Characterizing Factors Associated with Excess Body Weight: A Descriptive Study Using Principal Component Analysis in a Population with Overweight and Obesity
Highlights
- The study found a large inter-individual variability in dietary intake and physical activity, but body composition was more consistent between subjects.
- The participants’ diet was unbalanced, and they maintained a sedentary lifestyle, which could contribute to an increased risk of overweight, obesity, and other cardiometabolic disruptions.
- The Principal Component Analysis identified four key factors explaining 65.4% of the variance.
- The dietary factor (24% variance) was linked to energy intake, lipids, and saturated fats; the cardiometabolic factor (16.8% variance) was related to biochemical markers like triglycerides and HDL and LDL cholesterol; the adiposity factor (15.2% variance) was associated with body fat percentage and visceral fat; and the serum cholesterol factor (9.4% variance) focused on cholesterol levels.
- The findings underline the importance of a holistic approach to weight loss treatments that must include diet, physical activity, and other individual factors such as resting metabolic rate and metabolic health. Thus, it is essential to move towards a precision nutrition approach to effectively address the obesity epidemic, taking into account all of these factors through multivariate analyses.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
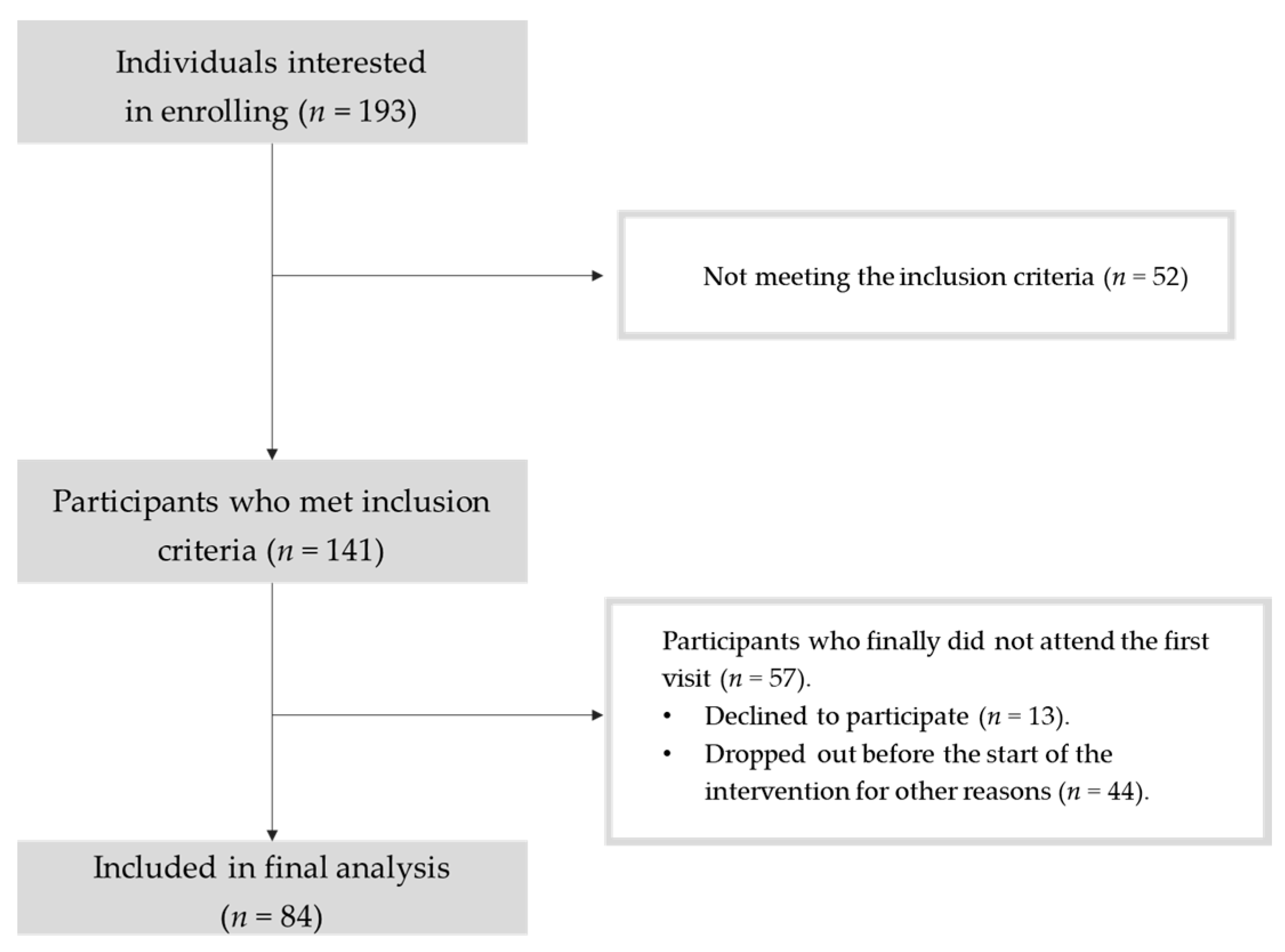
2.3. Recruitment
2.4. Dietary Intake Measurements
2.5. Anthropometric, Body Composition, Physical Activity, and Resting Metabolic Rate Analysis
2.6. Biochemical Analysis and Blood Pressure Measurement
2.7. Statistical Analysis
3. Results
3.1. Subjects Sociodemographic Characteristics
3.2. Dietary Intake
3.3. Biochemical Measurements
3.4. Anthropometric, Body Composition, Resting Metabolic Rate, and Physical Activity Measurements
3.5. Principal Component Analysis (PCA)
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Luli, M.; Yeo, G.; Farrell, E.; Ogden, J.; Parretti, H.; Frew, E.; Bevan, S.; Brown, A.; Logue, J.; Menon, V.; et al. The Implications of Defining Obesity as a Disease: A Report from the Association for the Study of Obesity 2021 Annual Conference. EClinicalMedicine 2023, 58, 101962. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 17 December 2023).
