Development of an Imaging Technique for Boron Neutron Capture Therapy
Abstract
:1. Introduction
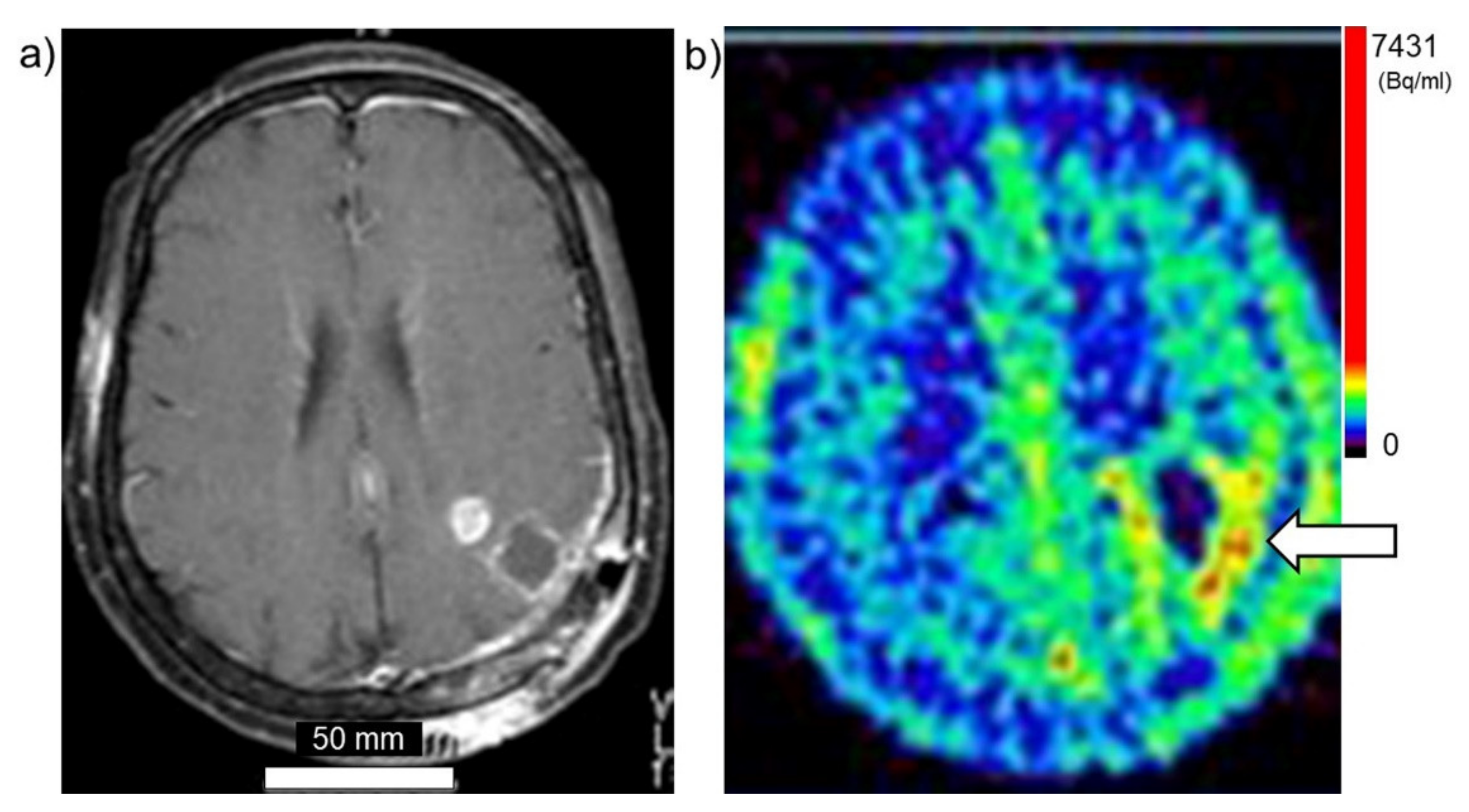
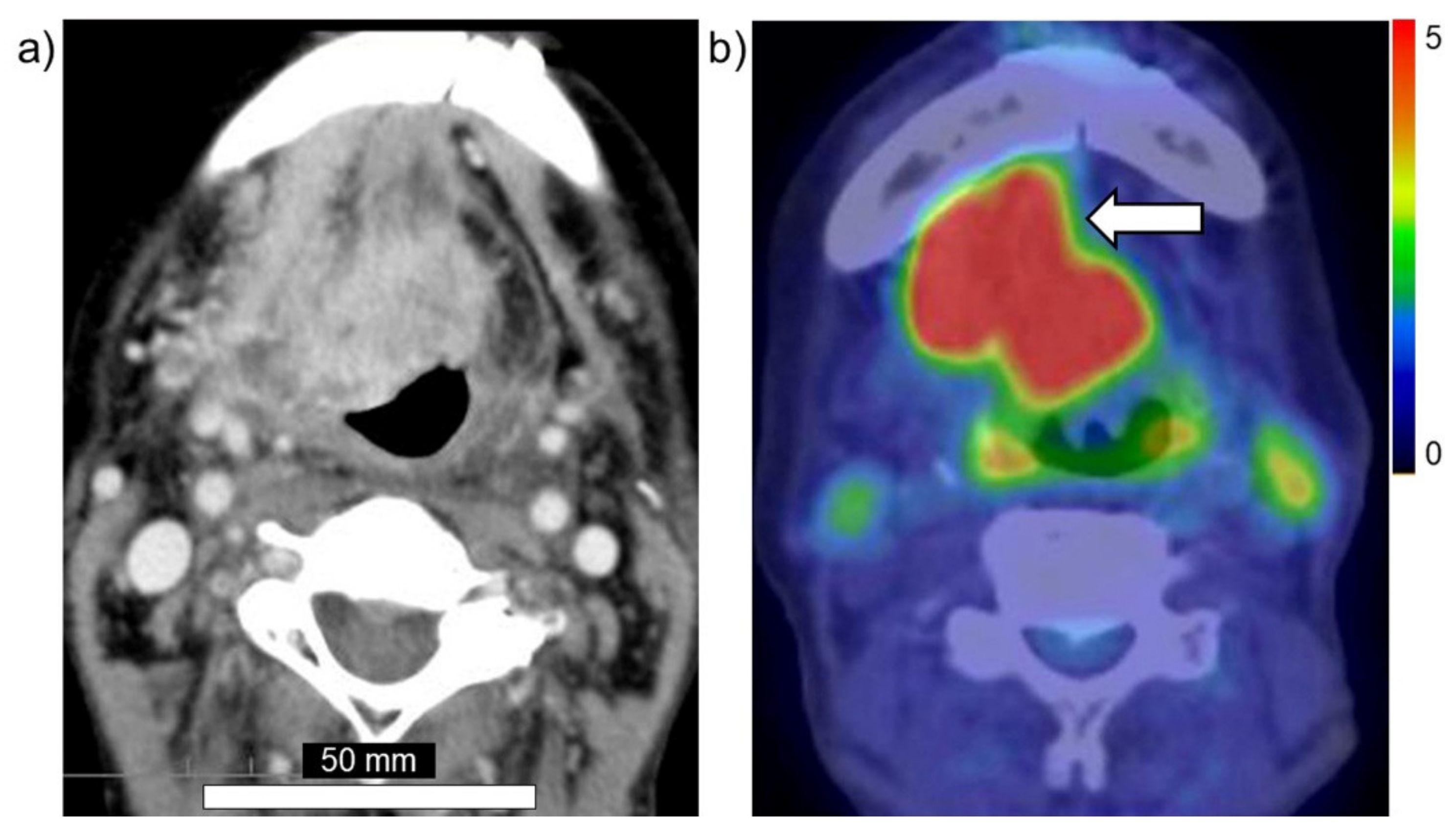
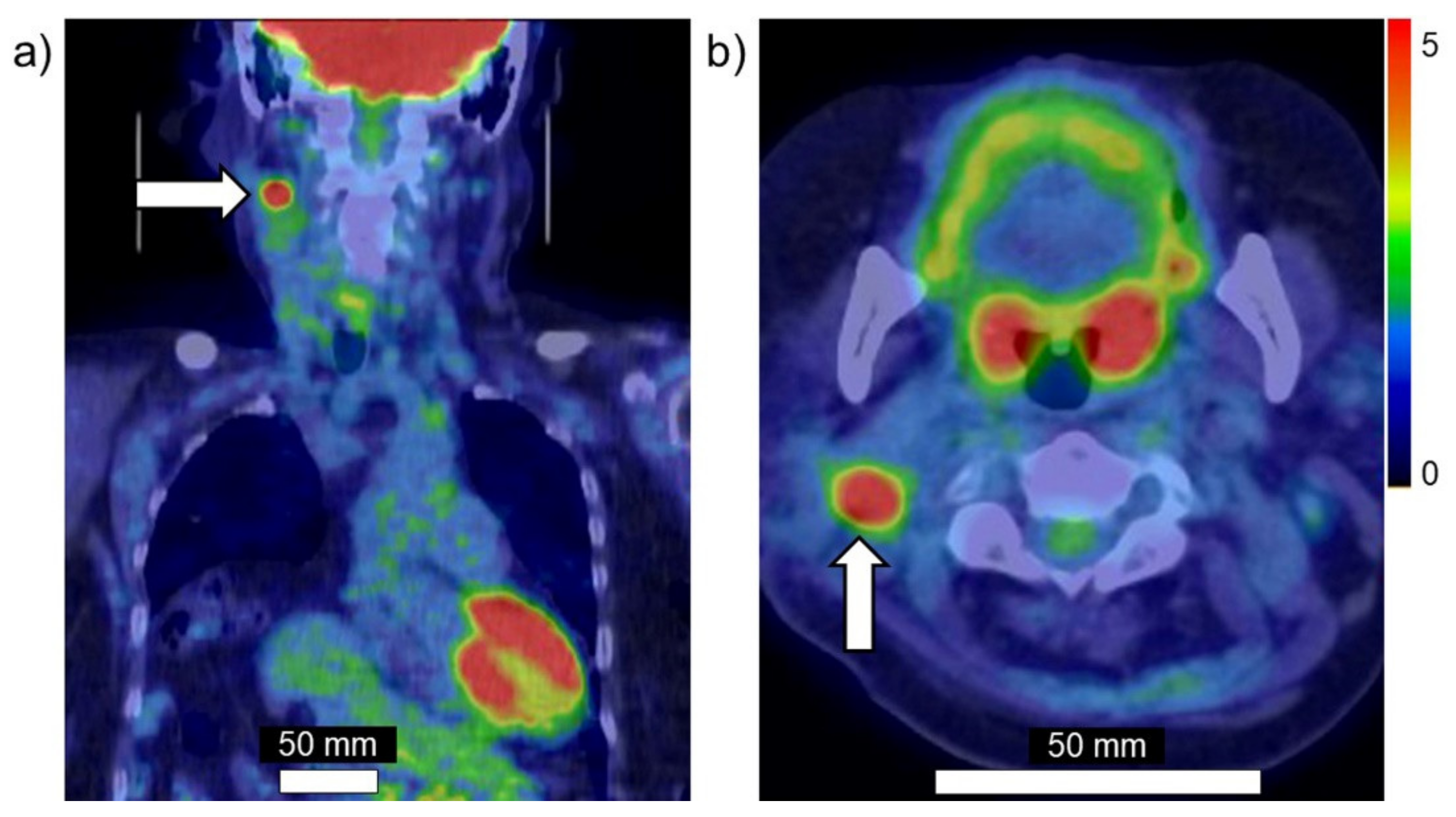
2. Development of 18FBPA PET
3. Synthesis and Basic Research of 18FBPA PET
4. Clinical Assessment of 18FBPA PET
5. Problems and Issues of 18FBPA PET
6. Imaging Techniques Other Than 18FBPA PET
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ishiwata, K.; Ido, T.; Mejia, A.A.; Ichihashi, M.; Mishima, Y. Synthesis and radiation dosimetry of 4-borono-2-[18F]fluoro-d,l-phenylalanine: A target compound for PET and boron neutron capture therapy. Int. J. Radiat. Appl. Instrum. Part A Appl. Radiat. Isot. 1991, 42, 325–328. [Google Scholar] [CrossRef]
- Imahori, Y.; Ueda, S.; Ohmori, Y.; Kusuki, T.; Ono, K.; Fujii, R.; Ido, T. Fluorine-18-labeled fluoroboronophenylalanine PET in patients with glioma. J. Nucl. Med. 1998, 39, 325–333. [Google Scholar]
- Kabalka, G.W.; Tang, C.; Bendel, P. The role of boron MRI in boron neutron capture therapy. J. Neurooncol. 1997, 33, 153–161. [Google Scholar] [CrossRef]
- Hanaoka, K.; Watabe, T.; Naka, S.; Kanai, Y.; Ikeda, H.; Horitsugi, G.; Kato, H.; Isohashi, K.; Shimosegawa, E.; Hatazawa, J. FBPA PET in boron neutron capture therapy for cancer: Prediction of (10)B concentration in the tumor and normal tissue in a rat xenograft model. EJNMMI Res. 2014, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Ishiwata, K. 4-Borono-2-18F-fluoro-L-phenylalanine PET for boron neutron capture therapy-oriented diagnosis: Overview of a quarter century of research. Ann. Nucl. Med. 2019, 33, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Ishiwata, K.; Ido, T.; Kawamura, M.; Kubota, K.; Ichihashi, M.; Mishima, Y. 4-Borono-2-[18F]fluoro-d,l-phenylalanine as a target compound for boron neutron capture therapy: Tumor imaging potential with positron emission tomography. Int. J. Radiat. Appl. Instrum. Part B Nucl. Med. Biol. 1991, 18, 745–751. [Google Scholar] [CrossRef]
