Virtual Versus Light Microscopy Usage among Students: A Systematic Review and Meta-Analytic Evidence in Medical Education
Abstract
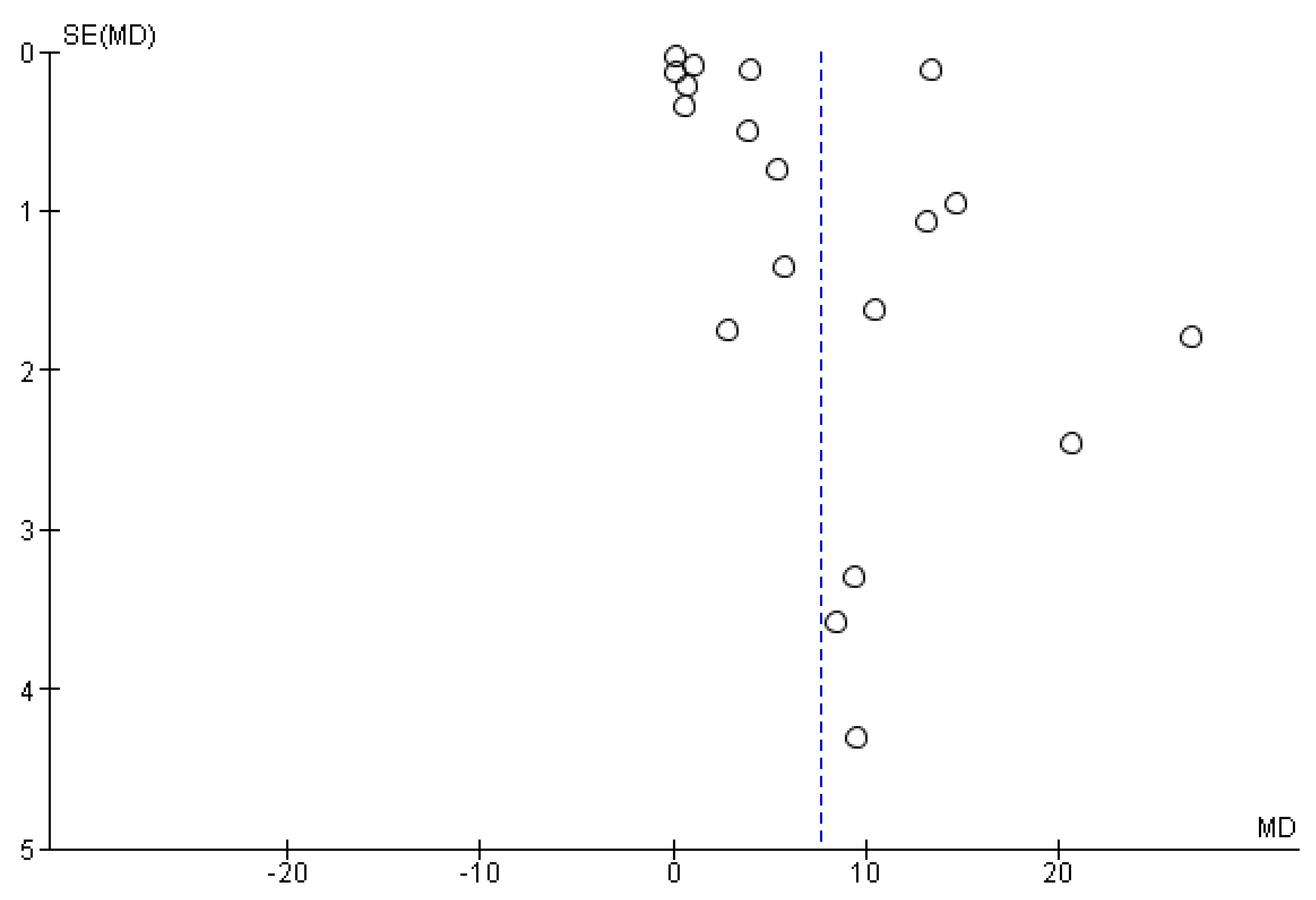
1. Introduction
1.1. Whole-Slide Imaging (WSI)
1.2. Virtual Microscopy and COVID-19
1.2.1. General
- No risk of deterioration of staining quality or breakage of slides, no fading or stored slides, shorter sign-out time, access from any device, better flexibility, easy image sharing in clinical communication
1.2.2. Telepathology
- Quick access, elimination of physical slide transfer, better availability of service for remote and understaffed areas
1.2.3. Cost and Efficiency
- Better archiving, sharing, and easy retrieval; faster turnaround times, reduced cost of equipment, lab maintenance, and auxiliary techniques (less immunohistochemistry).
2. Materials and Methods
2.1. Literature Review
2.2. Eligibility Criteria
2.3. Exclusion Criteria
2.4. Search Criteria and Database
2.5. Article Screening and Eligibility Evaluation
2.6. Extraction of Qualitative and Quantitative Data
2.7. Quality Assessment
2.8. Statistical Analyses
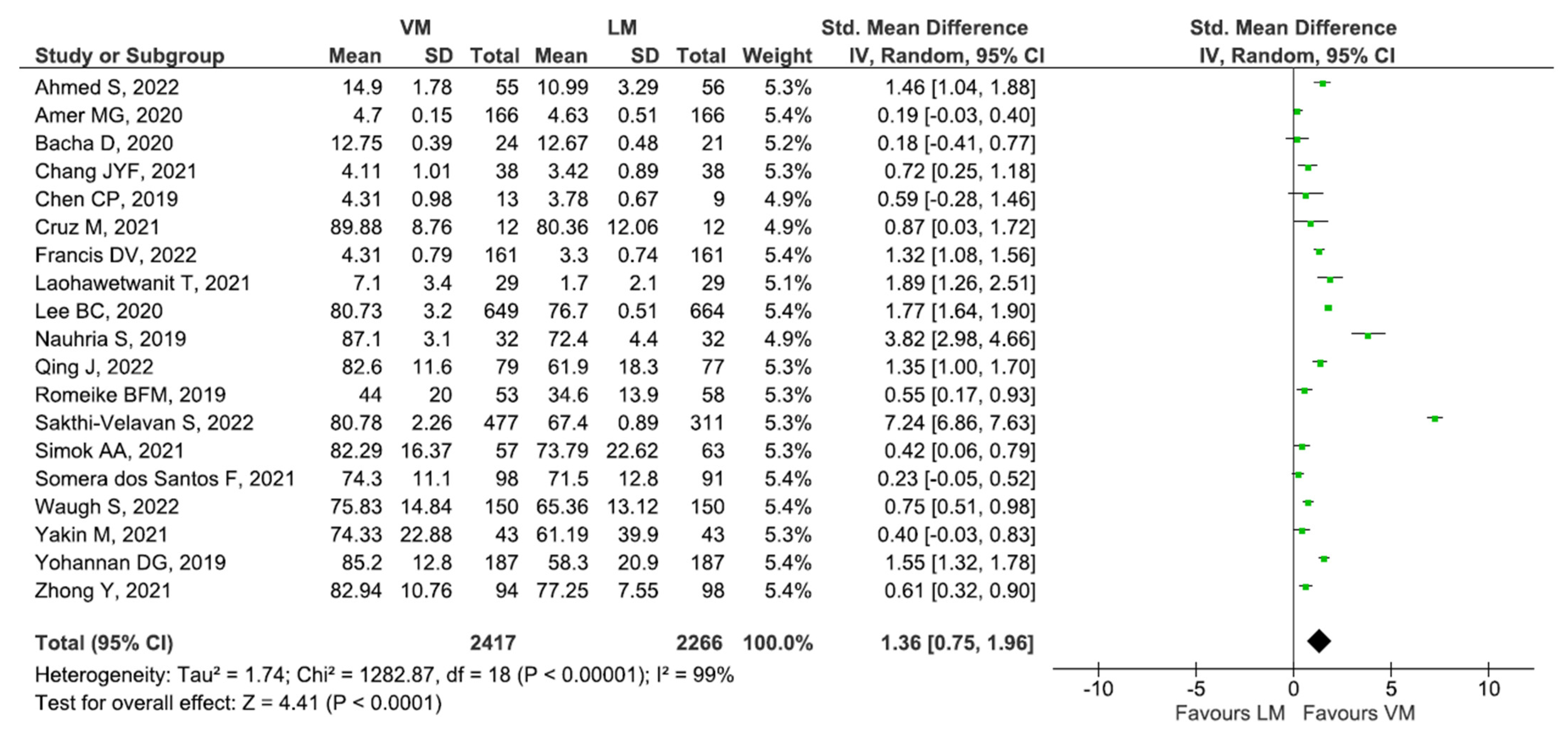
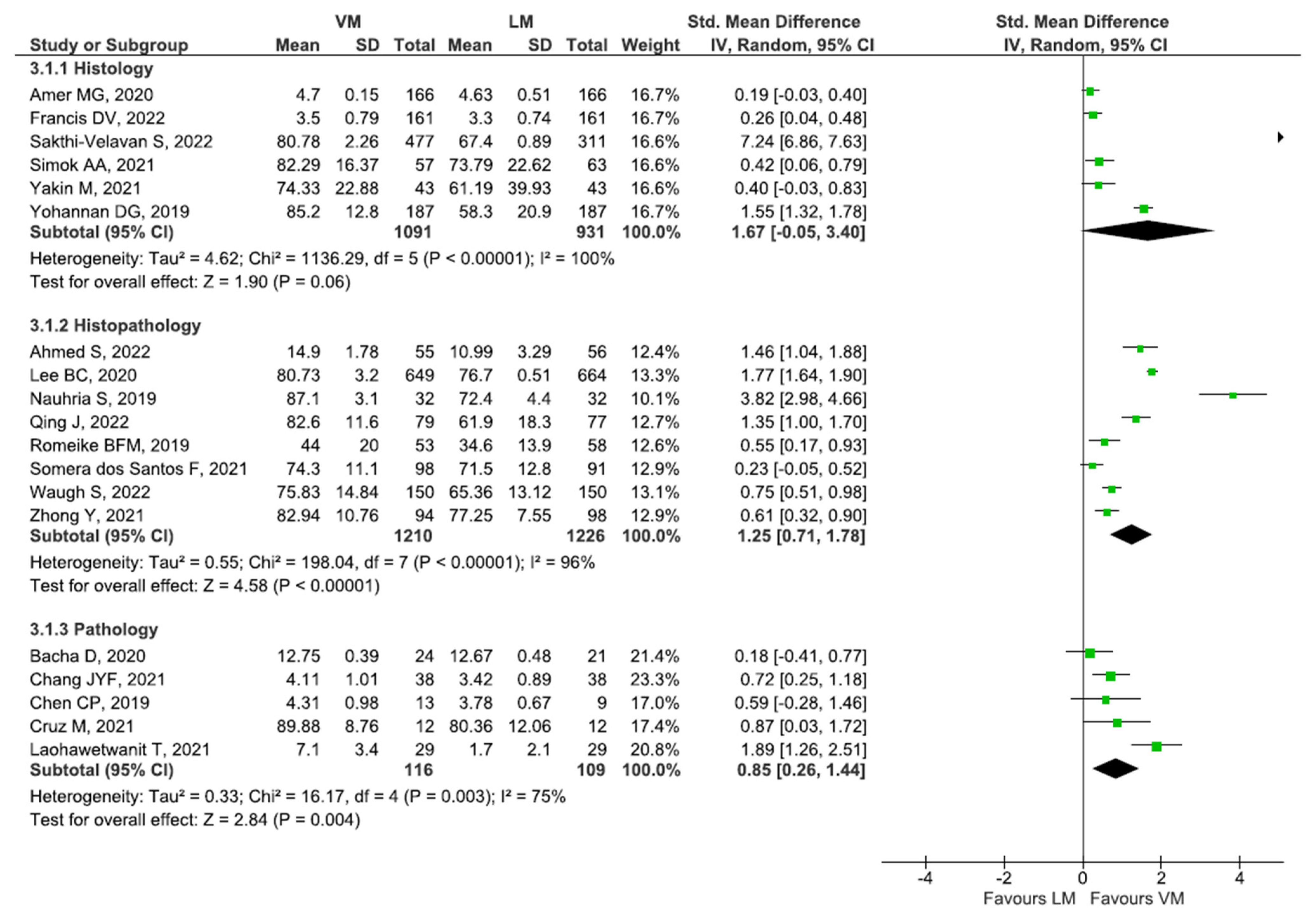
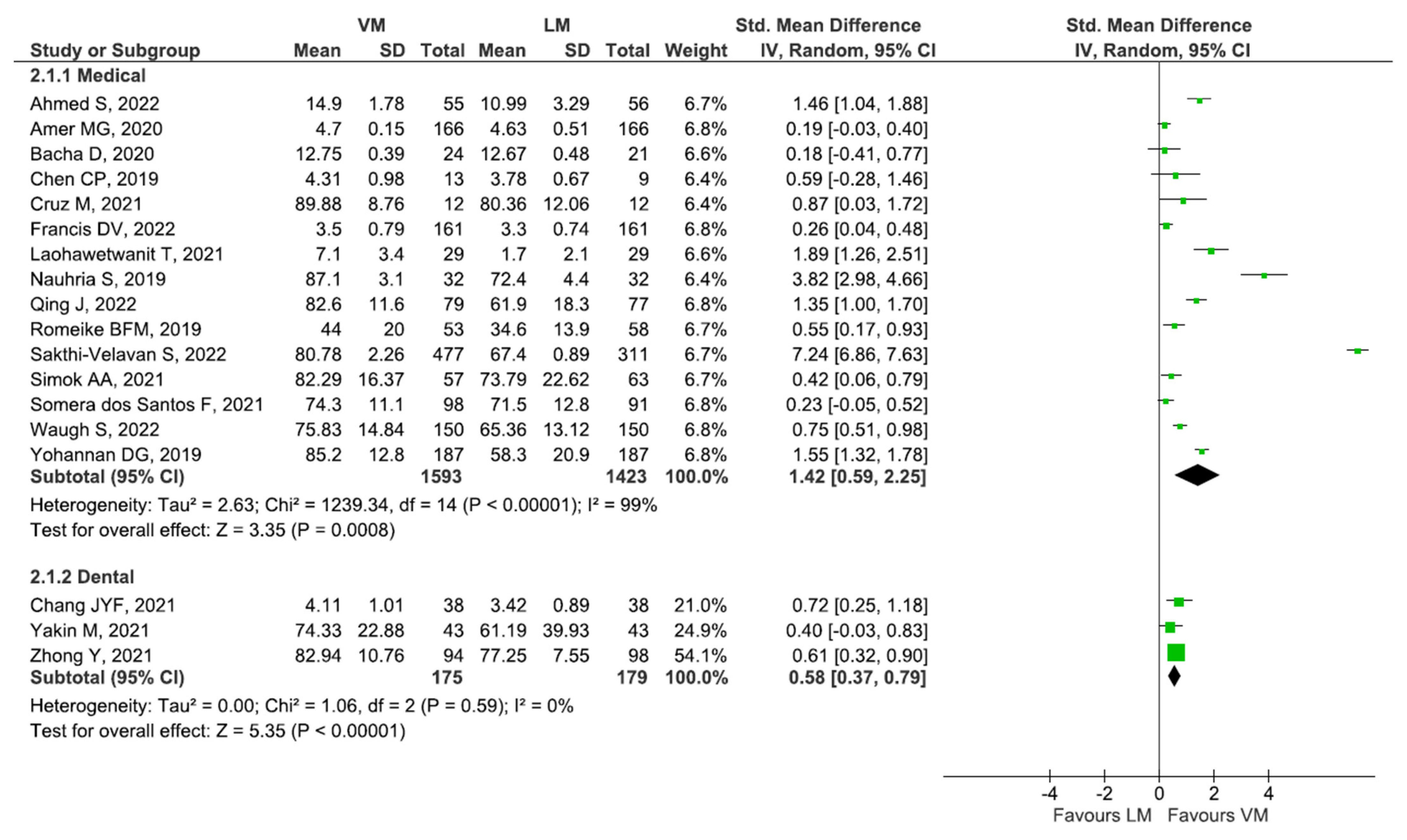
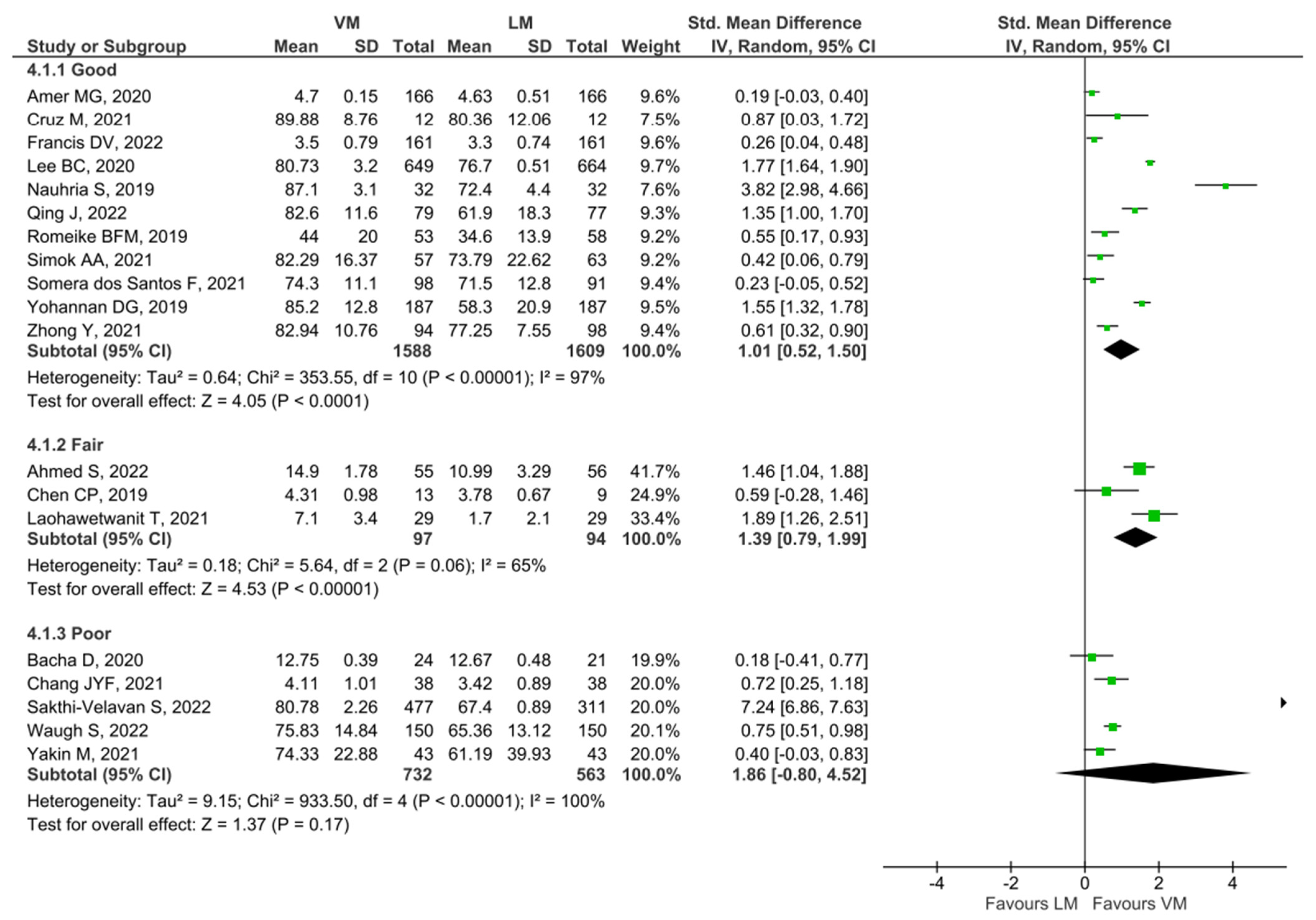
3. Results
3.1. Search Results and Study Characteristics
3.2. Quality Assessment of Included Studies Using NOS
4. Discussion
Limitations of this Review
5. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Camargo, C.P.; Tempski, P.Z.; Busnardo, F.F.; de Arruda Martins, M.; Gemperli, R. Online learning and COVID-19: A meta-synthesis analysis. Clinics 2020, 75, e2286. [Google Scholar] [CrossRef] [PubMed]
- Caruso, M.C. Virtual Microscopy and Other Technologies for Teaching Histology During COVID-19. Anat. Sci. Educ. 2020, 14, 19–21. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Chan, L.K.; Cai, H.; Zhou, D.; Yang, X. Adaptions and perceptions on histology and embryology teaching practice in China during the COVID-19 pandemic. Transl. Res. Anat. 2021, 24, 100115. [Google Scholar] [CrossRef]
- Retamero, J.A.; Aneiros-Fernandez, J.; del Moral, R.G. Complete Digital Pathology for Routine Histopathology Diagnosis in a Multicenter Hospital Network. Arch. Pathol. Lab. Med. 2019, 144, 221–228. [Google Scholar] [CrossRef]
- Volynskaya, Z.; Chow, H.; Evans, A.; Wolff, A.; Lagmay, T.C.; Asa, S.L. Integrated Pathology Informatics Enables High-Quality Personalized and Precision Medicine: Digital Pathology and Beyond. Arch. Pathol. Lab. Med. 2017, 142, 369–382. [Google Scholar] [CrossRef]
