An Overview of the Epidemiology of Multidrug Resistance and Bacterial Resistance Mechanisms: What Solutions Are Available? A Comprehensive Review
Abstract
1. Introduction
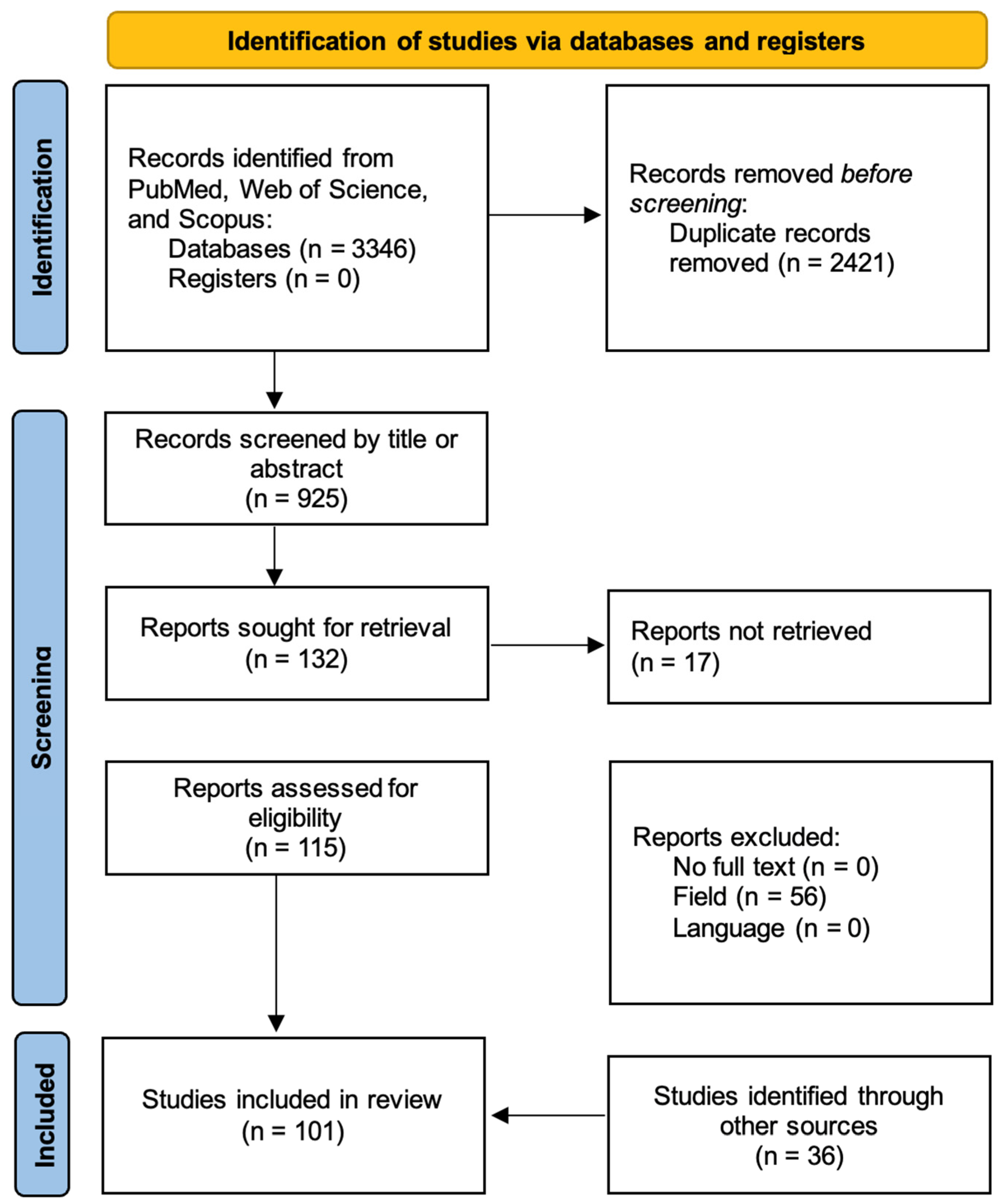
2. Materials and Methods
3. Discussion
3.1. Epidemiology and Mechanisms of Resistance
3.2. Future Possible Therapeutic Options
3.3. Strengths and Methodological Rigor
3.4. Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; Wool, E.E.; Aguilar, G.R.; Mestrovic, T.; Smith, G.; Han, C.; et al. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef]
- Xu, J.; Liu, J.; Li, X.; Zhao, L.; Shen, J.; Xia, X. Burden of bacterial antimicrobial resistance in China: A systematic analysis from 1990 to 2021 and projections to 2050. J. Adv. Res. 2025, in press. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655, Erratum in Lancet 2022, 400, 1102. [Google Scholar] [CrossRef]
- Kariuki, S. Global burden of antimicrobial resistance and forecasts to 2050. Lancet 2024, 404, 1172–1173. [Google Scholar] [CrossRef]
- Chong, C.E.; Pham, T.M.; Carey, M.E.; Wee, B.A.; Taouk, M.L.; Favieres, J.F.; Moore, C.E.; Dyson, Z.A.; Lim, C.; Brown, C.L.; et al. Conference report of the 2024 Antimicrobial Resistance Meeting. NPJ Antimicrob. Resist. 2024, 2, 43. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Das, N.K.; Mukhida, S.; Kannuri, S.; Desai, D.; Dudhat, V.L. Analyzing the WHO’s 2024 Priority Pathogens: Successes and Omissions. J. Mar. Med. Soc. 2025. [Google Scholar] [CrossRef]
- World Health Organization. WHO Bacterial Priority Pathogens List. 2024. Available online: https://iris.who.int/bitstream/handle/10665/376776/9789240093461-eng.pdf (accessed on 1 August 2025).
