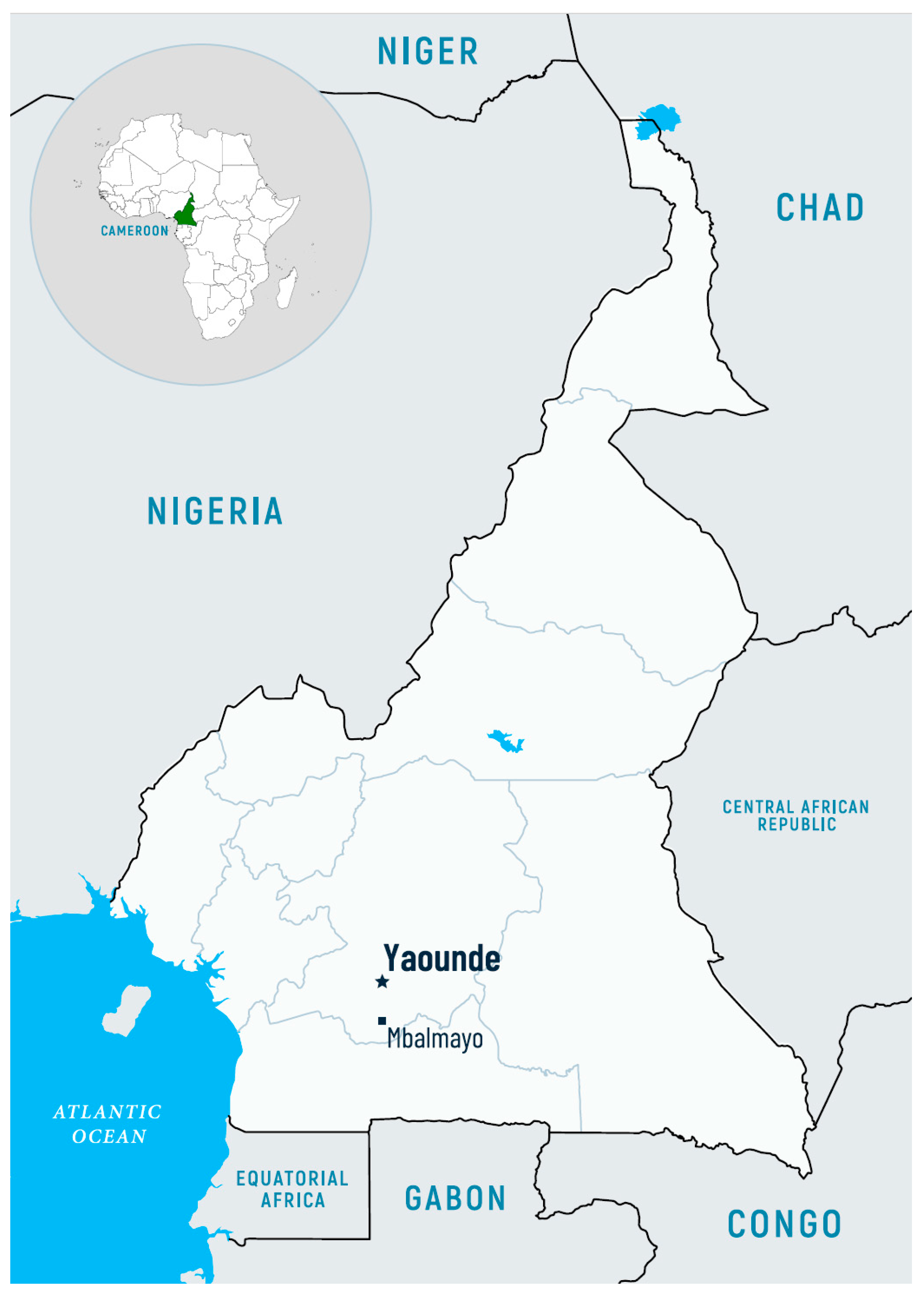
Plasmodium spp. Infections Among Mbalmayo Inhabitants of Central Region in Cameroon: Discrepancies Between Rapid Diagnostic Tests and Molecular Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Sample Collection
2.2.1. Malaria Rapid Diagnostic Tests (mRDTs)
2.2.2. Molecular Diagnostics (RT-PCR)
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
4. Discussion
5. Limitations of This Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mbenda, H.G.; Awasthi, G.; Singh, P.K.; Gouado, I.; Das, A. Does malaria epidemiology project Cameroon as “Africa in Miniature”? J. Biosci. 2014, 39, 727–738. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Cameroon. Available online: https://data.worldbank.org/country/cameroon (accessed on 18 February 2025).
