Association Between Exercise Behavior Stages and Obesity Transition in Children and Adolescents: A Nationwide Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
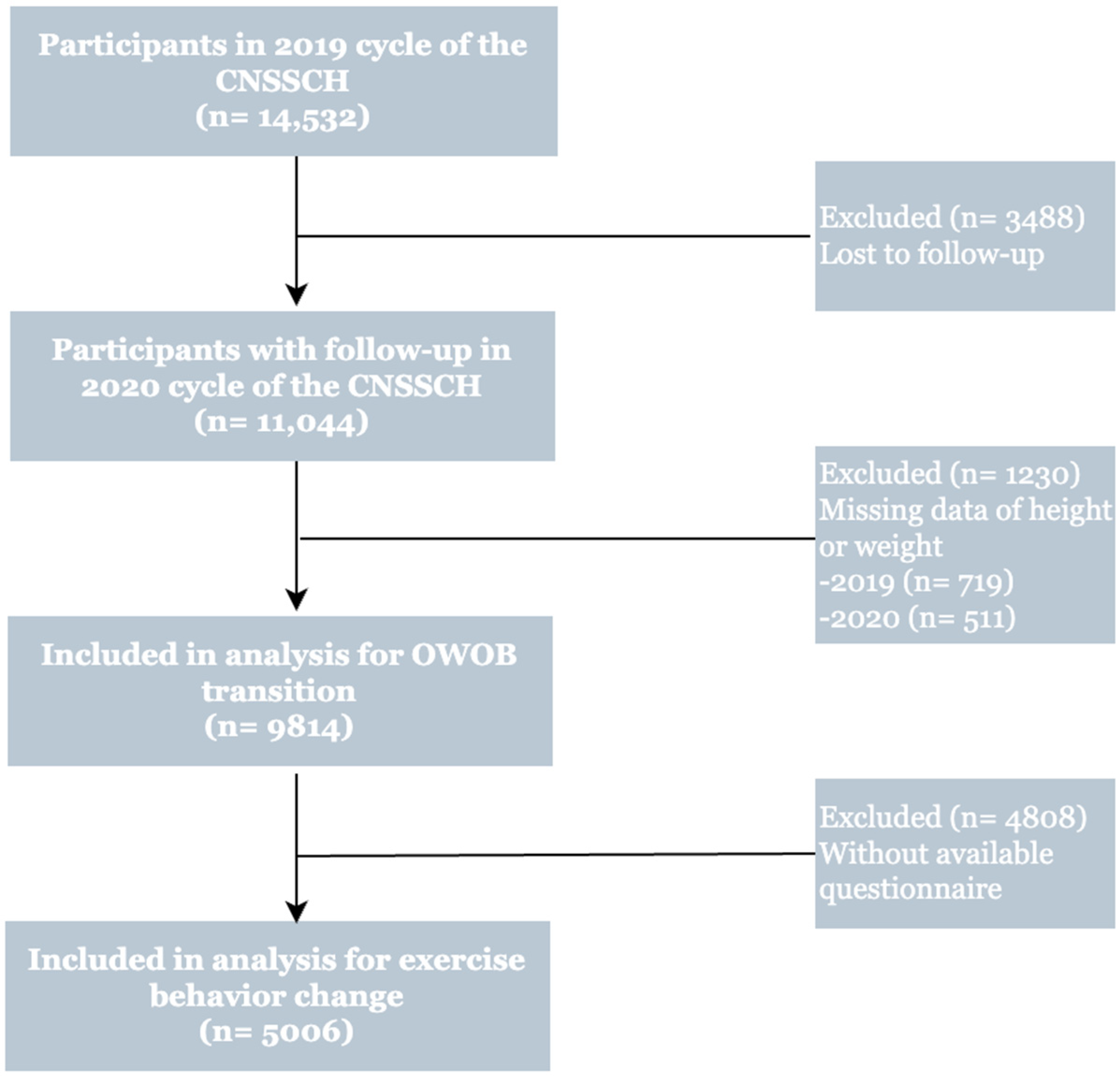
2.1. Study Design and Participants
2.2. Overweight (OW) and Obesity (OB) Measurement
2.3. Definition of the Stage of Change for Exercise Behavior Based on TTM
2.4. Questionnaire Survey
2.5. Statistical Analysis
3. Results
3.1. Overweight and Obesity Changes During the Follow-Up
3.2. Association Between Stages of Exercise Behavior Change and Risk of OWOB in 2019
3.3. Association Between Stages of Exercise Behavior Change and OWOB Transition During the Follow-Up
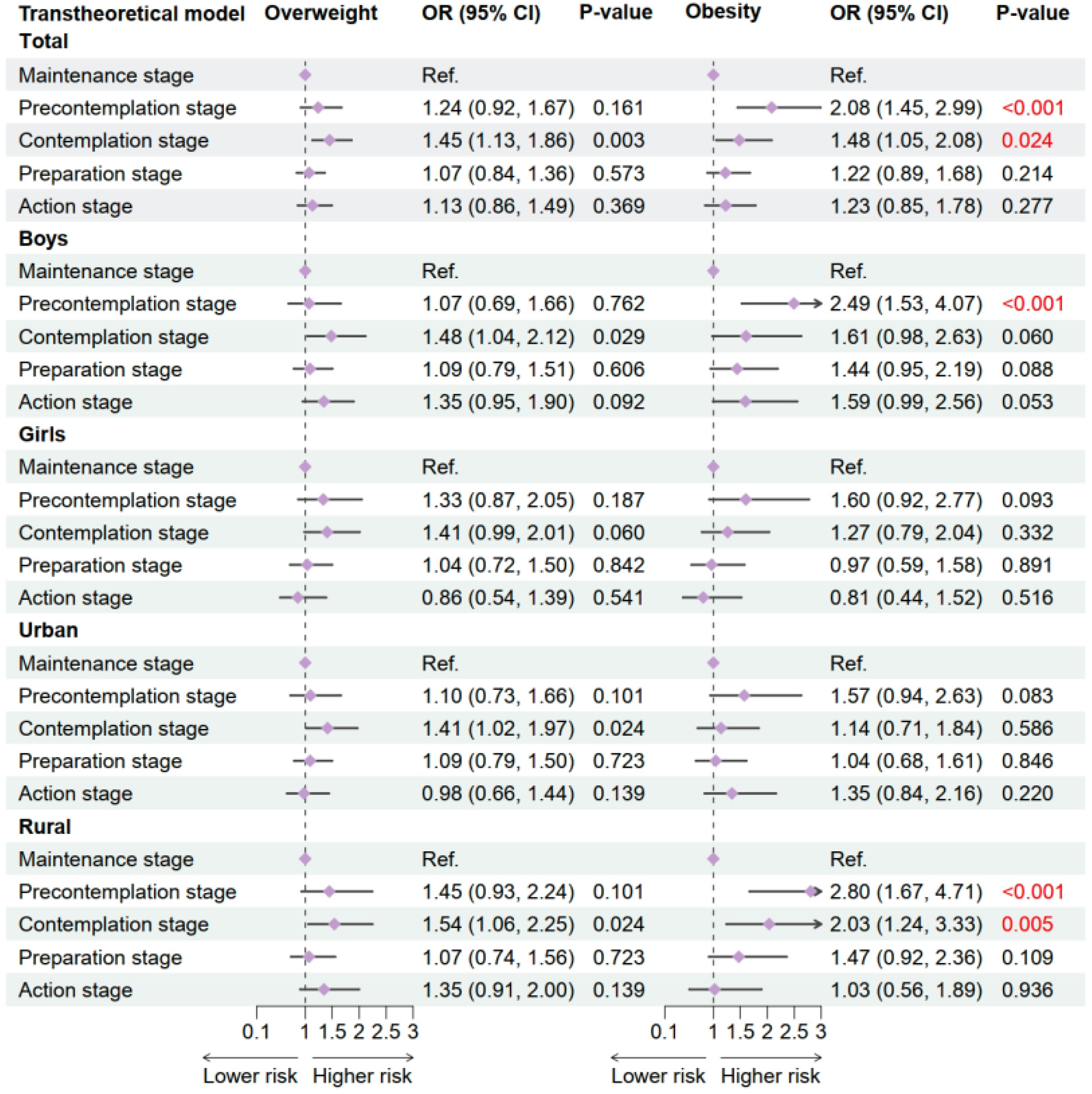
3.4. Interaction Effects of Exercise Behavior Stages with Gender and Region on OWOB Transitions During the Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OWOB | Overweight and Obesity |
| TTM | Transtheoretical Model |
| PA | Physical Activity |
References
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Lister, N.B.; Baur, L.A.; Felix, J.F.; Hill, A.J.; Marcus, C.; Reinehr, T.; Summerbell, C.; Wabitsch, M. Child and adolescent obesity. Nat. Rev. Dis. Primers 2023, 9, 24. [Google Scholar] [CrossRef]
- Hills, A.P.; Andersen, L.B.; Byrne, N.M. Physical activity and obesity in children. Br. J. Sports Med. 2011, 45, 866–870. [Google Scholar] [CrossRef]
- Elagizi, A.; Kachur, S.; Carbone, S.; Lavie, C.J.; Blair, S.N. A Review of Obesity, Physical Activity, and Cardiovascular Disease. Curr. Obes. Rep. 2020, 9, 571–581. [Google Scholar] [CrossRef]
- Marcus, B.H.; Simkin, L.R. The transtheoretical model: Applications to exercise behavior. Med. Sci. Sports Exerc. 1994, 26, 1400–1404. [Google Scholar] [CrossRef]
- Marcus, B.H.; Rossi, J.S.; Selby, V.C.; Niaura, R.S.; Abrams, D.B. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992, 11, 386–395. [Google Scholar] [CrossRef]
- Cheung, C.; Wyman, J.; Gross, C.; Peters, J.; Findorff, M.; Stock, H. Exercise behavior in older adults: A test of the transtheoretical model. J. Aging Phys. Act. 2007, 15, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Mastellos, N.; Gunn, L.H.; Felix, L.M.; Car, J.; Majeed, A. Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst. Rev. 2014, 2014, CD008066. [Google Scholar] [CrossRef] [PubMed]
