State-of-the-Art and Future Challenges for Nutritional Interventions in Facioscapulohumeral Dystrophy: A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
3. Pathophysiology of FSHD
4. Available Studies Involving Nutritional Interventions in FSHD
4.1. Antioxidants and Anti-Inflammatory Supplementation
4.2. Post-Exercise Protein–Carbohydrate Supplementation
4.3. Creatine Monohydrate Supplementation
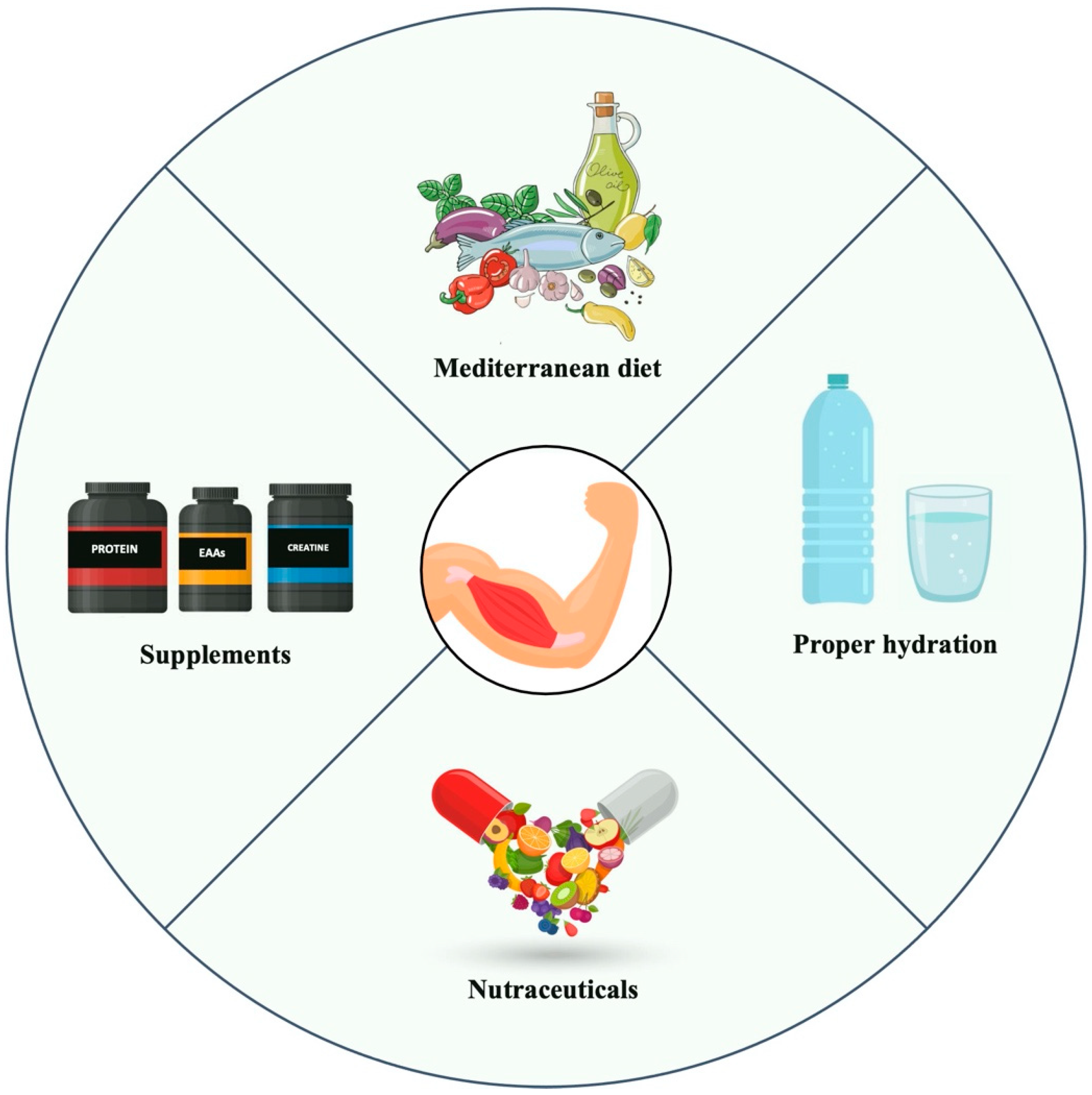
5. Promising Dietary Pattern and Supplements for Future Research in FSHD
5.1. The Mediterranean Diet: A Promising Anti-Inflammatory and Antioxidant Approach for FSHD
5.2. Proteins and Essential Amino Acids
5.3. β-Hydroxy-β-Methylbutyrate
5.4. Vitamin D
5.5. Strategies for Proper Muscle Hydration
5.6. Supplements for Gut Microbiota Health
6. Discussion
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Available online: https://www.orpha.net (accessed on 10 February 2025).