- World Health Organization. World Malaria Report 2024. Geneva: World Health Organization; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2024 (accessed on 18 February 2025).
- Jerving, S. Malaria: World Is ‘Badly off Track’ in Reaching Malaria Goals. DEVEX’s Daily Development Newsletter. 2021. Available online: www.devex.com (accessed on 11 February 2023).
- Minsanté-PNLP. Plan Stratégique National de lutte contre le paludisme au Cameroun; Ministère de la Santé Publique du Cameroun: Yaoundé, Cameroon, 2019. [Google Scholar]
- Jato, D.M.; Dina, B.; Nuotol, R.K.; Alebshehy, R.; Shuaib, N.M. Enhancing malaria prevention in Cameroon through community participation: An in-depth review. Cent. Afr. J. Public Health 2017, 3, 97–109. [Google Scholar]
- Massoda Tonye, S.G.; Kouambeng, C.; Wounang, R.; Vounatsou, P. Challenges of DHS and MIS to capture the entire pattern of malaria parasite risk and intervention effects in countries with different ecological zones: The case of Cameroon. Malar. J. 2018, 17, 156. [Google Scholar] [CrossRef]
- MINSANTE/NMCP. National Malaria Control Programme Annual Report; Ministry of Public Health, Republic of Cameroon: Yaoundé, Cameroon, 2015. [Google Scholar]
- United States Agency for International Development. U.S. President’s Malaria Initiative: Cameroon—Malaria Operational Plan FY 2029. Cameroon. 31 December 2019. Available online: https://reliefweb.int/report/cameroon/presidents-malaria-initiative-cameroon-malaria-operational-plan-fy-2019 (accessed on 18 February 2025).
- Antonio-Nkondjio, C.; Kerah, C.; Simard, F.; Awono-Ambene, H.; Mouhamadou, C.; Tchuinkam, T. Complexity of malaria vectorial system in Cameroon: Contribution of secondary vectors to malaria transmission. J. Med. Entomol. 2006, 43, 1215–1221. [Google Scholar] [CrossRef]
- Antonio-Nkondjio, C.; Ndo, C.; Njiokou, F.; Bigoga, J.D.; Awono-Ambene, P.; Etang, J.; Ekobo, A.S.; Wondji, C.S. Review of malaria situation in Cameroon: Technical viewpoint on challenges and prospects for disease elimination. Parasites Vectors 2019, 12, 501. [Google Scholar] [CrossRef]
- National Institute of Statistics (NIS); National Malaria Control Program (NMCP); ICF. Cameroon Malaria Indicator Survey 2022; NIS, NMCP, and ICF: Yaoundé, Cameroon; Rockville, MD, USA; Lexington, KY, USA, 2023. [Google Scholar]
- World Health Organization. World Malaria Report 2019. WHO World Malaria Statistics; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Nyasa, R.B.; Fotabe, E.L.; Ndip, R.N. Trends in malaria prevalence and risk factors associated with the disease in Nkongho-Mbeng; a typical rural setting in the equatorial rainforest of the South West Region of Cameroon. PLoS ONE 2021, 16, e0251380. [Google Scholar] [CrossRef] [PubMed]