- Oba, T.; Takano, K.; Katahira, K.; Kimura, K. Revisiting the Transtheoretical Model for Physical Activity: A Large-Scale Cross-Sectional Study on Japanese-Speaking Adults. Ann. Behav. Med. 2024, 58, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Kleis, R.R.; Hoch, M.C.; Hogg-Graham, R.; Hoch, J.M. The Effectiveness of the Transtheoretical Model to Improve Physical Activity in Healthy Adults: A Systematic Review. J. Phys. Act. Health 2021, 18, 94–108. [Google Scholar] [CrossRef]
- de Freitas, P.P.; de Menezes, M.C.; Dos Santos, L.C.; Pimenta, A.M.; Ferreira, A.V.M.; Lopes, A.C.S. The transtheoretical model is an effective weight management intervention: A randomized controlled trial. BMC Public Health 2020, 20, 652. [Google Scholar] [CrossRef]
- Tuah, N.A.; Amiel, C.; Qureshi, S.; Car, J.; Kaur, B.; Majeed, A. Transtheoretical model for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst. Rev. 2011, 2014, CD008066. [Google Scholar]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Hashemzadeh, M.; Rahimi, A.; Zare-Farashbandi, F.; Alavi-Naeini, A.M.; Daei, A. Transtheoretical Model of Health Behavioral Change: A Systematic Review. Iran J. Nurs. Midwifery Res. 2019, 24, 83–90. [Google Scholar] [PubMed]
- Selçuk-Tosun, A.; Zincir, H. The effect of a transtheoretical model-based motivational interview on self-efficacy, metabolic control, and health behaviour in adults with type 2 diabetes mellitus: A randomized controlled trial. Int. J. Nurs. Pract. 2019, 25, e12742. [Google Scholar] [CrossRef] [PubMed]
- Monahan, K.; Paiva, A.; Blissmer, B.; Sacco, A.; Robbins, M. Transtheoretical Model for Exercise: Measure Redevelopment and Assessing the Role of Barriers in a Diverse Population. Am. J. Health Promot. 2024, 38, 186–196. [Google Scholar] [CrossRef]
- Pudkasam, S.; Polman, R.; Pitcher, M.; Fisher, M.; Chinlumprasert, N.; Stojanovska, L.; Apostolopoulos, V. Physical activity and breast cancer survivors: Importance of adherence, motivational interviewing and psychological health. Maturitas 2018, 116, 66–72. [Google Scholar] [CrossRef]
- Jeon, D.J.; Kim, K.J.; Heo, M. Factors Related to Stages of Exercise Behavior Change among University Students Based on the Transtheoretical Model. J. Phys. Ther. Sci. 2014, 26, 1929–1932. [Google Scholar] [CrossRef]
- Salvo, D.; Aguilar-Farias, N.; Jauregui, A.; Ramirez Varela, A. Sex and age disparities in physical activity among Brazilian adolescents: Nature or nurture? J. Pediatr. (Rio J.) 2020, 96, 4–7. [Google Scholar] [CrossRef]