- World Health Organization. WHO Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 27 February 2017).
- Salam, M.d.A.; Al-Amin, M.d.Y.; Salam, M.T.; Pawar, J.S.; Akhter, N.; Rabaan, A.A.; Alqumber, M.A.A. Antimicrobial Resistance: A Growing Serious Threat for Global Public Health. Healthcare 2023, 11, 1946. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ikuta, K.S.; Swetschinski, L.R.; Robles Aguilar, G.; Sharara, F.; Mestrovic, T.; Gray, A.P.; Weaver, N.D.; Wool, E.E.; Han, C.; Hayoon, A.G.; et al. Global mortality associated with 33 bacterial pathogens in 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022, 400, 2221–2248. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Antimicrobial Resistance Surveillance in Europe 2023–2021 Data. Available online: https://www.ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2023-2021-data (accessed on 1 August 2025).
- Blair, J.M.A.; Webber, M.A.; Baylay, A.J.; Ogbolu, D.O.; Piddock, L.J.V. Molecular mechanisms of antibiotic resistance. Nat. Rev. Microbiol. 2015, 13, 42–51. [Google Scholar] [CrossRef]
- Darby, E.M.; Trampari, E.; Siasat, P.; Gaya, M.S.; Alav, I.; Webber, M.A.; Blair, J.M.A. Molecular mechanisms of antibiotic resistance revisited. Nat. Rev. Microbiol. 2023, 21, 280–295, Erratum in Nat. Rev. Microbiol. 2024, 22, 255. [Google Scholar] [CrossRef]
- Acosta-Gutiérrez, S.; Ferrara, L.; Pathania, M.; Masi, M.; Wang, J.; Bodrenko, I.; Zahn, M.; Winterhalter, M.; Stavenger, R.A.; Pagès, J.-M.; et al. Getting Drugs into Gram-Negative Bacteria: Rational Rules for Permeation through General Porins. ACS Infect. Dis. 2018, 4, 1487–1498. [Google Scholar] [CrossRef]
- Wong, J.L.C.; Romano, M.; Kerry, L.E.; Kwong, H.-S.; Low, W.-W.; Brett, S.J.; Clements, A.; Beis, K.; Frankel, G. OmpK36-mediated Carbapenem resistance attenuates ST258 Klebsiella pneumoniae in vivo. Nat. Commun. 2019, 10, 3957. [Google Scholar] [CrossRef] [PubMed]
- Lou, H.; Chen, M.; Black, S.S.; Bushell, S.R.; Ceccarelli, M.; Mach, T.; Beis, K.; Low, A.S.; Bamford, V.A.; Booth, I.R.; et al. Altered Antibiotic Transport in OmpC Mutants Isolated from a Series of Clinical Strains of Multi-Drug Resistant E. coli. PLoS ONE 2011, 6, e25825. [Google Scholar] [CrossRef]
- Eren, E.; Vijayaraghavan, J.; Liu, J.; Cheneke, B.R.; Touw, D.S.; Lepore, B.W.; Indic, M.; Movileanu, L.; Berg, B.v.D.; Dutzler, R. Substrate Specificity within a Family of Outer Membrane Carboxylate Channels. PLoS Biol. 2012, 10, e1001242. [Google Scholar] [CrossRef]
- Tynjälä, P.; Pennanen, M.; Markkanen, I.; Heikkinen, H.L.T. Finnish model of peer-group mentoring: Review of research. Ann. N. Y. Acad. Sci. 2021, 1483, 208–223. [Google Scholar] [CrossRef]
- Chevalier, S.; Bouffartigues, E.; Bodilis, J.; Maillot, O.; Lesouhaitier, O.; Feuilloley, M.G.J.; Orange, N.; Dufour, A.; Cornelis, P. Structure, function and regulation of Pseudomonas aeruginosa porins. FEMS Microbiol. Rev. 2017, 41, 698–722. [Google Scholar] [CrossRef]
- Ude, J.; Tripathi, V.; Buyck, J.M.; Söderholm, S.; Cunrath, O.; Fanous, J.; Claudi, B.; Egli, A.; Schleberger, C.; Hiller, S.; et al. Outer membrane permeability: Antimicrobials and diverse nutrients bypass porins in Pseudomonas aeruginosa. Proc. Natl. Acad. Sci. USA 2021, 118, e2107644118. [Google Scholar] [CrossRef] [PubMed]
- Du, D.; Wang-Kan, X.; Neuberger, A.; van Veen, H.W.; Pos, K.M.; Piddock, L.J.V.; Luisi, B.F. Multidrug efflux pumps: Structure, function and regulation. Nat. Rev. Microbiol. 2018, 16, 523–539. [Google Scholar] [CrossRef] [PubMed]
- Ebbensgaard, A.E.; Løbner-Olesen, A.; Frimodt-Møller, J. The Role of Efflux Pumps in the Transition from Low-Level to Clinical Antibiotic Resistance. Antibiotics 2020, 9, 855. [Google Scholar] [CrossRef]
- Saw, H.T.H.; Webber, M.A.; Mushtaq, S.; Woodford, N.; Piddock, L.J.V. Inactivation or inhibition of AcrAB-TolC increases resistance of carbapenemase-producing Enterobacteriaceae to carbapenems. J. Antimicrob. Chemother. 2016, 71, 1510–1519. [Google Scholar] [CrossRef]