- Evans, A.J.; Brown, R.W.; Bui, M.M.; Chlipala, E.A.; Lacchetti, C.; Milner, D.A.; Pantanowitz, L.; Parwani, A.V.; Reid, K.; Riben, M.W.; et al. Validating Whole Slide Imaging Systems for Diagnostic Purposes in Pathology. Arch. Pathol. Lab. Med. 2022, 146, 440–450. [Google Scholar] [CrossRef]
- Jahn, S.W.; Plass, M.; Moinfar, F. Digital Pathology: Advantages, Limitations and Emerging Perspectives. J. Clin. Med. 2020, 9, 3697. [Google Scholar] [CrossRef]
- FDA Allows Marketing of First Whole Slide Imaging System for Digital Pathology. Available online: https://www.fda.gov/news-events/press-announcements/fda-allows-marketing-first-whole-slide-imaging-system-digital-pathology (accessed on 22 January 2022).
- Nauhria, S.; Hangfu, L. Virtual microscopy enhances the reliability and validity in histopathology curriculum: Practical guidelines. MedEdPublish 2019, 8, 28. [Google Scholar] [CrossRef]
- Boyce, B.F. An update on the validation of whole slide imaging systems following FDA approval of a system for a routine pathology diagnostic service in the United States. Biotech. Histochem. 2017, 92, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Gupta, R.; Gupta, S. Whole Slide Imaging (WSI) in Pathology: Current Perspectives and Future Directions. J. Digit. Imaging 2020, 33, 1034–1040. [Google Scholar] [CrossRef]
- Araújo, A.L.D.; Arboleda, L.P.A.; Palmier, N.R.; Fonsêca, J.M.; de Pauli Paglioni, M.; Gomes-Silva, W.; Ribeiro, A.C.P.; Brandão, T.B.; Simonato, L.E.; Speight, P.M.; et al. The performance of digital microscopy for primary diagnosis in human pathology: A systematic review. Virchows Arch. 2019, 474, 269–287. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.B.; Taylor, M.A.; Klein, B.A.; Sugrue, M.K.; Whipple, E.C.; Brokaw, J.J. Meta-analysis and review of learner performance and preference: Virtual versus optical microscopy. Med. Educ. 2016, 50, 428–440. [Google Scholar] [CrossRef] [PubMed]
- Kuo, K.H.; Leo, J.M. Optical Versus Virtual Microscope for Medical Education: A Systematic Review. Anat. Sci. Educ. 2018, 12, 678–685. [Google Scholar] [CrossRef]
- Joaquim, D.C.; Hortsch, M.; Silva, A.S.R.d.; David, P.B.; Leite, A.C.R.d.M.; Girão-Carmona, V.C.C. Digital information and communication technologies on histology learning: What to expect?—An integrative review. Anat. Histol. Embryol. 2021, 51, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Indu, M.; Rathy, R.; Binu, M.P. “Slide less pathology”: Fairy tale or reality? J. Oral Maxillofac. Pathol. 2016, 20, 284–288. [Google Scholar] [CrossRef]
