A Modified Surgical Face Mask to Improve Protection and Wearing Comfort
Abstract
:1. Introduction
2. Research Methods
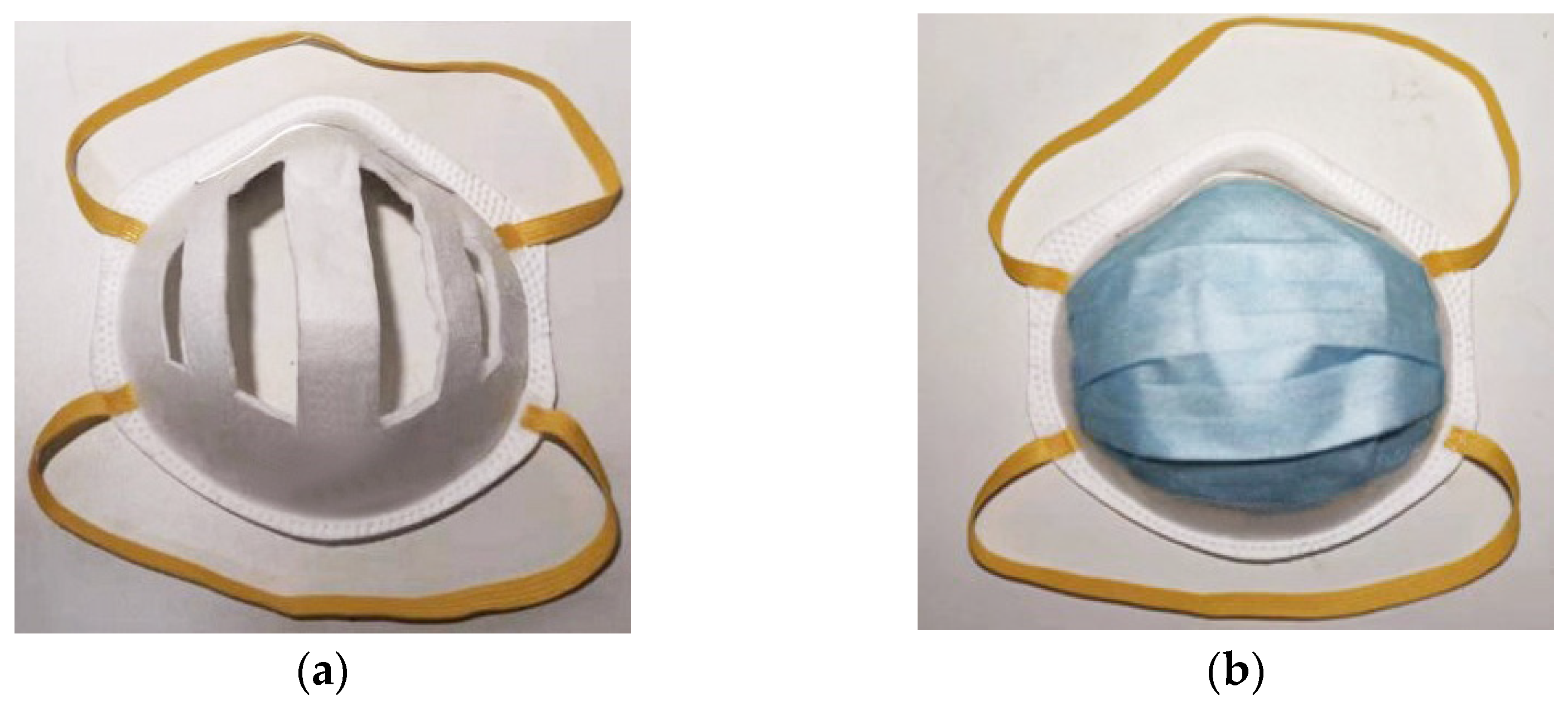
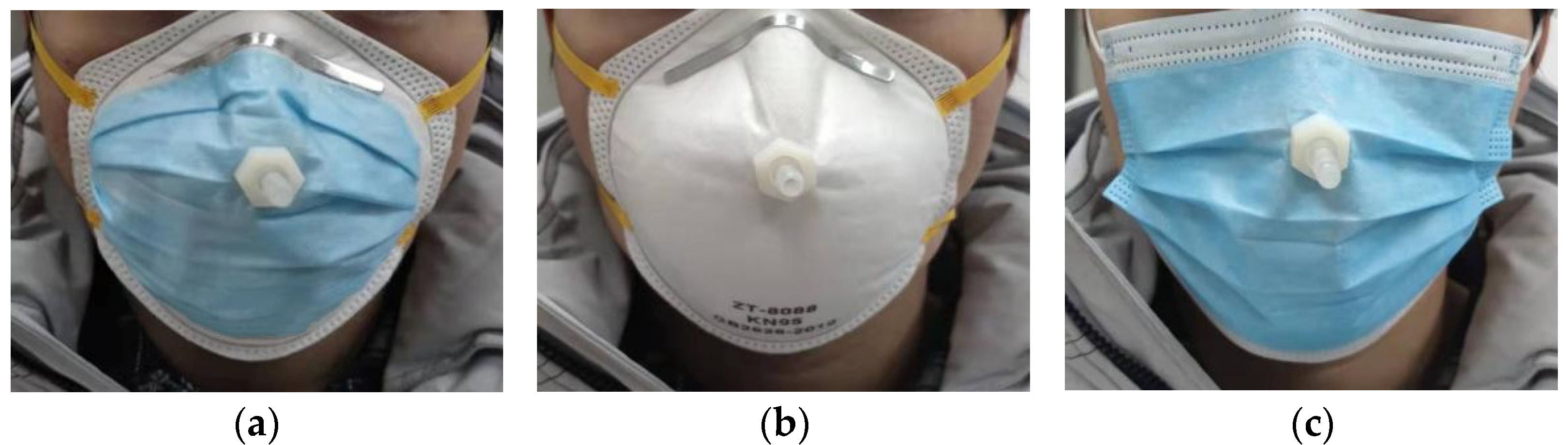
