The Impact of Education Level on Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program in Denmark: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Participants and Eligibility Criteria
2.3. Randomization
2.4. Outcomes and Data Collection
2.5. Intervention Group
2.6. Control Group
2.7. Characteristics of Health Coaches
2.8. Statistical Analysis
2.9. Creating New Variables
3. Results
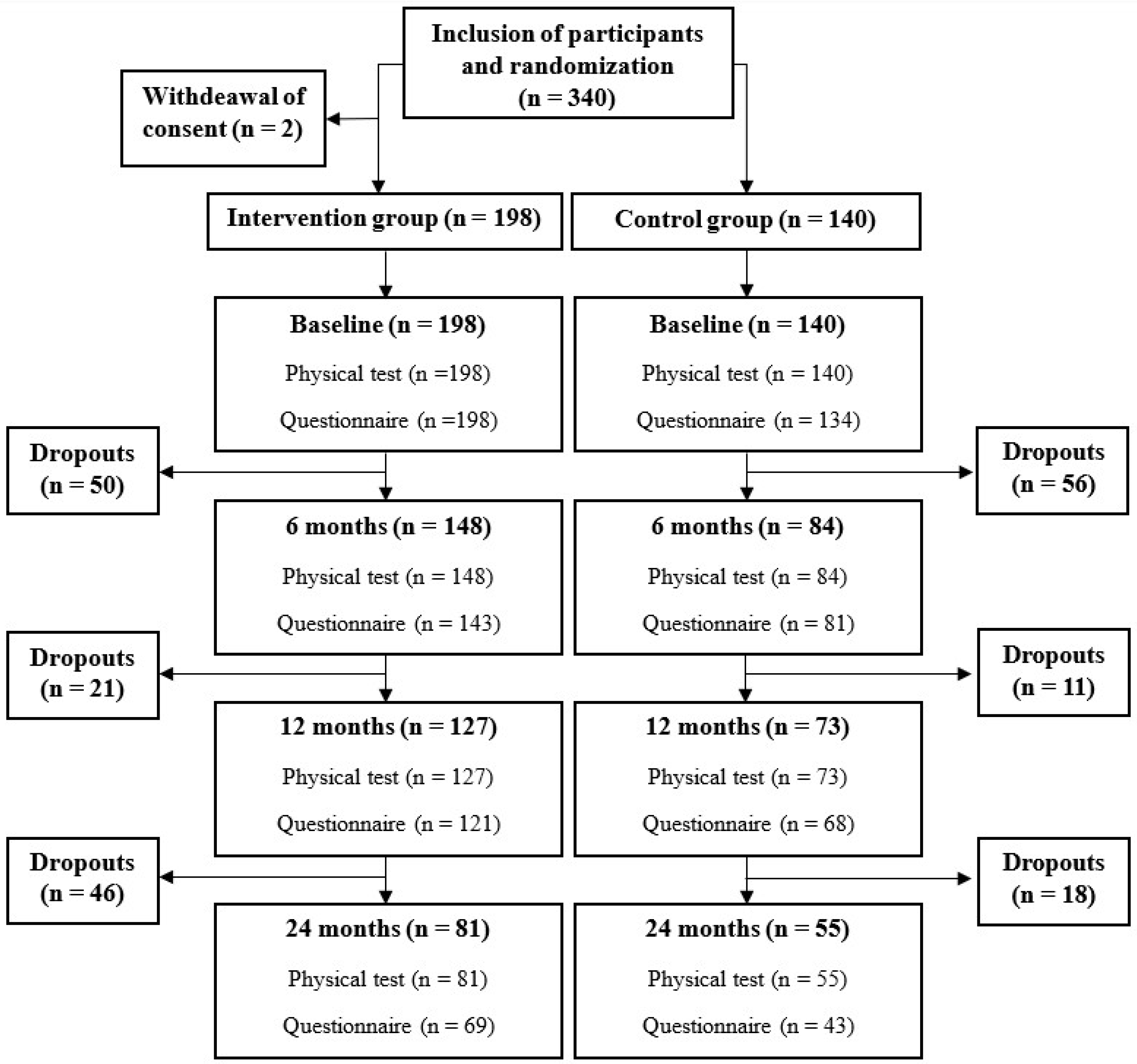
3.1. Participants Characteristics
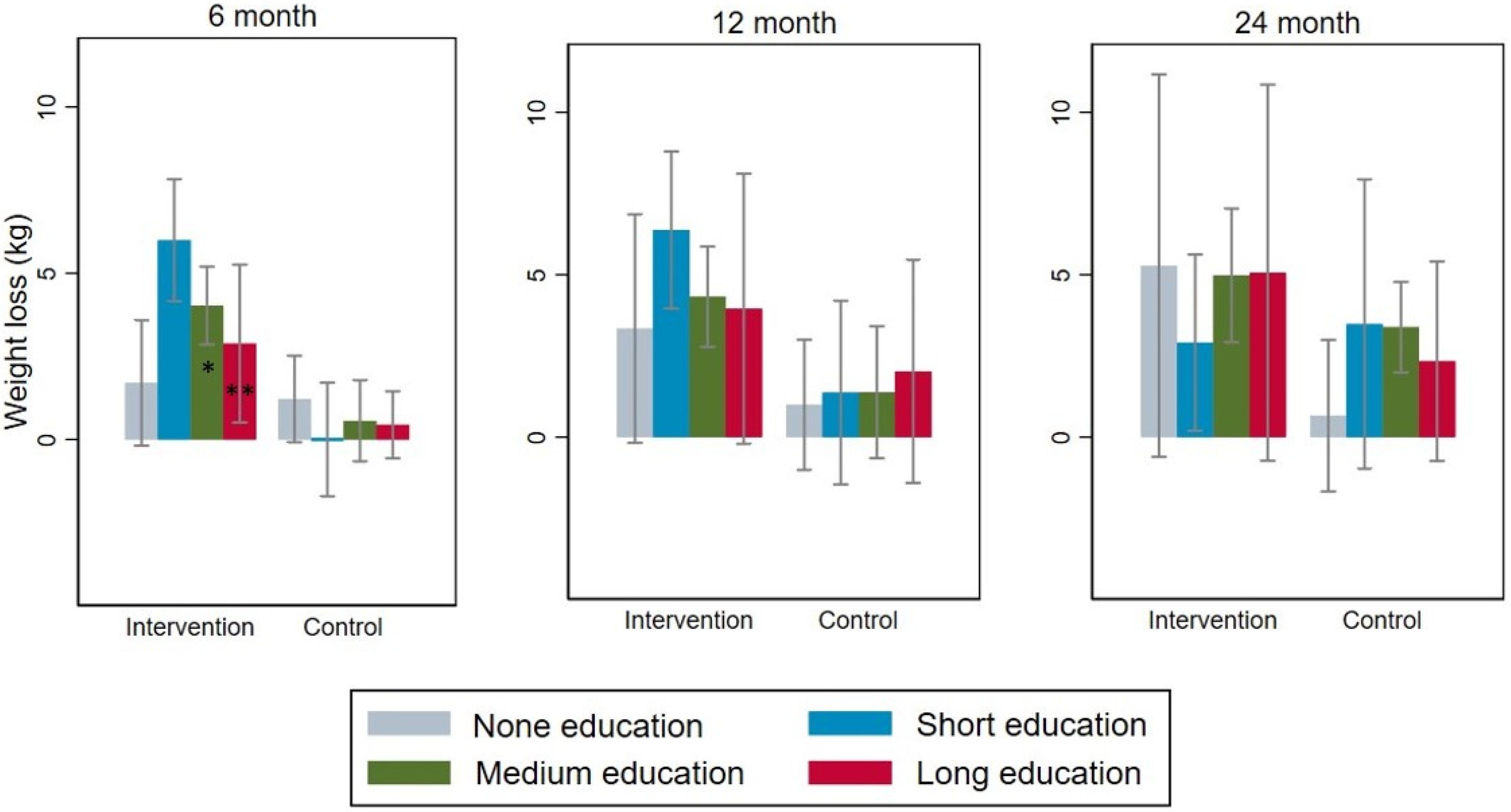
3.2. Measured Weight Loss in Different Subgroups
3.3. Self-Reported Improvement in Activity Levels and Dietary Habits
3.4. Correlation between Weight Loss, Baseline Characteristics and Behavioral Changes
3.5. Sensitivity Analyses for the Correlation between Weight Loss and Behavioral Changes
4. Discussion
4.1. Principal Findings
4.2. Comparison with Prior Research
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beckman, J.A.; Creager, M.A. Vascular Complications of Diabetes. Circ. Res. 2016, 118, 1771–1785. [Google Scholar] [CrossRef]
- Videncenter for Diabetes. Diabetes i tal. Available online: https://videncenterfordiabetes.dk/viden-om-diabetes/generelt-om-diabetes/diabetes-i-tal (accessed on 1 May 2023).