- Gatica, L.V.; Rosa, A.L. A complex interplay of genetic and epigenetic events leads to abnormal expression of the DUX4 gene in facioscapulohumeral muscular dystrophy. Neuromuscul. Disord. 2016, 26, 844–852. [Google Scholar] [CrossRef] [PubMed]
- Vera, K.A.; McConville, M.; Kyba, M.; Keller-Ross, M.L. Sarcopenic Obesity in Facioscapulohumeral Muscular Dystrophy. Front. Physiol. 2020, 11, 1008. [Google Scholar] [CrossRef] [PubMed]
- Voet, N.; Bleijenberg, G.; Hendriks, J.; de Groot, I.; Padberg, G.; van Engelen, B.; Geurts, A. Both aerobic exercise and cognitive-behavioral therapy reduce chronic fatigue in FSHD: An RCT. Neurology 2014, 83, 1914–1922. [Google Scholar] [CrossRef] [PubMed]
- Alphonsa, S.; Wuebbles, R.; Jones, T.; Pavilionis, P.; Murray, N. Spatio-temporal gait differences in facioscapulohumeral muscular dystrophy during single and dual task overground walking—A pilot study. J. Clin. Transl. Res. 2022, 8, 166–175. [Google Scholar]
- Huisinga, J.; Bruetsch, A.; Mccalley, A.; Currence, M.; Herbelin, L.; Jawdat, O.; Pasnoor, M.; Dimachkie, M.; Barohn, R.; Statland, J. An instrumented timed up and go in facioscapulohumeral muscular dystrophy. Muscle Nerve 2018, 57, 503–506. [Google Scholar] [CrossRef]
- Hamel, J.; Johnson, N.; Tawil, R.; Martens, W.B.; Dilek, N.; McDermott, M.P.; Heatwole, C. Patient-Reported Symptoms in Facioscapulohumeral Muscular Dystrophy (PRISM-FSHD). Neurology 2019, 93, e1180–e1192. [Google Scholar] [CrossRef]
- Skalsky, A.J.; Abresch, R.T.; Han, J.J.; Shin, C.S.; McDonald, C.M. The relationship between regional body composition and quantitative strength in facioscapulohumeral muscular dystrophy (FSHD). Neuromuscul. Disord. 2008, 18, 873–880. [Google Scholar] [CrossRef]
- Vera, K.A.; McConville, M.; Glazos, A.; Stokes, W.; Kyba, M.; Keller-Ross, M. Exercise Intolerance in Facioscapulohumeral Muscular Dystrophy. Med. Sci. Sports Exerc. 2022, 54, 887–895. [Google Scholar] [CrossRef]
- Crisafulli, O.; Bottoni, G.; Lacetera, J.; Fassio, F.; Grattarola, L.; Lavaselli, E.; Giovanetti, G.; Tupler, R.; Negro, M.; D’Antona, G. Bioimpedance analysis of fat free mass and its subcomponents and relative associations with maximal oxygen consumption in facioscapulohumeral dystrophy. Eur. J. Appl. Physiol. 2024, 125, 157–165. [Google Scholar] [CrossRef]
- Crisafulli, O.; Grattarola, L.; Bottoni, G.; Lacetera, J.; Lavaselli, E.; Beretta-Piccoli, M.; Tupler, R.; Soldini, E.; D’Antona, G. Maximal Oxygen Consumption Is Negatively Associated with Fat Mass in Facioscapulohumeral Dystrophy. Int. J. Environ. Res. Public Health 2024, 21, 979. [Google Scholar] [CrossRef]
- Crisafulli, O.; Baptista, R.; Drid, P.; Grattarola, L.; Bottoni, G.; Lavaselli, E.; Negro, M.; Tupler, R.; Quintiero, V.; D’Antona, G. Analysis of Body Fluid Distribution, Phase Angle and Its Association with Maximal Oxygen Consumption in Facioscapulohumeral Dystrophy: An Observational Study. Health Sci. Rep. 2025, 8, e70335. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, I.; Serra-Prat, M.; Yébenes, J.C. The Role of Water Homeostasis in Muscle Function and Frailty: A Review. Nutrients 2019, 11, 1857. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Yoshida, T.; Yokoyama, K.; Watanabe, Y.; Miyake, M.; Yamagata, E.; Yamada, M.; Kimura, M.; Kyoto-Kameoka Study. The Extracellular to Intracellular Water Ratio in Upper Legs is Negatively Associated with Skeletal Muscle Strength and Gait Speed in Older People. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Serra-Prat, M.; Lorenzo, I.; Palomera, E.; Yébenes, J.C.; Campins, L.; Cabré, M. Intracellular Water Content in Lean Mass is Associated with Muscle Strength, Functional Capacity, and Frailty in Community-Dwelling Elderly Individuals. A Cross-Sectional Study. Nutrients 2019, 11, 661. [Google Scholar] [CrossRef]
- Hioka, A.; Akazawa, N.; Okawa, N.; Nagahiro, S. Increased total body extracellular-to-intracellular water ratio in community-dwelling elderly women is associated with decreased handgrip strength and gait speed. Nutrition 2021, 86, 111175. [Google Scholar] [CrossRef]
- Nakamura, K.; Kinugasa, Y.; Sota, T.; Hirai, M.; Kato, M.; Yamamoto, K. The water imbalance of skeletal muscle and muscle weakness in patients with heart failure. ESC Heart Fail. 2024, 11, 3757–3766. [Google Scholar] [CrossRef]