- Zhang, J.; Xiao, S.; Shi, L.; Xue, Y.; Zheng, X.; Dong, F.; Xue, B.; Zhang, C. Differences in Health-Related Quality of Life and Its Associated Factors Among Older Adults in Urban and Rural Areas. Risk Manag. Healthc. Policy 2022, 15, 1447–1457. [Google Scholar] [CrossRef]
- Song, Y.; Ma, J.; Wang, H.J.; Wang, Z.; Lau, P.W.; Agardh, A. Age at spermarche: 15-year trend and its association with body mass index in Chinese school-aged boys. Pediatr. Obes. 2016, 11, 369–374. [Google Scholar] [CrossRef]
- Garg, S. Gender differences in pathways influencing leisure time physical activity: A structural equation analysis. Diabetes Metab. Syndr. 2023, 17, 102761. [Google Scholar] [CrossRef]
- Liu, M.; Tang, W.; Zhang, Y.; Wang, Y.; Kangzhuo, B.; Li, Y.; Liu, X.; Xu, S.; Ao, L.; Wang, Q.; et al. Urban-rural differences in the association between long-term exposure to ambient air pollution and obesity in China. Environ. Res. 2021, 201, 111597. [Google Scholar] [CrossRef]
- Song, X.; Zhou, B.; Baird, S.; Lu, C.; Ezzati, M.; Chen, L.; Liu, J.; Zhang, Y.; Wang, R.; Ma, Q.; et al. Trends and inequalities in thinness and obesity among Chinese children and adolescents: Evidence from seven national school surveys between 1985 and 2019. Lancet Public Health 2024, 9, e1025–e1036. [Google Scholar] [CrossRef]
- Zhou, Y.; Yu, P.; Zhang, Y.; Wang, T.; Wang, A. Distinct Patterns of Urban-Rural and Sex Disparities in Children’s BMI Trajectories From 2013 to 2018. Front. Public Health 2021, 9, 689021. [Google Scholar] [CrossRef]
- Lizana, P.A.; Aballay, J.; Vicente-Rodríguez, G.; Gómez-Bruton, A. Low interest in physical activity and higher rates of obesity among rural teachers. Work 2020, 67, 1015–1022. [Google Scholar] [CrossRef]
- Anderson, Y.C.; Wynter, L.E.; Grant, C.C.; Stewart, J.M.; Cave, T.L.; Wild, C.E.; Derraik, J.G.; Cutfield, W.S.; Hofman, P.L. Physical activity is low in obese New Zealand children and adolescents. Sci. Rep. 2017, 7, 41822. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Screening for Overweight and Obesity among School-Age Children and Adolescents; National Health Commission of the People’s Republic of China: Beijing, China, 2018; pp. 1–3. [Google Scholar]
- Reed, G.R.; Velicer, W.F.; Prochaska, J.O.; Rossi, J.S.; Marcus, B.H. What makes a good staging algorithm: Examples from regular exercise. Am. J. Health Promot. 1997, 12, 57–66. [Google Scholar] [CrossRef]
