1. Introduction
An adequate diet during lactation is important for maintaining good health, not only for the mother but also for her infant, as it ensures appropriate development by providing personalized and unique nourishment, facilitating essential nutrients and biologically active components [
1].
The macronutrient, micronutrient, and lipid composition of human milk (HM) depends on maternal nutrient intake, maternal nutrient stores, and nutrient production in the mammary gland [
2]. Therefore, an adequate diet for the mother could lead to a better nutritional balance of diverse micronutrients in her breast milk. In this sense, several reviews have reported on the relationship between maternal dietary intake and HM composition [
3,
4,
5,
6,
7]. For example, the concentration of water-soluble vitamins, as well as vitamins A and E, in HM is closely related to the maternal diet, as is the concentration of selenium, iodine, and the fatty acid (FA) profile [
6,
8,
9,
10]. The maternal nutrient status, determined by the nutrient concentration in plasma and erythrocytes rather than by body mass index (BMI), also showed relations with diverse nutrients in HM [
2,
3,
10,
11,
12,
13,
14], such as docosahexaenoic acid (DHA), linolenic acid, linoleic acid, iron, vitamin A, and vitamin B12.
The nutritional requirements of the lactating mother are high during lactation. Hence, achieving nutritional adequacy might be difficult, as the increased demand established during gestation not only continues but also increases [
1,
9,
15]. Even so, well-nourished mothers are generally able to produce HM containing all vitamins, minerals, and essential FAs needed by their healthy full-term infants [
1,
9].
However, in special circumstances, the nutritional ideality of HM might not be sufficient [
16,
17]. Preterm infants are born with nutritional deficits because of the early deprivation of maternal supply and the immaturity of their organs (e.g., the gut and brain, among others), which affects nutrient absorption, utilization, and retention [
18]. Nevertheless, mother’s fortified own milk is the first choice of enteral feeding for preterm infants in order to meet their special nutritional needs [
17,
19]. However, mothers of preterm infants experience major challenges in feeding their infants and face obstacles that mothers of healthy full-term infants do not have to face [
20,
21].
In general, the postpartum period is a sensitive time for nutritional inadequacies [
22,
23,
24]. Mother’s needs are relegated to second place due to the significant changes that parents face, such as lack of sleep and increased stress levels as a consequence of the high demands for their newborn baby [
25,
26]. For instance, Poulain et al. [
22] observed that snacking was more frequent during breastfeeding than during pregnancy and after weaning. This was attributed to the extra time spent on infant care, which, in turn, led to less attention being paid to the mother’s nutritional needs.
A premature birth puts parents into a particularly worrying and stressful situation, as they must deal with the challenges of an extended hospital stay, as well as the potential death of or future consequences for their newborn child [
27]. In this regard, most Level III neonatal intensive care units (NICUs) in hospitals designated as being part of the “Baby-friendly Hospital Initiative (BFHI)” follow the recommendation of the BFHI to extend neonatal wards and, therefore, greatly promote 24 h parental presence [
28]. Consequently, the continuous presence of parents in the neonatal unit leads to better care for the premature infant. However, this may mean that mothers of hospitalized very premature infants (MHVPIs) do not eat properly and, consequently, that they do not achieve the specific nutritional needs of their vulnerable infants [
29]. Usually, after being discharged following the birth of their child, they are excluded from the hospital meal supply. In addition, it is not uncommon for MHVPIs to develop complications after giving birth, prolonging their recovery and, therefore, their ability to feed properly.