- Saco, A.; Bombi, J.A.; Garcia, A.; Ramírez, J.; Ordi, J. Current Status of Whole-Slide Imaging in Education. Pathobiology 2016, 83, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Sasongko, W.D.; Widiastuti, I. Virtual lab for vocational education in Indonesia: A review of the literature. In Proceedings of the The 2nd International Conference on Science, Mathematics, Environment, and Education; AIP Publishing: Long Island, NY, USA, 2019. [Google Scholar]
- Lujan, G.M.; Savage, J.; Shana’ah, A.; Yearsley, M.; Thomas, D.; Allenby, P.; Otero, J.; Limbach, A.L.; Cui, X.; Scarl, R.T.; et al. Digital Pathology Initiatives and Experience of a Large Academic Institution During the Coronavirus Disease 2019 (COVID-19) Pandemic. Arch. Pathol. Lab. Med. 2021, 145, 1051–1061. [Google Scholar] [CrossRef] [PubMed]
- Nauhria, S.; Ramdass, P. Randomized cross-over study and a qualitative analysis comparing virtual microscopy and light microscopy for learning undergraduate histopathology. Indian J. Pathol. Microbiol. 2019, 62, 84–90. [Google Scholar] [CrossRef]
- Balseiro, A.; Pérez-Martínez, C.; de Paz, P.; García Iglesias, M.J. Evaluation of the COVID-19 Lockdown-Adapted Online Methodology for the Cytology and Histology Course as Part of the Degree in Veterinary Medicine. Vet. Sci. 2022, 9, 51. [Google Scholar] [CrossRef]
- Samueli, B.; Sror, N.; Jotkowitz, A.; Taragin, B. Remote pathology education during the COVID-19 era: Crisis converted to opportunity. Ann. Diagn. Pathol. 2020, 49, 151612. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-Fernandes, C.I.; Speight, P.M.; Khurram, S.A.; Araújo, A.L.D.; Perez, D.E.d.C.; Fonseca, F.P.; Lopes, M.A.; de Almeida, O.P.; Vargas, P.A.; Santos-Silva, A.R. The use of digital microscopy as a teaching method for human pathology: A systematic review. Virchows Arch. 2020, 477, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Mueen Ahmed, K.K.; Dhubaib, B.E.A. Zotero: A bibliographic assistant to researcher. J. Pharm. Pharm. 2022, 2, 304–305. [Google Scholar] [CrossRef]
- Luchini, C.; Stubbs, B.; Solmi, M.; Veronese, N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J. Meta-Anal. 2017, 5, 80–84. [Google Scholar] [CrossRef]
- Andrade, C. Mean Difference, Standardized Mean Difference (SMD), and Their Use in Meta-Analysis. J. Clin. Psychiatry 2020, 81, 20f13681. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar]
- Van Enst, W.A.; Ochodo, E.; Scholten, R.J.P.M.; Hooft, L.; Leeflang, M.M. Investigation of publication bias in meta-analyses of diagnostic test accuracy: A meta-epidemiological study. BMC Med. Res. Methodol. 2014, 14, 70. [Google Scholar] [CrossRef]
- Aperio ImageScope—Pathology Slide Viewing Software. Available online: https://www.leicabiosystems.com/digital-pathology/manage/aperio-imagescope/ (accessed on 14 December 2022).