- Buckner, M.M.C.; Saw, H.T.H.; Osagie, R.N.; McNally, A.; Ricci, V.; Wand, M.E.; Woodford, N.; Ivens, A.; Webber, M.A.; Piddock, L.J.V.; et al. Clinically Relevant Plasmid-Host Interactions Indicate that Transcriptional and Not Genomic Modifications Ameliorate Fitness Costs of Klebsiella pneumoniae Carbapenemase-Carrying Plasmids. mBio 2018, 9, e02303-17. [Google Scholar] [CrossRef]
- Bush, N.G.; Diez-Santos, I.; Abbott, L.R.; Maxwell, A. Quinolones: Mechanism, Lethality and Their Contributions to Antibiotic Resistance. Molecules 2020, 25, 5662. [Google Scholar] [CrossRef] [PubMed]
- Periasamy, H.; Joshi, P.; Palwe, S.; Shrivastava, R.; Bhagwat, S.; Patel, M. High prevalence of Escherichia coli clinical isolates in India harbouring four amino acid inserts in PBP3 adversely impacting activity of aztreonam/avibactam. J. Antimicrob. Chemother. 2020, 75, 1650–1651. [Google Scholar] [CrossRef] [PubMed]
- Bhujbalrao, R.; Anand, R. Deciphering Determinants in Ribosomal Methyltransferases That Confer Antimicrobial Resistance. J. Am. Chem. Soc. 2019, 141, 1425–1429. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Wachino, J.; Arakawa, Y. Aminoglycoside Resistance. Infect. Dis. Clin. N. Am. 2016, 30, 523–537. [Google Scholar] [CrossRef]
- Elias, R.; Duarte, A.; Perdigão, J. A Molecular Perspective on Colistin and Klebsiella pneumoniae: Mode of Action, Resistance Genetics, and Phenotypic Susceptibility. Diagnostics 2021, 11, 1165. [Google Scholar] [CrossRef]
- Sabnis, A.; Hagart, K.L.; Klöckner, A.; Becce, M.; Evans, L.E.; Furniss, R.C.D.; Mavridou, D.A.; Murphy, R.; Stevens, M.M.; Davies, J.C.; et al. Colistin kills bacteria by targeting lipopolysaccharide in the cytoplasmic membrane. eLife 2021, 10, e65836. [Google Scholar] [CrossRef]
- Hamel, M.; Rolain, J.-M.; Baron, S.A. The History of Colistin Resistance Mechanisms in Bacteria: Progress and Challenges. Microorganisms 2021, 9, 442. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J. Transferable Mechanisms of Quinolone Resistance from 1998 Onward. Clin. Microbiol. Rev. 2019, 32, e00007-19. [Google Scholar] [CrossRef]
- Mohamad, M.; Nicholson, D.; Saha, C.K.; Hauryliuk, V.; Edwards, T.A.; Atkinson, G.C.; Ranson, N.A.; O’nEill, A.J. Sal-type ABC-F proteins: Intrinsic and common mediators of pleuromutilin resistance by target protection in staphylococci. Nucleic Acids Res. 2022, 50, 2128–2142. [Google Scholar] [CrossRef] [PubMed]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.A.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef]
- Naas, T.; Oueslati, S.; Bonnin, R.A.; Dabos, M.L.; Zavala, A.; Dortet, L.; Retailleau, P.; Iorga, B.I. Beta-lactamase database (BLDB)—Structure and function. J. Enzym. Inhib. Med. Chem. 2017, 32, 917–919. [Google Scholar] [CrossRef]
- Ambler, R.P. The structure of β-lactamases. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1980, 289, 321–331. [Google Scholar] [CrossRef]
- Nepal, K.; Pant, N.D.; Neupane, B.; Belbase, A.; Baidhya, R.; Shrestha, R.K.; Lekhak, B.; Bhatta, D.R.; Jha, B. Extended spectrum beta-lactamase and metallo beta-lactamase production among Escherichia coli and Klebsiella pneumoniae isolated from different clinical samples in a tertiary care hospital in Kathmandu, Nepal. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 62. [Google Scholar] [CrossRef]
- Queenan, A.M.; Bush, K. Carbapenemases: The Versatile β-Lactamases. Clin. Microbiol. Rev. 2007, 20, 440–458. [Google Scholar] [CrossRef]
- Johnson, A.P.; Woodford, N. Global spread of antibiotic resistance: The example of New Delhi metallo-β-lactamase (NDM)-mediated carbapenem resistance. J. Med. Microbiol. 2013, 62, 499–513. [Google Scholar] [CrossRef]
- Sun, J.; Chen, C.; Cui, C.-Y.; Zhang, Y.; Liu, X.; Cui, Z.-H.; Ma, X.-Y.; Feng, Y.; Fang, L.-X.; Lian, X.-L.; et al. Plasmid-encoded tet(X) genes that confer high-level tigecycline resistance in Escherichia coli. Nat. Microbiol. 2019, 4, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, D.; Lv, Y.; Cui, L.; Li, Y.; Li, T.; Song, H.; Hao, Y.; Shen, J.; Wang, Y.; et al. Novel Plasmid-Mediated tet (X5) Gene Conferring Resistance to Tigecycline, Eravacycline, and Omadacycline in a Clinical Acinetobacter baumannii Isolate. Antimicrob. Agents Chemother. 2019, 64, e01326-19. [Google Scholar] [CrossRef]