Maternal intake has been widely investigated in healthy lactating women with healthy full-term babies [
23,
30,
31,
32]. However, MHVPIs face special circumstances, which might influence their dietary intake and, consequently, HM composition. To our knowledge, the diet and nutritional status of MHVPIs during their infant’s hospitalization, as a particular population, has rarely been investigated [
23,
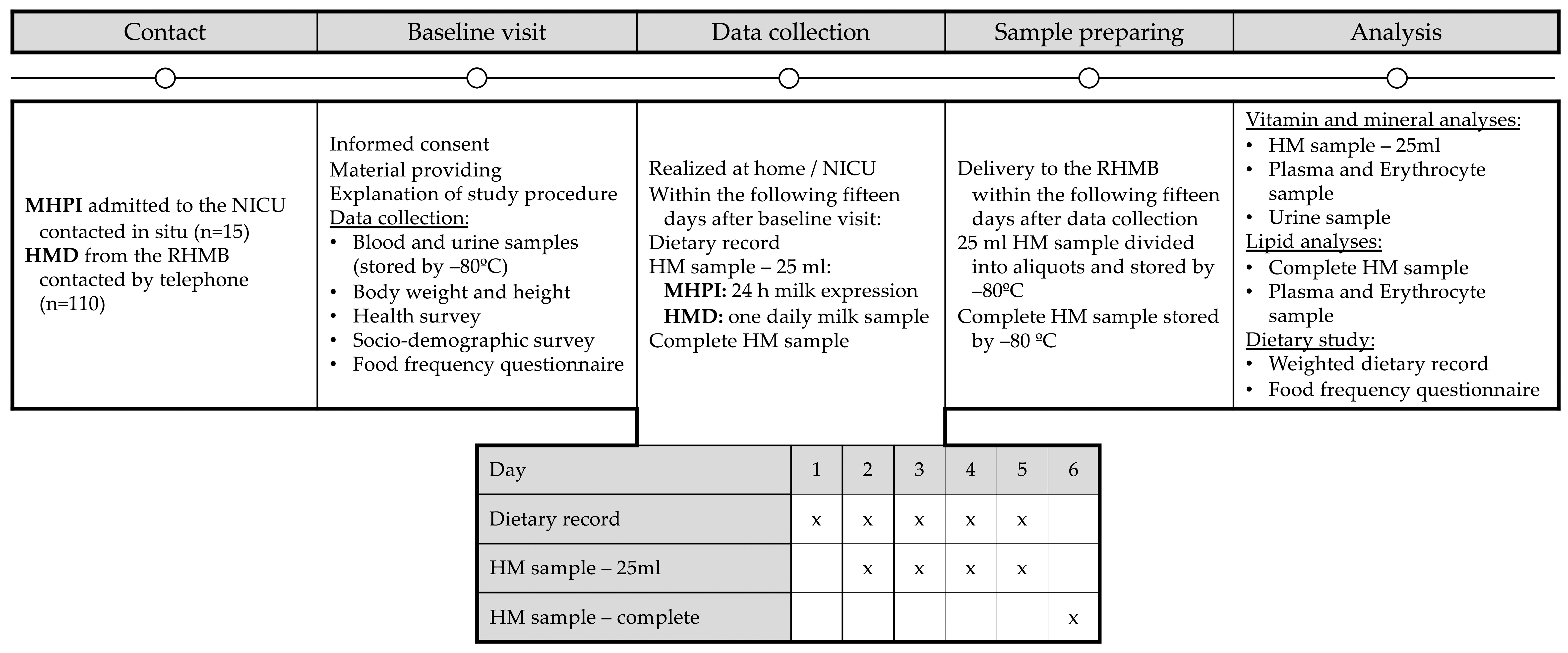
33]. Hence, the aim of our study was to determine macronutrient, micronutrient, and FA intakes, as well as the status of nutrients in plasma, erythrocytes, and urine samples from MHVPIs. The results were compared with those of a group of HM donors (HMDs). Finally, associations were established between the MHVPIs’ nutritional intake and status and the corresponding concentration of nutrients in HM.
3. Results
Table 1 shows the baseline characteristics of the 15 MHVPIs. As expected, gestational weight gain was low. A high percentage had twin pregnancies and around 40% of the MHVPIs were not originally from Spain. On the other hand, most of the MHVPIs had carried out university-level studies. In
Tables S1 and S2, further characteristics of the MHVPIs and HMDs can be observed. Baseline characteristics (
Table S1) did not show significant differences between the two study groups except for country of origin, with MHVPIs more likely to come from a country other than Spain; the number of women currently working, which was found to be more elevated in HMDs; and a lower gestational weight gain in MHVPIs. However, because of premature birth, infant and lactation-related characteristics (
Table S2) showed that the infants of MHVPIs had a lower gestational age, breastfeeding duration, birth weight, and current weight compared with the infants from HMDs, as well as significant differences in their respective weight percentiles. In the MHVPI group, higher frequencies of twin pregnancy and the use of double electric breast pumps were observed.
The pharmacological supplement consumption of MHVPIs during pregnancy and lactation are presented in
Table 2. During pregnancy, the majority (93.3%) took iodine, folic acid, and vitamin B12 supplements. This consumption was maintained during lactation by 86.7% of the women at the time of the study. Vitamin A and E intake, as well as calcium supplementation intake, were low (0 to 20%) during gestation, although this increased during lactation. Additionally,
Table S3 shows differences in the consumption of pharmacological supplements between the study groups. Aside from a higher daily dose of vitamin B9 during pregnancy in MHVPIs compared to HMDs, no other differences were found regarding the frequency and daily dosage of supplements during pregnancy and lactation.