- World Health Organization [WHO]. Regional Office for Europe WHO European Regional Obesity: Report 2022; WHO: Geneva, Switzerland, 2022; ISBN 978-92-890-5773-8. [Google Scholar]
- González-Muniesa, P.; Mártinez-González, M.A.; Hu, F.B.; Després, J.P.; Matsuzawa, Y.; Loos, R.J.F.; Moreno, L.A.; Bray, G.A.; Martinez, J.A. Obesity. Nat. Rev. Dis. Primers 2017, 3, 17034. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Bentham, J.; Stevens, G.A.; Zhou, B.; Danaei, G.; Lu, Y.; Bixby, H.; Cowan, M.J.; Riley, L.M.; Hajifathalian, K.; et al. Trends in Adult Body-Mass Index in 200 Countries from 1975 to 2014: A Pooled Analysis of 1698 Population-Based Measurement Studies with 19.2 Million Participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Chung, W.K.; Leibel, R.L. Considerations Regarding the Genetics of Obesity. Obesity 2008, 16, S33–S39. [Google Scholar] [CrossRef]
- Losavio, J.; Keenan, M.J.; Gollub, E.A.; Silver, H.J. Factors That Predict Weight Loss Success Differ by Diet Intervention Type. Front. Nutr. 2023, 10, 1192747. [Google Scholar] [CrossRef] [PubMed]
- Tsatsoulis, A.; Paschou, S.A. Metabolically Healthy Obesity: Criteria, Epidemiology, Controversies, and Consequences. Curr. Obes. Rep. 2020, 9, 109–120. [Google Scholar] [CrossRef]
- Chooi, Y.C.; Ding, C.; Magkos, F. The Epidemiology of Obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- Dent, R.; McPherson, R.; Harper, M.E. Factors Affecting Weight Loss Variability in Obesity. Metabolism 2020, 113, 154388. [Google Scholar] [CrossRef]
- Markle, J.G.M.; Frank, D.N.; Mortin-Toth, S.; Robertson, C.E.; Feazel, L.M.; Rolle-Kampczyk, U.; Von Bergen, M.; McCoy, K.D.; Macpherson, A.J.; Danska, J.S. Sex Differences in the Gut Microbiome Drive Hormone-Dependent Regulation of Autoimmunity. Science 2013, 339, 1084–1088. [Google Scholar] [CrossRef]
- Yurkovetskiy, L.; Burrows, M.; Khan, A.A.; Graham, L.; Volchkov, P.; Becker, L.; Antonopoulos, D.; Umesaki, Y.; Chervonsky, A.V. Gender Bias in Autoimmunity Is Influenced by Microbiota. Immunity 2013, 39, 400–412. [Google Scholar] [CrossRef]
- Cuevas-Sierra, A.; Milagro, F.I.; Guruceaga, E.; Cuervo, M.; Goni, L.; García-Granero, M.; Martinez, J.A.; Riezu-Boj, J.I. A Weight-Loss Model Based on Baseline Microbiota and Genetic Scores for Selection of Dietary Treatments in Overweight and Obese Population. Clin. Nutr. 2022, 41, 1712–1723. [Google Scholar] [CrossRef] [PubMed]
- Asarian, L.; Geary, N. Sex Differences in the Physiology of Eating. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013, 305, 1215–1267. [Google Scholar] [CrossRef] [PubMed]
- Anekwe, C.V.; Jarrell, A.R.; Townsend, M.J.; Gaudier, G.I.; Hiserodt, J.M.; Stanford, F.C. Socioeconomics of Obesity. Curr. Obes. Rep. 2020, 9, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Cai, T.; Tian, L.; Wong, P.H.; Wei, L.J. Analysis of Randomized Comparative Clinical Trial Data for Personalized Treatment Selections. Biostatistics 2011, 12, 270–282. [Google Scholar] [CrossRef] [PubMed]
- De Toro-Martín, J.; Arsenault, B.J.; Després, J.-P.; Vohl, M.-C. Precision Nutrition: A Review of Personalized Nutritional Approaches for the Prevention and Management of Metabolic Syndrome. Nutrients 2017, 9, 913. [Google Scholar] [CrossRef] [PubMed]
- Hinojosa-Nogueira, D.; Pérez-Burillo, S.; Garciá-Rincón, I.; Rufián-Henares, J.A.; Pastoriza, S. A Useful and Simple Tool to Evaluate and Compare the Intake of Total Dietary Polyphenols in Different Populations. Public Health Nutr. 2021, 24, 3818–3824. [Google Scholar] [CrossRef] [PubMed]