- Ishiwata, K.; Ido, T.; Honda, C.; Kawamura, M.; Ichihashi, M.; Mishima, Y. 4-Borono-2-[18F]fluoro-d,l-phenylalanine: A possible tracer for melanoma diagnosis with PET. Int. J. Radiat. Appl. Instrum. Part B Nucl. Med. Biol. 1992, 19, 311–318. [Google Scholar] [CrossRef]
- Kanazawa, M.; Nishiyama, S.; Hashimoto, F.; Kakiuchi, T.; Tsukada, H. Evaluation of D-isomers of 4-borono-2-18F-fluoro-phenylalanine and O-11C-methyl-tyrosine as brain tumor imaging agents: A comparative PET study with their L-isomers in rat brain glioma. EJNMMI Res. 2018, 8, 47. [Google Scholar] [CrossRef]
- Grunewald, C.; Sauberer, M.; Filip, T.; Wanek, T.; Stanek, J.; Mairinger, S.; Rollet, S.; Kudejova, P.; Langer, O.; Schütz, C.; et al. On the applicability of [18F]FBPA to predict L-BPA concentration after amino acid preloading in HuH-7 liver tumor model and the implication for liver boron neutron capture therapy. Nucl. Med. Biol. 2017, 44, 83–89. [Google Scholar] [CrossRef]
- Watanabe, T.; Hattori, Y.; Ohta, Y.; Ishimura, M.; Nakagawa, Y.; Sanada, Y.; Tanaka, H.; Fukutani, S.; Masunaga, S.-I.; Hiraoka, M.; et al. Comparison of the pharmacokinetics between L-BPA and L-FBPA using the same administration dose and protocol: A validation study for the theranostic approach using [18F]-L-FBPA positron emission tomography in boron neutron capture therapy. BMC Cancer 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.-E.; Liao, A.-H.; Deng, W.-P.; Chang, P.-F.; Chen, J.-C.; Chen, F.-D.; Liu, R.-S.; Lee, J.-S. Evaluation of 4-borono-2-18F-fluoro-L-phenylalanine-fructose as a probe for boron neutron capture therapy in a glioma-bearing rat model. J. Nucl. Med. 2004, 45, 302–308. [Google Scholar] [PubMed]