- He, T.; Wang, R.; Liu, D.; Walsh, T.R.; Zhang, R.; Lv, Y.; Ke, Y.; Ji, Q.; Wei, R.; Liu, Z.; et al. Emergence of plasmid-mediated high-level tigecycline resistance genes in animals and humans. Nat. Microbiol. 2019, 4, 1450–1456. [Google Scholar] [CrossRef]
- Bordeleau, E.; Stogios, P.J.; Evdokimova, E.; Koteva, K.; Savchenko, A.; Wright, G.D. ApmA Is a Unique Aminoglycoside Antibiotic Acetyltransferase That Inactivates Apramycin. mBio 2021, 12, e02705-20. [Google Scholar] [CrossRef]
- Rominski, A.; Roditscheff, A.; Selchow, P.; Böttger, E.C.; Sander, P. Intrinsic rifamycin resistance of Mycobacterium abscessus is mediated by ADP-ribosyltransferase MAB_0591. J. Antimicrob. Chemother. 2017, 72, 376–384. [Google Scholar] [CrossRef]
- Surette, M.D.; Spanogiannopoulos, P.; Wright, G.D. The Enzymes of the Rifamycin Antibiotic Resistome. Acc. Chem. Res. 2021, 54, 2065–2075. [Google Scholar] [CrossRef]
- Spanogiannopoulos, P.; Waglechner, N.; Koteva, K.; Wright, G.D. A rifamycin inactivating phosphotransferase family shared by environmental and pathogenic bacteria. Proc. Natl. Acad. Sci. USA 2014, 111, 7102–7107. [Google Scholar] [CrossRef] [PubMed]
- Koteva, K.; Cox, G.; Kelso, J.K.; Surette, M.D.; Zubyk, H.L.; Ejim, L.; Stogios, P.; Savchenko, A.; Sørensen, D.; Wright, G.D. Rox, a Rifamycin Resistance Enzyme with an Unprecedented Mechanism of Action. Cell Chem. Biol. 2018, 25, 403–412.e5. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, P.D.; Taylor, P.W. Methicillin Resistance in Staphylococcus Aureus: Mechanisms and Modulation. Sci. Prog. 2002, 85, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Hugonnet, J.-E.; Mengin-Lecreulx, D.; Monton, A.; den Blaauwen, T.; Carbonnelle, E.; Veckerlé, C.; Yves, V.B.; Van Nieuwenhze, M.; Bouchier, C.; Tu, K.; et al. Factors essential for L,D-transpeptidase-mediated peptidoglycan cross-linking and β-lactam resistance in Escherichia coli. eLife 2016, 5, e19469. [Google Scholar] [CrossRef]
- Arthur, M.; Reynolds, P.; Courvalin, P. Glycopeptide resistance in enterococci. Trends Microbiol. 1996, 4, 401–407. [Google Scholar] [CrossRef]
- Miller, W.R.; Munita, J.M.; Arias, C.A. Mechanisms of antibiotic resistance in enterococci. Expert Rev. Anti-Infect. Ther. 2014, 12, 1221–1236. [Google Scholar] [CrossRef]
- Gardete, S.; Tomasz, A. Mechanisms of vancomycin resistance in Staphylococcus aureus. J. Clin. Investig. 2014, 124, 2836–2840. [Google Scholar] [CrossRef]
- Sievert, D.M.; Rudrik, J.T.; Patel, J.B.; McDonald, L.C.; Wilkins, M.J.; Hageman, J.C. Vancomycin-Resistant Staphylococcus aureus in the United States, 2002–2006. Clin. Infect. Dis. 2008, 46, 668–674. [Google Scholar] [CrossRef]
- Lin, L.; Nonejuie, P.; Munguia, J.; Hollands, A.; Olson, J.; Dam, Q.; Kumaraswamy, M.; Rivera, H.; Corriden, R.; Rohde, M.; et al. Azithromycin Synergizes with Cationic Antimicrobial Peptides to Exert Bactericidal and Therapeutic Activity Against Highly Multidrug-Resistant Gram-Negative Bacterial Pathogens. eBioMedicine 2015, 2, 690–698. [Google Scholar] [CrossRef] [PubMed]
- Birlutiu, R.M.; Birlutiu, V.; Mihalache, M.; Mihalache, C.; Cismasiu, R.S. Diagnosis and management of orthopedic implant-associated infection: A comprehensive review of the literature. Biomed. Res. 2017, 28, 5063–5073. [Google Scholar]
- Birlutiu, V.; Birlutiu, R.M. Endocarditis due to Abiotrophia defectiva, a biofilm-related infection associated with the presence of fixed braces. Medicine 2017, 96, e8756. [Google Scholar] [CrossRef]
- Birlutiu, R.M.; Birlutiu, V.; Cismasiu, R.S.; Mihalache, M. bbFISH-ing in the sonication fluid. Medicine 2019, 98, e16501. [Google Scholar] [CrossRef]
- Birlutiu, R.-M.; Birlutiu, V.; Cismasiu, R.-S.; Mihalache, P.; Mihalache, M. BACTERIAL BIOFILM: A MINI-REVIEW OF AN EMERGING LIFE FORM OF BACTERIA. Acta Med. Transilv. 2017, 22, 68–71. [Google Scholar]
- Kohanski, M.A.; Dwyer, D.J.; Hayete, B.; Lawrence, C.A.; Collins, J.J. A Common Mechanism of Cellular Death Induced by Bactericidal Antibiotics. Cell 2007, 130, 797–810. [Google Scholar] [CrossRef]
- Claessen, D.; Errington, J. Cell Wall Deficiency as a Coping Strategy for Stress. Trends Microbiol. 2019, 27, 1025–1033. [Google Scholar] [CrossRef]