- Neveu, V.; Perez-Jiménez, J.; Vos, F.; Crespy, V.; Du Chaffaut, L.; Mennen, L.; Knox, C.; Eisner, R.; Cruz, J.; Wishart, D.; et al. Phenol-Explorer: An Online Comprehensive Database on Polyphenol Contents in Foods. Database 2010, 2010, bap024. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on Dietary Reference Values for Energy. EFSA J. 2013, 11, 3005. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.R.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis Model Assessment: Insulin Resistance and Fl-Cell Function from Fasting Plasma Glucose and Insulin Concentrations in Man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Meier, J.J.; Hü, K.; Holst, J.J.; Deacon, C.F.; Schmiegel, W.H.; Nauck, M.A. Reduced Insulinotropic Effect of Gastric Inhibitory Polypeptide in First-Degree Relatives of Patients with Type 2 Diabetes. Diabetes 2001, 50, 2497–2504. [Google Scholar] [CrossRef]
- Katz, A.; Nambi, S.S.; Mather, K.; Baron, A.D.; Follmann, D.A.; Sullivan, G.; Quon, M.J. Quantitative Insulin Sensitivity Check Index: A Simple, Accurate Method for Assessing Insulin Sensitivity In Humans. J. Clin. Endocrinol. Metab. 2000, 85, 2402–2410. [Google Scholar] [CrossRef] [PubMed]
- Vargas Franco, V. Estadística Descriptiva Para Ingeniería Ambiental Con SPSS; Vargas Franco, V., Ed.; Universidad Nacional de Colombia Editorial UN: Cali, Colombia, 2007; p. 49. ISBN 978-958-33-9319-3. [Google Scholar]
- Newby, P.K.; Tucker, K.L. Empirically Derived Eating Patterns Using Factor or Cluster Analysis: A Review. Nutr. Rev. 2004, 62, 177–203. [Google Scholar] [CrossRef] [PubMed]
- Stea, T.H.; Nordheim, O.; Bere, E.; Stornes, P.; Eikemo, T.A. Fruit and Vegetable Consumption in Europe According to Gender, Educational Attainment and Regional Affiliation—A Cross-Sectional Study in 21 European Countries. PLoS ONE 2020, 15, e0232521. [Google Scholar] [CrossRef] [PubMed]
- Pour-Abbasi, M.S.; Nikrad, N.; Farhangi, M.A.; Vahdat, S.; Jafarzadeh, F. Dietary Energy Density, Metabolic Parameters, and Blood Pressure in a Sample of Adults with Obesity. BMC Endocr. Disord. 2023, 23, 3. [Google Scholar] [CrossRef] [PubMed]
- Bartrina, J.A.; Majem, L.S. Objetivos nutricionales para la población española: Consenso de la Sociedad Española de Nutrición Comunitaria 2011. Rev. Esp. Nutr. Comunitaria 2011, 17, 178–199. [Google Scholar]
- Lichnovská, R.; Gwozdziewiczová, S.; Hrebícek, J. Gender Differences in Factors Influencing Insulin Resistance in Elderly Hyperlipemic Non-Diabetic Subjects. Cardiovasc. Diabetol. 2002, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Acosta, A.M.; Escalona, M.; Maiz, A.; Pollak, F.; Leighton, F. Determinación Del Índice de Resistencia Insulínica Mediante HOMA En Una Población de La Región Metropolitana de Chile. Rev. Med. Chil. 2002, 130, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consulation; WHO: Geneva, Switzerland, 2000; ISBN 92-4-120894-5. [Google Scholar]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic Syndrome—A New World-Wide Definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Raiman, L.; Amarnani, R.; Abdur-Rahman, M.; Marshall, A.; Mani-Babu, S. The Role of Physical Activity in Obesity: Let’s Actively Manage Obesity. Clin. Med. 2023, 23, 311–317. [Google Scholar] [CrossRef]
- Silveira, E.A.; Mendonça, C.R.; Delpino, F.M.; Elias Souza, G.V.; Pereira de Souza Rosa, L.; De Oliveira, C.; Noll, M. Sedentary Behavior, Physical Inactivity, Abdominal Obesity and Obesity in Adults and Older Adults: A Systematic Review and Meta-Analysis. Clin. Nutr. ESPEN 2022, 50, 63–73. [Google Scholar] [CrossRef]
- Black, A.E. Critical Evaluation of Energy Intake Using the Goldberg Cut-off for Energy Intake:Basal Metabolic Rate. A Practical Guide to Its Calculation, Use and Limitations. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority (EFSA). Example of a Protocol for Identification of Misreporting (Under-and Over-Reporting of Energy Intake) Based on the PILOT-PANEU Project. EFSA J. 2013, 11, 1–17. Available online: https://www.efsa.europa.eu/sites/default/files/efsa_rep/blobserver_assets/3944A-8-2-1.pdf (accessed on 15 December 2023).