- Waugh, S.; Devin, J.; Lam, A.K.-Y.; Gopalan, V. E-learning and the virtual transformation of histopathology teaching during COVID-19: Its impact on student learning experience and outcome. BMC Med. Educ. 2022, 22, 22. [Google Scholar] [CrossRef]
- Sakthi-Velavan, S.; Zahl, S. Integration of virtual microscopy podcasts in the histology discipline in osteopathic medical school: Learning outcomes. Anat. Sci. Educ. 2022, 16, 157–170. [Google Scholar] [CrossRef]
- Ahmed, S.; Habib, M.; Naveed, H.; Mudassir, G.; Bhatti, M.M.; Ahmad, R.N. Improving Medical Students’ Learning Experience of Pathology by Online Practical Sessions through Virtual Microscopy. J. Rawalpindi Med. Coll. 2022, 26, 122–127. [Google Scholar] [CrossRef]
- Qing, J.; Cheng, G.; Ni, X.-Q.; Yang, Y.; Zhang, W.; Li, Z. Implementation of an interactive virtual microscope laboratory system in teaching oral histopathology. Sci. Rep. 2022, 12, 5492. [Google Scholar] [CrossRef]
- Francis, D.V.; Charles, A.S.; Jacob, T.M.; Ruban, A.; Premkumar, P.S.; Rabi, S. Virtual microscopy as a teaching–learning tool for histology in a competency-based medical curriculum. Med. J. Armed India 2022. [Google Scholar] [CrossRef]
- Nikas, I.P.; Lamnisos, D.; Meletiou-Mavrotheris, M.; Themistocleous, S.C.; Pieridi, C.; Mytilinaios, D.G.; Michaelides, C.; Johnson, E.O. Shift to emergency remote preclinical medical education amidst the COVID-19 pandemic: A single-institution study. Anat. Sci. Educ. 2022, 15, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.; Sun, W.; Zhou, L.; Tang, M.; Zhang, W.; Xu, J.; Jiang, Y.; Liu, L.; Xu, Y. Application of remote online learning in oral histopathology teaching in China. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e533–e540. [Google Scholar] [CrossRef]
- Yakin, M.; Linden, K. Adaptive e-learning platforms can improve student performance and engagement in dental education. J. Dent. Educ. 2021, 85, 1309–1315. [Google Scholar] [CrossRef]
- Chang, J.Y.-F.; Lin, T.-C.; Wang, L.-H.; Cheng, F.-C.; Chiang, C.-P. Comparison of virtual microscopy and real microscopy for learning oral pathology laboratory course among dental students. J. Dent. Sci. 2021, 16, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Darici, D.; Reissner, C.; Brockhaus, J.; Missler, M. Implementation of a fully digital histology course in the anatomical teaching curriculum during COVID-19 pandemic. Ann. Anat.-Anat. Anz. 2021, 236, 151718. [Google Scholar] [CrossRef]
- Tanaka, K.S.; Ramachandran, R. Perceptions of a Remote Learning Pathology Elective for Advanced Clinical Medical Students. Acad. Pathol. 2021, 8, 23742895211006846. [Google Scholar] [CrossRef]
- Tauber, Z.; Lacey, H.; Lichnovska, R.; Erdosova, B.; Zizka, R.; Sedy, J.; Cizkova, K. Students’ preparedness, learning habits and the greatest difficulties in studying Histology in the digital era: A comparison between students of general and dental schools. Eur. J. Dent. Educ. 2020, 25, 371–376. [Google Scholar] [CrossRef]
- Guiter, G.E.; Sapia, S.; Wright, A.I.; Hutchins, G.G.A.; Arayssi, T. Development of a Remote Online Collaborative Medical School Pathology Curriculum with Clinical Correlations, across Several International Sites, through the COVID-19 Pandemic. Med. Sci. Educ. 2021, 31, 549–556. [Google Scholar] [CrossRef]
- Somera dos Santos, F.; Osako, M.K.; Perdoná, G.d.S.C.; Alves, M.G.; Sales, K.U. Virtual Microscopy as a Learning Tool in Brazilian Medical Education. Anat. Sci. Educ. 2021, 14, 408–416. [Google Scholar] [CrossRef]
- Cruz, M.; Murphy, M.; Gentile, M.M.; Stewart, K.; Barroeta, J.E.; Carrasco, G.A.; Kocher, W.D.; Behling, K.C. Assessment of Pathology Learning Modules With Virtual Microscopy in a Preclinical Medical School Curriculum. Am. J. Clin. Pathol. 2021, 156, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; King, T.S.; Hanson, E.R.; Fiebelkorn, K. Medical Histopathology Laboratories: Remote Teaching in Response to COVID-19 Pandemic. Acad. Pathol. 2021, 8, 2374289521998049. [Google Scholar] [CrossRef] [PubMed]
- White, M.J.; Birkness, J.E.; Salimian, K.J.; Meiss, A.E.; Butcher, M.; Davis, K.; Ware, A.D.; Zarella, M.D.; Lecksell, K.; Rooper, L.M.; et al. Continuing Undergraduate Pathology Medical Education in the Coronavirus Disease 2019 (COVID-19) Global Pandemic: The Johns Hopkins Virtual Surgical Pathology Clinical Elective. Arch. Pathol. Lab. Med. 2021, 145, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Lakhtakia, R. Virtual Microscopy in Undergraduate Pathology Education. Sultan Qaboos Univ. Med. J. SQUMJ 2021, 21, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Sun, W.; Du, C.; Yang, L.; Yuan, N.; Cui, H.; Song, W.; Ge, L. Medical Morphology Training Using the Xuexi Tong Platform During the COVID-19 Pandemic: Development and Validation of a Web-Based Teaching Approach. JMIR Med. Inform. 2021, 9, e24497. [Google Scholar] [CrossRef]
- Simok, A.A.; Kasim, F.; Hadie, S.N.H.; Abdul Manan@Sulong, H.; Yusoff, M.S.B.; Mohd Noor, N.F.; Asari, M.A. Knowledge Acquisition and Satisfaction of Virtual Microscopy Usage Among Medical Students of Universiti Sains Malaysia. Educ. Med. J. 2021, 13, 43–55. [Google Scholar] [CrossRef]
- Manou, E.; Lazari, E.-C.; Thomopoulou, G.-E.; Agrogiannis, G.; Kavantzas, N.; Lazaris, A.C. Participation and Interactivity in Synchronous E-Learning Pathology Course During the COVID-19 Pandemic. Adv. Med. Educ. Pract. 2021, 12, 1081–1091. [Google Scholar] [CrossRef]
- Laohawetwanit, T. The use of virtual pathology in teaching medical students: First experience of a medical school in Thailand. MedEdPublish 2020, 9, 116. [Google Scholar] [CrossRef]
- Uraiby, H.; Grafton-Clarke, C.; Gordon, M.; Sereno, M.; Powell, B.; McCarthy, M. Fostering intrinsic motivation in remote undergraduate histopathology education. J. Clin. Pathol. 2021, 75, 837–843. [Google Scholar] [CrossRef]
- Ali, S.A.A.; Syed, S. Teaching and Learning Strategies of Oral Histology Among Dental Students. Int. J. Morphol. 2020, 38, 634–639. [Google Scholar] [CrossRef]
- Parker, E.U.; Chang, O.; Koch, L. Remote Anatomic Pathology Medical Student Education in Washington State. Am. J. Clin. Pathol. 2020, 154, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Dennis, J.F. The HistoHustle: Supplemental Histology Sessions to Enrich Student Learning and Self-Efficacy. Med. Sci. Educ. 2020, 30, 1725–1726. [Google Scholar] [CrossRef] [PubMed]
- Bacha, D.; Ferjaoui, W.; Charfi, L.; Rejaibi, S.; Gharbi, L.; ben Slama, S.; Njim, L.; Lahmar, A. The interest of virtual microscopy as a means of simulation learning in pathological anatomy and cytology. Oncol. Radiother. 2020, 14, 23–29. [Google Scholar]