- Manuse, S.; Shan, Y.; Canas-Duarte, S.J.; Bakshi, S.; Sun, W.-S.; Mori, H.; Paulsson, J.; Lewis, K.; Bollenbach, T. Bacterial persisters are a stochastically formed subpopulation of low-energy cells. PLoS Biol. 2021, 19, e3001194. [Google Scholar] [CrossRef]
- Shan, Y.; Brown Gandt, A.; Rowe, S.E.; Deisinger, J.P.; Conlon, B.P.; Lewis, K. ATP-Dependent Persister Formation in Escherichia coli. mBio 2017, 8, e02267-16. [Google Scholar] [CrossRef]
- Zimmerli, W.; Moser, C. Pathogenesis and treatment concepts of orthopaedic biofilm infections. FEMS Immunol. Med. Microbiol. 2012, 65, 158–168. [Google Scholar] [CrossRef]
- Cao, B.; Christophersen, L.; Thomsen, K.; Sønderholm, M.; Bjarnsholt, T.; Jensen, P.Ø.; Høiby, N.; Moser, C. Antibiotic penetration and bacterial killing in a Pseudomonas aeruginosa biofilm model. J. Antimicrob. Chemother. 2015, 70, 2057–2063. [Google Scholar] [CrossRef] [PubMed]
- Lenhard, J.R.; Bulman, Z.P. Inoculum effect of β-lactam antibiotics. J. Antimicrob. Chemother. 2019, 74, 2825–2843. [Google Scholar] [CrossRef] [PubMed]
- Tängdén, T.; Carrara, E.; Hellou, M.M.; Yahav, D.; Paul, M. Introducing new antibiotics for multidrug-resistant bacteria: Obstacles and the way forward. Clin. Microbiol. Infect. 2025, 31, 354–359. [Google Scholar] [CrossRef]
- Global Antibiotic Research & Development Partnership (GARDP). Cefiderocol Manufacturing Sublicense and Technology Transfer Agreement. Available online: https://www.gardp.org/ (accessed on 15 September 2025).
- McKinnell, J.A.; Dwyer, J.P.; Talbot, G.H.; Connolly, L.E.; Friedland, I.; Smith, A.; Jubb, A.M.; Serio, A.W.; Krause, K.M.; Daikos, G.L. Plazomicin for Infections Caused by Carbapenem-Resistant Enterobacteriaceae. N. Engl. J. Med. 2019, 380, 791–793. [Google Scholar] [CrossRef]
- Kaye, K.S.; Bhowmick, T.; Metallidis, S.; Bleasdale, S.C.; Sagan, O.S.; Stus, V.; Vazquez, J.; Zaitsev, V.; Bidair, M.; Chorvat, E.; et al. Effect of Meropenem-Vaborbactam vs Piperacillin-Tazobactam on Clinical Cure or Improvement and Microbial Eradication in Complicated Urinary Tract Infection. JAMA 2018, 319, 788–799. [Google Scholar] [CrossRef]
- Lv, X.; Alder, J.; Li, L.; O’rIordan, W.; Rybak, M.J.; Ye, H.; Zhang, R.; Zhang, Z.; Zhu, X.; Wilcox, M.H. Efficacy and Safety of Tedizolid Phosphate versus Linezolid in a Randomized Phase 3 Trial in Patients with Acute Bacterial Skin and Skin Structure Infection. Antimicrob. Agents Chemother. 2019, 63, e02252-18. [Google Scholar] [CrossRef]
- Moran, G.J.; Fang, E.; Corey, G.R.; Das, A.F.; De Anda, C.; Prokocimer, P. Tedizolid for 6 days versus linezolid for 10 days for acute bacterial skin and skin-structure infections (ESTABLISH-2): A randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect. Dis. 2014, 14, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Prokocimer, P.; De Anda, C.; Fang, E.; Mehra, P.; Das, A. Tedizolid Phosphate vs Linezolid for Treatment of Acute Bacterial Skin and Skin Structure Infections. JAMA 2013, 309, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Mikamo, H.; Takesue, Y.; Iwamoto, Y.; Tanigawa, T.; Kato, M.; Tanimura, Y.; Kohno, S. Efficacy, safety and pharmacokinetics of tedizolid versus linezolid in patients with skin and soft tissue infections in Japan—Results of a randomised, multicentre phase 3 study. J. Infect. Chemother. 2018, 24, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Balkhair, A.; Al-Muharrmi, Z.; Al’Adawi, B.; Al Busaidi, I.; Taher, H.B.; Al-Siyabi, T.; Al Amin, M.; Hassan, K. Prevalence and 30-day all-cause mortality of carbapenem-and colistin-resistant bacteraemia caused by Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae: Description of a decade-long trend. Int. J. Infect. Dis. 2019, 85, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Suh, J.W.; Park, S.M.; Ju, Y.K.; Yang, K.S.; Kim, J.Y.; Kim, S.B.; Sohn, J.W.; Yoon, Y.K. Clinical and molecular predictors of mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: A retrospective cohort study. J. Microbiol. Immunol. Infect. 2024, 57, 148–155. [Google Scholar] [CrossRef]
- Kim, M.H.; Jeong, H.; Sim, Y.M.; Lee, S.; Yong, D.; Ryu, C.-M.; Choi, J.Y.; Ruan, Z. Using comparative genomics to understand molecular features of carbapenem-resistant Acinetobacter baumannii from South Korea causing invasive infections and their clinical implications. PLoS ONE 2020, 15, e0229416. [Google Scholar] [CrossRef]