- Wehling, H.; Lusher, J. People with a Body Mass Index ≥30 Under-Report Their Dietary Intake: A Systematic Review. J. Health Psychol. 2019, 24, 2042–2059. [Google Scholar] [CrossRef] [PubMed]
- Hannon, B.A.; Thompson, S.V.; An, R.; Teran-Garcia, M. Clinical Outcomes of Dietary Replacement of Saturated Fatty Acids with Unsaturated Fat Sources in Adults with Overweight and Obesity: A Systematic Review and Meta-Analysis of Randomized Control Trials. Ann. Nutr. Metab. 2017, 71, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Seifu, C.N.; Fahey, P.P.; Hailemariam, T.G.; Frost, S.A.; Atlantis, E. Dietary Patterns Associated with Obesity Outcomes in Adults: An Umbrella Review of Systematic Reviews. Public Health Nutr. 2021, 24, 6390–6414. [Google Scholar] [CrossRef] [PubMed]
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary Sugars and Body Weight: Systematic Review and Meta-Analyses of Randomised Controlled Trials and Cohort Studies. BMJ 2012, 346, e7492. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.A.; Sievenpiper, J.L. Controversies about Sugars: Results from Systematic Reviews and Meta-Analyses on Obesity, Cardiometabolic Disease and Diabetes. Eur. J. Nutr. 2016, 55, 25–43. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Verde, L.; Vetrani, C.; Barrea, L.; Savastano, S.; Colao, A. Obesity: A Gender-View. J. Endocrinol. Investig. 2023, 47, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, E.; Rodriguez, P.; Valero, T.; Ávila, J.M.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. Dietary Intake of Individual (Free and Intrinsic) Sugars and Food Sources in the Spanish Population: Findings from the ANIBES Study. Nutrients 2017, 9, 275. [Google Scholar] [CrossRef]
- Newby, P.K.; Muller, D.; Hallfrisch, J.; Andres, R.; Tucker, K.L. Food Patterns Measured by Factor Analysis and Anthropometric Changes in Adults. Am. J. Clin. Nutr. 2004, 80, 504–513. [Google Scholar] [CrossRef]
- Rice Bradley, B.H. Dietary Fat and Risk for Type 2 Diabetes: A Review of Recent Research. Curr. Nutr. Rep. 2018, 7, 214–226. [Google Scholar] [CrossRef]
- Kodoth, V.; Scaccia, S.; Aggarwal, B. Adverse Changes in Body Composition During the Menopausal Transition and Relation to Cardiovascular Risk: A Contemporary Review. Womens Health Rep. 2022, 3, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Holven, K.B.; Roeters van Lennep, J. Sex Differences in Lipids: A Life Course Approach. Atherosclerosis 2023, 384, 117270. [Google Scholar] [CrossRef] [PubMed]
- Buday, B.; Pach, P.F.; Literati-Nagy, B.; Vitai, M.; Kovacs, G.; Vecsei, Z.; Koranyi, L.; Lengyel, C. Sex Influenced Association of Directly Measured Insulin Sensitivity and Serum Transaminase Levels: Why Alanine Aminotransferase Only Predicts Cardiovascular Risk in Men? Cardiovasc. Diabetol. 2015, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Caballería, L.; Pera, G.; Auladell, M.A.; Torán, P.; Muñoz, L.; Miranda, D.; Alumà, A.; Casas, J.D.; Sánchez, C.; Gil, D.; et al. Prevalence and Factors Associated with the Presence of Nonalcoholic Fatty Liver Disease in an Adult Population in Spain. Eur. J. Gastroenterol. Hepatol. 2010, 22, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Du, T.; Sun, X.; Yuan, G.; Zhou, X.; Lu, H.; Lin, X.; Yu, X. Sex Differences in the Impact of Nonalcoholic Fatty Liver Disease on Cardiovascular Risk Factors. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Ballestri, S.; Nascimbeni, F.; Baldelli, E.; Marrazzo, A.; Romagnoli, D.; Lonardo, A. NAFLD as a Sexual Dimorphic Disease: Role of Gender and Reproductive Status in the Development and Progression of Nonalcoholic Fatty Liver Disease and Inherent Cardiovascular Risk. Adv. Ther. 2017, 34, 1291–1326. [Google Scholar] [CrossRef] [PubMed]