Table 3 shows the daily nutrient intake, determined from the 5-day dietary record, and the prevalence of inadequate nutrient intake relative to the thresholds compiled from various sources, including the harmonized average requirement (H-AR) [
15], the acceptable macronutrient distribution ranges (Institute of Medicine) [
38], and Ortega et al. [
37]. For comparison, the table also includes the median intake of various nutrients, based on the results of different studies from industrialized countries that examined lactating mothers of term infants, as provided by Di Maso et al. [
31] in their systematic review.
Median total energy intake was 2272.6 Kcal (kilocalories), which is below the recommended dietary intake of 2430 Kcal proposed by Ortega et al. for lactating women with a sedentary lifestyle. Almost 70% of MHVPIs had an inadequate energy intake. Median daily protein intake exceeded the recommended daily protein intake of 66 g by almost 30 g. Protein intake below this value was, therefore, not observed. The median percentage of energy from carbohydrates was below its acceptable macronutrient distribution range, whereas the median percentage of energy from fat was above its acceptable macronutrient distribution ranges. Hence, we observed that more than 70% of MHVPIs showed a deficit, whereas almost 90% exceeded the ranges in relation of percentage of energy from carbohydrates and fat, respectively. The median percentages of total energy from protein and omega 3 polyunsaturated fatty acids (PUFAs) were within their respective ranges. Regardig vitamins and minerals, more than 80% of MHVPIs showed an inadequate intake for vitamin D and around 40% demonstrated an inadequate intake of iodine, as well as vitamins B8, B9, C, and E. On the other hand, except for the percentages of energy from carbohydrates, all nutrient intakes were observed to be above the medians provided by Di Maso et al. [
31]. Considering study group differences, the daily nutrient intake from MHVPI’s of almost all nutrients was similar, as shown in
Table S4. Disparities were only found for the percentage of caloric intake from omega 3 FAs, the intake of DHA, and, hence, the sum of eicosapentaenoic acid (EPA) and DHA intake, as well as in vitamin B12, all of which showed a higher intake in MHVPIs. Furthermore, between the two investigated groups, no differences were observed in relation to the prevalence of inadequate micronutrient intake (
Table S5).
Table 4 presents the daily number of food servings from five food groups, the HEI, and the intake of dietary supplements and iodized salt, all determined from the 5-day dietary record. The table also includes the number of food servings as assessed by the food consumption frequency questionnaire. Considering the daily recommended servings for lactating mothers provided by Ortega et al. (2015) [
42] and shown in
Table 4, MHVPIs did not meet the recommended intake of dairy; grains, legumes, and nuts; vegetables and greens; and fruits, independent of the method used to assess food frequency (5-day dietary record or food consumption questionnaire). Furthermore, the median HEI score was 61.9 points. No differences in food servings were observed between MHVPIs and HMDs, according to the results from either the 5-day dietary record (
Table S6) or the food consumption frequency questionnaire (
Table S7).
Table 5 describes the FA composition (g/100 g of total fat) in the erythrocytes and plasma of 14 MHVPIs. In both samples, i.e., plasma and erythrocytes, the highest concentration of saturated fatty acids (SFAs) was observed for palmitic acid (C16:0), whereas oleic acid (C18:1
cis-9) was the most abundant monounsaturated fatty acid (MUFA). In erythrocytes, C20:4 presented the greatest concentration within the studied PUFAs compared with C18:2 in plasma. Several FA concentrations presented differences between HMDs and MHVPIs, as observed in
Table S8. In both blood components, the concentration of DMA palmitic acid (C16:0) was higher in HMDs, whereas the
cis vaccenic acid (C18:1
cis-11), dihomo-γ-linolenic acid (C20:3), DHA (C22:6), and the total omega 3 PUFAs were higher in MHVPIs. Furthermore, in erythrocytes, a higher concentration was found for DMA C18:0, arachidonic acid (20:4), and total DMAs in HMDs. On the other hand, MHVPIs presented elevated concentrations of lignoceric acid (C24:0) and linoleic acid (C18:2) in erythrocytes, as well as palmitoleic acid (C16:1
cis-9) and medium-chain FAs (MFCAs) in plasma.