- Kristensen, J.K. Type 2-Diabetes: Opfølgning og Behandling. Available online: https://www.dsam.dk/vejledninger/type2 (accessed on 2 May 2023).
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef]
- Bo, A.; Thomsen, R.W.; Nielsen, J.S.; Nicolaisen, S.K.; Beck-Nielsen, H.; Rungby, J.; Sørensen, H.T.; Hansen, T.K.; Søndergaard, J.; Friborg, S.; et al. Early-onset type 2 diabetes: Age gradient in clinical and behavioural risk factors in 5115 persons with newly diagnosed type 2 diabetes-Results from the DD2 study. Diabetes Metab. Res. Rev. 2018, 34, e2968. [Google Scholar] [CrossRef]
- du Pon, E.; Wildeboer, A.T.; van Dooren, A.A.; Bilo, H.J.G.; Kleefstra, N.; van Dulmen, S. Active participation of patients with type 2 diabetes in consultations with their primary care practice nurses—What helps and what hinders: A qualitative study. BMC Health Serv. Res. 2019, 19, 814. [Google Scholar] [CrossRef]
- Hutchesson, M.J.; Rollo, M.E.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.J.; Callister, R.; Plotnikoff, R.; Collins, C.E. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, A.; Newham, J.J.; Bell, R.; Adamson, A.; McColl, E.; Araujo-Soares, V. Systematic review and meta-analysis of internet-delivered interventions providing personalized feedback for weight loss in overweight and obese adults. Obes. Rev. 2016, 17, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Juul, L. Overvægt og Fedme. Available online: https://www.sundhed.dk/borger/patienthaandbogen/hormoner-og-stofskifte/sygdomme/overvaegt-og-kost/overvaegt-og-fedme/#:~:text=Verdenssundhedsorganisationen%20WHO%20har%20defineret%20gr%C3%A6nser%20for%20normalv%C3%A6gt%20og,6%20BMI%20%E2%89%A540%20define (accessed on 2 May 2023).
- Hesseldal, L.; Christensen, J.R.; Olesen, T.B.; Olsen, M.H.; Jakobsen, P.R.; Laursen, D.H.; Lauridsen, J.T.; Nielsen, J.B.; Søndergaard, J.; Brandt, C.J. Long-term Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program: Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e39741. [Google Scholar] [CrossRef]
- Donkin, L.; Christensen, H.; Naismith, S.L.; Neal, B.; Hickie, I.B.; Glozier, N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011, 13, e52. [Google Scholar] [CrossRef] [PubMed]
- Myers-Ingram, R.; Sampford, J.; Milton-Cole, R.; Jones, G.D. Effectiveness of eHealth weight management interventions in overweight and obese adults from low socioeconomic groups: A systematic review. Syst. Rev. 2023, 12, 59. [Google Scholar] [CrossRef]
- Brandt, C.J.; Christensen, J.R.; Lauridsen, J.T.; Nielsen, J.B.; Søndergaard, J.; Sortsø, C. Evaluation of the Clinical and Economic Effects of a Primary Care Anchored, Collaborative, Electronic Health Lifestyle Coaching Program in Denmark: Protocol for a Two-Year Randomized Controlled Trial. JMIR Res. Protoc. 2020, 9, e19172. [Google Scholar] [CrossRef]