- Maranon, R.; Reckelhoff, J.F. Sex and Gender Differences in Control of Blood Pressure. Clin. Sci. 2013, 125, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Connelly, P.J.; Currie, G.; Delles, C. Sex Differences in the Prevalence, Outcomes and Management of Hypertension. Curr. Hypertens. Rep. 2022, 24, 185–192. [Google Scholar] [CrossRef]
- Garaulet, M.; Pérez-Llamas, F.; Canteras, M.; Tebar, F.J.; Zamora, S. Endocrine, Metabolic and Nutritional Factors in Obesity and Their Relative Significance as Studied by Factor Analysis. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 243–251. [Google Scholar] [CrossRef][Green Version]
- Neuenschwander, M.; Stadelmaier, J.; Eble, J.; Grummich, K.; Szczerba, E.; Kiesswetter, E.; Schlesinger, S.; Schwingshackl, L. Substitution of Animal-Based with Plant-Based Foods on Cardiometabolic Health and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. BMC Med. 2023, 21, 404. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, L.; Panaite, S.-A.; Bertazzo, A.; Visioli, F. Animal- and Plant-Based Protein Sources: A Scoping Review of Human Health Outcomes and Environmental Impact. Nutrients 2022, 14, 5115. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Ros, R.; Knaze, V.; Rothwell, J.A.; Hémon, B.; Moskal, A.; Overvad, K.; Tjønneland, A.; Kyrø, C.; Fagherazzi, G.; Boutron-Ruault, M.C.; et al. Dietary Polyphenol Intake in Europe: The European Prospective Investigation into Cancer and Nutrition (EPIC) Study. Eur. J. Nutr. 2016, 55, 1359–1375. [Google Scholar] [CrossRef] [PubMed]
- Amiot, M.J.; Riva, C.; Vinet, A. Effects of Dietary Polyphenols on Metabolic Syndrome Features in Humans: A Systematic Review. Obes. Rev. 2016, 17, 573–586. [Google Scholar] [CrossRef] [PubMed]
- Aloo, S.O.; Ofosu, F.K.; Kim, N.H.; Kilonzi, S.M.; Oh, D.H. Insights on Dietary Polyphenols as Agents against Metabolic Disorders: Obesity as a Target Disease. Antioxidants 2023, 12, 416. [Google Scholar] [CrossRef] [PubMed]
- Sarriá, B.; Martínez-López, S.; Sierra-Cinos, J.L.; García-Diz, L.; Mateos, R.; Bravo-Clemente, L. Regularly Consuming a Green/Roasted Coffee Blend Reduces the Risk of Metabolic Syndrome. Eur. J. Nutr. 2018, 57, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Martínez-López, S.; Sarriá, B.; Mateos, R.; Bravo-Clemente, L. Moderate Consumption of a Soluble Green/Roasted Coffee Rich in Caffeoylquinic Acids Reduces Cardiovascular Risk Markers: Results from a Randomized, Cross-over, Controlled Trial in Healthy and Hypercholesterolemic Subjects. Eur. J. Nutr. 2019, 58, 865–878. [Google Scholar] [CrossRef] [PubMed]
- Sarriá, B.; Sierra-Cinos, J.L.; García-Diz, L.; Martínez-López, S.; Mateos, R.; Bravo-Clemente, L. Green/Roasted Coffee May Reduce Cardiovascular Risk in Hypercholesterolemic Subjects by Decreasing Body Weight, Abdominal Adiposity and Blood Pressure. Foods 2020, 9, 1191. [Google Scholar] [CrossRef] [PubMed]
- Van de Woestijne, A.P.; Monajemi, H.; Kalkhoven, E.; Visseren, F.L.J. Adipose Tissue Dysfunction and Hypertriglyceridemia: Mechanisms and Management. Obes. Rev. 2011, 12, 829–840. [Google Scholar] [CrossRef]
- Gómez-Hernández, A.; Beneit, N.; Díaz-Castroverde, S.; Escribano, Ó. Differential Role of Adipose Tissues in Obesity and Related Metabolic and Vascular Complications. Int. J. Endocrinol. 2016, 2016, 1216783. [Google Scholar] [CrossRef]
| Absolute Frequency (n) | Relative Frequency (%) | |
|---|---|---|
| Men | 35 | 41.7 |
| Women | 49 | 58.3 |
| European origin | 78 | 97.5 |
| Latin-American origin | 2 | 2.5 |
| Low educational level | 7 | 8.7 |
| Medium educational level | 14 | 17.5 |
| High educational level | 59 | 73.8 |
| Median (IQR) | ||
| Monthly income per person (€) | 1167 (900) | |
| Monthly income per family unit (€) | 3000 (1900) | |
| Age | 51.0 (11.3) | |
| Total (n = 81) | Men (n = 35) | Women (n = 46) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD (%CV) | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||