- Tebit, E.K.; Tayong, D.B.K.; Longdoh, A.N.; Andreas, L.; Kukwah, A.T.; Theresa, N.A. Identification of the Plasmodium species in clinical samples from children residing in five epidemiological strata of malaria in Cameroon. Trop. Med. Health 2017, 45, 14. [Google Scholar] [CrossRef]
- Ngum, N.H.; Fakeh, N.B.; Lem, A.E.; Mahamat, O. Prevalence of malaria and associated clinical manifestations and myeloperoxidase amongst populations living in different altitudes of Mezam division, North West Region, Cameroon. Malar. J. 2023, 22, 20. [Google Scholar] [CrossRef]
- Nguiffo-Nguete, D.; Nongley Nkemngo, F.; Ndo, C.; Agbor, J.-P.; Boussougou-Sambe, S.T.; Djogbénou, L.S.; Ntoumi, F.; Adegnika, A.A.; Borrmann, S.; Wondji, C.S. Plasmodium malariae contributes to high levels of malaria transmission in a forest–savannah transition area in Cameroon. Parasites Vectors 2023, 16, 31. [Google Scholar] [CrossRef]
- Nyasa, R.B.; Zofou, D.; Kimbi, H.K.; Kum, K.M.; Ngu, R.C.; Titanji, V.P.K. The current status of malaria epidemiology in Bolifamba, atypical Cameroonian rainforest zone: An assessment of intervention strategies and seasonal variations. BMC Public Health 2015, 15, 1105. [Google Scholar] [CrossRef]
- Teh, R.N.; Sumbele, I.U.N.; Nkeudem, G.A.; Meduke, D.N.; Ojong, S.T.; Kimbi, H.K. Concurrence of Care Start Malaria HRP2 RDT with microscopy in population screening for Plasmodium falciparum infection in the Mount Cameroon area: Predictors for RDT positivity. Trop. Med. Hyg. 2019, 47, 17. [Google Scholar] [CrossRef]
- Sumbele, I.U.; Nkemnji, G.B.; Kimbi, H.K. Soil-transmitted helminths and Plasmodium falciparum malaria among individuals living in different agro-ecosystems in two rural communities in the Mount Cameroon area: A cross-sectional study. Infect. Dis. Poverty 2017, 6, 67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kimbi, H.K.; Nana, Y.; Sumbele, I.N.; Anchang-Kimbi, J.K.; Lum, E.; Tonga, C.; Nweboh, M.; Lehman, L.G. Environmental factors and preventive methods against malaria parasite prevalence in rural Bomaka and urban Molyko, Southwest Cameroon. J. Bacteriol. Parasitol. 2013, 4, 1. [Google Scholar] [CrossRef]
- Tangi, L.N.; Ajonina, M.U.; Moyeh, M.N.; Chi, H.F.; Ntui, V.N.; Kwi, P.N.; Toussi, E.C.T.; Fung, M.P.S.; Fah, F.; Mayaba, J.M.; et al. Knowledge, attitude, and adherence to malaria control guidelines and the prevalence of Plasmodium species infection in localities across transmission and ecological zones in Cameroon. Front. Public Health 2023, 11, 1060479. [Google Scholar] [CrossRef] [PubMed]
- Nkemngo, F.N.; Raissa, L.; Nebangwa, D.N.; Nkeng, A.M.; Kengne, A.; Mugenzi, L.M.J.; Fotso-Toguem, Y.G.; Wondji, M.J.; Shey, R.A.; Nguiffo-Nguete, D.; et al. Epidemiology of malaria, schistosomiasis, and geohelminthiasis amongst children aged 3–15 years during the dry season in Northern Cameroon. PLoS ONE 2023, 18, e0288560. [Google Scholar] [CrossRef]