- Attarian, S.; Beloribi-Djefaflia, S.; Bernard, R.; Nguyen, K.; Cances, C.; Gavazza, C.; Echaniz-Laguna, A.; Espil, C.; Evangelista, T.; Feasson, L.; et al. French National Protocol for diagnosis and care of facioscapulohumeral muscular dystrophy (FSHD). J. Neurol. 2024, 271, 5778–5803. [Google Scholar] [CrossRef]
- Leone, E.; Pandyan, A.; Rogers, A.; Kulshrestha, R.; Hill, J.; Philp, F. Effectiveness of conservative non-pharmacological interventions in people with muscular dystrophies: A systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2024, 95, 442–453. [Google Scholar] [CrossRef]
- Aprile, I.; Bordieri, C.; Gilardi, A.; Lainieri Milazzo, M.; Russo, G.; De Santis, F.; Frusciante, R.; Iannaccone, E.; Erra, C.; Ricci, E.; et al. Balance and walking involvement in facioscapulohumeral dystrophy: A pilot study on the effects of custom lower limb orthoses. Eur. J. Phys. Rehabil. Med. 2013, 49, 169–178. [Google Scholar]
- Colson, S.S.; Benchortane, M.; Tanant, V.; Faghan, J.P.; Fournier-Mehouas, M.; Benaïm, C.; Desnuelle, C.; Sacconi, S. Neuromuscular electrical stimulation training: A safe and effective treatment for facioscapulohumeral muscular dystrophy patients. Arch. Phys. Med. Rehabil. 2010, 91, 697–702. [Google Scholar] [CrossRef]
- Ribot-Ciscar, E.; Milhe-De Bovis, V.; Aimonetti, J.M.; Lapeyssonnie, B.; Campana-Salort, E.; Pouget, J.; Attarian, S. Functional impact of vibratory proprioceptive assistance in patients with facioscapulohumeral muscular dystrophy. Muscle Nerve 2015, 52, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Olsen, D.B.; Ørngreen, M.C.; Vissing, J. Aerobic training improves exercise performance in facioscapulohumeral muscular dystrophy. Neurology 2005, 64, 1064–1066. [Google Scholar] [CrossRef] [PubMed]
- Andersen, G.; Heje, K.; Buch, A.E.; Vissing, J. High-intensity interval training in facioscapulohumeral muscular dystrophy type 1: A randomized clinical trial. J. Neurol. 2017, 264, 1099–1106. [Google Scholar] [CrossRef]
- Bankolé, L.C.; Millet, G.Y.; Temesi, J.; Bachasson, D.; Ravelojaona, M.; Wuyam, B.; Verges, S.; Ponsot, E.; Antoine, J.C.; Kadi, F.; et al. Safety and efficacy of a 6-month home-based exercise program in patients with facioscapulohumeral muscular dystrophy: A randomized controlled trial. Medicine 2016, 95, e4497. [Google Scholar] [CrossRef]
- Bostock, E.L.; O’Dowd, D.N.; Payton, C.J.; Smith, D.; Orme, P.; Edwards, B.T.; Morse, C.I. The Effects of Resistance Exercise Training on Strength and Functional Tasks in Adults with Limb-Girdle, Becker, and Facioscapulohumeral Dystrophies. Front. Neurol. 2019, 10, 1216. [Google Scholar] [CrossRef]
- O’Dowd, D.N.; Bostock, E.L.; Smith, D.; Morse, C.I.; Orme, P.; Payton, C.J. The effects of 12 weeks’ resistance training on psychological parameters and quality of life in adults with Facioscapulohumeral, Becker, and Limb-girdle dystrophies. Disabil. Rehabil. 2022, 44, 59505956. [Google Scholar] [CrossRef]
- Lim, K.R.Q.; Nguyen, Q.; Yokota, T. DUX4 Signalling in the Pathogenesis of Facioscapulohumeral Muscular Dystrophy. Int. J. Mol. Sci. 2020, 21, 729. [Google Scholar] [CrossRef]
- Hewitt, J.E.; Lyle, R.; Clark, L.N.; Valleley, E.M.; Wright, T.J.; Wijmenga, C.; van Deutekom, J.C.; Francis, F.; Sharpe, P.T.; Hofker, M.; et al. Analysis of the tandem repeat locus D4Z4 associated with facioscapulohumeral muscular dystrophy. Hum. Mol. Genet. 1994, 3, 1287–1295. [Google Scholar] [CrossRef]
- Schiaffino, S.; Dyar, K.A.; Ciciliot, S.; Blaauw, B.; Sandri, M. Mechanisms regulating skeletal muscle growth and atrophy. FEBS J. 2013, 280, 4294–4314. [Google Scholar] [CrossRef]
- Bosnakovski, D.; Xu, Z.; Gang, E.J.; Galindo, C.L.; Liu, M.; Simsek, T.; Garner, H.R.; Agha-Mohammadi, S.; Tassin, A.; Coppée, F.; et al. An isogenetic myoblast expression screen identifies DUX4-mediated FSHD-associated molecular pathologies. EMBO J. 2008, 27, 2766–2779. [Google Scholar] [CrossRef]
- Celegato, B.; Capitanio, D.; Pescatori, M.; Romualdi, C.; Pacchioni, B.; Cagnin, S.; Viganò, A.; Colantoni, L.; Begum, S.; Ricci, E.; et al. Parallel protein and transcript profiles of FSHD patient muscles correlate to the D4Z4 arrangement and reveal a common impairment of slow to fast fibre differentiation and a general deregulation of MyoD-dependent genes. Proteomics 2006, 6, 5303–5321. [Google Scholar] [CrossRef] [PubMed]