- Haste, A.; Adamson, A.J.; McColl, E.; Araujo-Soares, V.; Bell, R. Web-Based Weight Loss Intervention for Men With Type 2 Diabetes: Pilot Randomized Controlled Trial. JMIR Diabetes 2017, 2, e14. [Google Scholar] [CrossRef]
- Fredriksson, E.; Brekke, H.K.; Ellegård, L. Validation of four questions on food habits from the Swedish board of health and social welfare by 3-day food records in medical and nursing students. Food Nutr. Res. 2014, 58, 23438. [Google Scholar] [CrossRef][Green Version]
- Ryan, P. Integrated Theory of Health Behavior Change: Background and intervention development. Clin. Nurse Spec. 2009, 23, 161–170; quiz 171–172. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Brandt, C.J.; Clemensen, J.; Nielsen, J.B.; Søndergaard, J. Drivers for successful long-term lifestyle change, the role of e-health: A qualitative interview study. BMJ Open 2018, 8, e017466. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory. In Encyclopedia of Quality of Life and Well-Being Research; Maggino, F., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–7. [Google Scholar]
- Epstein, R.M.; Franks, P.; Fiscella, K.; Shields, C.G.; Meldrum, S.C.; Kravitz, R.L.; Duberstein, P.R. Measuring patient-centered communication in patient-physician consultations: Theoretical and practical issues. Soc. Sci. Med. 2005, 61, 1516–1528. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Miller, W.R.; Rose, G.S. Toward a theory of motivational interviewing. Am. Psychol. 2009, 64, 527–537. [Google Scholar] [CrossRef]
- Coupe, N.; Cotterill, S.; Peters, S. Tailoring lifestyle interventions to low socio-economic populations: A qualitative study. BMC Public. Health 2018, 18, 967. [Google Scholar] [CrossRef]
- Bennett, G.G.; Warner, E.T.; Glasgow, R.E.; Askew, S.; Goldman, J.; Ritzwoller, D.P.; Emmons, K.M.; Rosner, B.A.; Colditz, G.A. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch. Intern. Med. 2012, 172, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Serdula, M.K.; Mokdad, A.H.; Williamson, D.F.; Galuska, D.A.; Mendlein, J.M.; Heath, G.W. Prevalence of attempting weight loss and strategies for controlling weight. JAMA 1999, 282, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Earnest, C.P.; Church, T.S. A Retrospective Analysis of Employee Education Level on Weight Loss Following Participation in an Online, Corporately Sponsored, Weight Loss Program. J. Occup. Environ. Med. 2020, 62, e573–e580. [Google Scholar] [CrossRef] [PubMed]
| 6 Months | 12 Months | 24 Months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Attendance | Non-Attendance | p-Value | Attendance | Non-Attendance | p-Value | Attendance | Non-Attendance | p-Value | |
| n (%) | 232 (68.6) | 106 (31.4) | 200 (59.2) | 138 (40.8) | 136 (40.2) | 202 (59.8) | |||
| Age, mean (SD) | 52.0 (10.6) | 52.5 (11.9) | 0.75 | 52.3 (10.8) | 51.9 (11.3) | 0.75 | 53.5 (10.2) | 51.3 (11.4) | 0.07 |
| Sex (female), n (%) | 141 (60.8) | 72 (67.9) | 0.21 | 127 (63.5) | 86 (62.3) | 0.83 | 83 (61.0) | 130 (64.4) | 0.53 |