2.1. Modified Face Mask and Measurement of Air Contents Inside
2.2. Measurement of Dead Space and Respiratory Resistance
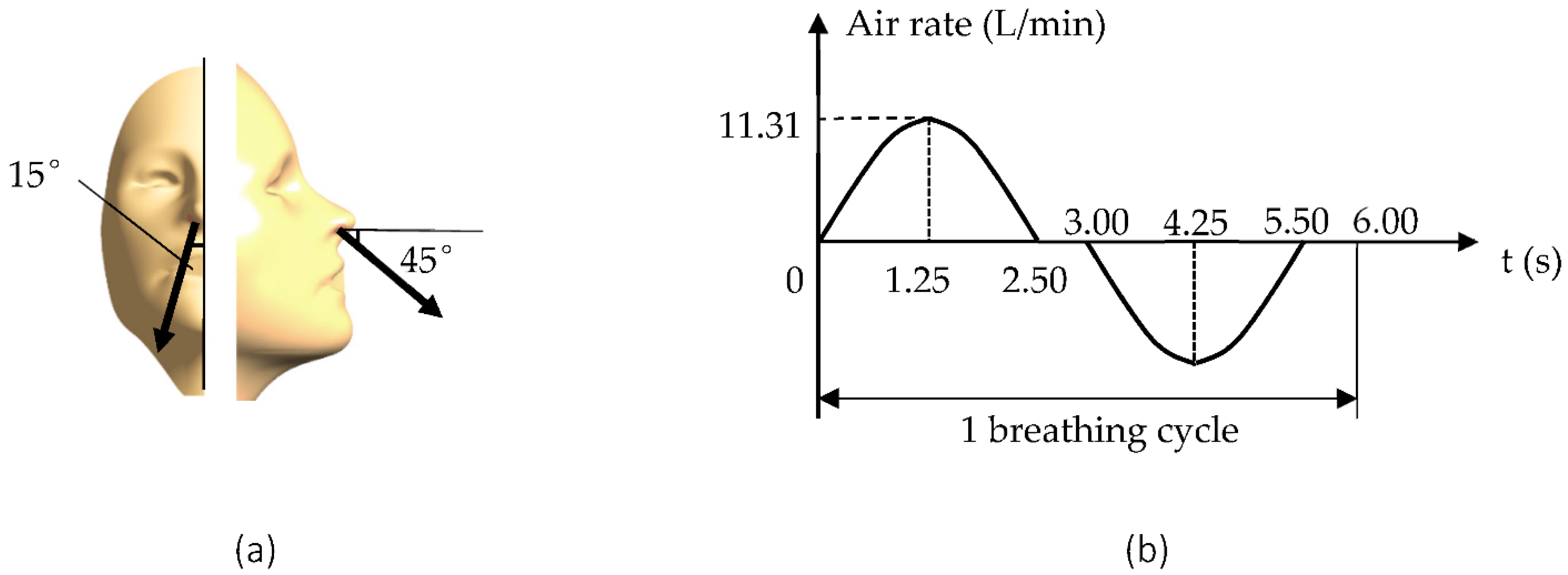