Concentrations of nutrients and biochemical determinations in the erythrocyte, plasma, and urine samples of MHVPIs are shown in
Table 6. Riboflavin deficiency in erythrocytes was 100%, when considering riboflavin concentration; however, this value was only 33.3%, when considering the erythrocyte glutathione reductase activity coefficient. In plasma, a lack of vitamin D was observed for all 15 MHVPIs and for vitamin E in 73.3%. Methylmalonic acid, a vitamin B12 deficiency marker, was used to identify that more than 70% of MHVPIs were vitamin B12 deficient. In contrast, when considering cobalamin and holotranscobalamin II concentrations, vitamin B12 deficiency was inexistent. Scurvy and a lack of vitamin A were not detected. Differences between study groups (
Table S9) were observed in erythrocytes for nicotinamide, which was higher in MHVPIs, while pantothenic acid was more elevated in HMDs. On the other hand, the concentration of retinol, ascorbic acid, y-tocopherol, total cholesterol, TAG, and LDL were more elevated in MHVPIs’ plasma. However, cobalamin in plasma, as well as creatinine and phosphorus concentration in urine, were shown to be greater in HMDs.
Table 7 shows the HM lipid class profile, TAG molecular species content, and relative composition of the phospholipids from MHVPIs (
n = 12). As expected, the most abundant lipid class was TAGs. Among these, the highest concentrations were observed in those with a molecular species of 52 carbon atoms (CNs), followed by the TAGs with 54 CNs. A comparison between MHVPIs and HMDs is shown in
Table S10. The concentration of TAGs with a molecular species of 28, 30, and 32 CNs was higher in HMDs. Regarding phospholipid distribution; sphingomyelin constituted the majority in HMDs but was shown to be the lowest phospholipid in MHVPIs, where the main phospholipid groups consisted of phosphatidylcholine and phosphatidylethanolamine. All the phospholipids showed differences between the two study groups.
The FA composition (g/100 g of total fat) in HM of MHVPIs (
n = 14) is presented in
Table 8. Compared to the European references and the worldwide values [
12,
52], we observed that the HM concentrations in MHVPIs were lower regarding SFAs, but higher for oleic acid (C18:1
cis-9 (n9)), omega-6 PUFAs, and linolenic acid (C18:3). In MHVPIs, compared with HMDs (
Table S11), higher concentrations were found for the PUFAs eicosadienoic acid (C20:2), dihomo-γ-linolenic acid (C20:3), and linolenic acid (C18:3), as well as for the concentrations of total PUFAs, very long-chain fatty acids (VLCFAs), and
n-6 PUFAs, whereas lower concentrations of caproic acid (C6:0) and short-chain fatty acids (SCFAs) were found.
Table 9 shows the macronutrient, vitamin and mineral composition of the HM of MHVPIs. When compared to the references provided [
14,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68] within
Table 9, MHVPIs showed higher concentrations of carbohydrates, proteins, free riboflavin, cobalamin, and iodine. Furthermore, total vitamin C, vitamer D
3, and phosphorus levels were within their reference ranges. However, nicotinamide and calcium concentration were far below the reference values. The differences between MHVPIs and HMDs are shown in
Table S12. As concerns the HM of MHVPIs, higher concentrations were determined for protein, selenium and iodine, where the difference between the two study groups was considerable.
The associations between HM nutrient concentration and nutrient intake, concentration in plasma, erythrocytes, and urine, and study group (MHVPIs–HMDs) are described in
Table 10. Independent of nutrient intake, plasma, erythrocyte, and urine concentration, as well as breastfeeding duration, the MHVPI group was associated with higher HM concentration of proteins, vitamer 25(OH)D
3, iodine, selenium,
n-3 PUFAs, VLCFAs, and the FAs dihomo-γ-linolenic acid (C20:3) and linolenic acid (C18:3); however, it was also associated with lower concentrations of free riboflavin, dehydroascorbic acid, palmitoleic acid (C16:1
cis-9), and
cis vaccenic acid (C18:1
cis-11). Associations were also observed between diverse HM nutrient concentrations and nutrient intake, as well as concentrations of plasma, erythrocytes, and urine, regardless of whether they were MHVPI or HMD and regardless of breastfeeding duration.
4. Discussion
This cross-sectional study investigated the nutrient intake and plasma, erythrocyte, and urine content of mothers whose preterm infants were admitted to the NICU of the “12 de Octubre” University Hospital in Madrid, Spain. There is a wide range of studies assessing the intake of lactating mothers [
23,
30,
31,
32] and, to a much lesser extent, their plasma, erythrocyte and urine nutritional status [
2,
12,
13,
14]. However, MHVPIs are a special population since they face circumstances related to their personal health, their preterm child’s health, and hospitalization, which goes beyond normal adaptations to the postpartum period [
27].
Hence, to the best of our knowledge, this is the first study assessing not only dietary intake [
33] using dietary reference intakes [
15,
37,
38] but also by evaluating nutrient concentration in plasma, erythrocytes, and urine in MHVPIs of a large number of nutrients. Additionally, it provides a detailed analysis of their milk, including macronutrients, lipid classes, molecular species of TAGs, phospholipids, FAs, vitamins, and minerals. The results were further compared with the concentrations found in HM from donors, as they provide the second-best option to nourish a preterm infant when a mother’s own milk is not available [
17,
19]. Differences in HM concentration, related to prematurity rather than dietary intake, plasma and erythrocyte content, or breastfeeding duration were also assessed.