- Jiménez-Zazo, F.; Romero-Blanco, C.; Castro-Lemus, N.; Dorado-Suárez, A.; Aznar, S. Transtheoretical Model for Physical Activity in Older Adults: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9262. [Google Scholar] [CrossRef]
- Si, Q. Study on phase change and mental decisive factors of sport exercise behavior of college students. China Sport Sci. 2005, 25, 76–83. [Google Scholar]
- Si, Q. Path analysis on exploring the relationship between psychological determinants in stage transition of college students. China Sport Sci. 2006, 26, 29–32. [Google Scholar]
- Si, Q.; Yu, K.; Li, F.; Lee, H.; Maddalozzo, G.F.; Cardinal, B.J. Examining exercise behavior among Chinese students with hearing impairments: Application of the transtheoretical model. Med. Sci. Sports Exerc. 2011, 43 (Suppl. 5), S223. [Google Scholar] [CrossRef]
- Si, Q.; Yu, K.; Loprinzi, P.D.; Cardinal, B.J.; Lee, H.; Yan, Z.; Li, F.; Liu, H. Promoting exercise behavior among Chinese youth with hearing loss: A randomized controlled trial based on the transtheoretical model. Psychol. Rep. 2011, 109, 896–906. [Google Scholar] [CrossRef]
- Dong, Y.; Chen, M.; Chen, L.; Wen, B.; Yang, Y.; Wang, Z.; Ma, Y.; Song, Y.; Ma, J.; Lau, P.W.C. Individual-, Family-, and School-Level Ecological Correlates With Physical Fitness Among Chinese School-Aged Children and Adolescents: A National Cross-Sectional Survey in 2014. Front. Nutr. 2021, 8, 684286. [Google Scholar] [CrossRef]
- Gouran, P.; Nadimi-Shahraki, M.H.; Rahmani, A.M.; Mirjalili, S. An Effective Imputation Method Using Data Enrichment for Missing Data of Loop Detectors in Intelligent Traffic Control Systems. Remote Sens. 2023, 15, 3374. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef]
- Surís, A.M.; Trapp, M.C.; DiClemente, C.C.; Cousins, J. Application of the transtheoretical model of behavior change for obesity in Mexican American women. Addict. Behav. 1998, 23, 655–668. [Google Scholar] [CrossRef]
- Wu, Y.K.; Chu, N.F. Introduction of the transtheoretical model and organisational development theory in weight management: A narrative review. Obes. Res. Clin. Pract. 2015, 9, 203–213. [Google Scholar] [CrossRef]
- Boff, R.M.; Dornelles, M.A.; Feoli, A.M.P.; Gustavo, A.D.S.; Oliveira, M.D.S. Transtheoretical model for change in obese adolescents: MERC randomized clinical trial. J. Health Psychol. 2020, 25, 2272–2285. [Google Scholar] [CrossRef]