- Yoshimoto, M.; Honda, N.; Kurihara, H.; Hiroi, K.; Nakamura, S.; Ito, M.; Shikano, N.; Itami, J.; Fujii, H. Non-invasive estimation of 10 B-4-borono-L-phenylalanine-derived boron concentration in tumors by PET using 4-borono-2-(18) F-fluoro-phenylalanine. Cancer Sci. 2018, 109, 1617–1626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imahori, Y.; Ueda, S.; Ohmori, Y.; Sakae, K.; Kusuki, T.; Kobayashi, T.; Takagaki, M.; Ono, K.; Ido, T.; Fujii, R. Positron emission tomography-based boron neutron capture therapy using boronophenylalanine for high-grade gliomas: Part I. Clin. Cancer Res. 1998, 4, 1825–1832. [Google Scholar] [PubMed]
- Mishima, Y.; Imahori, Y.; Honda, C.; Hiratsuka, J.; Ueda, S.; Ido, T. In vivo diagnosis of human malignant melanoma with positron emission tomography using specific melanoma-seeking 18F-DOPA analogue. J. Neurooncol. 1997, 33, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Imahori, Y.; Ueda, S.; Ohmori, Y.; Sakae, K.; Kusuki, T.; Kobayashi, T.; Takagaki, M.; Ono, K.; Ido, T.; Fujii, R. Positron emission tomography-based boron neutron capture therapy using boronophenylalanine for high-grade gliomas: Part II. Clin. Cancer Res. 1998, 4, 1833–1841. [Google Scholar]
- Nichols, T.L.; Kabalka, G.W.; Miller, L.F.; Khan, M.K.; Smith, G.T. Improved treatment planning for boron neutron capture therapy for glioblastoma multiforme using fluorine-18 labeled boronophenylalanine and positron emission tomography. Med. Phys. 2002, 29, 2351–2358. [Google Scholar] [CrossRef]
- Takahashi, Y.; Imahori, Y.; Mineura, K. Prognostic and therapeutic indicator of fluoroboronophenylalanine positron emission tomography in patients with gliomas. Clin. Cancer Res. 2003, 9, 5888–5895. [Google Scholar] [PubMed]
- Shimosegawa, E.; Isohashi, K.; Naka, S.; Horitsugi, G.; Hatazawa, J. Assessment of 10B concentration in boron neutron capture therapy: Potential of image-guided therapy using 18FBPA PET. Ann. Nucl. Med. 2016, 30, 749–755. [Google Scholar] [CrossRef]