- Duranti, E.; Villa, C. Influence of DUX4 Expression in Facioscapulohumeral Muscular Dystrophy and Possible Treatments. Int. J. Mol. Sci. 2023, 24, 9503. [Google Scholar] [CrossRef] [PubMed]
- Shadle, S.C.; Zhong, J.W.; Campbell, A.E.; Conerly, M.L.; Jagannathan, S.; Wong, C.J.; Morello, T.D.; van der Maarel, S.M.; Tapscott, S.J. DUX4-induced dsRNA and MYC mRNA stabilization activate apoptotic pathways in human cell models of facioscapulohumeral dystrophy. PLoS Genet. 2017, 13, e1006658. [Google Scholar] [CrossRef] [PubMed]
- Ganassi, M.; Zammit, P.S. Involvement of muscle satellite cell dysfunction in neuromuscular disorders: Expanding the portfolio of satellite cell-opathies. Eur. J. Transl. Myol. 2022, 32, 10064. [Google Scholar] [CrossRef]
- Turki, A.; Hayot, M.; Carnac, G.; Pillard, F.; Passerieux, E.; Bommart, S.; Raynaud de Mauverger, E.; Hugon, G.; Pincemail, J.; Pietri, S.; et al. Functional muscle impairment in facioscapulohumeral muscular dystrophy is correlated with oxidative stress and mitochondrial dysfunction. Free Radic. Biol. Med. 2012, 53, 1068–1079. [Google Scholar] [CrossRef]
- Dahlqvist, J.R.; Andersen, G.; Khawajazada, T.; Vissing, C.; Thomsen, C.; Vissing, J. Relationship between muscle inflammation and fat replacement assessed by MRI in facioscapulohumeral muscular dystrophy. J. Neurol. 2019, 266, 1127–1135. [Google Scholar] [CrossRef]
- Zalejska-Fiolka, J.; Birková, A.; Wielkoszyński, T.; Hubková, B.; Szlachta, B.; Fiolka, R.; Błaszczyk, U.; Kuzan, A.; Gamian, A.; Mareková, M.; et al. Loss of Skeletal Muscle Mass and Intracellular Water as Undesired Outcomes of Weight Reduction in Obese Hyperglycemic Women: A Short-Term Longitudinal Study. Int. J. Environ. Res. Public Health 2022, 19, 1001. [Google Scholar] [CrossRef]
- Soeters, P.B.; Wolfe, R.R.; Shenkin, A. Hypoalbuminemia: Pathogenesis and Clinical Significance. JPEN J. Parenter. Enter. Nutr. 2019, 43, 181–193. [Google Scholar] [CrossRef]
- Liu, G.Y.; Sabatini, D.M. mTOR at the nexus of nutrition, growth, ageing and disease. Nat. Rev. Mol. Cell Biol. 2020, 21, 183–203. [Google Scholar] [CrossRef]
- Mancin, L.; Wu, G.D.; Paoli, A. Gut microbiota-bile acid-skeletal muscle axis. Trends Microbiol. 2023, 31, 254–269. [Google Scholar] [CrossRef]
- Grosicki, G.J.; Fielding, R.A.; Lustgarten, M.S. Gut Microbiota Contribute to Age-Related Changes in Skeletal Muscle Size, Composition, and Function: Biological Basis for a Gut-Muscle Axis. Calcif. Tissue Int. 2018, 102, 433–442. [Google Scholar] [CrossRef]
- Shreiner, A.B.; Kao, J.Y.; Young, V.B. The gut microbiome in health and in disease. Curr. Opin. Gastroenterol. 2015, 31, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Passerieux, E.; Hayot, M.; Jaussent, A.; Carnac, G.; Gouzi, F.; Pillard, F.; Picot, M.C.; Böcker, K.; Hugon, G.; Pincemail, J.; et al. Effects of vitamin C, vitamin E, zinc gluconate, and selenomethionine supplementation on muscle function and oxidative stress biomarkers in patients with facioscapulohumeral dystrophy: A double-blind randomized controlled clinical trial. Free Radic Biol. Med. 2015, 81, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Sitzia, C.; Meregalli, M.; Belicchi, M.; Farini, A.; Arosio, M.; Bestetti, D.; Villa, C.; Valenti, L.; Brambilla, P.; Torrente, Y. Preliminary Evidences of Safety and Efficacy of Flavonoids- and Omega 3-Based Compound for Muscular Dystrophies Treatment: A Randomized Double-Blind Placebo Controlled Pilot Clinical Trial. Front. Neurol. 2019, 10, 755. [Google Scholar] [CrossRef] [PubMed]
- Wilson, V.D.; Bommart, S.; Passerieux, E.; Thomas, C.; Pincemail, J.; Picot, M.C.; Mercier, J.; Portet, F.; Arbogast, S.; Laoudj-Chenivesse, D. Muscle strength, quantity and quality and muscle fat quantity and their association with oxidative stress in patients with facioscapulohumeral muscular dystrophy: Effect of antioxidant supplementation. Free Radic. Biol. Med. 2024, 219, 112–126. [Google Scholar] [CrossRef]
- Andersen, G.; Prahm, K.P.; Dahlqvist, J.R.; Citirak, G.; Vissing, J. Protein-carbohydrate supplements improve muscle protein balance in muscular dystrophy patients after endurance exercise: A placebo-controlled crossover study. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 308, R123–R130. [Google Scholar] [CrossRef]