2.3. CFD Modeling of Dynamic Air Exchange and Air Sampling to a Face Mask
3. Results
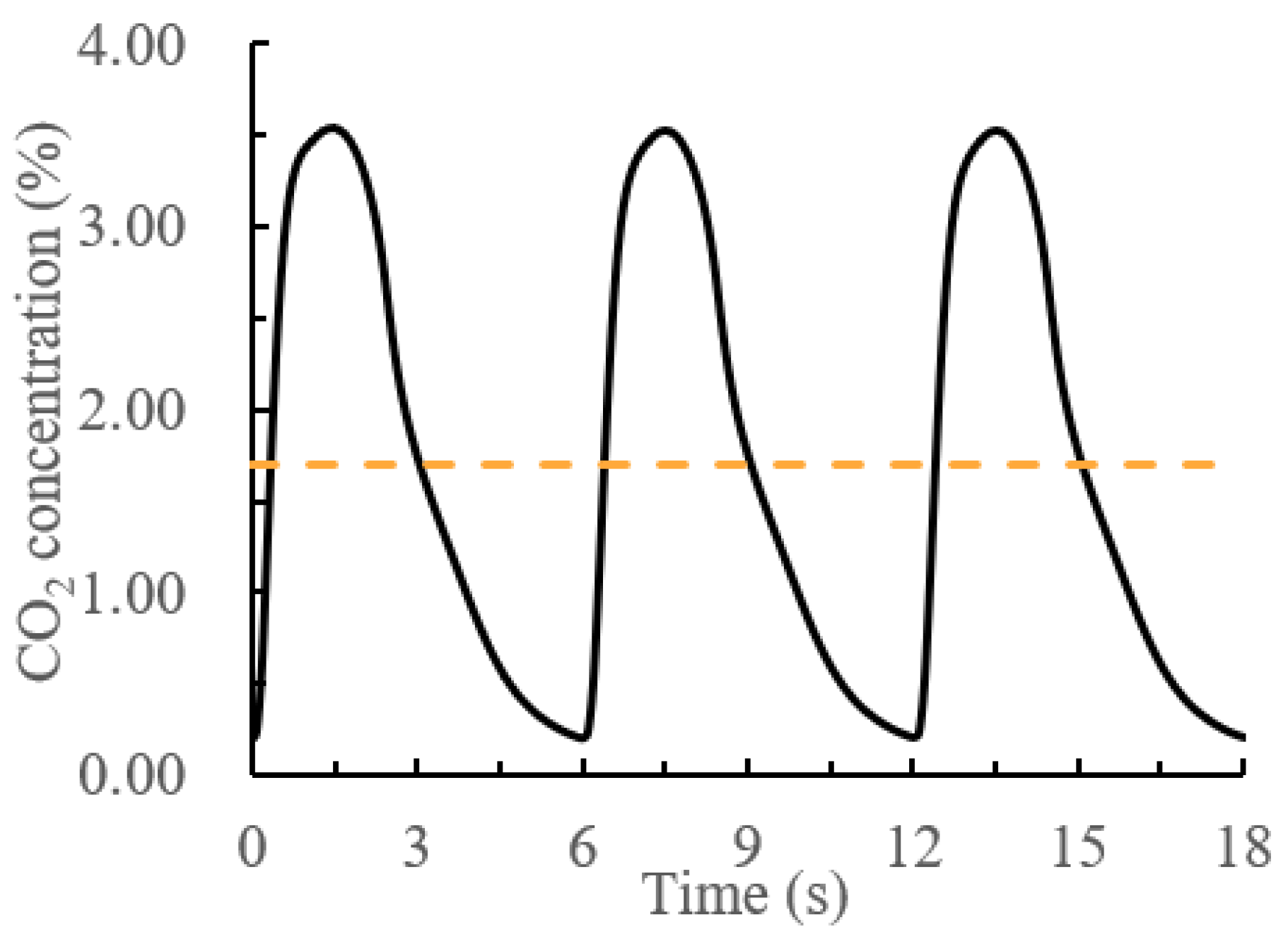
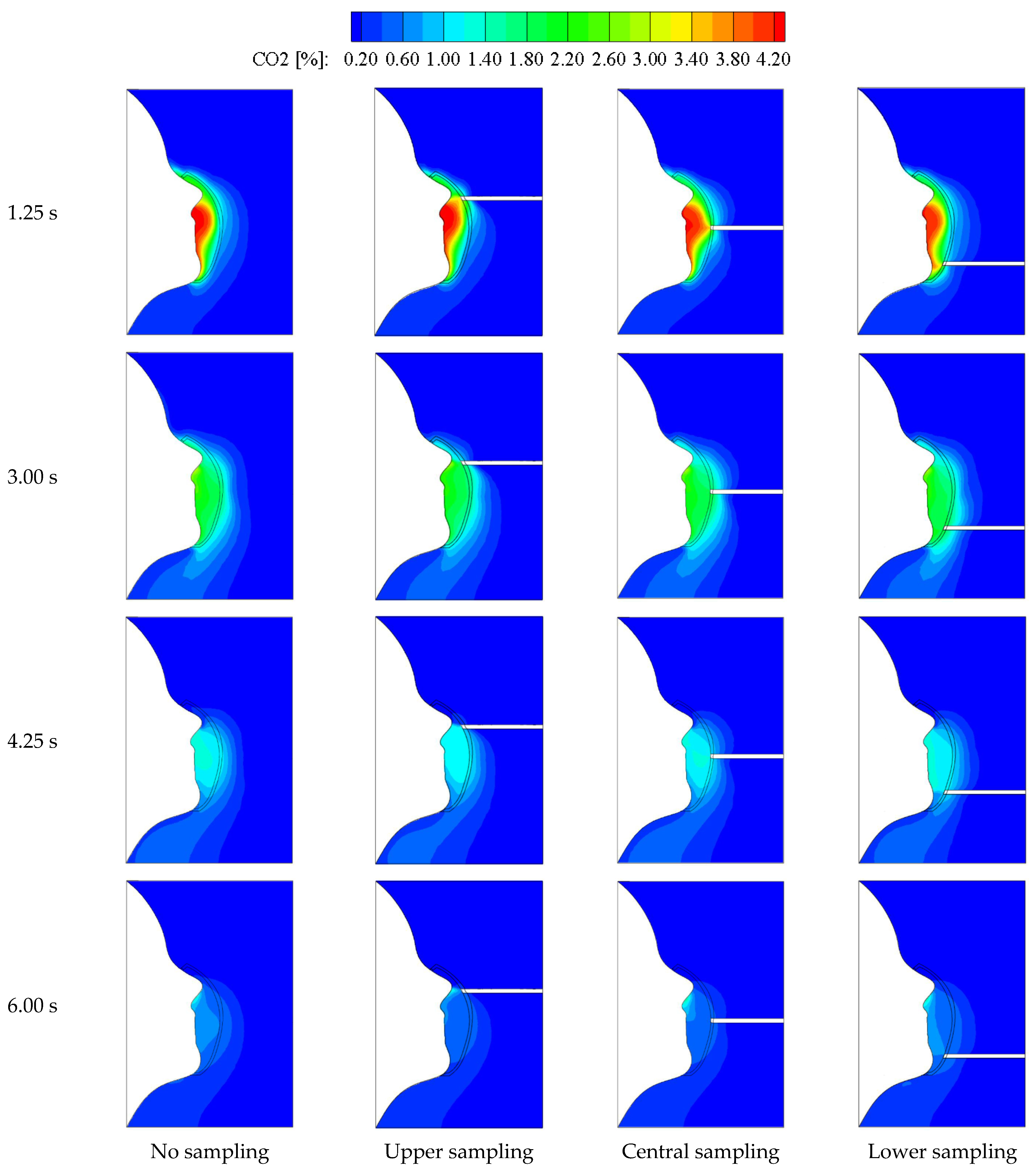
3.1. Dynamic Air Exchange and Air Sampling of the N95 Face Mask