| Type 2 Diabetes | 115 (49.6) | 53 (50.0) | 0.94 | 98 (49.0) | 70 (50.7) | 0.76 | 65 (47.8) | 103 (51.0) | 0.56 |
| Education level, n (%) | |||||||||
| None | 37 (15.9) | 18 (17.1) | 34 (17.0) | 21 (15.3) | 28 (20.6) | 27 (13.4) | |||
| Short | 57 (24.6) | 27 (25.7) | 52 (26.0) | 32 (23.4) | 33 (24.3) | 51 (25.4) | |||
| Medium | 105 (45.3) | 54 (51.4) | 91 (45.5) | 68 (49.6) | 56 (41.2) | 103 (51.2) | |||
| Long | 28 (12.1) | 5 (4.8) | 21 (10.5) | 12 (8.8) | 17 (12.5) | 16 (8.0) | |||
| Do not know | 5 (2.2) | 1 (1.0) | 0.27 | 2 (1.0) | 4 (2.9) | 0.63 | 2 (1.5) | 4 (2.0) | 0.19 |
| Married or registered partnership, n (%) | 162 (69.8) | 54 (51.4) | <0.001 | 141 (70.5) | 75 (54.7) | <0.001 | 93 (68.4) | 123 (61.2) | 0.18 |
| Employed or student, n (%) | 171 (73.7) | 69 (65.7) | 0.13 | 147 (73.5) | 93 (67.9) | 0.26 | 100 (73.5) | 140 (69.7) | 0.44 |
| 6 Months | 12 Months | 24 Months | ||||
|---|---|---|---|---|---|---|
| Weight Change, kg [95% CI] | Weight Change, kg [95% CI] | Weight Change, kg [95% CI] | ||||
| (Number) | (Number) | (Number) | ||||
| Intervention | Control | Intervention | Control | Intervention | Control | |
| All | 3.99 [3.14; 4.84] | 0.65 [−0.10; 1.39] ** | 4.57 [3.38; 5.76] | 1.38 [0.13; 2.63] ** | 4.45 [2.79; 6.10] | 2.54 [1.13; 3.95] |
| (n = 148) | (n = 84) | (n = 127) | (n = 73) | (n = 81) | (n = 55) | |
| Male | 4.04 [2.56; 5.53] | 0.57 [−0.57; 1.71] ** | 4.86 [2.75; 6.97] | 1.38 [−0.27; 3.03] * | 5.10 [1.79; 6.33] | 2.58 [0.36; 4.66] |
| (n = 52) | (n = 39) | (n = 41) | (n = 32) | (n = 30) | (n = 23) | |
| Female | 3.96 [2.90; 5.02] | 0.71 [−0.30; 1.73] ** | 4.44 [2.97; 5.90] | 1.37 [−9.50; 3.25] * | 4.06 [2.75; 6.97] | 2.51 [−0.27; 3.03] |
| (n = 96) | (n = 45) | (n = 86) | (n = 41) | (n = 51) | (n = 32) | |
| Age ≤ 54 years | 3.86 [2.73; 4.98] | −0.18 [−1.21; 0.84] ** | 4.55 [2.79; 6.31] | 1.04 [−0.70; 2.78] * | 5.54 [2.83; 8.24] | 1.46 [−0.66; 3.58] * e |
| (n = 87) | (n = 47) | (n = 73) | (n = 40) | (n = 43) | (n = 28) | |
| Age > 54 years | 4.18 [2.83; 5.53] | 1.69 [0.67; 2.72] ** | 4.60 [3.07; 6.13] | 1.78 [−0.10; 3.67] * | 3.21 [1.41; 5.01] | 3.66 [1.78; 5.55] |
| (n = 61) | (n = 37) | (n = 54) | (n = 33) | (n = 38) | (n = 27) | |
| BMI ≤ 34 kg/m2 | 3.81 [2.61; 5.02] | 0.96 [−0.10; 2.02] ** | 4.09 [2.57; 5.60] | 1.28 [−1.12; 3.68] * | 3.57 [1.69; 5.45] | 1.98 [−0.77; 4.72] |
| (n = 69) | (n = 35) | (n = 61) | (n = 28) | (n = 42) | (n = 24) | |
| BMI > 34 kg/m2 | 4.14 [2.92; 5.36] | 0.42 [−0.63; 1.47] ** | 5.02 [3.18; 6.86] | 1.44 [−0.02; 2.89] ** | 5.39 [2.55; 8.23] | 2.98 [1.52; 4.44] |
| (n = 79) | (n = 49) | (n = 66) | (n = 45) | (n = 39) | (n = 31) | |
| T2D | 4.00 [2.80; 5.20] | 1.63 [0.58; 2.68] ** | 4.50 [3.04; 5.95] | 2.09 [0.18; 4.00] * | 5.35 [3.21; 7.50] | 3.81 [1.92; 5.71] |
| (n = 74) | (n = 41) | (n = 62) | (n = 36) | (n = 40) | (n = 25) | |
| Without T2D | 3.98 [2.74; 5.22] | −0.29 [−1.30; 0.72] ** | 4.64 [2.74; 6.55] | 0.68 [−1.00; 2.37] ** | 3.56 [0.99; 6.13] | 1.48 [−0.58; 3.53] |