Considering the available dietary reference intakes, our results revealed that around 40% of MHVPIs showed low intakes of total energy, iodine, and vitamins B8, B9, C, D, and E, whereas an adequate percentage of energy from omega 3 PUFAs was observed. Intake of proteins was considerably higher than the recommended intake from Ortega et al. [
37], although the percentage of energy from proteins was within the IOM acceptable macronutrient distribution ranges [
38]. However, the percentage of energy from carbohydrates was low, while the percentage of energy from fat was high, considering the reference intake ranges.
The median energy intake of MHVPIs was 2272.6 Kcal and was, therefore, considered low in 66.7% when compared to the reference intake of 2430 Kcal from Ortega et al. [
37] for Spanish lactating women with a sedentary lifestyle. Di Maso et al. [
31], in their systematic review about dietary intake of lactating mothers of term infants in developed countries, summarized diverse nutrient intakes by calculating the median from the results of the included studies. The calculated median energy intake from this systematic review was 2111 kcal/day, with a range of 1411–2781 kcal, indicating that energy intake in other studies is also lower than recommended. The high percentage of energy from fat and the contrasting low Kcal percentage from carbohydrates is found to be a general occurrence in studies set in the Mediterranean area [
31,
69,
70].
When considering the HM macronutrient content, MHVPIs showed a higher carbohydrate concentration than the reference value reported by Leghi et al. [
55]; however, the lipid concentration in MHVPIs was slightly lower. The protein concentration in HM was also higher in MHVPIs compared to HMDs, with 1.36 g/dL vs. 1.19 g/dL, respectively, although both groups exceeded the reference value of 0.94 g/dL [
55]. Our regression analysis showed a positive association between MHVPIs and HM protein concentration. Therefore, the higher protein concentration in HM from MHVPIs is more likely to be associated with characteristics related to prematurity, as no link with protein intake was observed.
Special attention should be paid to vitamin D intake, as in our study, over 80% of MHVPIs had an inadequate intake. Although the median intake of 6.8 µg is high compared with that of other studies [
23,
31], the value is below the recommended daily intake of 15 µg [
37]. This finding is consistent with a review carried out by Carretero-Krug et al. [
71], who determined that eight studies reported not reaching the recommended daily intake for vitamin D, while no studies reported exceeding this amount. Vitamin D deficiency was also determined in plasma for all MHVPIs and vitamer 25(OH)D
3 showed concentrations of less than 12 ng/mL [
51]. The concentration of vitamin D
3 was within the reference range of 0.25–2.00 µg/L [
64], whereas the 25(OH)D
3 vitamer concentration (66.23 pg/mL) was substantially lower than the median value of 1100 pg/mL (44 UI/L) calculated in a meta-analysis [
72], which also documented a broad range of concentrations, from 0 to 176,440 pg/mL. However, as neither the intake nor the concentration in plasma, erythrocytes, or HM were different compared with HMDs, we suppose that the vitamin D deficit is not an exclusive issue for MHVPIs. Nevertheless, the regression analysis conducted in our study showed a positive association between 25(OH)D
3 concentrations in HM and MHVPIs as well as plasma concentration, but not with intake or erythrocyte concentration.
The increased inadequate intake of vitamin E in MHVPIs, also observed in other studies [
31,
73], was reflected in its plasma concentration. Furthermore, the HM concentration appeared to be lower compared to the values reported by EFSA and IOM [
49,
65] with 4.15 vs. 4.6 mg/L, respectively. Since no differences were found between MHVPIs and HMDs regarding vitamin E intake and α-tocopherol concentrations in plasma, erythrocytes, and HM, vitamin E deficiency should not be considered a problem exclusively for the MHVPI group but as something that also occurs in other groups of lactating mothers.
In the case of iodine, although intake was insufficient in 40% of MHVPIs, the median intake exceeded 250 µg/L and the urinary concentration was above 100 µg/L, indicating an iodine-sufficient population [
74,
75]. The HM concentration was above 200 µg/L, which is considered sufficient for the needs of premature infants [
53,
76]. In our study, the supplement intake of MHVPIs during the 5-day dietary record was over 64%, which could explain the high iodine concentrations in HM and urine. As reported in a previous study [
8], iodine supplementation appears to increase HM concentration. The high percentage of inadequate intake could, therefore, be attributed to MHVPIs who did not take iodine supplements. The iodine concentration in HM was even higher in MHVPIs than in HMD. The observed positive associations between iodine HM concentration and MHPVIs as well as iodine intake confirm that prematurity but also iodine intake might affect iodine HM concentration independent from each other.