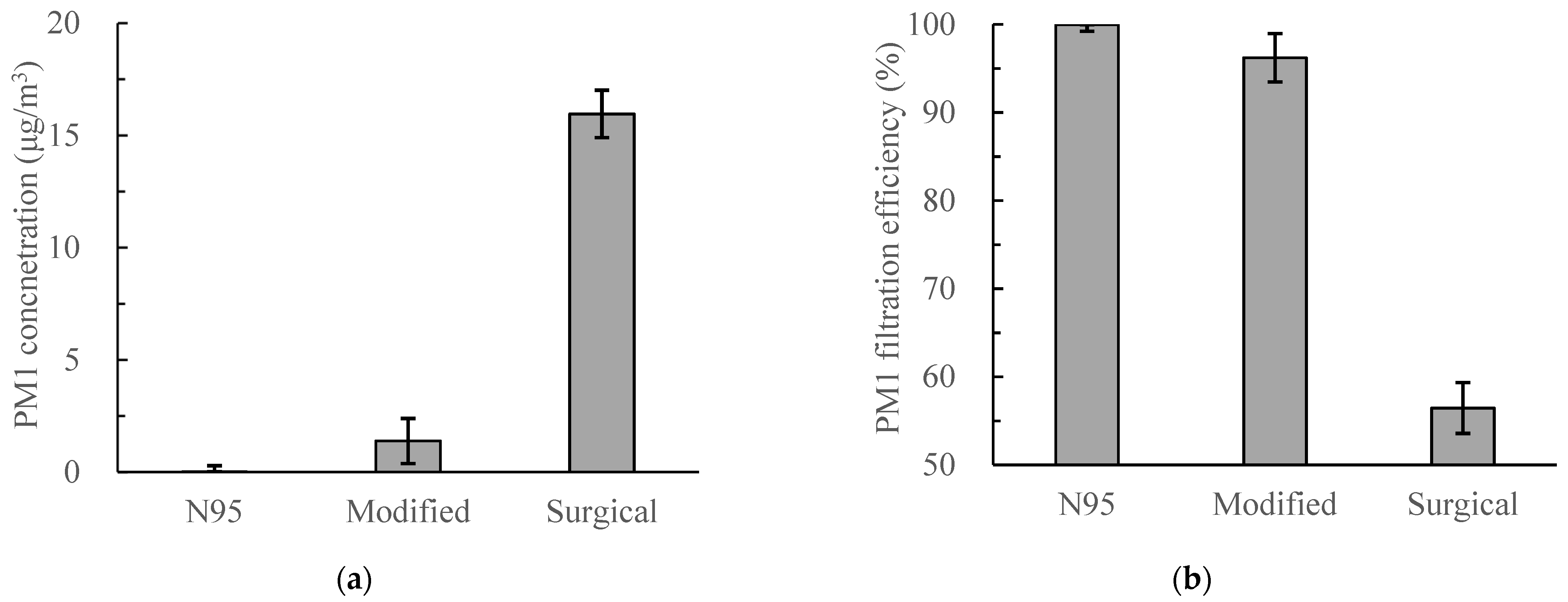
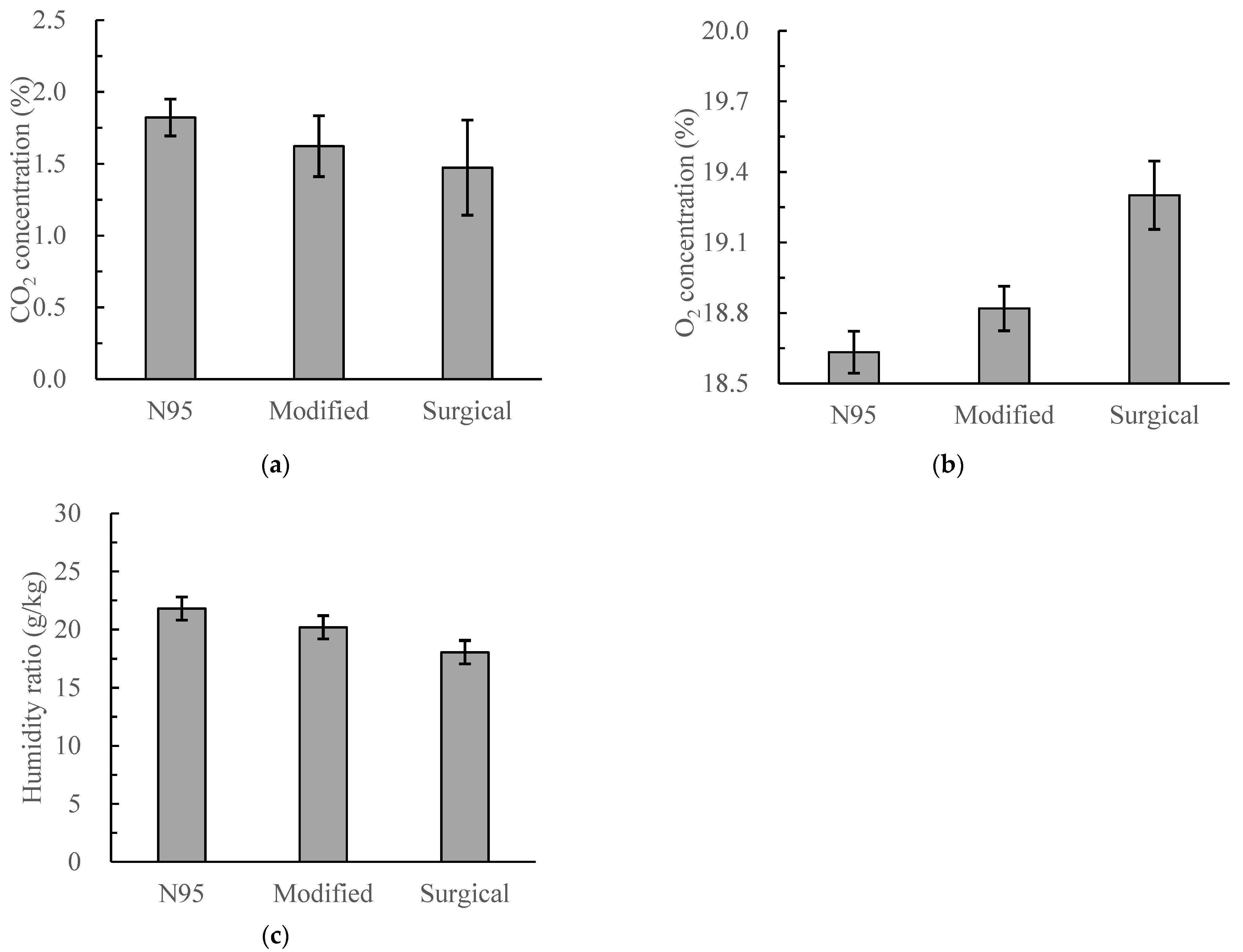
3.2. Measured Particle Filtration Efficiency and Air Contents
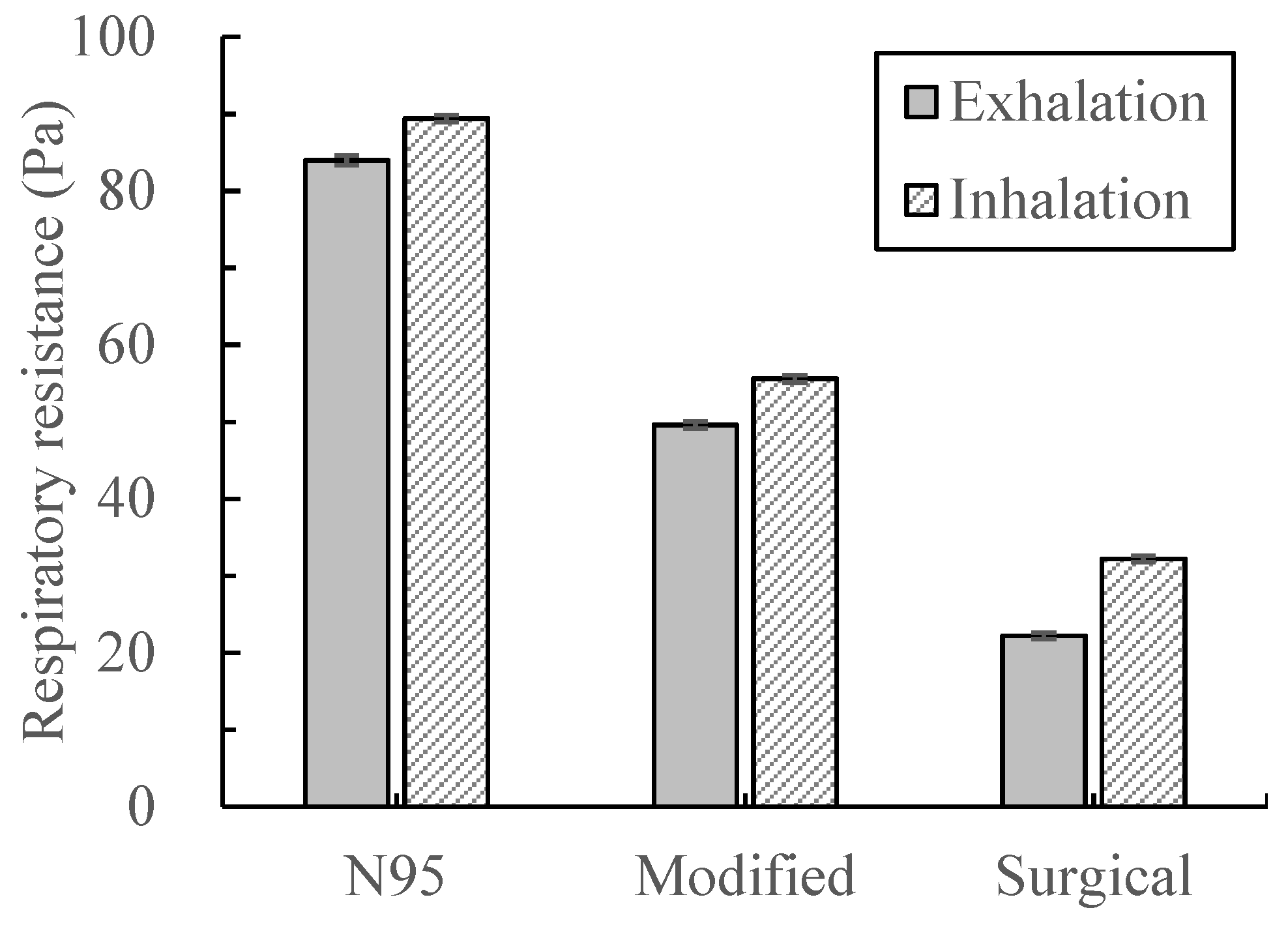
3.3. Measured Dead Space and Respiratory Flow Resistance
4. Discussion
5. Conclusions
- As compared with the surgical face masks, the airtightness and protective performance of the modified masks were greatly enhanced. The overall PM1 filtration efficiency of the face mask reached 96.21%, which was much higher than that of the surgical face mask and only slightly lower than the N95 face mask.