- Du, X.; Xu, X.; Yao, J.; Deng, K.; Chen, S.; Shen, Z.; Yang, L.; Feng, G. Predictors of mortality in patients infected with carbapenem-resistant Acinetobacter baumannii: A systematic review and meta-analysis. Am. J. Infect. Control 2019, 47, 1140–1145. [Google Scholar] [CrossRef]
- Ruiz, J.; Favieres, C.; Broch, M.J.; Villarreal, E.; Gordon, M.; Quinzá, A.; Ortega, Á.C.; Ramirez, P. Individualised antimicrobial dosing in critically ill patients undergoing continuous renal replacement therapy: Focus on total drug clearance. Eur. J. Hosp. Pharm. 2018, 25, 123–126. [Google Scholar] [CrossRef]
- Marchaim, D.; Perez, F.; Lee, J.; Bheemreddy, S.; Hujer, A.M.; Rudin, S.; Hayakawa, K.; Lephart, P.R.; Blunden, C.; Shango, M.; et al. “Swimming in resistance”: Co-colonization with carbapenem-resistant Enterobacteriaceae and Acinetobacter baumannii or Pseudomonas aeruginosa. Am. J. Infect. Control 2012, 40, 830–835. [Google Scholar] [CrossRef]
- Amat, T.; Gutiérrez-Pizarraya, A.; Machuca, I.; Gracia-Ahufinger, I.; Pérez-Nadales, E.; Torre-Giménez, Á.; Garnacho-Montero, J.; Cisneros, J.; Torre-Cisneros, J. The combined use of tigecycline with high-dose colistin might not be associated with higher survival in critically ill patients with bacteraemia due to carbapenem-resistant Acinetobacter baumannii. Clin. Microbiol. Infect. 2018, 24, 630–634. [Google Scholar] [CrossRef]
- ECDC. New Genomic Surveillance Studies Reveal Circulation of Multidrug-Resistant Pathogens. Available online: https://www.ecdc.europa.eu/en/news-events/new-genomic-surveillance-studies-reveal-circulation-multidrug-resistant (accessed on 11 September 2025).
- Karanika, S.; Karantanos, T.; Arvanitis, M.; Grigoras, C.; Mylonakis, E. Fecal Colonization With Extended-spectrum Beta-lactamase–Producing Enterobacteriaceae and Risk Factors Among Healthy Individuals: A Systematic Review and Metaanalysis. Clin. Infect. Dis. 2016, 63, 310–318, Erratum in Clin. Infect. Dis. 2016, 63. 851. [Google Scholar] [CrossRef][Green Version]
- Kelly, A.M.; Mathema, B.; Larson, E.L. Carbapenem-resistant Enterobacteriaceae in the community: A scoping review. Int. J. Antimicrob. Agents 2017, 50, 127–134. [Google Scholar] [CrossRef]
- Walsh, T.R.; Weeks, J.; Livermore, D.M.; Toleman, M.A. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: An environmental point prevalence study. Lancet Infect. Dis. 2011, 11, 355–362. [Google Scholar] [CrossRef]
- Islam, M.A.; Islam, M.; Hasan, R.; Hossain, M.I.; Nabi, A.; Rahman, M.; Goessens, W.H.F.; Endtz, H.P.; Boehm, A.B.; Faruque, S.M. Environmental Spread of New Delhi Metallo-β-Lactamase-1-Producing Multidrug-Resistant Bacteria in Dhaka, Bangladesh. Appl. Environ. Microbiol. 2017, 83, e00793-17. [Google Scholar] [CrossRef]
- Ruppé, E.; Andremont, A.; Armand-Lefèvre, L. Digestive tract colonization by multidrug-resistant Enterobacteriaceae in travellers: An update. Travel Med. Infect. Dis. 2018, 21, 28–35. [Google Scholar] [CrossRef]
- Woerther, P.-L.; Andremont, A.; Kantele, A. Travel-acquired ESBL-producing Enterobacteriaceae: Impact of colonization at individual and community level. J. Travel Med. 2017, 24, S29–S34. [Google Scholar] [CrossRef]
- Voor in‘t holt, A.F.; Mourik, K.; Beishuizen, B.; van der Schoor, A.S.; Verbon, A.; Vos, M.C.; Severin, J.A. Acquisition of multidrug-resistant Enterobacterales during international travel: A systematic review of clinical and microbiological characteristics and meta-analyses of risk factors. Antimicrob. Resist. Infect. Control. 2020, 9, 71. [Google Scholar] [CrossRef]
- Jangra, M.; Travin, D.Y.; Aleksandrova, E.V.; Kaur, M.; Darwish, L.; Koteva, K.; Klepacki, D.; Wang, W.; Tiffany, M.; Sokaribo, A.; et al. A broad-spectrum lasso peptide antibiotic targeting the bacterial ribosome. Nature 2025, 640, 1022–1030. [Google Scholar] [CrossRef] [PubMed]
- German Center for Infection Research. World AMR Awareness Week 2024 (18–24 November): Educate. Advocate. Act Now. 2024. Available online: https://www.dzif.de/en/world-amr-awareness-week-2024-18-24-november-educate-advocate-act-now (accessed on 10 September 2025).
