-assisted stereotaxic navigation improves the accuracy of mechanical alignment and component positioning in total knee arthroplasty. Arch. Orthop. Trauma Surg. 2016, 136, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- MMoo, I.H.; Chen, J.Y.Q.; Chau, D.H.H.; Tan, S.W.; Lau, A.C.K.; Teo, Y.S. Similar radiological results with accelerometer-based navigation versus conventional technique in total knee arthroplasty. J. Orthop. Surg. 2018, 26, 2309499018772374. [Google Scholar] [CrossRef] [PubMed]
- Nam, D.; Cody, E.A.; Nguyen, J.T.; Figgie, M.P.; Mayman, D.J. Extramedullary Guides Versus Portable, Accelerometer-Based Navigation for Tibial Alignment in Total Knee Arthroplasty: A Randomized, Controlled Trial: Winner of the 2013 HAP PAUL Award. J. Arthroplast. 2014, 29, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Jagadeesh, N.; Kumar, H.; Sarparaju, V.; Shivalingappa, V. Comparative Analysis of Radiological Evaluation and Early Functional Outcomes of Total Knee Arthroplasty Using an Accelerometer-Based Handheld Navigation System and Conventional Instrumentation: A Prospective Study. Cureus 2022, 14, e21039. [Google Scholar] [CrossRef]
- Wood, D.S.; Eckel, T.M.; Kitziger, K.J.; Peters, P.C.; Gladnick, B.P. Accelerometer-based navigation improves early patient-reported outcomes after gap-balanced total knee arthroplasty. J. Orthop. 2020, 23, 37–40. [Google Scholar] [CrossRef]
- Lepri, A.C.; Innocenti, M.; Matassi, F.; Villano, M.; Civinini, R.; Innocenti, M. Accelerometer-Based Navigation in Total Knee Arthroplasty for the Management of Extra-Articular Deformity and Retained Femoral Hardware: Analysis of Component Alignment. Joints 2019, 7, 1–7. [Google Scholar] [CrossRef]
- Matassi, F.; Lepri, A.C.; Innocenti, M.; Zanna, L.; Civinini, R.; Innocenti, M. Total Knee Arthroplasty in Patients with Extra-Articular Deformity: Restoration of Mechanical Alignment Using Accelerometer-Based Navigation System. J. Arthroplast. 2019, 34, 676–681. [Google Scholar] [CrossRef]
- Tsubosaka, M.; Kamenaga, T.; Kuroda, Y.; Takayama, K.; Hashimoto, S.; Ishida, K.; Hayashi, S.; Kuroda, R.; Matsumoto, T. Accelerometer-Based Portable Navigation System Is Useful for Tibial Bone Cutting in Modified Kinematically Aligned Total Knee Arthroplasty. J. Knee Surg. 2019, 34, 870–876. [Google Scholar] [CrossRef]
- Bonanzinga, T.; Giuffrida, A.; Di Matteo, B.; Raspugli, G.F.; Iacono, F.; Marcacci, M. In vitro validation of a novel inertial-based cutting guide for tibial resection in total knee arthroplasty. Knee 2020, 27, 1433–1438. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).