- Carvalho, G.X.; Nunes, A.P.N.; Moraes, C.L.; Veiga, G.V.D. Body image dissatisfaction and associated factors in adolescents. Cien Saude Colet. 2020, 25, 2769–2782. [Google Scholar] [CrossRef]
- Flannery, M. Self-Determination Theory: Intrinsic Motivation and Behavioral Change. Oncol. Nurs. Forum 2017, 44, 155–156. [Google Scholar]
- Papakonstantinou, E.; Oikonomou, C.; Nychas, G.; Dimitriadis, G.D. Effects of Diet, Lifestyle, Chrononutrition and Alternative Dietary Interventions on Postprandial Glycemia and Insulin Resistance. Nutrients 2022, 14, 823. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D. A review of the carbohydrate-insulin model of obesity. Eur. J. Clin. Nutr. 2017, 71, 323–326, Erratum in Eur. J. Clin. Nutr. 2017, 71, 679. [Google Scholar] [CrossRef]
- Marson, E.C.; Delevatti, R.S.; Prado, A.K.; Netto, N.; Kruel, L.F. Effects of aerobic, resistance, and combined exercise training on insulin resistance markers in overweight or obese children and adolescents: A systematic review and meta-analysis. Prev. Med. 2016, 93, 211–218. [Google Scholar] [CrossRef]
- Batsis, J.A.; Villareal, D.T. Sarcopenic obesity in older adults: Aetiology, epidemiology and treatment strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Roemmich, J.N.; Rogol, A.D. Hormonal changes during puberty and their relationship to fat distribution. Am. J. Hum. Biol. 1999, 11, 209–224. [Google Scholar] [CrossRef]
- Cheah, H.F. Using shanghai municipal data to examine whether student sacrifice exercise in response to academic pressure. Heliyon 2024, 10, e33527. [Google Scholar] [CrossRef] [PubMed]
- Young, M.D.; Plotnikoff, R.C.; Collins, C.E.; Callister, R.; Morgan, P.J. Social cognitive theory and physical activity: A systematic review and meta-analysis. Obes. Rev. 2014, 15, 983–995. [Google Scholar] [CrossRef] [PubMed]
- Armitage, J.M.; Wang, R.A.H.; Davis, O.S.P.; Bowes, L.; Haworth, C.M.A. Peer victimisation during adolescence and its impact on wellbeing in adulthood: A prospective cohort study. BMC Public Health 2021, 21, 148. [Google Scholar] [CrossRef]
- Kanaan, M.N.; Afifi, R.A. Gender differences in determinants of weight-control behaviours among adolescents in Beirut. Public Health Nutr. 2010, 13, 71–81. [Google Scholar] [CrossRef]
- Aina Mardiah, B.; Hazizi, A.; Nasir, M.M.; Zaitun, Y.; Jan, J.H. Gender Differences in the Attitude and Strategy towards Weight Control among Government Employees in Penang, Malaysia. Iran J. Public Health 2012, 41, 28–36. [Google Scholar]