- Isohashi, K.; Shimosegawa, E.; Naka, S.; Kanai, Y.; Horitsugi, G.; Mochida, I.; Matsunaga, K.; Watabe, T.; Kato, H.; Tatsumi, M.; et al. Comparison of the image-derived radioactivity and blood-sample radioactivity for estimating the clinical indicators of the efficacy of boron neutron capture therapy (BNCT): 4-borono-2-18F-fluoro-phenylalanine (FBPA) PET study. EJNMMI Res. 2016, 6, 75. [Google Scholar] [CrossRef] [Green Version]
- Kankaanranta, L.; Seppälä, T.; Koivunoro, H.; Saarilahti, K.; Atula, T.; Collan, J.; Salli, E.; Kortesniemi, M.; Uusi-Simola, J.; Välimäki, P.; et al. Boron Neutron Capture Therapy in the Treatment of Locally Recurred Head-and-Neck Cancer: Final Analysis of a Phase I/II Trial. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, e67–e75. [Google Scholar] [CrossRef]
- Wang, L.; Wang, S.; Chu, P.; Ho, C.; Jiang, S.; Liu, Y.; Liu, Y.; Liu, H.; Peir, J.; Chou, F.; et al. BNCT for locally recurrent head and neck cancer: Preliminary clinical experience from a phase I/II trial at Tsing Hua Open-Pool Reactor. Appl. Radiat. Isot. 2011, 69, 1803–1806. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-W.; Liu, Y.-W.H.; Chou, F.-I.; Jiang, S.-H. Clinical trials for treating recurrent head and neck cancer with boron neutron capture therapy using the Tsing-Hua Open Pool Reactor. Cancer Commun. 2018, 38, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soloway, A.; Tjarks, W.; Barnum, B.A.; Rong, F.-G.; Barth, R.F.; Codogni, I.M.; Wilson, J.G. The Chemistry of Neutron Capture Therapy. Chem. Rev. 1998, 98, 1515–1562. [Google Scholar] [CrossRef] [PubMed]
- Barth, R.F.; Soloway, A.H. Boron neutron capture therapy of brain tumors—Current status and future prospects. J. Neurooncol. 1997, 33, 3–7. [Google Scholar] [CrossRef]
- Pisarev, M.A.; Dagrosa, M.A.; Juvenal, G.J. Boron neutron capture therapy in cancer: Past, present and future. Arq. Bras. Endocrinol. Metabol. 2007, 51, 852–856. [Google Scholar] [CrossRef] [Green Version]