- Lee, B.C.; Hsieh, S.T.; Chang, Y.L.; Tseng, F.Y.; Lin, Y.J.; Chen, Y.L.; Wang, S.H.; Chang, Y.F.; Ho, Y.L.; Ni, Y.H.; et al. A Web-Based Virtual Microscopy Platform for Improving Academic Performance in Histology and Pathology Laboratory Courses: A Pilot Study. Anat. Sci. Educ. 2020, 13, 743–758. [Google Scholar] [CrossRef] [PubMed]
- Amer, M.; Nemenqani, D. Successful use of virtual microscopy in the assessment of practical histology during pandemic COVID-19: A descriptive study. J. Microsc. Ultrastruct. 2020, 8, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Romeike, B.F.M.; Fischer, M. Buzz groups facilitate collaborative learning and improve histopathological competencies of students. Clin. Neuropathol. 2019, 38, 285–293. [Google Scholar] [CrossRef]
- King, T.S.; Sharma, R.; Jackson, J.; Fiebelkorn, K.R. Clinical Case-Based Image Portfolios in Medical Histopathology. Anat. Sci. Educ. 2019, 12, 200–209. [Google Scholar] [CrossRef]
- Husmann, P.R.; O’Loughlin, V.D. Another Nail in the Coffin for Learning Styles? Disparities among Undergraduate Anatomy Students’ Study Strategies, Class Performance, and Reported VARK Learning Styles. Anat. Sci. Educ. 2019, 12, 6–19. [Google Scholar] [CrossRef]
- Yohannan, D.G.; Oommen, A.M.; Umesan, K.G.; Raveendran, V.L.; Sreedhar, L.S.L.; Anish, T.S.N.; Hortsch, M.; Krishnapillai, R. Overcoming Barriers in a Traditional Medical Education System by the Stepwise, Evidence-Based Introduction of a Modern Learning Technology. Med. Sci. Educ. 2019, 29, 803–817. [Google Scholar] [CrossRef]
- Chen, C.P.; Clifford, B.M.; O’Leary, M.J.; Hartman, D.J.; Picarsic, J.L. Improving Medical Students’ Understanding of Pediatric Diseases through an Innovative and Tailored Web-based Digital Pathology Program with Philips Pathology Tutor (Formerly PathXL). J. Pathol. Inform. 2019, 10, 18. [Google Scholar] [CrossRef]
- Tauber, Z.; Cizkova, K.; Lichnovska, R.; Lacey, H.; Erdosova, B.; Zizka, R.; Kamarad, V. Evaluation of the effectiveness of the presentation of virtual histology slides by students during classes. Are there any differences in approach between dentistry and general medicine students? Eur. J. Dent. Educ. 2019, 23, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Felszeghy, S.; Pasonen-Seppänen, S.; Koskela, A.; Nieminen, P.; Härkönen, K.; Paldanius, K.M.A.; Gabbouj, S.; Ketola, K.; Hiltunen, M.; Lundin, M.; et al. Using online game-based platforms to improve student performance and engagement in histology teaching. BMC Med. Educ. 2019, 19, 273. [Google Scholar] [CrossRef] [PubMed]
- Yazid, F.; Ghazali, N.; Rosli, M.S.A.; Apandi, N.I.M.; Ibrahim, N. The Use of Digital Microscope in Oral Pathology Teaching. J. Int. Dent. Med. Res. 2019, 12, 1095–1099. [Google Scholar]
- Lionetti, K.A.; Townsend, H. Teaching Microscopy Remotely: Two Engaging Options. J. Microbiol. Biol. Educ. 2022, 23, 1–3. [Google Scholar] [CrossRef]
- Clarke, E.; Doherty, D.; Randell, R.; Grek, J.; Thomas, R.; Ruddle, R.A.; Treanor, D. Faster than light (microscopy): Superiority of digital pathology over microscopy for assessment of immunohistochemistry. J. Clin. Pathol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Samuelson, M.I.; Chen, S.J.; Boukhar, S.A.; Schnieders, E.M.; Walhof, M.L.; Bellizzi, A.M.; Robinson, R.A.; Rajan, K.D.A. Rapid Validation of Whole-Slide Imaging for Primary Histopathology Diagnosis. Am. J. Clin. Pathol. 2021, 155, 638–648. [Google Scholar] [CrossRef]
- Liscia, D.S.; Bellis, D.; Biletta, E.; D’Andrea, M.; Croci, G.A.; Dianzani, U. Whole-Slide Imaging Allows Pathologists to Work Remotely in Regions with Severe Logistical Constraints Due to COVID-19 Pandemic. J. Pathol. Inform. 2020, 11, 20. [Google Scholar] [CrossRef]
- Blum, A.E.; Murphy, G.F.; Lee, J.J. Digital dermatopathology: The time is now. J. Cutan. Pathol. 2021, 48, 469–471. [Google Scholar] [CrossRef] [PubMed]
- Alassiri, A.; Almutrafi, A.; Alsufiani, F.; Al Nehkilan, A.; Al Salim, A.; Musleh, H.; Aziz, M.; Khalbuss, W. Whole slide imaging compared with light microscopy for primary diagnosis in surgical neuropathology: A validation study. Ann. Saudi Med. 2020, 40, 36–41. [Google Scholar] [CrossRef]
- Ammendola, S.; Bariani, E.; Eccher, A.; Capitanio, A.; Ghimenton, C.; Pantanowitz, L.; Parwani, A.; Girolami, I.; Scarpa, A.; Barresi, V. The histopathological diagnosis of atypical meningioma: Glass slide versus whole slide imaging for grading assessment. Virchows Arch. 2020, 478, 747–756. [Google Scholar] [CrossRef]
- Babawale, M.; Gunavardhan, A.; Walker, J.; Corfield, T.; Huey, P.; Savage, A.; Bansal, A.; Atkinson, M.; Abdelsalam, H.; Raweily, E.; et al. Verification and Validation of Digital Pathology (Whole Slide Imaging) for Primary Histopathological Diagnosis: All Wales Experience. J. Pathol. Inform. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Borowsky, A.D.; Glassy, E.F.; Wallace, W.D.; Kallichanda, N.S.; Behling, C.A.; Miller, D.V.; Oswal, H.N.; Feddersen, R.M.; Bakhtar, O.R.; Mendoza, A.E.; et al. Digital Whole Slide Imaging Compared With Light Microscopy for Primary Diagnosis in Surgical Pathology. Arch. Pathol. Lab. Med. 2020, 144, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Lam, A.K.; Leung, M. Whole-Slide Imaging for Esophageal Adenocarcinoma. In Esophageal Adenocarcinoma; Methods in Molecular Biology; Springer: Berlin/Heidelberg, Germany, 2018; pp. 135–142. [Google Scholar]
- Wang, C.; Wei, X.-L.; Li, C.-X.; Wang, Y.-Z.; Wu, Y.; Niu, Y.-X.; Zhang, C.; Yu, Y. Efficient and Highly Accurate Diagnosis of Malignant Hematological Diseases Based on Whole-Slide Images Using Deep Learning. Front. Oncol. 2022, 12, 879308. [Google Scholar] [CrossRef] [PubMed]
- Niazi, M.K.K.; Parwani, A.V.; Gurcan, M.N. Digital pathology and artificial intelligence. Lancet Oncol. 2019, 20, e253–e261. [Google Scholar] [CrossRef] [PubMed]
- Frazier, P.I.; Cashore, J.M.; Duan, N.; Henderson, S.G.; Janmohamed, A.; Liu, B.; Shmoys, D.B.; Wan, J.; Zhang, Y. Modeling for COVID-19 college reopening decisions: Cornell, a case study. Proc. Natl. Acad. Sci. USA 2022, 119, e2112532119. [Google Scholar] [CrossRef] [PubMed]
- Van Gaalen, A.E.J.; Brouwer, J.; Schönrock-Adema, J.; Bouwkamp-Timmer, T.; Jaarsma, A.D.C.; Georgiadis, J.R. Gamification of health professions education: A systematic review. Adv. Health Sci. Educ. 2020, 26, 683–711. [Google Scholar] [CrossRef]
- Bai, S.; Hew, K.F.; Gonda, D.E.; Huang, B.; Liang, X. Incorporating fantasy into gamification promotes student learning and quality of online interaction. Int. J. Educ. Technol. High. Educ. 2022, 19, 29. [Google Scholar] [CrossRef]
- Roth, J.; Chang, A.; Ricci, B.; Hall, M.; Mehta, N. Why Not a Podcast? Assessing Narrative Audio and Written Curricula in Obstetrical Neurology. J. Grad. Med. Educ. 2020, 12, 86–91. [Google Scholar] [CrossRef]
- Biolucida. Available online: https://www.mbfbioscience.com/biolucida (accessed on 14 December 2022).