- Walter, M.C.; Lochmüller, H.; Reilich, P.; Klopstock, T.; Huber, R.; Hartard, M.; Hennig, M.; Pongratz, D.; Müller-Felber, W. Creatine monohydrate in muscular dystrophies: A double-blind, placebo-controlled clinical study. Neurology. 2000, 54, 1848–1850. [Google Scholar] [CrossRef]
- Ricker, M.A.; Haas, W.C. Anti-Inflammatory Diet in Clinical Practice: A Review. Nutr. Clin. Pract. 2017, 32, 318–325. [Google Scholar] [CrossRef]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef]
- Makki, K.; Deehan, E.C.; Walter, J.; Bäckhed, F. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host Microbe 2018, 23, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Kenđel Jovanović, G.; Mrakovcic-Sutic, I.; Pavičić Žeželj, S.; Šuša, B.; Rahelić, D.; Klobučar Majanović, S. The Efficacy of an Energy-Restricted Anti-Inflammatory Diet for the Management of Obesity in Younger Adults. Nutrients 2020, 12, 3583. [Google Scholar] [CrossRef] [PubMed]
- Al-Aubaidy, H.A.; Dayan, A.; Deseo, M.A.; Itsiopoulos, C.; Jamil, D.; Hadi, N.R.; Thomas, C.J. Twelve-Week Mediterranean Diet Intervention Increases Citrus Bioflavonoid Levels and Reduces Inflammation in People with Type 2 Diabetes Mellitus. Nutrients 2021, 13, 1133. [Google Scholar] [CrossRef] [PubMed]
- Georgoulis, M.; Yiannakouris, N.; Tenta, R.; Fragopoulou, E.; Kechribari, I.; Lamprou, K.; Perraki, E.; Vagiakis, E.; Kontogianni, M.D. A weight-loss Mediterranean diet/lifestyle intervention ameliorates inflammation and oxidative stress in patients with obstructive sleep apnea: Results of the “MIMOSA” randomized clinical trial. Eur. J. Nutr. 2021, 60, 3799–3810. [Google Scholar] [CrossRef]
- Petrella, C.; Di Certo, M.G.; Gabanella, F.; Barbato, C.; Ceci, F.M.; Greco, A.; Ralli, M.; Polimeni, A.; Angeloni, A.; Severini, C.; et al. Mediterranean Diet, Brain and Muscle: Olive Polyphenols and Resveratrol Protection in Neurodegenerative and Neuromuscular Disorders. Curr. Med. Chem. 2021, 28, 7595–7613. [Google Scholar] [CrossRef]
- Amzali, S.; Wilson, V.D.; Bommart, S.; Picot, M.C.; Galas, S.; Mercier, J.; Poucheret, P.; Cristol, J.P.; Arbogast, S.; Laoudj-Chenivesse, D. Nutritional Status of Patients with Facioscapulohumeral Muscular Dystrophy. Nutrients 2023, 15, 1673. [Google Scholar] [CrossRef]
- Rogeri, P.S.; Zanella, R., Jr.; Martins, G.L.; Garcia, M.D.A.; Leite, G.; Lugaresi, R.; Gasparini, S.O.; Sperandio, G.A.; Ferreira, L.H.B.; Souza-Junior, T.P.; et al. Strategies to Prevent Sarcopenia in the Aging Process: Role of Protein Intake and Exercise. Nutrients 2021, 14, 52. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.; Sobotka, L.; et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin. Nutr. 2022, 41, 958–989. [Google Scholar] [CrossRef]
- Deer, R.R.; Volpi, E. Protein intake and muscle function in older adults. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 248–253. [Google Scholar] [CrossRef]
- Park, Y.; Choi, J.E.; Hwang, H.S. Protein supplementation improves muscle mass and physical performance in undernourished prefrail and frail elderly subjects: A randomized, double-blind, placebo-controlled trial. Am. J. Clin. Nutr. 2018, 108, 1026–1033. [Google Scholar] [CrossRef]
- Mori, H.; Tokuda, Y. De-Training Effects Following Leucine-Enriched Whey Protein Supplementation and Resistance Training in Older Adults with Sarcopenia: A Randomized Controlled Trial with 24 Weeks of Follow-Up. J. Nutr. Health Aging 2022, 26, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Jäger, R.; Kerksick, C.M.; Campbell, B.I.; Cribb, P.J.; Wells, S.D.; Skwiat, T.M.; Purpura, M.; Ziegenfuss, T.N.; Ferrando, A.A.; Arent, S.M.; et al. International Society of Sports Nutrition Position Stand: Protein and exercise. J. Int. Soc. Sports Nutr. 2017, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Elango, R.; Ball, R.O.; Pencharz, P.B. Recent advances in determining protein and amino acid requirements in humans. Br. J. Nutr. 2012, 108 (Suppl. S2), S22–S30. [Google Scholar] [CrossRef] [PubMed]
- Cereda, E.; Pisati, R.; Rondanelli, M.; Caccialanza, R. Whey Protein, Leucine- and Vitamin-D-Enriched Oral Nutritional Supplementation for the Treatment of Sarcopenia. Nutrients 2022, 14, 1524. [Google Scholar] [CrossRef]