- Aihara, T.; Hiratsuka, J.; Fukumitsu, N.; Ishikawa, H.; Morita, N.; Kumada, H.; Kamitani, N.; Ohnishi, K.; Suzuki, M.; Sakurai, H.; et al. Evaluation of Fluoride-18-Labeled Boronophenylalanine-Positron Emission Tomography Imaging for the Assessment of Boron Neutron Capture Therapy in Patients with Recurrent Head and Neck Squamous Cell Carcinoma. Otolaryngology 2016, 6, 1–5. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Lee, Y.-Y.; Lin, C.-F.; Pan, P.-S.; Chen, J.-K.; Wang, C.-W.; Hsu, S.-M.; Kuo, Y.-C.; Lan, T.-L.; Hsu, S.; et al. Salvage Boron Neutron Capture Therapy for Malignant Brain Tumor Patients in Compliance with Emergency and Compassionate Use: Evaluation of 34 Cases in Taiwan. Biology 2021, 10, 334. [Google Scholar] [CrossRef]
- Lim, R.; Eaton, A.; Lee, N.Y.; Setton, J.; Ohri, N.; Rao, S.; Wong, R.; Fury, M.; Schöder, H. 18F-FDG PET/CT Metabolic Tumor Volume and Total Lesion Glycolysis Predict Outcome in Oropharyngeal Squamous Cell Carcinoma. J. Nucl. Med. 2012, 53, 1506–1513. [Google Scholar] [CrossRef] [Green Version]
- Hyun, S.H.; Ahn, H.K.; Kim, H.; Ahn, M.-J.; Park, K.; Ahn, Y.C.; Kim, J.; Shim, Y.M.; Choi, J.Y. Volume-based assessment by 18F-FDG PET/CT predicts survival in patients with stage III non-small-cell lung cancer. Eur. J. Nucl. Med. Mol. Imaging 2013, 41, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Im, H.-J.; Pak, K.; Cheon, G.J.; Kang, K.W.; Kim, S.-J.; Kim, I.-J.; Chung, J.-K.; Kim, E.E.; Lee, D.S. Prognostic value of volumetric parameters of 18F-FDG PET in non-small-cell lung cancer: A meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2014, 42, 241–251. [Google Scholar] [CrossRef]
- Langstrom, B.; Antoni, G.; Gullberg, P.; Halldin, C.; Malmborg, P.; Någren, K.; Rimland, A.; Svärd, H. Synthesis of L- and D-[methyl-11C]methionine. J. Nucl. Med. 1987, 28, 1037–1040. [Google Scholar]