- As compared with the N95 face mask, the modified mask reduced both the concentrations of CO2 and water vapor and increased the concentration of O2. Both the steady exhalation and inhalation resistances were reduced by 41.67% and 37.81%, respectively, against the N95 face mask. The modified face mask could thus improve the breathing comfort.
- Air sampling increased the inward leakage of the face mask. The air mixing condition inside the face mask was highly nonuniform and varied with time. The highest CO2 concentration was near the mouth. The central sampling could better indicate the inhaled air status.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Validation of CFD Modeling
References
- Law, R.C.K.; Lai, J.H.K.; Edwards, D.J.; Hou, H. COVID-19: Research Directions for Non-Clinical Aerosol-Generating Facilities in the Built Environment. Buildings 2021, 11, 282. [Google Scholar] [CrossRef]
- Leung, N.H.L.; Chu, D.K.W.; Shiu, E.Y.C.; Chan, K.H.; McDevitt, J.J.; Hau, B.J.P.; Yen, H.L.; Li, Y.; Ip, D.K.M.; Peiris, J.S.M.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arumuru, V.; Pasa, J.; Samantaray, S.S. Experimental visualization of sneezing and efficacy of face masks and shields. Phys. Fluids 2020, 32, 115129. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Ma, N.; Witt, C.; Rapp, S.; Wild, P.S.; Andreae, M.O.; Poschl, U.; Su, H. Face masks effectively limit the probability of SARS-CoV-2 transmission. Science 2021, 372, 1439–1443. [Google Scholar] [CrossRef] [PubMed]
- Dbouk, T.; Drikakis, D. On respiratory droplets and face masks. Phys. Fluids 2020, 32, 063303. [Google Scholar] [CrossRef]
- WHO. Mask Use in the Context of COVID-19, Interim Guidance; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Cheok, G.J.W.; Gatot, C.; Sim, C.H.S.; Ng, Y.H.; Tay, K.X.K.; Howe, T.S.; Koh, J.S.B. Appropriate attitude promotes mask wearing in spite of a significant experience of varying discomfort. Infect. Dis. Health 2021, 26, 145–151. [Google Scholar] [CrossRef]
- Drewnick, F.; Pikmann, J.; Fachinger, F.; Moormann, L.; Sprang, F.; Borrmann, S. Aerosol filtration efficiency of household materials for homemade face masks: Influence of material properties, particle size, particle electrical charge, face velocity, and leaks. Aerosol. Sci. Technol. 2020, 55, 63–79. [Google Scholar] [CrossRef]
- Dhivyadharshini, J.S.J.; Brundha, M.P. composition and uses of N95 masks-a review. Eur. J. Mol. Clin. Med. 2020, 7, 1529–1540. [Google Scholar]
- Sato, J.; Yamawaki, Y.; Ito, M.; Endo, M.; Tanaka, R.; Shino, M. Measurement of the leak rate of masks used for anticancer drug handling using a mask fitting tester. J. Oncol. Pharm. Pract. 2020, 26, 1318–1323. [Google Scholar] [CrossRef]
- Huo, S.; Zhang, T.T. Ventilation of ordinary face masks. Build. Environ. 2021, 205, 108261. [Google Scholar] [CrossRef]
- Akhtar, J.; Garcia, A.L.; Saenz, L.; Kuravi, S.; Shu, F.; Kota, K. Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions?—A quantitative study. Phys. Fluids 2020, 32, 127112. [Google Scholar] [CrossRef]
- Zhang, R.; Liu, J.; Zhang, L.; Lin, J.; Wu, Q. The distorted power of medical surgical masks for changing the human thermal psychology of indoor personnel in summer. Indoor Air 2021, 31, 1645–1656. [Google Scholar] [CrossRef] [PubMed]
- Sinkule, E.J.; Powell, J.B.; Goss, F.L. Evaluation of N95 respirator use with a surgical mask cover: Effects on breathing resistance and inhaled carbon dioxide. Ann. Occup. Hyg. 2013, 57, 384–398. [Google Scholar]
- Lee, H.P.; Wang, D.Y. Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann. Occup. Hyg. 2011, 55, 917–921. [Google Scholar] [PubMed] [Green Version]
- Tcharkhtchi, A.; Abbasnezhad, N.; Seydani, M.Z.; Zirak, N.; Farzaneh, S.; Shirinbayan, M. An overview of filtration efficiency through the masks: Mechanisms of the aerosols penetration. Bioact. Mater. 2021, 6, 106–122. [Google Scholar] [CrossRef]
- Choi, S.; Jeon, H.; Jang, M.; Kim, H.; Shin, G.; Koo, J.M.; Lee, M.; Sung, H.K.; Eom, Y.; Yang, H.S.; et al. Biodegradable, Efficient, and Breathable Multi-Use Face Mask Filter. Adv. Sci. 2021, 8, 2003155. [Google Scholar] [CrossRef]
- Li, X.; Gong, Y. Design of Polymeric Nanofiber Gauze Mask to Prevent Inhaling PM2.5 Particles from Haze Pollution. J. Chem. 2015, 2015, 460392. [Google Scholar] [CrossRef]
- Wang, N.; Cai, M.; Yang, X.; Yang, Y. Electret nanofibrous membrane with enhanced filtration performance and wearing comfortability for face mask. J. Colloid Interface Sci. 2018, 530, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, H.; Shen, S.; Rao, Y.; Chen, F. An Improved FFR Design with a Ventilation Fan: CFD Simulation and Validation. PLoS ONE 2016, 11, e0159848. [Google Scholar] [CrossRef] [PubMed]
- Suen, W.S.; Huang, G.; Kang, Z.; Gu, Y.; Fan, J.; Shou, D. Development of wearable air-conditioned mask for personal thermal management. Build. Environ. 2021, 205, 108236. [Google Scholar] [CrossRef]
- Morris, L.A. Dead Space and Inhaled Carbon Dioxide Levels in Respiratory Protective Equipment; HSE Contract Research Report No. 27; Health and Safety Executive: London, UK, 1991.