- Negro, M.; Crisafulli, O.; D’Antona, G. Effects of essential amino acid (EAA) and glutamine supplementation on skeletal muscle wasting in acute, subacute, and postacute conditions. Clin. Nutr. ESPEN 2024, 62, 224–233. [Google Scholar] [CrossRef]
- Rathmacher, J.A.; Pitchford, L.M.; Stout, J.R.; Townsend, J.R.; Jäger, R.; Kreider, R.B.; Campbell, B.I.; Kerksick, C.M.; Harty, P.S.; Candow, D.G.; et al. International society of sports nutrition position stand: β-hydroxy-β-methylbutyrate (HMB). J. Int. Soc. Sports Nutr. 2025, 22, 2434734. [Google Scholar] [CrossRef]
- Kuriyan, R.; Lokesh, D.P.; Selvam, S.; Jayakumar, J.; Philip, M.G.; Shreeram, S.; Kurpad, A.V. The relationship of endogenous plasma concentrations of β-Hydroxy β-Methyl Butyrate (HMB) to age and total appendicular lean mass in humans. Exp. Gerontol. 2016, 81, 13–18. [Google Scholar] [CrossRef]
- Yang, C.; Song, Y.; Li, T.; Chen, X.; Zhou, J.; Pan, Q.; Jiang, W.; Wang, M.; Jia, H. Effects of Beta-Hydroxy-Beta-Methylbutyrate Supplementation on Older Adults with Sarcopenia: A Randomized, Double-Blind, Placebo-Controlled Study. J. Nutr. Health Aging 2023, 27, 329–339. [Google Scholar] [CrossRef]
- Din, U.S.U.; Brook, M.S.; Selby, A.; Quinlan, J.; Boereboom, C.; Abdulla, H.; Franchi, M.; Narici, M.V.; Phillips, B.E.; Williams, J.W.; et al. A double-blind placebo controlled trial into the impacts of HMB supplementation and exercise on free-living muscle protein synthesis, muscle mass and function, in older adults. Clin. Nutr. 2019, 38, 2071–2078. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meza-Valderrama, D.; Sánchez-Rodríguez, D.; Messaggi-Sartor, M.; Muñoz-Redondo, E.; Morgado-Pérez, A.; Tejero-Sánchez, M.; De Jaime-Gil, E.; Leiva-Banuelos, N.; Marco, E. Supplementation with β-hydroxy-β-methylbutyrate after resistance training in post-acute care patients with sarcopenia: A randomized, double-blind placebo-controlled trial. Arch. Gerontol. Geriatr. 2024, 119, 105323. [Google Scholar] [CrossRef]
- Bollen, S.E.; Bass, J.J.; Fujita, S.; Wilkinson, D.; Hewison, M.; Atherton, P.J. The Vitamin D/Vitamin D receptor (VDR) axis in muscle atrophy and sarcopenia. Cell. Signal. 2022, 96, 110355. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.M.; Ismaeel, A.; Griffis, R.B.; Weems, S. Effects of Vitamin D Supplementation on Muscle Strength in Athletes: A Systematic Review. J. Strength Cond. Res. 2017, 31, 566–574. [Google Scholar] [CrossRef]
- Chen, Y.; Liang, Y.; Guo, H.; Meng, K.; Qiu, J.; Benardot, D. Muscle-Related Effect of Whey Protein and Vitamin D3 Supplementation Provided before or after Bedtime in Males Undergoing Resistance Training. Nutrients 2022, 14, 2289. [Google Scholar] [CrossRef]
- Pilch, W.; Kita, B.; Piotrowska, A.; Tota, Ł.; Maciejczyk, M.; Czerwińska-Ledwig, O.; Sadowska-Krepa, E.; Kita, S.; Pałka, T. The effect of vitamin D supplementation on the muscle damage after eccentric exercise in young men: A randomized, control trial. J. Int. Soc. Sports Nutr. 2020, 17, 53. [Google Scholar] [CrossRef]
- Bauer, J.M.; Verlaan, S.; Bautmans, I.; Brandt, K.; Donini, L.M.; Maggio, M.; McMurdo, M.E.; Mets, T.; Seal, C.; Wijers, S.L.; et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2015, 16, 740–747. [Google Scholar] [CrossRef]
- Chang, M.C.; Choo, Y.J. Effects of Whey Protein, Leucine, and Vitamin D Supplementation in Patients with Sarcopenia: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 521. [Google Scholar] [CrossRef]
- Lin, C.C.; Shih, M.H.; Chen, C.D.; Yeh, S.L. Effects of adequate dietary protein with whey protein, leucine, and vitamin D supplementation on sarcopenia in older adults: An open-label, parallel-group study. Clin. Nutr. 2021, 40, 1323–1329. [Google Scholar] [CrossRef]
- Häussinger, D.; Roth, E.; Lang, F.; Gerok, W. Cellular hydration state: An important determinant of protein catabolism in health and disease. Lancet 1993, 341, 1330–1332. [Google Scholar] [CrossRef]
- Schoenfeld, B.J. Does exercise-induced muscle damage play a role in skeletal muscle hypertrophy? J. Strength Cond. Res. 2012, 26, 1441–1453. [Google Scholar] [CrossRef]