- Han, J.; Kim, S.; Park, C.G. Gender Differences in Risk Factors Influencing Unhealthy Weight Control Behaviors among Adolescents. West J. Nurs. Res. 2020, 42, 690–697. [Google Scholar] [CrossRef]
- Kelly, D.M.; Jones, T.H. Testosterone and obesity. Obes. Rev. 2015, 16, 581–606. [Google Scholar] [CrossRef]
- Guddal, M.H.; Stensland, S.Ø.; Småstuen, M.C.; Johnsen, M.B.; Zwart, J.A.; Storheim, K. Physical activity and sport participation among adolescents: Associations with mental health in different age groups. Results from the Young-HUNT study: A cross-sectional survey. BMJ Open 2019, 9, e028555. [Google Scholar] [CrossRef]
- Hellström, L.; Beckman, L. Adolescents’ perception of gender differences in bullying. Scand. J. Psychol. 2020, 61, 90–96. [Google Scholar] [CrossRef]
- Wang, W.; Zhang, Y.; Lin, B.; Mei, Y.; Ping, Z.; Zhang, Z. The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China. Int. J. Environ. Res. Public Health 2020, 17, 3848. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Liang, Z.; Zhou, Q.; Tuersun, Y.; Liu, S.; Wang, C.; Xie, Y.; Wang, X.; Wu, Z.; Qian, Y. Decomposition and Comparative Analysis of Urban-Rural Disparities in eHealth Literacy Among Chinese University Students: Cross-Sectional Study. J. Med. Internet Res. 2025, 27, e63671. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.-J.; Li, F.; Hu, Y.-F.; Li, C.-F.; Yuan, S.; Song, Y.; Zheng, M.; Gong, J.; He, Q.-Q. Improving the Metabolic and Mental Health of Children with Obesity: A School-Based Nutrition Education and Physical Activity Intervention in Wuhan, China. Nutrients 2020, 12, 194. [Google Scholar] [CrossRef] [PubMed]



| Exercise Behaviour Stages | Definition |
|---|---|
| Maintenance stage | I have been exercising for more than 6 months |
| Precontemplation stage | I don’t plan to start exercising |
| Contemplation stage | I’m planning to start in the next 6 months |
| Preparation stage | I’m planning to start in the next 30 days |
| Action stage | I have been exercising for more less than 6 months |
| Characterictics | Total (n = 5006) | Boys (n = 2501) | Girls (n = 2505) | p-Value |
|---|---|---|---|---|
| Residence | <0.001 | |||
| Urban | 2754 (55.0) | 1321 (52.8) | 1433 (57.2) | |
| Rural | 2252 (45.0) | 1180 (47.2) | 1072 (42.8) | |
| Incidence | <0.001 | |||