- Roman, D.N.R.; Rosalie, N.N.A.; Kumar, A.; Luther, K.M.M.; Singh, V.; Albert, M.S. Asymptomatic Plasmodium malariae infections in children from suburban areas of Yaoundé, Cameroon. Parasitol. Int. 2018, 67, 29–33. [Google Scholar] [CrossRef]
- Djoufounna, J.; Mayi, M.P.A.; Bamou, R.; Foyet, J.V.; Tabue, R.; Lontsi-Demano, M.; Achu-Fosah, D.; Antonio-Nkondjio, C.; Tchuinkam, T. High prevalence of asymptomatic Plasmodium falciparum malaria in Makenene, a locality in the forest-savannah transition zone, Centre Region of Cameroon. Curr. Res. Parasitol. Vector Borne Dis. 2022, 2, 100104. [Google Scholar] [CrossRef]
- Berhane, A.; Anderson, K.; Mihreteab, S.; Gresty, K.; Rogier, E.; Mohamed, S.; Hagos, F.; Embaye, G.; Chinorumba, A.; Zehaie, A.; et al. Major threat to malaria control programs by Plasmodium falciparum lacking histidine-rich protein 2, Eritrea. Emerg. Infect. Dis. 2018, 24, 462–470. [Google Scholar] [CrossRef]
- Golassa, L.; Messele, A.; Amambua-Ngwa, A.; Swedberg, G. High prevalence and extended deletions in Plasmodium falciparum hrp2/3 genomic loci in Ethiopia. PLoS ONE 2020, 15, e0241807. [Google Scholar] [CrossRef]
- Bally, D.R.; Santos, S.d.S.; Arregue, D.C.; de Mattos, M.K.; Suárez-Mutis, M.C. High frequency of deletions in the pfhrp2 and pfhrp3 genes of Plasmodium falciparum in the Middle Rio Negro region of the Brazilian Amazon. Trop. Med. Infect. Dis. 2024, 9, 149. [Google Scholar] [CrossRef]
- Kojom Foko, L.P.; Eboumbou Moukoko, C.E.; Jakhan, J.; Narang, G.; Hawadak, J.; Kouemo Motse, F.D.; Pande, V.; Singh, V. Deletions of Histidine-Rich Protein 2/3 Genes in Natural Plasmodium falciparum Populations from Cameroon and India: Role of Asymptomatic and Submicroscopic Infections. Am. J. Trop. Med. Hyg. 2024, 110, 1100–1109. [Google Scholar] [CrossRef] [PubMed]
- Eyong, E.M.; Etutu, S.J.M.; Jerome, F.C.; Nyasa, R.B.; Kwenti, T.E.; Moyeh, M.N. Plasmodium falciparum histidine-rich protein 2 and 3 gene deletion in the Mount Cameroon region. IJID Reg. 2022, 3, 300–307. [Google Scholar] [CrossRef]
- Apinjoh, T.O.; Tangi, L.N.; Oriero, E.C.; Drammeh, S.; Ntui-Njock, V.N.; Etoketim, B.; Chi, H.F.; Kwi, P.N.; Njie, B.; Oboh, M.A.; et al. Histidine-rich protein (hrp) 2-based RDT false-negatives and Plasmodium falciparum hrp 2 and 3 gene deletions in low, seasonal and intense perennial transmission zones in Cameroon: A cross-sectional study. BMC Infect. Dis. 2024, 24, 1080. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; van den Hoogen, L.L.; Slater, H.; Walker, P.G.; Ghani, A.C.; Drakeley, C.J.; Okell, L.C. Comparison of diagnostics for the detection of asymptomatic Plasmodium falciparum infections to inform control and elimination strategies. Nature 2015, 528, S86–S93. [Google Scholar] [CrossRef]
- Bamou, R.; Nematchoua-Weyou, Z.; Lontsi-Demano, M.; Ningahi, L.G.; Tchoumbou, M.A.; Defo-Talom, B.A.; Mayi, M.P.A.; Tchuinkam, T. Performance assessment of a widely used rapid diagnostic test CareStartTM compared to microscopy for the detection of Plasmodium in asymptomatic patients in the Western region of Cameroon. Heliyon 2021, 7, e06271. [Google Scholar] [CrossRef] [PubMed]