- University of Michigan Virtual Slide Box. Available online: https://www.pathology.med.umich.edu/apps/slides/ (accessed on 14 December 2022).
- Virtual Pathology at the University of Leeds. Available online: https://www.virtualpathology.leeds.ac.uk/ (accessed on 10 October 2022).
- The Milestones Guidebook. Available online: https://www.acgme.org/globalassets/MilestonesGuidebook.pdf (accessed on 25 December 2021).
- Standards, Publications, & Notification Forms. Available online: https://lcme.org/publications/ (accessed on 10 January 2021).
- Hassell, L.A.; Fung, K.-M.; Chaser, B. Digital slides and ACGME resident competencies in anatomic pathology: An altered paradigm for acquisition and assessment. J. Pathol. Inform. 2011, 2, 27. [Google Scholar] [CrossRef]

| Author and Year | University and Location | Course Subject/Medical or Dental | Study Design | Total Participants | VM Setup Used | Conclusion/Results |
|---|---|---|---|---|---|---|
| Waugh S, 2022 [31] | Griffith University, Australia | Histopathology, medical students | Observational case–control study | 150 | BEST slice cloud-based library | A thematic analysis of the qualitative comments strongly indicated that online histopathology teaching was instrumental, more comfortable to engage in and better structured compared to face-to-face teaching. Compared to the prior cohort completing the same curriculum the mean overall mark was significantly improved. |
| Sakthi-Velavan S, 2022 [32] | Marian University College of Osteopathic Medicine, USA | Histology, medical students | Observational case–control study | 477 | VM podcast | Most students indicated that the podcasts enabled more efficient study time and improved their confidence in the histology content on examinations. A summary of students’ feedback and academic performance supported that integration of the VMPs into Histology teaching improved the learning experience. The findings align with previous studies on the effectiveness of multimedia-based teaching in histology laboratory modules. There was a significant difference between the average histology performance of earlier classes that did not have access to the VMPs versus the average performance of the classes that had access to the VMPs. |
| Ahmed S, 2022 [33] | Shifa College of Medicine, Pakistan | Pathology, 3rd-year medical students | Randomized crossover control study | 111 | Not specified | Evidence showed that the microscopic practical skills achieved by virtual microscopy are comparable to or even better than those achieved by light microscopy. |
| Qing J, 2022 [34] | Wuhan University, China | Histopathology, dental students | Observational case–control study | 156 | NanoZoomer Digital Pathology sofware | Study compared results of assignments and exams between VM group and LM group and a questionnaire survey was used to collect feedback. Results showed an increase laboratory final test grades increased and the feedback of the questionnaire was positive, indicating that students were satisfied with the system. This study concluded that VM is an efficient and feasible teaching technology and improves students’ academic performance. |
| Francis DV, 2022 [35] | Christian Medical College, Vellore, India | Histology, medical students | Observational case–control study | 100 (cohort one), 99 (cohort 2) | VM software-Open Microscopy Environment Remote Objects (OMERO), University of Dundee, UK. WSI scanner-Digiscan (https://digiscan.co.in/) | Majority students were reported to be enthusiastic about using VM. Some of the benefits of VM as cited by the students were the ease of usage, annotations, the superior quality of images, accessibility to slides outside of lab time, in class internet access to additional learning material, promotion of self-learning and efficient use of their study time. Performance score analysis showed a statistically significant improvement of grades in the VM arm. |
| Nikas IP, 2021 [36] | School of Medicine, European University, Cyprus | Histology and pathology, medical students | Cross-sectional surveys | 173 | Websites e.g., Michigan Histology and Virtual Microscopy Learning Resources | Both histology and pathology online delivery was well-accepted by most medical students. Pathology students and students with high final examination scores perceived their virtual education more favorably. |
| Zhong Y, 2021 [37] | Nanjing Medical University, China | Histopathology, dental students | Comparative cross-sectional | 192 | NanoZoomer Digital Pathology | The mean scores of the online group (VM) were significantly higher than those of the traditional group (LM). Furthermore, both remote learning and virtual microscopy courses were well accepted by students according to the questionnaire. |
| Yakin M, 2021 [38] | Adelaide Dental School, University of Adelaide, Australia | Histology, year 1 and year 3, dental students | Comparative prospective cohort study | 43 | Biomedical Education Skills and Training network (www.best.edu.au) | Students obtained significantly higher scores in experimental exam questions than control exam questions. A significantly larger number of students perceived that the adaptive lessons improved their knowledge of the subject. |
| Chang JYF, 2021 [39] | National Taiwan University, Taiwan | Oral pathology, dental students | Comparative cross-sectional | 38 | Dot-slide system developed by Soft Imaging System GmbH (Olympus Deutschland GmbH, Hamburg, Germany) | Results showed a significantly higher acceptance rate and a significantly better histopathological diagnosis ability among dental students using the virtual slide learning than those using the glass-slide learning for the oral pathology laboratory course.VM with digitized virtual slides may gradually replace the real microscopy with glass slides for the learning of oral pathology laboratory course. |
| Darici D, 2021 [40] | Westfälische-Wilhelms-University, Germany | Histology, preclinical medical students | Cross-sectional cohort study | 400 | Custom histology software-Virtuelle Mikroskopie | The study concluded that the implementation of a curricular histology course in an online-format is technically realizable, effective and well accepted among students. The study also reported that availability and prior experience with digitized specimen in VM facilitates transition into an online-only setting. |
| Tanaka KS, 2021 [41] | University of California, USA | Pathology, fourth year medical students | Cross-sectional cohort study | 37 | Custom UCSF digital library | End-of-rotation data showed the remote pathology course performed well when compared to the traditional in-person pathology elective. Core strengths highlighted in this study include a high educational value, flexibility of content and schedule, organization, tailoring to an individual’s learning goals and a positive education environment. Drawbacks were the inability to gross surgical specimens, inadequate observation or feedback about students’ skills, and impaired social connections. |
| Tauber Z, 2021 [42] | Palacky University, Czech Republic | Histology, dental students | Structured questionnaire | 82 Dentistry, 192 General medicine | Not mentioned | All students in this study indicated that they prefer the use of VM or the combination of VM together with the examination of glass mounted specimens by microscope. |
| Guiter GE, 2021 [43] | Weill Cornell Medicine, Qatar | Pathology, medical students | Cross-sectional surveys | 29 | University of Leeds’ Virtual Pathology Library | Students conveyed high levels of satisfaction about the elective’s overall quality, their pathology learning and online interactions, with minimal challenges related to the remote nature of the course. |
| Somera dos Santos F, 2021 [44] | Ribeirao Preto Medical School, Brazil | Histology, medical students | Cross-sectional Cohort study | 189 | NanoZoomer S60 digital whole slide scanner | The study reported positive subjective feedback related to handling, suitability, learning effectiveness, and pleasure using the tools for VM. Although no statistically significant differences were found between groups for academic performance, VM proved to be adequate to the Brazilian medical education in light of Brazilian social contexts and COVID-19 pandemic. |