| Edible food intake (g) a | 2091 ± 572 (27.3%) | 2038 (646) | 2053 (513) | 1967 (773) | 0.498 | ||
| Energy intake (kcal) | 2015 ± 521 (25.9%) | 1960 (716) | 2095 ± 509 | 1953 ± 527 | 0.227 | ||
| Energy density (kcal/g) b | 1.00 ± 0.25 (24.8%) | 1.00 (0.32) | 1.01 ± 0.20 | 0.99 ± 0.28 | 0.643 | ||
| Proteins (g) a | 88.9 ± 23.9 (26.9%) | 88.8 (22.4) | 88.8 (18.6) | 87.2 (28.4) | 0.985 | ||
| Carbohydrates (g) | 186 ± 56 (30.1%) | 179 (72) | 200.6 ± 57.6 | 174.7 ± 52.6 | 0.038 * | ||
| Simple sugars (g) a | 75.8 ± 27.7 (36.6%) | 70.8 (34.2) | 73.1 (29.3) | 68.1 (37.1) | 0.448 | ||
| Intrinsic sugars (g) | 47.9 ± 17.6 (36.8%) | 48.3 (22.5) | 47.9 ± 17.7 | 47.9 ± 17.8 | 0.986 | ||
| Added sugars (g) a | 28.1 ± 18.8 (66.9%) | 24.9 (20.3) | 25.8 (20.1) | 23.5 (21.2) | 0.381 | ||
| Lipids (g) a | 92.1 ± 29.9 (32.4%) | 86.8 (42.5) | 90.4 (46.4) | 83.7 (44.1) | 0.706 | ||
| SFA (g) a | 28.6 ± 10.7 (37.5%) | 24.6 (17.0) | 25.3 (16.2) | 24.3 (17.2) | 0.706 | ||
| MUFA (g) a | 40.5 ± 14.3 (35.3%) | 37.5 (13.7) | 37.3 (13.1) | 38.7 (15.3) | 0.838 | ||
| PUFA (g) a | 12.3 ± 5.3 (43.2%) | 11.2 (5.3) | 11.2 (5.4) | 11.3 (4.6) | 0.637 | ||
| W6 (g) a | 10.3 ± 4.9 (47.6%) | 9.2 (5.0) | 9.7 (5.5) | 8.8 (4.9) | 0.520 | ||
| W3 (g) a | 1.9 ± 1.0 (50.6%) | 1.5 (1.1) | 1.40 (0.95) | 1.80 (1.15) | 0.359 | ||
| W6/W3 ratio a | 6.5 ± 3.8 (59.0%) | 6.1 (4.5) | 6.43 (3.98) | 5.05 (4.67) | 0.564 | ||
| Total dietary cholesterol (mg) a | 339 ± 132 (39.0%) | 317 (163) | 317 (157) | 319 (161) | 0.577 | ||
| Cholesterol (mg/1000 kcal) a | 172.3 ± 68.5 (39.7%) | 166.1 (80.6) | 166.1 (69.1) | 169.1 (90.5) | 0.659 | ||
| Alcohol (g) a | 6.7 ± 9.6 (143.9%) | 2.9 (10.1) | 4.1 (13.3) | 2.8 (7.9) | 0.503 | ||
| Dietary fibre (g) a | 19.8 ± 8.1 (40.7%) | 19.7 (10.5) | 19.8 (11.8) | 19.2 (8.4) | 0.501 | ||
| Dietary fibre (g/1000 kcal) a | 10.0 ± 3.5 (34.7%) | 9.7 (5.0) | 9.2 (3.9) | 10.1 (5.0) | 0.370 | ||
| Total (poly)phenols (mg) a | 1278 ± 809 (63.3%) | 1073 (1017) | 1073 (688) | 1075 (1095) | 0.802 | ||
| (Poly)phenols (mg/1000 kcal) a | 642 ± 371 (57.8%) | 535 (426) | 509 (412) | 594 (437) | 0.659 | ||
| Total (n = 81) | Men (n = 35) | Women (n = 46) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD (%CV) | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||
| % Carbohydrates | 36.9 ± 6.4 (17.4%) | 37.1 (10.3) | 38.4 ± 6.6 | 35.8 ± 6.1 | 0.067 | ||
| % Simple sugars | 14.9 ± 4.1 (27.4%) | 14.7 (4.9) | 15.1 ± 4.7 | 14.8 ± 3.6 | 0.792 | ||
| % Intrinsic sugars | 9.7 ± 3.4 (35.1%) | 9.1 (4.9) | 9.3 ± 3.5 | 10.0 ± 3.3 | 0.352 | ||
| % Added sugars | 5.4 ± 3.1 (57.0%) | 5.1 (4.2) | 5.6 ± 3.4 | 5.2 ± 2.8 | 0.541 | ||
| % Proteins | 17.9 ± 2.9 (16.3%) | 17.8 (4.1) | 17.2 ± 2.8 | 18.3 ± 2.9 | 0.089 | ||
| % Lipids | 40.9 ± 6.0 (14.6%) | 40.7 (9.7) | 39.5 ± 5.8 | 41.9 ± 6.0 | 0.072 | ||
| % SFA a | 12.6 ± 2.6 (20.7%) | 12.4 (3.7) | 12.0 (3.5) | 13.1 (3.5) | 0.113 | ||
| % MUFA | 18.1 ± 3.8 (21.2%) | 17.5 (4.5) | 17.2 ± 3.5 | 18.7 ± 4.0 | 0.096 | ||
| % PUFA a | 5.5 ± 1.8 (33.2%) | 5.2 (2.2) | 5.1 (2.6) | 5.3 (1.9) | 0.396 | ||
| % W3 a | 0.87 ± 0.50 (52.3%) | 0.76 (0.59) | 0.61 (0.44) | 0.87 (0.55) | 0.088 | ||
| % α-Linolenic acid a | 0.5 ± 0.2 (42.3%) | 0.44 (0.23) | 0.40 (0.17) | 0.49 (0.22) | 0.029 * | ||
| % W6 a | 4.6 ± 1.7 (37.0%) | 4.1 (2.1) | 4.3 (2.3) | 4.1 (1.9) | 0.652 | ||
| % Linoleic acid a | 4.5 ± 1.7 (37.5%) | 4.1 (2.1) | 4.1 (2.2) | 4.0 (1.8) | 0.744 | ||
| % Trans FA | 0.38 ± 0.19 (49.3%) | 0.38 (0.27) | 0.38 ± 0.17 | 0.36 (0.23) | 0.39 ± 0.21 | 0.41 (0.29) | 0.871 |
| % Alcohol a | 2.3 ± 3.3 (145.5%) | 1.0 (3.2) | 1.2 (4.3) | 1.0 (2.5) | 0.565 | ||
| % Dietary fibre a | 2.0 ± 0.7 (34.7%) | 1.9 (1.0) | 1.8 (0.8) | 2.0 (1.0) | 0.370 | ||
| Total (n = 83) | Men (n = 35) | Women (n = 48) | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD (%CV) | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | p Value | |