- Hosch, S.; Yoboue, C.A.; Donfack, O.T.; Guirou, E.A.; Dangy, J.P.; Mpina, M.; Nyakurungu, E.; Blöchliger, K.; Guerra, C.A.; Phiri, W.P.; et al. Analysis of nucleic acids extracted from rapid diagnostic tests reveals a significant proportion of false positive test results associated with recent malaria treatment. Malar. J. 2022, 21, 23. [Google Scholar] [CrossRef]
- Ngassa Mbenda, H.G.; Das, A. Molecular evidence of Plasmodium vivax mono and mixed malaria parasite infections in Duffy-negative native Cameroonians. PLoS ONE 2014, 9, e103262. [Google Scholar] [CrossRef]
- Russo, G.; Faggioni, G.; Paganotti, G.M.; Djeunang Dongho, G.B.; Pomponi, A.; De Santis, R.; Tebano, G.; Mbida, M.; Sanou Sobze, M.; Vullo, V.; et al. Molecular evidence of Plasmodium vivax infection in Duffy negative symptomatic individuals from Dschang, West Cameroon. Malar. J. 2017, 16, 74. [Google Scholar] [CrossRef]
- Bello, I.S.; Olajubu, T.O.; Osundiya, O.O.; Salami, O.T.; Ibrahim, A.O.; Ahmed, A.A. Malaria among the elderly in five communities of Osun East district, Southwest Nigeria: Prevalence and association with non-communicable diseases. SAGE Open Med. 2023, 11, 1–8. [Google Scholar] [CrossRef]
- Bousema, T.; Okell, L.; Felger, I.; Drakeley, C. Asymptomatic malaria infections: Detectability, transmissibility and public health relevance. Nat. Rev. Microbiol. 2014, 12, 833–840. [Google Scholar] [CrossRef]
- Qu, Z.; Patterson, D.; Childs, L.; Edholm, C.; Ponce, J.; Prosper, O.; Zhao, L. Modeling immunity to malaria with an age-structured PDE framework. SIAM J. Appl. Math. 2023, 83, 1098–1125. [Google Scholar] [CrossRef]
- Mbohou, C.N.; Foko, L.P.K.; Nyabeyeu, H.N.; Tonga, C.; Nono, L.K.; Kangam, L.; Bunda, G.W.; Mbou, I.M.; Hondt, E.O.N.; Mde, A.J.K.; et al. Malaria screening at the workplace in Cameroon. PLoS ONE 2019, 14, e0225219. [Google Scholar] [CrossRef] [PubMed]
- Bartoloni, A.; Zammarchi, L. Clinical aspects of uncomplicated and severe malaria. Mediterr. J. Hematol. Infect. Dis. 2012, 4, e2012026. [Google Scholar] [CrossRef]
- Ibrahim, A.O.; Bello, I.S.; Ajetunmobi, A.O.; Ayodapo, A.; Afolabi, B.A.; Adeniyi, M.A. Prevalence of asymptomatic malaria infection by microscopy and its determinants among residents of Ido-Ekiti, Southwestern Nigeria. PLoS ONE 2023, 18, e0280981. [Google Scholar] [CrossRef]
- Adeka, P.; Imandeh, G.N.; Ikpa, T.F.; Okafor, I.D. Prevalence of Asymptomatic Falciparum Malaria, Risk Factors, and Absence of PfHRP2 Gene Deletion in Makurdi, Nigeria. South Asian J. Res. Microbiol. 2024, 18, 1–7. [Google Scholar] [CrossRef]
- Nkoghe, D.; Akue, J.P.; Gonzalez, J.P.; Leroy, E.M. Prevalence of Plasmodium falciparum infection in asymptomatic rural Gabonese populations. Malar. J. 2011, 10, 33. [Google Scholar] [CrossRef]