| Cruz M, 2021 [45] | Cooper Medical School of Rowan University, USA | Pathology, medical students | Comparative cross-sectional | 44 | Web-basedprogram (Aperio) | VM could help first- and second-year medical students understand case-based scenarios and clinical pathology more deeply than photomicrographs, particularly with direct faculty support for navigating virtual slides. Participation in and completion of pathology-VM learning modules enhances student learning of pathology-related topics. |
| Sharma R, 2021 [46] | School of Medicine, University of Texas Health San Antonio, USA | Histopathology, medical students | Cross-sectional cohort study | 215 (MS1); 207 (MS2) | Not specified | Majority students agreed that the VM helped in their learning. Students performed better in module examinations in 2020 than in the previous years. |
| White MJ, 2021 [47] | Johns Hopkins University, USA | Pathology, medical students | Cross-sectional surveys | 43 | Leica Aperio AT and Roche iScan HT | Most students provided positive objective feedback related to VM use. |
| Lakhtakia R, 2021 [48] | Mohammed Bin Rashid University of Medicine and Health Sciences, UAE | Pathology, medical students | Cross-sectional surveys | 49 | Cirdan PathXL Tutor, Lisburn, Ireland | VM usage was reported as a user-friendly resource that helped students develop a strong clinical foundation and clinico-pathological correlation. High student attendance and improved assessment scores on critical thinking were observed. Easy access was a significant student-centric advantage reported by this study. |
| Liu Q, 2021 [49] | Shandong First Medical University, China | Histology, embryology and pathology, medical students | Observational case–control study | 512 | Medical Morphology Digital Teaching System | With regard to the teaching performance of VM based teaching, students demonstrated a high degree of satisfaction. Majority students achieved high scores in the web-based learning group than in the offline learning control group. |
| Simok AA, 2021 [50] | Universiti Sains, Malaysia | Histology, medical students | Randomized control study | 120 | Pannoramic viewer VM software by 3DHISTECH Ltd. | The VM group had a significantly higher satisfaction score towards the learning tool than the LM group. The knowledge acquisition of the VM group was equal to the LM group as they were shown to have a similar improvement in the test scores, comprehension level and learning ability. The study revealed a significant improvement in test scores for VM. |
| Manou E, 2021 [51] | National and Kapodistrian University of Athens, Greece | Pathology, medical students | Observational cohort study | 91 | e-learning platform HIPON (HistoPathology Online) | The study concluded that further research to enhance understanding of the aspects of the e-learning environment towards the formulation of policies for higher-quality education is needed. |
| Laohawetwanit T, 2021 [52] | Thammasat University, Thailand | Pathology, second year medical students | Observational case–control study | 29 | PathPresenter | There was a significant improvement between student pre-test scores and post-test scores. VM was viewed as a preferred learning modality, mainly because of its portability, satisfactory quality of images, permitting learning in less time, and stimulating cooperation between students while improving interaction with teachers. |
| Uraiby H, 2021 [53] | University Hospitals of Leicester, UK | Histopathology, medical students | Cross-sectional surveys | 90 | VM software-Philips Xplore, WSI scanner-Hamamatsu NanoZoomer S210 | Study showed a significant improvement in interest, confidence and competence in histopathology. The mean performance scores were significantly increased. |
| Ali SAA, 2020 [54] | King Khalid University, Saudi Arabia | Histology, dental students | Cross-sectional surveys | 129 | Not specified | Majority students reported that using VM for practical training sessions makes the oral histology course easier and more interesting. |
| Samueli B, 2020 [22] | Ben Gurion University of the Negev, Israel | Pathology, medical students | Cross-sectional surveys | 59 | VM software-CaseViewer (3DHistech, Budapest) and Aperio ImageScope (Leica, Illinois). WSI scanner-Pannoramic MIDI automated digital slide scanner (3DHistech, Budapest). | Study reported an overall favorable response on questions relating to course interest and improvement in understanding of the covered diseases. The most significant disadvantage was technical challenges in accessing the slides. |
| Parker EU, 2020 [55] | University of Washington School of Medicine, USA | Pathology, medical students | Structured questionnaire survey | 70 | PathPresenter | The study reported an overwhelmingly positive result regarding understanding of pathology concepts as well as attitudes toward pathology. |
| Dennis JF, 2020 [56] | Kansas City University, USA | Histology and pathology, medical students | Cross-sectional surveys | 200 | Virtual Microscopy Database (VMD) | VM use improved student attitudes towards histology content and had a positive impact on student-faculty rapport. Students self-reporting an increased comfortability and understanding with differential diagnosis suggested a strengthening of self-efficacy skills. |
| Bacha D, 2020 [57] | University of Tunis El Manar, Tunisia | Pathology, medical students | Observational cohort study | 45 | Not specified | This study reported that performance of the VM is comparable to that of the LM. Thus, VM could serve as an alternative tool to LM in teaching students’ general pathological anatomy. |
| Lee BC, 2020 [58] | National Taiwan University, Taiwan | Histology and pathology, medical and dental students | Observational case–control study | 649 | EBM Technologies Inc., Taiwan | The study reported a positive effect of the VM platform on laboratory test Grades was associated with prior experience using the VM platform and was synergistic with more interim tests. Both teachers and students agreed that the VM platform enhanced laboratory learning. The incorporation of the VM platform in the context of test-enhanced learning may help more students master microscopic laboratory content. |
| Amer MG, 2020 [59] | Taif University, Saudi Arabia | Histology, medical students | Cross-sectional surveys | 166 | VM software-Aperio’s ImageScope. WSI scanner-Aperio AT2 High Volume (Leica Biosystems). | The study used VM during online objective structural practical examination (OSPE) of 3rd year medical students. The net students feedback was positive and the students recorded the easy image access at any time and place with VM as the most distinctive feature. |
| Romeike BFM, 2019 [60] | Jena University Hospital, Germany | Histopathology, medical students | Observational case–control study | 140 | Not specified | This study reported impact of VM use in collaborative “buzz groups’ and showed an overall improvement of the histopathological competencies. The course also increased the appreciation of students for histopathology. |
| King TS, 2019 [61] | UT-Health, San Antonio, USA | Histology and pathology, medical students | Observational case–control study | 220 | VM software-Biolucida (MicroBrightField Bioscience). WSI scanner-BLiSSTM-200 (MicroBrightField Bioscience) | The study concluded that VM promoted understanding and encouraged discussion of the topics covered during the week and that group members worked well together and contributed to the completion of the portfolios. Performances on the Histology and Cell Biology and Pathology sections on the United States Medical Licensing Examination (USMLE) remained consistent and in line with national averages. |
| Husmann PR, 2019 [62] | Indiana University School of Medicine, Indiana, USA | Anatomy, medical students | Cross-sectional surveys | 426 | Bacus Laboratories (Olympus, 2008) | Statistically significant positive correlations were found with use of VM suggesting that increased use of these resources was more common in students with higher exam scores in the class. |
| Yohannan DG, 2019 [63] | Government Medical College, Thiruvananthapuram, India | Histopathology, first year medical students | Nonrandomized controlled trial with a crossover design | 200 | VM software-Aperio’s ImageScope | Majority students agreed that VM made them understand histology better than LM. Almost 90% students agreed that they preferred VM for viewing a histology slide. A paired t test indicated that the histology knowledge of the students of both control and test groups significantly improved. |