| TC (mg/dL) | 211.0 ± 31.1 (14.7%) | 214 (42.5) | 204.1 ± 31.7 | 216.0 ± 30.2 | 0.085 | ||
| TG (mg/dL) a | 127.7 ± 68.1 (53.3%) | 111 (52) | 121 (61.5) | 104.5 (50) | 0.091 | ||
| HDL (mg/dL) a | 61.6 ± 17.0 (27.6%) | 56 (26) | 51 (14) | 68 (23.3) | <0.001 *** | ||
| LDL (mg/dL) | 124.0 ± 25.0 (20.2%) | 126.8 (36.6) | 120.9 ± 25.6 | 126.2 ± 24.6 | 0.337 | ||
| VLDL (mg/dL) a | 25.5 ± 13.6 (53.2%) | 22.0 (10.3) | 24.0 (12.0) | 21.0 (10.3) | 0.094 | ||
| HbA1c (%) | 5.75 ± 0.35 (6.1%) | 5.70 (0.40) | 5.71 ± 0.32 | 5.77 ± 0.37 | 0.504 | ||
| FBG (mg/dL) | 93.1 ± 11.3 (12.2%) | 92 (12.5) | 92.3 ± 12.0 | 93.7 ± 11.0 | 0.586 | ||
| Insulin (µUI/mL) a | 10.5 ± 5.7 (54.2%) | 9.2 (6.6) | 10.5 (5.1) | 8.0 (7.0) | 0.173 | ||
| HOMA-IR a | 2.41 ± 1.32 (54.5%) | 1.98 (1.66) | 2.41 (1.22) | 1.84 (2.05) | 0.243 | ||
| HOMA-β a | 146 ± 123 (84.2%) | 111 (97) | 119 (123) | 98 (83) | 0.437 | ||
| QUICKI | 0.343 ± 0.027 (7.8%) | 0.344 (0.040) | 0.340 ± 0.027 | 0.345 ± 0.026 | 0.417 | ||
| AST (UI/L) a | 24.8 ± 12.0 (48.4%) | 22.0 (8.0) | 24.0 (9.3) | 21.0 (5.5) | 0.014 * | ||
| ALT (UI/L) a | 30.1 ± 18.9 (62.9%) | 24.0 (16.0) | 30.0 (20.0) | 21.0 (10.0) | 0.006 ** | ||
| hsCRP (mg/dL) a | 0.345 ± 0.562 (162.8%) | 0.153 (0.301) | 0.158 (0.248) | 0.151 (0.440) | 0.843 | ||
| Blood pressure | |||||||
| SBP (mmHg) a | 126.2 ± 18.6 (14.7%) | 124.7 (25.1) | 130.7 (18.7) | 121.3 (25.0) | 0.01 * | ||
| DBP (mmHg) a | 84.8 ± 10.9 (12.8%) | 82.0 (14.8) | 87.3 (18.6) | 80.7 (12.7) | 0.110 | ||
| Total (n = 84) | Men (n = 35) | Women (n = 49) | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD (%CV) | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | p Value | |
| Height (cm) | 165.4 ± 8.1 (4.9%) | 163.6 (13) | 172.1 ± 6.7 | 160.7 ± 5.0 | <0.001 *** | ||
| Weight (kg) b | 83.6 ± 11.1 (13.2%) | 83.6 (12.0) | 91.2 ± 10.9 | 78.1 ± 7.4 | <0.001 *** | ||
| BMI (kg/m2) | 30.5 ± 2.9 (9.6%) | 30.4 (3.5) | 30.8 ± 2.8 | 30.3 ± 3.0 | 0.471 | ||
| WC (cm) | 96.0 ± 11.5 (11.9%) | 94.7 (15.4) | 102.2 ± 11.1 | 91.5 ± 9.5 | <0.001 *** | ||
| HC (cm) a | 108.5 ± 6.8 (6.3%) | 106.8 (10.4) | 104.5 (6.2) | 110.2 (10) | <0.001 *** | ||
| WC/HC b | 0.89 ± 0.11 (12.8%) | 0.88 (0.15) | 0.97 ± 0.11 | 0.83 ± 0.08 | <0.001 *** | ||
| WC/Height | 0.58 ± 0.07 (11.3%) | 0.58 (0.09) | 0.59 ± 0.06 | 0.57 ± 0.07 | 0.107 | ||
| SUMM 6 FOLDS a | 153.6 (33.0) (21.5%) | 162.1 (46.5) | 130.0 (36.8) | 170.2 (24.6) | <0.001 *** | ||
| Body composition measured by bioimpedance | |||||||
| Fat weight (kg) | 30.2 ± 7.3 (24.0%) | 29.8 (9.7) | 28.4 ± 7.6 | 31.5 ± 6.8 | 0.053 | ||
| % Body fat | 36.2 ± 7.8 (21.5%) | 35.6 (11.8) | 30.8 ± 6.5 | 40.1 ± 6.2 | <0.001 *** | ||
| VFA (cm2) a | 141.9 ± 43.6 (30.7%) | 137.6 (70.7) | 115.4 (53.2) | 155.9 (56.2) | 0.003 ** | ||
| SMM (kg) b | 29.9 ± 6.4 (21.5%) | 27.7 (9.3) | 35.9 ± 5.2 | 25.7 ± 2.9 | <0.001 *** | ||
| % Muscle mass | 35.7 ± 5.1 (14.3%) | 35.8 (7.0) | 39.4 ± 4.5 | 33.1 ± 3.6 | <0.001 *** | ||
| SMI (kg/m2) b | 7.94 ± 0.95 (12.0%) | 7.70 (1.40) | 8.79 ± 0.74 | 7.33 ± 0.51 | <0.001 *** | ||
| Total | Men | Women | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD (%CV) | Median (IQR) | Mean± SD | Median (IQR) | Mean± SD | Median (IQR) | p Value | |
| RMR (kcal/day) (n = 56) | 1778 ± 310 (17.4%) | 1712 (472) | 2038 ± 240 | 1596 ± 206 | <0.001 *** | ||
| TEE (n = 50) | 2427 ± 453 (18.7%) | 2372 (507) | 2723 ± 419 | 2194 ± 329 | <0.001 *** | ||
| Average PAE (kcal/day) a (n = 60) | 463 ± 185 (39.9%) | 447(169.1) | 443.5 (190.7) | 454.1 (140.6) | 0.662 | ||
| METs a (n = 60) | 1.14 ± 0.09 (7.6%) | 1.12 (0.09) | 1.12 (0.10) | 1.12 (0.08) | 0.676 | ||
| Steps per day a (n = 60) | 7961 ± 3149 (42.0%) | 7281 (3445) | 6866 (2048) | 8193 (3353) | 0.048 * | ||
| PAL (n = 50) | 1.36 ± 0.10 (7.0%) | 1.36 (0.11) | 1.34 ± 0.10 | 1.38 ± 0.09 | 0.084 | ||