- Korzeniewski, K.; Bylicka-Szczepanowska, E.; Lass, A. Prevalence of Asymptomatic Malaria Infections in Seemingly Healthy Children, the Rural Dzanga Sangha Region, Central African Republic. Int. J. Environ. Res. Public Health 2021, 18, 814. [Google Scholar] [CrossRef] [PubMed]
- Cibulskis, R.E.; Aregawi, M.; Williams, R.; Otten, M.; Dye, C. Worldwide incidence of malaria in 2009: Estimates, time trends, and a critique of methods. PLoS Med. 2011, 8, e1001142. [Google Scholar] [CrossRef]
- Hamilton, J.L.; John, S.P. Evaluation of fever in infants and young children. Am. Fam. Physician 2013, 87, 254–260. [Google Scholar]
- Quakyi, I.A.; Ngu, J.; Lohoue, J.; Fogako, J.; Befidi-Mengue, R.; Harun, L.T.; Eno, A.; Walker-Abbey, A.; Folefack, A.; Alake, G.; et al. The epidemiology of Plasmodium falciparum malaria in two Cameroonian villages: Simbok and Etoa. Am. J. Trop. Med. Hyg. 2000, 63, 222–230. [Google Scholar] [CrossRef]
- Etang, J.; Manga, L.; Chandre, F.; Guillet, P.; Fondjo, E.; Mimpfoundi, R.; Toto, J.C.; Fontenille, D. Insecticide susceptibility status of Anopheles gambiae s.l. (Diptera: Culicidae) in the Republic of Cameroon. J. Med. Entomol. 2003, 40, 491–497. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Treatment of Malaria, 3rd ed.; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Tuedom, A.G.B.; Sarah-Matio, E.M.; Moukoko, C.E.E.; Feufack-Donfack, B.L.; Maffo, C.N.; Bayibeki, A.N.; Awono-Ambene, H.P.; Ayong, L.; Berry, A.; Abate, L.; et al. Antimalarial drug resistance in the Central and Adamawa regions of Cameroon: Prevalence of mutations in P. falciparum crt, Pfmdr1, Pfdhfr and Pfdhps genes. PLoS ONE 2021, 16, e0256343. [Google Scholar] [CrossRef] [PubMed]
- Achonduh, O.A.; Mbacham, W.F.; Mangham-Jefferies, L.; Cundill, B.; Chandler, C.; Pamen-Ngako, J.; Lele, A.K.; Ndong, I.C.; Ndive, S.N.; Ambebila, J.N.; et al. Designing and implementing interventions to change clinicians’ practice in the management of uncomplicated malaria: Lessons from Cameroon. Malar. J. 2014, 13, 204. [Google Scholar] [CrossRef] [PubMed]
| Phase | Cycles | Temperature [°C] | Time [min] |
|---|---|---|---|
| Polymerase activation | 1 | 95 | 14:30 |
| Denaturation | 50 | 97 | 00:30 |
| Annealing (data collection) | 60 | 01:00 | |
| Hold | 1 | 32 | 05:00 |
| Variable | mRDT | RT-PCR | ||||||
|---|---|---|---|---|---|---|---|---|
| Pf | Pan | Pf + Pan | Total | P. falciparum | P. vivax | Total | ||
| Total | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 93 (100%) | 19 (20.4%) | 6 (6.5%) | 3 (3.2%) | 28 (30.1%) | 55 (59.1%) | 1 (1.1%) | 56 (60.2%) | |
| Sex | ||||||||
| Female | 44 (47.3%) | 7 (15.9%) | 2 (4.5%) | 2 (4.5%) | 11 (25.0%) | 24 (54.5%) | 0 (0.0%) | 24 (54.5%) |
| Male | 49 (52.7%) | 12 (24.5%) | 4 (8.2%) | 1 (2.0%) | 17 (34.7%) | 31 (63.3%) | 1 (2.0%) | 32 (65.3%) |
| Age | ||||||||