An adequate percentage of energy from omega-3 PUFAs was observed in MHVPIs, in line with the acceptable macronutrient distribution ranges established by the Institute of Medicine [
38]. Both the percentage of energy derived from omega-3 PUFAs and the dietary intake of DHA (and DHA + EPA) were higher in the MHVPI group compared to the HMD group. In HM, the percentage of energy from omega-3 PUFAs and the content of α-linolenic acid were also higher in MHVPIs. In our regression analyses, both omega-3 and α-linolenic acid content in milk were positively associated with prematurity, independently of maternal intake and breastfeeding duration. Conversely, DHA content in HM was positively associated with maternal DHA intake as well as with maternal plasma and erythrocyte DHA concentrations.
Regarding the higher DHA intake in MHVPIs compared to HMDs, this was reflected in its increased concentration in plasma and erythrocytes, but not significantly in HM. Nonetheless, the median DHA concentration in HM was 0.41% for MHVPIs vs. 0.27% for HMDs. We suggest that statistical significance might have been achieved with a larger sample size of MHVPIs. These findings are surprising, as there are no differences between the study groups regarding food consumption, especially fish intake or supplementation for omega-3 FAs. However, the food consumption questionnaire and the food groups analysis provided by the 5-day dietary record did not differentiate between whitefish and oily fish; thus, a higher intake of oily fish in the MHVPI group might explain these divergences. The DHA intake found in our study was also shown to be much higher than that of the studies included in the systematic review by Di Maso et al. [
31]. Regarding the plasma and erythrocyte content, Giuffrida et al. [
12] reported a similar DHA concentration in erythrocytes; however, in plasma, a higher concentration was observed, at 2.36% vs. the 0.98% found in MHVPIs. Erythrocyte concentration is supposed to represent long-term intake due to its half-life of weeks or even months. Instead, plasma content might reflect short-term intake, which can be absorbed directly and transferred to HM [
12,
77]. Hence, a high concentration in both blood compounds might assume a regular intake and a continuous supply of DHA. It is important to mention that DHA deprivation due to preterm birth is related to a higher risk of cognitive impairment as it is an essential component for optimal brain development [
78]. However, several studies suggested a daily consumption of at least 200 mg of DHA [
79,
80] to reach an HM concentration of 0.30% [
79], which was fulfilled by the MHVPIs, who presented a median concentration of 0.41%. Regarding the special needs of low birth weight infants, the required DHA range established is 12 to 60 mg/kg/day [
81]. Assuming a 1 kg preterm infant with a daily intake of 175 mL/kg/day, considering the determined lipid concentration of 3.36 g/dL found in MHVPIs in our study, we calculated a possible intake of 24.1 mg/kg/day. The calculated intake is within the recommended range but is lower than the estimated 60 mg/kg/day of the in utero requirement [
78]. We showed that the HM concentration of DHA is associated with its intake and its erythrocyte status independent of prematurity and breastfeeding duration, emphasizing the influence that intake and maternal stores can have on DHA concentration in HM.
To better understand the diet of MHVPIs, we further examined their food consumption and dietary sources. MHVPIs did not achieve the recommended food servings for the five investigated food groups, according to the 5-day dietary record or food consumption questionnaire, except for the intake of eggs, meat, and fish [
42]. These results are confirmed by other studies [
82,
83]. In this sense, Lee et al. [
32] reported a transition to a less healthy maternal dietary pattern from pregnancy to postpartum, especially considering fruit and vegetable intake. On the other hand, the HEI, as a measure of dietary quality, showed a score of 61.9 points. Even though 61–70 points indicates a good diet [
84], nutrition can be improved considerably. Since no differences were found in HMDs, diet quality can be considered a general issue during lactation and is not specific to MHVPIs.