- Bergstrom, M.; Lundqvist, H.; Ericson, K.; Lilja, A.; Johnstrom, P.; Langstrom, B.; von Holst, H.; Eriksson, L.; Blomqvist, G. Comparison of the accumulation kinetics of L-(methyl-11C)-methionine and D-(methyl-11C)-methionine in brain tumors studied with positron emission tomography. Acta Radiol. 1987, 28, 225–229. [Google Scholar]
- Kubota, K. From tumor biology to clinical PET: A review of positron emission tomography (PET) in oncology. Ann. Nucl. Med. 2001, 15, 471–486. [Google Scholar] [CrossRef]
- Wang, Y.; Rapalino, O.; Heidari, P.; Loeffler, J.; Shih, H.; Oh, K.; Mahmood, U. C11 Methionine PET (MET-PET) Imaging of Glioblastoma for Detecting Postoperative Residual Disease and Response to Chemoradiation Therapy. Int. J. Radiat. Oncol. 2018, 102, 1024–1028. [Google Scholar] [CrossRef] [PubMed]
- Nariai, T.; Ishiwata, K.; Kimura, Y.; Inaji, M.; Momose, T.; Yamamoto, T.; Matsumura, A.; Ishii, K.; Ohno, K. PET pharmacokinetic analysis to estimate boron concentration in tumor and brain as a guide to plan BNCT for malignant cerebral glioma. Appl. Radiat. Isot. 2009, 67, S348–S350. [Google Scholar] [CrossRef]
- Yamamoto, T.; Nakai, K.; Nariai, T.; Kumada, H.; Okumura, T.; Mizumoto, M.; Tsuboi, K.; Zaboronok, A.; Ishikawa, E.; Aiyama, H.; et al. The status of Tsukuba BNCT trial: BPA-based boron neutron capture therapy combined with X-ray irradiation. Appl. Radiat. Isot. 2011, 69, 1817–1818. [Google Scholar] [CrossRef]
- Watanabe, Y.; Kurihara, H.; Itami, J.; Sasaki, R.; Arai, Y.; Sugimura, K. Relationship between the uptake of 18F-borono-L-phenylalanine and L-[methyl-11C] methionine in head and neck tumors and normal organs. Radiat. Oncol. 2017, 12, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, D.; Deagostino, A.; Toppino, A.; Protti, N.; Bortolussi, S.; Altieri, S.; Aime, S.; Crich, S.G. An innovative therapeutic approach for malignant mesothelioma treatment based on the use of Gd/boron multimodal probes for MRI guided BNCT. J. Control Release 2018, 280, 31–38. [Google Scholar] [CrossRef]