- Schoenfeld, B.J. Potential mechanisms for a role of metabolic stress in hypertrophic adaptations to resistance training. Sports Med. 2013, 43, 179–194. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.S.; Avelar, A.; Schoenfeld, B.J.; Ritti Dias, R.M.; Altimari, L.R.; Cyrino, E.S. Resistance training promotes increase in intracellular hydration in men and women. Eur. J. Sport Sci. 2014, 14, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.; Trojian, T.H. Creatine supplementation. Curr. Sports Med. Rep. 2013, 12, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Liang, R.; Song, Q.; Song, S.; Yue, J.; Wu, C. Investigating association between gut microbiota and sarcopenia-related traits: A Mendelian randomization study. Precis. Clin. Med. 2023, 6, pbad010. [Google Scholar] [CrossRef]
- Zhang, T.; Cheng, J.K.; Hu, Y.M. Gut microbiota as a promising therapeutic target for age-related sarcopenia. Ageing Res. Rev. 2022, 81, 101739. [Google Scholar] [CrossRef]
- Lustgarten, M.S. The Role of the Gut Microbiome on Skeletal Muscle Mass and Physical Function: 2019 Update. Front. Physiol. 2019, 10, 1435. [Google Scholar] [CrossRef]
- Giron, M.; Thomas, M.; Dardevet, D.; Chassard, C.; Savary-Auzeloux, I. Gut microbes and muscle function: Can probiotics make our muscles stronger? J. Cachexia Sarcopenia Muscle 2022, 13, 1460–1476. [Google Scholar] [CrossRef]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Tawil, R.; McDermott, M.P.; Pandya, S.; King, W.; Kissel, J.; Mendell, J.R.; Griggs, R.C. A pilot trial of prednisone in facioscapulohumeral muscular dystrophy. FSH-DY Group. Neurology 1997, 48, 46–49. [Google Scholar] [CrossRef]
- Angelini, C. The role of corticosteroids in muscular dystrophy: A critical appraisal. Muscle Nerve 2007, 36, 424–435. [Google Scholar] [CrossRef]
- Cohen, J.; DeSimone, A.; Lek, M.; Lek, A. Therapeutic Approaches in Facioscapulohumeral Muscular Dystrophy. Trends Mol. Med. 2021, 27, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Weston, M.; Taylor, K.L.; Batterham, A.M.; Hopkins, W.G. Effects of low-volume high-intensity interval training (HIT) on fitness in adults: A meta-analysis of controlled and non-controlled trials. Sports Med. 2014, 44, 1005–1017. [Google Scholar] [CrossRef]
- Damas, F.; Libardi, C.A.; Ugrinowitsch, C. The development of skeletal muscle hypertrophy through resistance training: The role of muscle damage and muscle protein synthesis. Eur. J. Appl. Physiol. 2018, 118, 485–500. [Google Scholar] [CrossRef] [PubMed]
- Damas, F.; Phillips, S.; Vechin, F.C.; Ugrinowitsch, C. A review of resistance training-induced changes in skeletal muscle protein synthesis and their contribution to hypertrophy. Sports Med. 2015, 45, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Cheng, R.; Song, G.; Teng, J.; Shen, S.; Fu, X.; Yan, Y.; Liu, C. The Effect of Resistance Training on the Rehabilitation of Elderly Patients with Sarcopenia: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15491. [Google Scholar] [CrossRef]
- Lu, L.; Mao, L.; Feng, Y.; Ainsworth, B.E.; Liu, Y.; Chen, N. Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: A systematic review and meta-analysis. BMC Geriatr. 2021, 21, 708. [Google Scholar] [CrossRef]
- Hartono, F.A.; Martin-Arrowsmith, P.W.; Peeters, W.M.; Churchward-Venne, T.A. The Effects of Dietary Protein Supplementation on Acute Changes in Muscle Protein Synthesis and Longer-Term Changes in Muscle Mass, Strength, and Aerobic Capacity in Response to Concurrent Resistance and Endurance Exercise in Healthy Adults: A Systematic Review. Sports Med. 2022, 52, 1295–1328. [Google Scholar] [CrossRef]
- Nasimi, N.; Sohrabi, Z.; Nunes, E.A.; Sadeghi, E.; Jamshidi, S.; Gholami, Z.; Akbarzadeh, M.; Faghih, S.; Akhlaghi, M.; Phillips, S.M. Whey Protein Supplementation with or without Vitamin D on Sarcopenia-Related Measures: A Systematic Review and Meta-Analysis. Adv. Nutr. 2023, 14, 762–773. [Google Scholar] [CrossRef]
- Kreider, R.B.; Kalman, D.S.; Antonio, J.; Ziegenfuss, T.N.; Wildman, R.; Collins, R.; Candow, D.G.; Kleiner, S.M.; Almada, A.L.; Lopez, H.L. International Society of Sports Nutrition position stand: Safety and efficacy of creatine supplementation in exercise, sport, and medicine. J. Int. Soc. Sports Nutr. 2017, 14, 18. [Google Scholar] [CrossRef]
- Louis, M.; Lebacq, J.; Poortmans, J.R.; Belpaire-Dethiou, M.C.; Devogelaer, J.P.; Van Hecke, P.; Goubel, F.; Francaux, M. Beneficial effects of creatine supplementation in dystrophic patients. Muscle Nerve 2003, 27, 604–610. [Google Scholar] [CrossRef]