| <5 | 35 (37.6%) | 8 (22.9%) | 3 (8.6%) | 1 (2.9%) | 12 (34.3%) | 22 (62.9%) | 1 (2.9%) | 23 (65.7%) |
| 5–14 | 17 (18.3%) | 7 (41.2%) | 0 (0.0%) | 2 (11.8%) | 9 (52.9%) | 12 (70.6%) | 0 (0.0%) | 12 (70.6%) |
| 15–29 | 14 (15.1%) | 2 (14.3%) | 2 (14.3%) | 0 (0.0%) | 4 (28.6%) | 7 (50%) | 0 (0.0%) | 7 (50%) |
| 30–49 | 14 (15.1%) | 1 (7.1%) | 1 (7.1%) | 0 (0.0%) | 2 (14.3%) | 6 (42.9%) | 0 (0.0%) | 6 (42.9%) |
| ≥50 | 13 (14.0%) | 1 (7.7%) | 0 (0.0%) | 0 (0.0%) | 1 (7.7%) | 8 (61.5%) | 0 (0.0%) | 8 (61.5%) |
| Clinical phenotype | ||||||||
| Symptoms | 36 (38.7%) | 18 (50.0%) | 2 (5.6%) | 3 (8.3%) | 23 (63.9%) | 30 (83.3%) | 0 (0.0%) | 30 (83.3%) |
| Fever | 26 (28.0%) | 9 (34.6%) | 2 (7.7%) | 2 (7.7%) | 13 (50.0%) | 20 (76.9%) | 0 (0.0%) | 20 (76.9%) |
| Respiratory | 12 (12.9%) | 8 (66.7%) | 0 (0.0%) | 1 (8.3%) | 9 (75.0%) | 10 (83.3%) | 0 (0.0%) | 10 (83.3%) |
| Gastroenterological | 7 (7.5%) | 4 (57.1%) | 0 (0.0%) | 2 (28.6%) | 6 (85.7%) | 5 (71.4%) | 0 (0.0%) | 5 (71.4%) |
| No symptoms | 57 (61.3%) | 1 (1.8%) | 4 (7.0%) | 0 (0.0%) | 5 (8.8%) | 25 (43.9%) | 1 (1.8%) | 26 (45.6%) |
| Variable | Infected (n = 56) | Non-Infected (n = 37) | Total (n = 93) | p-Value |
|---|---|---|---|---|
| Gender | 0.2899 1 | |||
| Female | 24 (42.9%) | 20 (54.1%) | 44 (47.3%) | |
| Male | 32 (57.1%) | 17 (45.9%) | 49 (52.7%) | |
| Age | 0.2328 2 | |||
| Mean (SD) | 18.5 (21.5) | 23.0 (21.2) | 20.3 (21.5) | |
| Range | 1–70 | 1–70 | 1–70 | |
| Median | 8.5 | 23 | 10 | |
| Clinical phenotype | 0.0002 1 | |||
| Symptoms | 30 (53.6%) | 6 (16.2%) | 36 (38.7%) | |
| Asymptomatic infection | 26 (46.4%) | 31 (83.8%) | 57 (61.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stopyra, L.; Wilczyńska, W.; Kołodziej, D.; Noel, A.; Korzeniewski, K. Plasmodium spp. Infections Among Mbalmayo Inhabitants of Central Region in Cameroon: Discrepancies Between Rapid Diagnostic Tests and Molecular Methods. Pathogens 2025, 14, 462. https://doi.org/10.3390/pathogens14050462
Stopyra L, Wilczyńska W, Kołodziej D, Noel A, Korzeniewski K. Plasmodium spp. Infections Among Mbalmayo Inhabitants of Central Region in Cameroon: Discrepancies Between Rapid Diagnostic Tests and Molecular Methods. Pathogens. 2025; 14(5):462. https://doi.org/10.3390/pathogens14050462
Chicago/Turabian StyleStopyra, Lidia, Wanesa Wilczyńska, Daria Kołodziej, Assamba Noel, and Krzysztof Korzeniewski. 2025. "Plasmodium spp. Infections Among Mbalmayo Inhabitants of Central Region in Cameroon: Discrepancies Between Rapid Diagnostic Tests and Molecular Methods" Pathogens 14, no. 5: 462. https://doi.org/10.3390/pathogens14050462
APA StyleStopyra, L., Wilczyńska, W., Kołodziej, D., Noel, A., & Korzeniewski, K. (2025). Plasmodium spp. Infections Among Mbalmayo Inhabitants of Central Region in Cameroon: Discrepancies Between Rapid Diagnostic Tests and Molecular Methods. Pathogens, 14(5), 462. https://doi.org/10.3390/pathogens14050462