- Zampaloni, C.; Mattei, P.; Bleicher, K.; Winther, L.; Thäte, C.; Bucher, C.; Adam, J.-M.; Alanine, A.; Amrein, K.E.; Baidin, V.; et al. A novel antibiotic class targeting the lipopolysaccharide transporter. Nature 2024, 625, 566–571, Erratum in Nature 2024, 631, E17. [Google Scholar] [CrossRef]
- Weng, Q.; Zhang, F.; Zheng, Q. Zosurabalpin: A novel tethered macrocyclic peptide antibiotic that kills carbapenem-resistant Acinetobacter baumannii. MedComm 2024, 5, e696. [Google Scholar] [CrossRef] [PubMed]
- GARDP Backs Debiopharm’s Swiss-Developed Compound to Treat Drug-Resistant Gonorrhoea Infections. 14 January 2025. Available online: https://gardp.org/gardp-backs-debiopharms-swiss-developed-compound-to-treat-drug-resistant-gonorrhoea-infections/ (accessed on 17 August 2025).
- Birlutiu, R.-M.; Birlutiu, V. Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review. Pharmaceuticals 2025, 18, 1217. [Google Scholar] [CrossRef] [PubMed]
- Carcione, D.; Intra, J.; Andriani, L.; Campanile, F.; Gona, F.; Carletti, S.; Mancini, N.; Brigante, G.; Cattaneo, D.; Baldelli, S.; et al. New Antimicrobials for Gram-Positive Sustained Infections: A Comprehensive Guide for Clinicians. Pharmaceuticals 2023, 16, 1304. [Google Scholar] [CrossRef] [PubMed]
- Tsilika, M.; Ntziora, F.; Giannitsioti, E. Antimicrobial Treatment Options for Multidrug Resistant Gram-Negative Pathogens in Bone and Joint Infections. Pathogens 2025, 14, 130. [Google Scholar] [CrossRef] [PubMed]
| Antibiotic/Antibiotic Class | Mechanism of Action | Spectrum of Activity | Observation/Limitations |
|---|---|---|---|
| Tigecycline | Inhibits protein synthesis by binding to the bacterial 30S ribosomal subunit | ESBL, CRE (all classes including MBL), DTR A. baumannii | No activity against P. aeruginosa |
| Colistin | Disrupts bacterial cell membrane integrity by binding to LPS and phospholipids in the outer membrane of GNB bacteria | ESBL, CRE (all classes including MBL), DTR P. aeruginosa, DTR A. baumannii | Should be used in combination with one or more additional agents that highlights a susceptible MIC |
| Fosfomycin | Inhibits bacterial cell wall synthesis by targeting MurA enzyme | ESBL, CRE (all classes including MBL), DTR P. aeruginosa | Its use as monotherapy is not recommended |
| Cefiderocol | Siderophore cephalosporin: actively transported into the bacteria via iron transport systems | ESBL, KPC, MBL, AmpC β-lactamases, OXA-48 carbapenemase, DTR P. aeruginosa, DTR A. baumannii | |
| Ceftazidime– avibactam | Inhibits bacterial cell wall synthesis; avibactam inhibits β-lactamases, including KPC and OXA-48 carbapenemase | ESBL, KPC, AmpC β-lactamases, OXA-48 carbapenemase, DTR P. aeruginosa | No activity against MBL Important resistance rates in A. baumannii isolates |
| Ceftolozane– tazobactam | Inhibits bacterial cell wall synthesis; tazobactam inhibits β-lactamases | ESBL, DTR P. aeruginosa | No activity against carbapenemases-producing strains, DTR A. baumannii, AmpC β-lactamases |
| Imipenem– cilastatin– relebactam | Inhibits bacterial cell wall synthesis; relebactam inhibits KPC | ESBL, KPC, Relebactam may slighty enhance the activity of imipenem against OXA-carbapenemases, DTR P. aeruginosa | No activity against MBL producing strains |
| Carbapenems (e.g., meropenem, imipenem–cilastatin, ertapenem) | Inhibit bacterial cell wall synthesis by binding to PBPs | ESBL | No activity against carbapenemases, DTR A. baumannii or P. aeruginosa Ertapenem is inactive against P. aeruginosa |
| Meropenem– vaborbactam | Inhibits bacterial cell wall synthesis; vaborbactam inhibits KPC-producing β-lactamases | KPC, and ESBL | No activity against MBL- or OXA-type carbapenemases, DTR P. aeruginosa or A. baumannii |
| Ceftaroline | Binds with high affinity to penicillin-binding proteins (especially PBP2a in MRSA and PBPs 1–3), inhibiting peptidoglycan cross-linking and leading to cell wall weakening and lysis | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Viridans group streptococci | Partial antimicrobial activity against Vancomycin-resistant Enterococcus |
| Ceftobiprole | Forms stable complexes with PBPs, including PBP2a (MRSA) and PBP2x (penicillin-resistant S. pneumoniae), blocking peptidoglycan cross-linking and causing bacterial cell apoptosis | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Viridans group streptococci | No antimicrobial activity against Vancomycin-resistant Enterococcus |