- NIOSH. Determination of Exhalation Resistance. 2019. Available online: https://www.cdc.gov/niosh/npptl/stps/pdfs/TEB-APR-STP-0003-508.pdf (accessed on 27 March 2022).
- NIOSH. Determination of Inhalation Resistance. 2019. Available online: https://www.cdc.gov/niosh/npptl/stps/pdfs/TEB-APR-STP-0007-508.pdf (accessed on 27 March 2022).
- Zhang, T.T.; Yin, S.; Wang, S. Quantify impacted scope of human expired air under different head postures and varying exhalation rates. Build. Environ. 2011, 46, 1928–1936. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, H.; Shen, S.; Cai, M. Investigation of the flow-field in the upper respiratory system when wearing N95 filtering facepiece respirator. J. Occup. Environ. Hyg. 2016, 13, 372–382. [Google Scholar] [CrossRef] [PubMed]



| Item | Setting |
|---|---|
| Nostril opening | Velocity-inlet (profile shown as Figure 5); 33 °C; CO2: 4.20% |
| Air sampling tube opening | Velocity-inlet, 3.98 m/s |
| Face skin | Wall, 32 °C |
| Right domain boundary | Velocity-inlet, 0.05 m/s; 22 °C; CO2: 0.05% |
| Other domain boundaries (except for the symmetric boundary) | Pressure-outlet, backflow air temperature: 22 °C |
| Face mask | Porous media, porosity: 0.88 |
| Leakage clearance | Porous media, porosity: 0.99 |
| No Sampling | Upper Sampling | Central Sampling | Lower Sampling | |
|---|---|---|---|---|
| QF,in, L/min | 2.513 | 3.205 | 3.205 | 3.205 |
| QL,in, L/min | 0.488 | 0.623 | 0.623 | 0.623 |
| QF,out, L/min | 2.510 | 1.953 | 1.953 | 1.953 |
| QL,out, L/min | 0.484 | 0.374 | 0.375 | 0.374 |
| Inward leakage rate | 16.26% | 20.78% | 20.76% | 20.78% |
| Outward leakage rate | 16.13% | 12.47% | 12.49% | 12.48% |
| No Sampling | Upper Sampling | Central Sampling | Lower Sampling | |
|---|---|---|---|---|
| csampling | - | 1.37% | 1.70% | 1.51% |
| cmask | 1.20% | 1.14% | 1.16% | 1.15% |
| N2 | CO2 | O2 | |
|---|---|---|---|
| N95 | 76.58% | 2.71% | 17.08% |
| Modified | 76.89% | 2.22% | 18.05% |
| Surgical | 76.96% | 1.64% | 18.81% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Zhang, T.; Liu, S. A Modified Surgical Face Mask to Improve Protection and Wearing Comfort. Buildings 2022, 12, 663. https://doi.org/10.3390/buildings12050663
Zhang T, Zhang T, Liu S. A Modified Surgical Face Mask to Improve Protection and Wearing Comfort. Buildings. 2022; 12(5):663. https://doi.org/10.3390/buildings12050663
Chicago/Turabian StyleZhang, Tengfei (Tim), Tinglu Zhang, and Sumei Liu. 2022. "A Modified Surgical Face Mask to Improve Protection and Wearing Comfort" Buildings 12, no. 5: 663. https://doi.org/10.3390/buildings12050663
APA StyleZhang, T., Zhang, T., & Liu, S. (2022). A Modified Surgical Face Mask to Improve Protection and Wearing Comfort. Buildings, 12(5), 663. https://doi.org/10.3390/buildings12050663