As pointed out by Neville et al. [
85], most studies are designed to focus principally on sampling HM, without considering the mother’s intake or plasma and erythrocyte status and, hence, fall short of investigating HM as a biological system. With the regression analysis carried out in the present study, we could determine that a diversity of macronutrients, micronutrients, and FAs in HM, independent of corresponding maternal intake, plasma and erythrocyte concentration, and breastfeeding duration, were related to prematurity. In this sense, being an MHVPI was positively associated with the HM content in terms of protein, vitamer 25(OH)D
3, iodine, selenium, omega 3 PUFAs, VLCFAs, myristic acid, dihomo-γ-linolenic acid, and linolenic acid, and negatively associated with free riboflavin, dehydroascorbic acid, palmitoleic acid, and
cis vaccenic acid. In most studies [
86,
87,
88,
89], differences between HM concentrations from term and preterm mothers can be observed. Preterm HM is known to have higher concentrations of certain nutrients, particularly in the first weeks postpartum. However, this composition changes rapidly and remains variable among individuals. Most studies primarily examined the concentration of macronutrients, like proteins. They found that the protein content in preterm mothers’ HM was higher, while no differences were observed for lactose and fat. There is less data available on micronutrients, but Redeuil et al. [
87] reported higher levels of vitamins B1, B2, B3, B6, and B9, along with lower levels of vitamins A and E in the HM of mothers who delivered prematurely. Nevertheless, the possibility that some of these associations might be based on maternal intake rather than preterm and term delivery cannot be ruled out. Many factors related to preterm delivery can influence HM composition, such as shortening the prenatal preparation of the mammary gland, immature oral feeding skills of the infant, and the use of alternative milk removal methods [
18]. The shortened gestation period might be a further reason [
18]. Maternal body fat is accumulated during the first two trimesters of gestation, whereas in the last trimester, a transfer of fat occurs to fill the stores of the infant’s adipose tissue [
90]. Preterm delivery interrupts this process; therefore, preterm infants are deprived of maternal supply, and the amount of maternal fat that is not used can be used as a reserve of FAs during breastfeeding. To the best of our knowledge, this is the first study that attributes changes in HM concentration to MHVPIs independent of maternal diet. However, the small number of MHVPIs and the great heterogeneity in the characteristics of both study groups should be taken into account when interpreting these results. Additionally, associations were also found in the regression analysis for nutrient intake, as well as nutrient plasma and erythrocyte status with HM concentration for several vitamers, minerals, and FAs independent of the study group and breastfeeding duration.
Adequate nutritional intake is important for lactating women, particularly for MHVPIs and HMDs, as they provide their milk to infants who have nutritional deficiencies and an immature organ system, which makes adequate absorption, utilization, and retention of nutrients difficult [
18]. Very preterm infants have markedly higher nutritional requirements, especially for protein, calcium, phosphorus, DHA, and several micronutrients, due to their limited body stores and the need to support rapid growth and organ development [
91,
92]. Even though HM provides immunological and gastrointestinal benefits, its native nutrient content is often insufficient to meet these elevated demands, especially when donor milk is used. Variability in the composition of maternal or donor milk can lead to suboptimal nutrient intake if not properly addressed through individualized fortification strategies. Inadequate intake during this critical window may negatively impact neurodevelopment, bone mineralization, and growth outcomes, as shown in previous studies [
93,
94,
95,
96,
97]. Furthermore, some nutrients naturally present in milk (e.g., DHA, iron, and vitamin B12) may have better bioavailability than those added through fortification or supplementation. Despite the benefits of HM, its nutrient content alone is often insufficient to meet the elevated needs of preterm neonates, particularly for protein, calcium, phosphorus, and other micronutrients. Recent ESPGHAN guidelines support the routine use of multicomponent fortifiers rather than isolated nutrient supplements [
98]. However, the biodisponibility of nutrients may differ depending on whether they are naturally present in milk or added through fortifiers. This is partly because HM contains bioactive components that protect nutrients during digestion and enhance their absorption and utilization, either through natural binding to specific transport proteins or through their incorporation into milk fat globules, both of which support efficient nutrient uptake and of tissue distribution [
99]. For example, vitamin B12 in HM is bound to haptocorrin, which protects it during digestion and enhances absorption [
100]. In the case of DHA, it has been shown that its incorporation into infant tissues is more efficient when derived from HM compared to direct supplementation with isolated fish oil capsules [
101,
102,
103]. These findings reinforce the importance of preserving and optimizing the nutritional quality of HM, particularly in vulnerable populations, such as preterm infants. For this reason, it becomes especially important to study the impact of maternal diet on milk composition and to implement strategies aimed at improving the nutritional status of lactating women, with the goal of optimizing the quality of milk available to preterm infants.