| Chen CP, 2019 [64] | University of Pittsburgh School of Medicine, USA | Pathology, medical students | Observational case–control study | 123 control group and 164 test group | Tutor (Philips Pathology, Amsterdam, Netherlands), formerly PathXL | The majority students responded positively that the test questions improved their understanding of pediatric diseases (75%) and test questions were helpful in assessing their knowledge of the pediatric pathology (90%), and relative ease of use for the Tutor program (80%). |
| Nauhria S, 2019 [20] | Windsor University School of Medicine, St. Kitts and Nevis | Pathology, second year medical students | Randomized crossover control study | 152 | VM software-Aperio’s ImageScope. WSI-IOWA Virtual Slide Box | A majority (83%) of the students preferred to use VM over LM. Students who used VM scored significantly higher in the crossover study compared to those who used LM. This study concluded that using VM to learn histopathology significantly increased student learning and performance compared to using LM. |
| Tauber Z, 2019 [65] | Palacky University, Czech Republic | Histology, dentistry and general medicine students | Observational case–control study | 82 dentistry and 126 general medicine students | Not specified | This study reported that a combination of both electronic materials (VM) and textbooks was commonly used by students with electronic resources being used regularly by the majority of students. No statistically relevant differences were found between the approaches of dentistry versus general medicine students. Cooperation amongst students for individual presentations was seen to be beneficial by a majority of dentistry students. |
| Felszeghy S, 2019 [66] | University of Eastern Finland, Finland | Histology, medical and dental students | Cross-sectional surveys | 160 | Whole-slide imaging platform (Aiforia, Fimmic Oy, Finland). | In the open-ended survey, most students viewed collaborative team- and gamification-based learning positively. |
| Yazid F, 2019 [67] | Universiti Kebangsaan Malaysia, Malaysia | Oral pathology, fourth year dentistry students | Observational case–control study | 53 | VM software-OlyVIA viewer. WSI-Precipoint M8 microscopescanner. | A majority of students preferred VM over LM and agreed that DM was effective for the course purpose. For the diagnosis exercise, all participants managed to answer correctly using VM compared to LM. Thus, indicating that VM should certainly be integrated as a teaching tool to enhance the learning process within the dental curriculum. |
| Selection | Comparability | Outcomes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Representation of Sample | Selection of the Non-Exposed Cohort | Ascertainment of Exposure | Demonstration That Outcome of Interest was not Present at Start of Study | Comparability of Cohorts on the Basis of the Design or Analysis Controlled for Confounders | Assessment of Outcome | Was Follow-up Long Enough for Outcomes to Occur | Adequacy of Follow-up of Cohorts | ||||||
| Truly representative | Somewhat representative | Drawn from the same community as the exposed cohort | Drawn from a different source | Secure record (e.g., surgical record) | Structured interview | Yes | The study controls for age, sex and marital status | Study controls for other factors | Independent blind assessment | Record linkage | Yes | Complete follow up- all subject accounted for | Subjects lost to follow-up unlikely to introduce bias; number lost less than or equal to 20% or description of those lost suggested no different from those followed | |
| Darici D, 2021 [40] | * | * | * | * | * | * | ||||||||
| Tauber Z, 2021 [42] | * | * | * | * | * | |||||||||
| Somera dos Santos F, 2021 [44] | * | * | * | * | * | * | * | |||||||
| Cruz M, 2021 [45] | * | * | * | * | * | * | * | * | ||||||
| Sharma R, 2021 [46] | * | * | * | * | * | |||||||||
| Liu Q, 2021 [49] | * | * | * | * | * | * | * | |||||||
| Lee BC, 2020 [58] | * | * | * | * | * | * | * | * | ||||||
| Yohannan DG, 2019 [63] | * | * | * | * | * | * | * | * | ||||||
| Sakthi-Velavan S, 2022 [32] | * | * | * | * | * | * | * | |||||||
| Author, Year | Selection | Comparability | Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Representation | Sample Size Justified | Non-Respondents | Ascertainment of the Exposure | Important Confounding Factors Controlled | Study Control for any Additional Factors | Outcome Assessment | Statistical Test | ||||
| All Subjects/Random Sampling | Non-Random Sampling | Validated Measurement Tool. ** | Non-Validated Measurement Tool, but the Tool is Available or Described. * | Independent Blind Assessment/Record Linkage. ** | Self-Report * | ||||||
| Nikas IP, 2021 [36] | * | ** | ** | * | |||||||
| Chang JYF, 2021 [39] | * | * | ** | * | |||||||
| Tanaka KS, 2021 [41] | * | * | * | * | |||||||
| Guiter GE, 2021 [43] | * | * | * | * | |||||||
| White MJ, 2021 [47] | * | * | * | ||||||||
| Yakin M, 2021 [38] | * | * | |||||||||
| Lakhtakia R, 2021 [48] | * | * | |||||||||
| Uraiby H, 2021 [53] | * | ||||||||||
| Samueli B, 2020 [22] | * | * | |||||||||
| Bacha D, 2020 [57] | * | * | * | ||||||||
| Amer M, 2020 [59] | * | * | ** | * | ** | * | |||||
| Ali SAA, 2020 [54] | * | * | * | * | |||||||
| Romeike BFM, 2019 [60] | * | * | * | ** | * | ** | * | ||||
| Tauber Z, 2019 [65] | * | * | * | ||||||||
| King TS, 2019 [61] | * | * | ** | * | |||||||
| Husmann PR, 2019 [62] | |||||||||||
| Felszeghy S, 2019 [66] | * | * | * | * | ** | ||||||
| Manou E, 2021 [51] | * | * | |||||||||
| Yazid F, 2019 [67] | |||||||||||
| Laohawetwanit T, 2021 [52] | * | * | * | ** | |||||||
| Author, Year | Selection | Comparability | Exposure | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Adequate Case Definition | Case Representativeness | Selection of Control | Definition of Control | Important Study Control | Study Controls for any Additional Factors | Ascertainment of Exposure | Same Method of Ascertainment for Cases and Controls | Non-Response Rate | |
| Nauhria S, 2019 [20] | * | * | * | * | * | * | * | * | |
| Simok, A.A. 2021 [50] | * | * | * | * | * | * | * | * | |
| Ahmed S, 2022 [33] | * | * | * | * | * | * | |||
| Author, Year | Selection | Comparability | Exposure | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Adequate Case Definition (Yes, with Independent Validation) | Case representativeness (Consecutive or Obviously Representative Series of Cases) | Selection of Control (Community Controls) | Definition of Control: no History of Disease (Endpoint) | Important Study Control | Study Control for any Additional Factors | Ascertainment of Exposure | Same Method of Ascertainment for Cases and Controls | Non-Response Rate | |
| Waugh S, 2022 [31] | * | * | * | * | * | * | |||
| Zhong Y, 2021 [37] | * | * | * | * | * | * | |||
| Chen CP, 2019 [64] | * | * | * | * | * | * | |||
| Sakthi-Velavan S, 2022 [32] | |||||||||
| Yazid F, 2019 [67] | * | * | * | * | * | ||||
| Qing J, 2022 [34] | * | * | * | * | * | * | * | ||
| Francis DV, 2022 [35] | * | * | * | * | * | * | * | * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maity, S.; Nauhria, S.; Nayak, N.; Nauhria, S.; Coffin, T.; Wray, J.; Haerianardakani, S.; Sah, R.; Spruce, A.; Jeong, Y.; et al. Virtual Versus Light Microscopy Usage among Students: A Systematic Review and Meta-Analytic Evidence in Medical Education. Diagnostics 2023, 13, 558. https://doi.org/10.3390/diagnostics13030558
Maity S, Nauhria S, Nayak N, Nauhria S, Coffin T, Wray J, Haerianardakani S, Sah R, Spruce A, Jeong Y, et al. Virtual Versus Light Microscopy Usage among Students: A Systematic Review and Meta-Analytic Evidence in Medical Education. Diagnostics. 2023; 13(3):558. https://doi.org/10.3390/diagnostics13030558
Chicago/Turabian StyleMaity, Sabyasachi, Samal Nauhria, Narendra Nayak, Shreya Nauhria, Tamara Coffin, Jadzia Wray, Sepehr Haerianardakani, Ramsagar Sah, Andrew Spruce, Yujin Jeong, and et al. 2023. "Virtual Versus Light Microscopy Usage among Students: A Systematic Review and Meta-Analytic Evidence in Medical Education" Diagnostics 13, no. 3: 558. https://doi.org/10.3390/diagnostics13030558
APA StyleMaity, S., Nauhria, S., Nayak, N., Nauhria, S., Coffin, T., Wray, J., Haerianardakani, S., Sah, R., Spruce, A., Jeong, Y., Maj, M. C., Sharma, A., Okpara, N., Ike, C. J., Nath, R., Nelson, J., & Parwani, A. V. (2023). Virtual Versus Light Microscopy Usage among Students: A Systematic Review and Meta-Analytic Evidence in Medical Education. Diagnostics, 13(3), 558. https://doi.org/10.3390/diagnostics13030558