| Overweight | 723 (14.3) | 438 (17.3) | 285 (11.3) | |
| Obesity | 573 (11.3) | 309 (12.2) | 264 (10.5) | |
| Transition | <0.001 | |||
| Overweight | 309 (6.2) | 172 (6.9) | 137 (5.5) | |
| Obesity | 508 (10.1) | 267 (10.7) | 241 (9.6) | |
| Exercise behavior stages | <0.001 | |||
| Maintenance stage | 502 (10.0) | 224 (9.0) | 278 (11.1) | |
| Precontemplation stage | 690 (13.8) | 266 (10.6) | 424 (16.9) | |
| Contemplation stage | 883 (17.6) | 410 (16.4) | 473 (18.9) | |
| Preparation stage | 546 (10.9) | 286 (11.4) | 260 (10.4) | |
| Action stage | 2385 (47.6) | 1315 (52.6) | 1070 (42.7) | |
| Specific indicators of exercise behavior stages | ||||
| I am currently actively participating in physical exercise | 3824 (75.3) | 2022 (52.9) | 1802 (47.1) | <0.001 |
| I will participate more actively in physical activities in the next six months | 2863 (56.4) | 1524 (53.2) | 1339 (46.8) | <0.001 |
| I currently maintain regular physical activity | 3436 (67.7) | 1818 (52.9) | 1618 (47.1) | <0.001 |
| I have been engaging in regular physical activity for the past six months | 4212 (83.0) | 2108 (50.0) | 2104 (50.0) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Z.; Dang, J.; Cai, S.; Liu, Y.; Shi, D.; Li, J.; Zhang, Y.; Chen, Z.; Huang, T.; Yang, Y.; et al. Association Between Exercise Behavior Stages and Obesity Transition in Children and Adolescents: A Nationwide Follow-Up Study. Nutrients 2025, 17, 2608. https://doi.org/10.3390/nu17162608
Sun Z, Dang J, Cai S, Liu Y, Shi D, Li J, Zhang Y, Chen Z, Huang T, Yang Y, et al. Association Between Exercise Behavior Stages and Obesity Transition in Children and Adolescents: A Nationwide Follow-Up Study. Nutrients. 2025; 17(16):2608. https://doi.org/10.3390/nu17162608
Chicago/Turabian StyleSun, Ziyue, Jiajia Dang, Shan Cai, Yunfei Liu, Di Shi, Jiaxin Li, Yihang Zhang, Ziyue Chen, Tianyu Huang, Yang Yang, and et al. 2025. "Association Between Exercise Behavior Stages and Obesity Transition in Children and Adolescents: A Nationwide Follow-Up Study" Nutrients 17, no. 16: 2608. https://doi.org/10.3390/nu17162608
APA StyleSun, Z., Dang, J., Cai, S., Liu, Y., Shi, D., Li, J., Zhang, Y., Chen, Z., Huang, T., Yang, Y., Hu, P., Ma, J., Chen, T., & Song, Y. (2025). Association Between Exercise Behavior Stages and Obesity Transition in Children and Adolescents: A Nationwide Follow-Up Study. Nutrients, 17(16), 2608. https://doi.org/10.3390/nu17162608