Our study showed that the nutritional intake of MHVPIs did not differ greatly from the intake of HMDs or from the intake of breastfeeding mothers of term infants, considering the results of Di Maso et al. [
31]. Hence, the nutritional deficiencies found in MHVPIs are also present in other lactating populations. There are ways to improve the diets of MHVPIs. For example, the total energy requirements of MHVPIs were not met, and this gap could be closed by a higher intake of fruits, vegetables, whole grains, legumes, and nuts, which would simultaneously add important micronutrients to their diet and, thus, reduce vitamin and mineral deficiencies. In addition, the percentage of energy from carbohydrates was below the acceptable macronutrient distribution ranges, while the percentage of energy from fat was above the corresponding range. Including the above-mentioned food groups in the diet of MHVPIs could compensate for this imbalance. On the other hand, the realized regression analysis confirmed associations with HM concentration not only in terms of study groups but also with intake and nutritional status, which further emphasizes the importance of both aspects in lactating mothers.
Hence, dietary education should be offered to MHVPIs. Professionals, such as dietitians, should provide supportive educational and intervention programs that explain the importance of nutrition for MHVPIs themselves and their premature infants. Just as NICUs offer workshops and training courses to promote successful breastfeeding [
104], similar efforts could be made to successfully adapt the diet of MHVPIs to meet their nutritional and dietary needs, as well as those of their premature infants [
105]. On the other hand, MHVPIs should be included in hospital meal services to facilitate their access to healthy food. Although they are not hospitalized patients, they are still the nutritional care keepers of their hospitalized preterm children [
18,
85]. Furthermore, nutrient supplementation for MHVPIs should also be considered, as several studies have observed that this could increase the concentration of several nutrients in HM [
3,
8,
10]. Currently, in the region of Madrid, free supplementation is only offered for the nutrients iodine, vitamin B9, and vitamin B12, which should be extended.
This study has several limitations. First of all, the sample size is small in the MHVPI group. Still, the study provides a very comprehensive assessment of their dietary conditions, evaluating nutrient intake, including food consumption and dietary sources but also nutrient concentrations in plasma, erythrocytes, and urine, along with information about HM composition. As concerns the statistical bivariate and multivariate analysis, the small sample size and unbalanced categories were overcome to some extent with such tools as bootstrapping and the determination of the exact p-values rather than the use of approximations. Nevertheless, the results should be confirmed by further studies with a more representative sample size.
Secondly, the sample was not randomly selected. Participants were enrolled through opportunity sampling, and their inclusion was based on voluntary consent. For example, it is plausible that mothers with higher educational levels were more likely to understand the study objectives, felt confident in engaging with the research process, and, therefore, were more inclined to participate [
106]. On the other hand, the inclusion of MHVPIs in the study depended on the milk supply, as it was essential for us to assure that the MHVPIs who participated in our study were able to express enough milk to fulfill the needs of their preterm infants before delivering HM for study purposes, especially as a full expression was required. Mothers who could not express enough milk did not participate in the study. Those who participated joined the study at different postpartum time points. Both the amount of HM and the duration of breastfeeding affect HM composition. In addition, we would like to emphasize that the studied HM in both groups was mature milk, as one of the inclusion criteria was that mothers had been lactating for at least three weeks postpartum.
Regarding reporting bias, the 5-day dietary record, when administered with appropriate instructions and a sufficient number of observation days, has been shown to have high validity and precision, and is often considered a reference method in validation studies. One of the main strengths of the 5-day dietary record is that foods and beverages are recorded at the time of consumption, which minimizes memory-related omissions. Additionally, it allows for the registration of dietary intake as actually consumed, including preparation details and portion sizes, especially when weighed records are used. Nonetheless, we acknowledge the limitations of this method. These include potential social desirability bias, where participants may underreport foods perceived as less healthy; respondent burden, which may affect compliance and accuracy; and altered eating behaviors, where participants modify their intake to simplify the recording process. Some individuals may also face challenges in accurately describing portion sizes or recording all items consumed. Furthermore, increasing the number of recording days may reduce data quality, and the method entails a high cost of data processing and coding.
Untreated donor HM was examined, and it is uncertain whether the observed results—particularly the associations from the regression analysis—would persist if pasteurized donor HM were studied. However, preservation through Holder pasteurization appears to primarily affect bioactive and immunomodulatory components rather than nutrients [
107]. A significant decrease was observed in vitamin B6, C, and folic acid due to pasteurization, while other vitamins and fatty acids remained unaffected [
108].
Finally, while a large number of nutrients were considered in this study, gaps remain for many nutrients that still need to be addressed. This applies, for example, for choline intake and the three water-soluble forms of choline (free choline, phosphocholine, and glycerophosphocholine) in HM, which are essential for lipid synthesis, neurotransmission, and methylation, and are, therefore, crucial for normal growth in infants.
Nevertheless, the wide range of nutrients examined, the detailed dietary assessment, the biochemical analysis of plasma, erythrocytes, and urine, and the multiple milk samples collected from a rarely studied group of breastfeeding women are strengths that set our study apart from others.