- Tarnopolsky, M.A.; Mahoney, D.J.; Vajsar, J.; Rodriguez, C.; Doherty, T.J.; Roy, B.D.; Biggar, D. Creatine monohydrate enhances strength and body composition in Duchenne muscular dystrophy. Neurology 2004, 62, 1771–1777. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, B.; Sharma, U.; Balasubramanian, K.; Kalaivani, M.; Kalra, V.; Jagannathan, N.R. Effect of creatine monohydrate in improving cellular energetics and muscle strength in ambulatory Duchenne muscular dystrophy patients: A randomized, placebo-controlled 31P MRS study. Magn. Reson. Imaging 2010, 28, 698–707. [Google Scholar] [CrossRef] [PubMed]
- Felber, S.; Skladal, D.; Wyss, M.; Kremser, C.; Koller, A.; Sperl, W. Oral creatine supplementation in Duchenne muscular dystrophy: A clinical and 31P magnetic resonance spectroscopy study. Neurol. Res. 2000, 22, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Davidson, Z.E.; Hughes, I.; Ryan, M.M.; Kornberg, A.J.; Cairns, A.G.; Jones, K.; Hutchence, M.; Sampaio, H.; Morrison, M.; Truby, H. Effect of a multicomponent nutritional supplement on functional outcomes for Duchenne muscular dystrophy: A randomized controlled trial. Clin. Nutr. 2021, 40, 4702–4711. [Google Scholar] [CrossRef]
- Farini, A.; Tripodi, L.; Villa, C.; Strati, F.; Facoetti, A.; Baselli, G.; Troisi, J.; Landolfi, A.; Lonati, C.; Molinaro, D.; et al. Microbiota dysbiosis influences immune system and muscle pathophysiology of dystrophin-deficient mice. EMBO Mol. Med. 2023, 15, e16244. [Google Scholar] [CrossRef]
- Kalkan, H.; Pagano, E.; Paris, D.; Panza, E.; Cuozzo, M.; Moriello, C.; Piscitelli, F.; Abolghasemi, A.; Gazzerro, E.; Silvestri, C.; et al. Targeting gut dysbiosis against inflammation and impaired autophagy in Duchenne muscular dystrophy. EMBO Mol. Med. 2023, 15, e16225. [Google Scholar] [CrossRef]
| Authors (year) | Sample | Nutritional Interventions (Duration) | Targeted Clinical Features | Main Outcomes |
|---|---|---|---|---|
| Passerieux et al. (2015) [44] | 53 patients, of which 26 were in the supplemented group (15 males and 11 females, mean age of 42.4 ± 10.2 years) and 27 were in the placebo group (13 males and 14 females, mean age of 37.6 ± 9.3 years). | Vitamin C, E, zinc gluconate, and selenomethionine (17 weeks) | Inflammation and oxidative stress | ↓ oxidative stress markers ↑ muscle function, muscle maximal voluntary contraction, and resistance |
| Sitzia et al. (2019) [45] | 5 patients (5 males, mean age of 36.8 ± 9.8 years) | Flavonoids and omega-3 (24 weeks) | Inflammation and oxidative stress | ↑ 6 min walk test and knee extension |
| Wilson et al. (2024) [46] | 20 patients (mean age 39.1 ± 11.6 years) | Vitamin C, E, zinc gluconate, and selenomethionine (17 weeks) | Inflammation and oxidative stress | ↓ muscle fat ↑ muscle mass and strength |
| Andersen et al. (2015) [47] | 41 patients (21 males and 20 females, range age 19–65 years) | Post exercise protein–carbohydrate supplementation (12 weeks) | Muscle atrophy | ↓ MPB |
| Walter et al. (2000) [48] | 12 patients (mean age 37 ± 19 years) | Creatine monohydrate (8 weeks) | Muscle strength deficit | no significant improvements |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quintiero, V.; Crisafulli, O.; Diotti, D.; Tupler, R.; Negro, M.; Lavaselli, E.; D’Antona, G. State-of-the-Art and Future Challenges for Nutritional Interventions in Facioscapulohumeral Dystrophy: A Narrative Review. Nutrients 2025, 17, 1056. https://doi.org/10.3390/nu17061056
Quintiero V, Crisafulli O, Diotti D, Tupler R, Negro M, Lavaselli E, D’Antona G. State-of-the-Art and Future Challenges for Nutritional Interventions in Facioscapulohumeral Dystrophy: A Narrative Review. Nutrients. 2025; 17(6):1056. https://doi.org/10.3390/nu17061056
Chicago/Turabian StyleQuintiero, Venere, Oscar Crisafulli, Daniele Diotti, Rossella Tupler, Massimo Negro, Emanuela Lavaselli, and Giuseppe D’Antona. 2025. "State-of-the-Art and Future Challenges for Nutritional Interventions in Facioscapulohumeral Dystrophy: A Narrative Review" Nutrients 17, no. 6: 1056. https://doi.org/10.3390/nu17061056
APA StyleQuintiero, V., Crisafulli, O., Diotti, D., Tupler, R., Negro, M., Lavaselli, E., & D’Antona, G. (2025). State-of-the-Art and Future Challenges for Nutritional Interventions in Facioscapulohumeral Dystrophy: A Narrative Review. Nutrients, 17(6), 1056. https://doi.org/10.3390/nu17061056