| (n = 74) | (n = 43) | (n = 65) | (n = 37) | (n = 41) | (n = 30) | |
| Education level a | ||||||
| None | 1.70 [−0.30; 3.70] | 1.22 [−0.18; 2.62] | −3.34 [−0.40; 7.09] | 0.99 [−1.19; 3.17] | 5.28 [−1.15; 11.71] | 0.66 [−1.89; 3.21] |
| (n = 20) | (n = 17) | (n = 19) | (n = 15) | (n = 14) | (n = 14) | |
| Short | 5.99 [4.10; 7.88] | 2.20 [−1.81; 1.81] ** b | 6.38 [3.88; 8.88] | 1.37 [−1.64; 4.38] ** | 2.91 [0.04; 5.78] | 3.48 [−1.43; 8.38] |
| (n = 37) | (n = 20) | (n = 33) | (n = 19) | (n = 20) | (n = 13) | |
| Medium | 4.03 [2.84; 5.21] | 0.56 [−0.70; 1.82] ** c | 4.32 [2.75; 5.89] | 1.38 [−0.73; 3.49] * | 4.98 [2.87; 7.09] | 3.38 [1.90; 4.87] |
| (n = 71) | (n = 34) | (n = 61) | (n = 30) | (n = 37) | (n = 19) | |
| Long | 2.88 [0.34; 5.42] | 0.44 [−0.71; 1.59] ** | 3.95 [−0.69; 8.59] | 2.02 [−1.99; 6.04] | 5.06 [−1.86; 11.98] | 2.33 [−1.25; 5.91] |
| (n = 18) | (n = 10) | (n = 12) | (n = 9) | (n = 8) | (n = 9) | |
| Marital status | ||||||
| Married | 4.15 [3.13; 5.18] | 0.24 [−0.64; 1.12] ** | 4.90 [3.54; 6.25] | 1.38 [−0.10; 2.86] ** | 3.77 [1.70; 5.84] | 3.47 [1.70; 5.23] f |
| (n = 107) | (n = 55) | (n = 92) | (n = 49) | (n = 54) | (n = 39) | |
| Single | 3.57 [1.98; 5.15] | 1.41 [0.03; 2.79] * | 3.72 [1.20; 6.24] | 1.37 [−1.11; 3.84] | 5.80 [2.95; 8.64] | 0.28 [−1.77; 2.33] ** |
| (n = 41) | (n = 29) | (n = 35) | (n = 24) | (n = 27) | (n = 16) | |
| Employment | ||||||
| Employed/student | 3.83 [2.87; 4.79] | 0.08 [−0.77; 0.94] ** | 4.59 [3.18; 6.00] | 1.90 [0.34; 3.48] * | 4.19 [2.53; 5.85] | 2.78 [1.20; 4.36] |
| (n = 113) | (n = 58) | (n = 97) | (n = 50) | (n = 61) | (n = 39) | |
| Unemployed/retired | 4.49 [2.58; 6.41] | 1.90 [0.48; 3.32] * | 4.51 [2.24; 6.78] | 0.22 [−1.90; 2.34] ** | 5.22 [0.52; 9.93] | 1.95 [−1.28; 5.18] |
| (n = 35) | (n = 26) | (n = 30) | (n = 23) | (n = 20) | (n = 16) | |
| Everyday physical activity | ||||||
| <30 min | 3.90 [2.08; 5.71] | −0.52 [−0.68; 1.71] ** | 5.60 [−8.54; −3.37] | 0.01 [−2.12; 2.13] ** | 3.71 [−0.02; 7.43] | 2.00 [−1.16; 5.10] |
| (n = 30) | (n = 16) | (n = 25) | (n = 14) | (n = 19) | (n = 9) | |
| 30 min–2.5 h | 3.82 [2.76; 4.89] | 1.13 [0.04; 2.21] ** | 4.03 [−5.36; −2.70] | 1.63 [−0.39; 3.64] * | 4.49 [2.14; 6.82] | 1.85 [−0.17; 3.87] |
| (n = 78) | (n = 42) | (n = 67) | (n = 36) | (n = 41) | (n = 28) | |
| >2.5 h | 4.38 [2.30; 6.46] | 0.58 [−0.97; 2.14] ** | 4.62 [1.50; 7.74] | 1.82 [−0.47; 4.11] | 5.04 [1.55; 8.53] | 3.90 [1.08; 6.72] |
| (n = 40) | (n = 26) | (n = 35) | (n = 23) | (n = 21) | (n = 18) | |
| Physical exercise | ||||||
| <30 min | 4.20 [3.20; 5.20] | 0.05 [−0.89; 1.00] ** | 5.07 [3.56; 6.58] | 0.62 [−0.82; 2.05] ** | 4.11 [1.80; 6.42] | 2.00 [0.24; 3.77] |
| (n = 93) | (n = 51) | (n = 78) | (n = 44) | (n = 48) | (n = 33) | |
| 30 min–2 h | 3.24 [1.68; 4.80] | 1.62 [−3.03; −0.22] d | 3.64 [2.13; 5.15] | 2.13 [−0.59; 4.84] | 4.42 [1.77; 7.07] | 3.41 [0.44; 6.37] |