| Oritavancin | Binds to D-Ala-D-Ala termini of peptidoglycan precursors, inhibiting transglycosylation and transpeptidation. It also disrupts membrane integrity and inhibits RNA synthesis | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Vancomycin-resistant Enterococcus, Viridans group streptococci | |
| Dalbavancin | Binds tightly to the D-Ala-D-Ala residues of peptidoglycan chains, preventing cell wall elongation and cross-linking | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Viridans group streptococci | No antimicrobial activity against Vancomycin-resistant Enterococcus |
| Omadacycline | Inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit, blocking tRNA binding and peptide elongation | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Vancomycin-resistant Enterococcus, Viridans group streptococci | |
| Tedizolid | Binds to the 23S rRNA of the 50S ribosomal subunit, preventing the formation of the 70S initiation complex and thereby inhibiting protein synthesis | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Vancomycin-resistant Enterococcus, Viridans group streptococci | |
| Delafloxacin | Inhibits bacterial DNA gyrase and topoisomerase IV, enzymes essential for DNA replication, transcription, and repair | Beta-hemolytic streptococci, Methicillin-resistant Staphylococcus aureus, Methicillin-resistant Staphylococcus epidermidis, Streptococcus pneumoniae, Viridans group streptococci | No antimicrobial activity against Vancomycin-resistant Enterococcus |
| Novel therapeutic agents | |||
| Darobactin | Binds to BamA | Gram-negative pathogens | Still in preclinical and early clinical development |
| Metazzobactam | Inhibits PBPs involved in bacterial cell wall synthesis | Gram-negative pathogens | Limited or no activity against carbapenemase-producing strains. Clinical development |
| Zosurabalpin | Blocks the lipopolysaccharide (LPS) transporter (LptB2FGC complex) | Carbapenem-resistant Acinetobacter baumannii | Active in preclinical and early clinical studies |
| Cefepime/Enmetazobactam |
Cefepime: inhibits PBPs, disrupting peptidoglycan synthesis.
Enmetazobactam: inhibits class A β-lactamases (including ESBLs) | Active against Enterobacterales (including ESBL-producers), some activity against Pseudomonas aeruginosa | not effective against carbapenemase producers. Approved in Europe (2024) for complicated urinary tract infections (cUTIs); phase III showed non-inferiority/superiority vs. piperacillin-tazobactam. Limited coverage against carbapenem-resistant strains |
| Cresomycin | Binds to the 50S ribosomal subunit, inhibiting protein elongation | Against macrolide-resistant Gram-positive bacteria | Still under investigation; clinical development status is early, with no large-scale trials completed yet |
| Lariocidin | Binds to the 16S rRNA of the small ribosomal subunit, interfering with aminoacyl-tRNA accommodation and protein synthesis | Gram-positive bacteria (e.g., Bacillus subtilis) and selected Gram-negative species (e.g., Escherichia coli, Acinetobacter baumannii, Mycobacterium smegmatis) | Preclinical stage |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birlutiu, V.; Birlutiu, R.-M. An Overview of the Epidemiology of Multidrug Resistance and Bacterial Resistance Mechanisms: What Solutions Are Available? A Comprehensive Review. Microorganisms 2025, 13, 2194. https://doi.org/10.3390/microorganisms13092194
Birlutiu V, Birlutiu R-M. An Overview of the Epidemiology of Multidrug Resistance and Bacterial Resistance Mechanisms: What Solutions Are Available? A Comprehensive Review. Microorganisms. 2025; 13(9):2194. https://doi.org/10.3390/microorganisms13092194
Chicago/Turabian StyleBirlutiu, Victoria, and Rares-Mircea Birlutiu. 2025. "An Overview of the Epidemiology of Multidrug Resistance and Bacterial Resistance Mechanisms: What Solutions Are Available? A Comprehensive Review" Microorganisms 13, no. 9: 2194. https://doi.org/10.3390/microorganisms13092194
APA StyleBirlutiu, V., & Birlutiu, R.-M. (2025). An Overview of the Epidemiology of Multidrug Resistance and Bacterial Resistance Mechanisms: What Solutions Are Available? A Comprehensive Review. Microorganisms, 13(9), 2194. https://doi.org/10.3390/microorganisms13092194