| PC1 | PC2 | Uniqueness | |
|---|---|---|---|
| Energy Intake | 0.903 | 0.062 | |
| Lipids | 0.896 | 0.120 | |
| SFA a | 0.895 | 0.180 | |
| Proteins a | 0.830 | 0.287 | |
| MUFA a | 0.801 | 0.279 | |
| Dietary cholesterol | 0.634 | 0.591 | |
| Carbohydrates | 0.623 | 0.515 | |
| PUFA a | 0.615 | 0.510 | |
| (Poly)phenol a | 0.881 | 0.213 | |
| Dietary fibre a | 0.814 | 0.274 | |
| Intrinsic sugars | 0.762 | 0.393 | |
| Added sugars a | 0.836 | ||
| Eigenvalues | 6.123 | 1.617 | |
| Percentage of total variance | 43.1 | 21.4 |
| PC1 | PC2 | PC3 | Uniqueness | |
|---|---|---|---|---|
| TG a | 0.860 | 0.259 | ||
| VLDL a | 0.857 | 0.264 | ||
| Waist/hip ratio | 0.764 | 0.379 | ||
| HDL a | −0.731 | 0.471 | 0.238 | |
| HOMA-IR a | 0.684 | 0.457 | ||
| SBP | 0.609 | 0.427 | 0.447 | |
| DBP | 0.560 | 0.429 | 0.502 | |
| BMI | 0.535 | 0.643 | 0.279 | |
| % Body fat | 0.972 | 0.042 | ||
| % Muscle mass | −0.941 | 0.086 | ||
| Visceral fat area | 0.932 | 0.086 | ||
| SUMM 6 skinfolds a | 0.812 | 0.286 | ||
| Total cholesterol | 0.914 | 0.159 | ||
| LDL | 0.853 | 0.270 | ||
| Eigenvalues | 4.268 | 3.717 | 2.260 | |
| Percentage of total variance (rotated solution) | 29.4 | 27.5 | 16.2 |
| PC1 | PC2 | PC3 | PC4 | Uniqueness | |
|---|---|---|---|---|---|
| Energy Intake | 0.950 | 0.072 | |||
| Lipids | 0.921 | 0.145 | |||
| SFA a | 0.865 | 0.239 | |||
| MUFA a | 0.839 | 0.275 | |||
| Proteins a | 0.792 | 0.254 | |||
| PUFA a | 0.702 | 0.492 | |||
| Carbohydrates | 0.678 | 0.457 | |||
| Dietary fibre | 0.570 | 0.545 | |||
| Dietary cholesterol | 0.523 | 0.567 | |||
| Intrinsic sugars | 0.510 | 0.731 | |||
| Polyphenols a | 0.487 | 0.716 | |||
| Added sugars a | 0.411 | 0.711 | |||
| TG a | 0.871 | 0.220 | |||
| VLDL a | 0.868 | 0.224 | |||
| Waist/hip ratio | 0.764 | 0.386 | |||
| HDL a | −0.726 | 0.472 | 0.241 | ||
| HOMA-IR a | 0.683 | 0.477 | |||
| SBP | 0.589 | 0.536 | |||
| DBP a | 0.572 | 0.529 | |||
| BMI | 0.519 | 0.653 | 0.269 | ||
| % Body fat | 0.960 | 0.047 | |||
| % Muscle mass | −0.926 | 0.090 | |||
| Visceral fat area | 0.923 | 0.087 | |||
| SUMM 6 skinfolds | 0.790 | 0.321 | |||
| Total cholesterol | 0.928 | 0.129 | |||
| LDL | 0.868 | 0.243 | |||
| Eigenvalues | 6.734 | 4.394 | 3.431 | 2.440 | |
| Percentage of total variance (rotated solution) | 24.0 | 16.8 | 15.2 | 9.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Cardero, Á.; Sierra-Cinos, J.L.; López-Jiménez, A.; Beltrán, B.; Cuadrado, C.; García-Conesa, M.T.; Bravo, L.; Sarriá, B. Characterizing Factors Associated with Excess Body Weight: A Descriptive Study Using Principal Component Analysis in a Population with Overweight and Obesity. Nutrients 2024, 16, 1143. https://doi.org/10.3390/nu16081143
Fernández-Cardero Á, Sierra-Cinos JL, López-Jiménez A, Beltrán B, Cuadrado C, García-Conesa MT, Bravo L, Sarriá B. Characterizing Factors Associated with Excess Body Weight: A Descriptive Study Using Principal Component Analysis in a Population with Overweight and Obesity. Nutrients. 2024; 16(8):1143. https://doi.org/10.3390/nu16081143
Chicago/Turabian StyleFernández-Cardero, Álvaro, José Luis Sierra-Cinos, Adrián López-Jiménez, Beatriz Beltrán, Carmen Cuadrado, María Teresa García-Conesa, Laura Bravo, and Beatriz Sarriá. 2024. "Characterizing Factors Associated with Excess Body Weight: A Descriptive Study Using Principal Component Analysis in a Population with Overweight and Obesity" Nutrients 16, no. 8: 1143. https://doi.org/10.3390/nu16081143
APA StyleFernández-Cardero, Á., Sierra-Cinos, J. L., López-Jiménez, A., Beltrán, B., Cuadrado, C., García-Conesa, M. T., Bravo, L., & Sarriá, B. (2024). Characterizing Factors Associated with Excess Body Weight: A Descriptive Study Using Principal Component Analysis in a Population with Overweight and Obesity. Nutrients, 16(8), 1143. https://doi.org/10.3390/nu16081143