| (n = 42) | (n = 27) | (n = 38) | (n = 23) | (n = 24) | (n = 18) | |
| >2 h | 4.91 [−0.05; 9.87] | 1.28 [−1.52; 4.09] | 4.25 [−3.96; 12.46] | 4.08 [−1.82; 9.98] | 6.31 [−0.05; −12.67] | 3.08 [−3.00; 9.15] |
| (n = 13) | (n = 6) | (n = 11) | (n = 6) | (n = 9) | (n = 4) | |
| Diet | ||||||
| Unhealthy | 3.96 [2.87; 5.05] | 0.71 [−0.17; 1.60] ** | 4.93 [3.34; 6.52] | 1.59 [0.26; 2.92] ** | 4.20 [1.77; 6.63] | 2.10 [0.63; 3.57] |
| (n = 84) | (n = 47) | (n = 72) | (n = 41) | (n = 47) | (n = 33) | |
| Healthy | 4.03 [2.64; 5.42] | 0.56 [−0.75; 1.87] ** | 4.10 [2.26; 5.94] | 1.10 [−1.28; 3.48] * | 4.79 [2.58; 6.99] | 3.20 [0.30; 6.09] |
| (n = 64) | (n = 37) | (n = 55) | (n = 32) | (n = 34) | (n = 22) | |
| Baseline to 6 Months | Baseline to 12 Months | Baseline to 24 Months | ||||
|---|---|---|---|---|---|---|
| Improved/Total, (%) | Improved/Total, (%) | Improved/Total, (%) | ||||
| Intervention | Control | Intervention | Control | Intervention | Control | |
| Physical exercise | ||||||
| No education | 10/22 (45.5) | 8/17 (47.1) | 11/18 (61.1) | 8/15 (53.3) | 7/14 (50.0) | 5/11 (45.5) |
| Short education | 23/38 (60.5) | 13/22 (59.1) | 18/31 (58.1) | 10/19 (52.6) | 14/24 (58.3) | 7/13 (53.9) |
| Medium education | 36/74 (48.7) | 17/42 (40.5) | 26/58 (44.8) | 13/31 (41.9) | 18/41 (43.9) | 8/20 (40.0) |
| Long education | 6/17 (35.3) | 3/11 (27.3) | 9/13 (69.2) | 2/9 (22.2) * | 3/9 (33.3) | 0/7 (0.0) |
| Everyday physical activity | ||||||
| No education | 11/22 (50) | 11/17 (64.7) | 10/18 (55.6) | 9/15 (60.0) | 5/14 (35.7) | 6/11 (54.6) |
| Short education | 19/38 (50) | 5/22 (22.7) * | 14/31 (45.2) | 6/19 (31.6) | 13/24 (54.2) | 7/13 (53.9) |
| Medium education | 34/74 (46.0) | 12/42 (28.6) | 30/58 (51.7) | 9/31 (29.0) * | 18/41 (43.9) | 8/20 (40.0) |
| Long education | 6/17 (35.3) | 7/11 (63.6) | 5/13 (38.5) | 4/9 (44.4) | 5/9 (55.6) | 2/7 (28.6) |
| Dietary habits—Vegetables and/or root vegetables | ||||||
| No education | 8/22 (36.36) | 5/17 (29.4) | 10/18 (55.6) | 5/15 (33.3) | 3/14 (21.4) | 4/11 (36.4) |
| Short education | 19/38 (50) | 5/22 (22.7) * | 15/31 (48.4) | 7/19 (36.8) | 9/24 (37.5) | 4/13 (30.8) |
| Medium education | 36/74 (48.65) | 10/42 (23.8) ** | 22/58 (37.9) | 11/31 (35.5) | 21/41 (51.2) | 10/20 (50.0) |
| Long education | 2/17 (11.76) | 3/11 (27.3) | 4/13 (30.8) | 1/9 (11.1) | 0/9 (0.0) | 3/7 (42.9) * |
| Dietary habits—Fruit and/or berries | ||||||
| No education | 7/22 (31.8) | 4/17 (23.5) | 8/18 (44.4) | 6/15 (40.0) | 6/14 (42.9) | 5/11 (44.0) |
| Short education | 14/38 (36.8) | 6/22 (27.3) | 14/31 (45.2) | 5/19 (26.3) | 8/24 (33.3) | 1/13 (7.7) |
| Medium education | 28/74 (37.8) | 9/42 (21.4) | 16/58 (27.6) | 9/31 (29.0) | 13/41 (31.7) | 7/20 (35.0) |
| Long education | 2/17 (11.8) | 2/11 (18.2) | 4/13 (30.8) | 2/9 (22.2) | 2/9 (22.2) | 3/7 (42.9) |
| Dietary habits—Seafood | ||||||
| No education | 4/22 (18.2) | 5/17 (29.4) | 6/18 (33.3) | 5/15 (33.3) | 3/14 (21.4) | 5/11 (45.5) |