- Bonora, M.; Corti, M.; Borsa, F.; Bortolussi, S.; Protti, N.; Santoro, D.; Stella, S.; Altieri, S.; Zonta, C.; Clerici, A.; et al. 1H and 10B NMR and MRI investigation of boron- and gadolinium–boron compounds in boron neutron capture therapy. Appl. Radiat. Isot. 2011, 69, 1702–1705. [Google Scholar] [CrossRef]
- Aime, S.; Barge, A.; Crivello, A.; Deagostino, A.; Gobetto, R.; Nervi, C.; Prandi, C.; Toppino, A.; Venturello, P. Synthesis of Gd(III)-C-palmitamidomethyl-C′-DOTAMA-C6-o-carborane: A new dual agent for innovative MRI/BNCT applications. Org. Biomol. Chem. 2008, 6, 4460–4466. [Google Scholar] [CrossRef] [PubMed]
- Crich, S.G.; Alberti, D.; Szabo, I.; Deagostino, A.; Toppino, A.; Barge, A.; Ballarini, F.; Bortolussi, S.; Bruschi, P.; Protti, N.; et al. MRI-Guided Neutron Capture Therapy by Use of a Dual Gadolinium/Boron Agent Targeted at Tumour Cells through Upregulated Low-Density Lipoprotein Transporters. Chemistry 2011, 17, 8479–8486. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukumitsu, N.; Matsumoto, Y. Development of an Imaging Technique for Boron Neutron Capture Therapy. Cells 2021, 10, 2135. https://doi.org/10.3390/cells10082135
Fukumitsu N, Matsumoto Y. Development of an Imaging Technique for Boron Neutron Capture Therapy. Cells. 2021; 10(8):2135. https://doi.org/10.3390/cells10082135
Chicago/Turabian StyleFukumitsu, Nobuyoshi, and Yoshitaka Matsumoto. 2021. "Development of an Imaging Technique for Boron Neutron Capture Therapy" Cells 10, no. 8: 2135. https://doi.org/10.3390/cells10082135
APA StyleFukumitsu, N., & Matsumoto, Y. (2021). Development of an Imaging Technique for Boron Neutron Capture Therapy. Cells, 10(8), 2135. https://doi.org/10.3390/cells10082135