| Short education | 11/38 (29.0) | 5/22 (22.7) | 11/31 (35.5) | 4/19 (21.1) | 7/24 (28.2) | 4/13 (30.8) |
| Medium education | 23/74 (31.1) | 9/42 (21.4) | 16/58 (27.6) | 9/31 (29.0) | 6/41 (14.6) | 6/20 (30.0) |
| Long education | 4/17 (23.5) | 3/11 (27.3) | 5/13 (38.5) | 3/9 (33.3) | 3/9 (33.3) | 4/7 (57.1) |
| Dietary habits—Pastry, chocolate, sweets, soda | ||||||
| No education | 8/22 (36.4) | 10/17 (58.8) | 10/18 (55.6) | 5/15 (33.3) | 4/14 (28.6) | 5/11 (45.5) |
| Short education | 23/38 (60.5) | 11/22 (50.0) | 13/31 (41.9) | 6/19 (31.6) | 7/24 (29.2) | 5/14 (35.7) |
| Medium education | 39/74 (52.7) | 11/42 (26.2) ** | 30/58 (51.7) | 14/31 (45.2) | 17/42 (40.5) | 7/21 (33.3) |
| Long education | 3/17 (17.7) | 5/11 (45.5) | 5/13 (38.5) | 3/9 (33.3) | 0/12 (0.0) | 5/8 (62.5) ** |
| All Participants | Intervention | Control | |
|---|---|---|---|
| Beta-Coefficient [95% CI] | Beta-Coefficient [95% CI] | Beta-Coefficient [95% CI] | |
| Age (years) | 0.07 [0.01; 0.13] * | 0.076 [−0.01; 0.16] | 0.041 [−0.020; 0.10] |
| Sex (male vs. female) | −0.37 [−1.68; 0.94] | 0.085 [−1.71; 1.88] | −0.15 [−1.64; 1.35] |
| BMI (kg/m2) | −0.18 [−0.35; −0.01] * | −0.10 [−0.33; 0.13] | −0.21 [−0.41; −0.010] * |
| Without T2D vs. with T2D | −0.75 [−2.02; 0.53] | −0.02 [−1.73; 1.69] | −1.91 [−3.35; −0.48] ** |
| Education level | |||
| None vs. medium | −1.43 [−3.27; 0.42] | −2.33 [−4.88; 0.22] | 0.66 [−1.38; 2.69] |
| Short vs. medium | 0.98 [−0.61; 2.57] | 1.96 [−0.08; 4.00] | −0.56 [−2.49; 1.37] |
| Long vs. medium | −0.89 [−2.95; 1.16] | −1.14 [- 3.80; 1.51] | −0.12 [−2.58; 2.35] |
| Married or registered partnership vs. single, divorced or widow | 0.15 [−1.24; 1.54] | 0.59 [−1.32; 2.49] | −1.17 [−2.72; 0.38] |
| Employed or student vs. Unemployed or retired | −0.82 [−2.27; 0.63] | −0.66 [−2.68; 1.35] | −1.81 [−3.38; −0.24] * |
| Physical exercise | |||
| Stable vs. worsened | 1.65 [−0.39; 3.68] | 2.70 [−0.03; 5.42] * | −0.09 [−2.42–2.24] |
| Improved vs. worsened | 1.70 [−0.28; 3.67] | 2.11 [−0.52; 4.74] | 0.76 [−1.52–3.05] |
| Everyday physical activity | |||
| Stable vs. worsened | 1.93 [0.24; 3.62] * | 1.64 [−0.66; 3.94] | 1.41 [−0.57; 3.40] |
| Improved vs. worsened | 2.35 [0.81; 3.88] ** | 2.77 [0.65; 4.90] * | 0.44 [−1.30; 2.18] |
| Dietary habits—Vegetables and/or root vegetables | |||
| Stable vs. worsened | 0.82 [−1.26; 2.90] | 1.49 [−1.57; 4.55] | −0.39 [−2.57; 1.79] |
| Improved vs. worsened | 3.20 [1.06; 5.34] ** | 4.09 [1.01; 7.17] * | 0.057 [−2.34; 2.46] |
| Dietary habits—Fruit and/or berries | |||
| Stable vs. worsened | 1.22 [−0.60; 3.05] | 0.98 [−1.66; 3.63] | 0.79 [−1.12; 2.69] |
| Improved vs. worsened | 2.08 [0.10; 4.06] * | 1.24 [−1.53; 4.02] | 1.73 [−0.54; 4.01] |
| Dietary habits—Seafood | |||
| Stable vs. worsened | −0.79 [−3.71; 2.13] | −0.10 [−4.18; 3.98] | −2.21 [−5.30; 0.89] |
| Improved vs. worsened | 1.15 [−1.94; 4.23] | 1.52 [−2.76; 5.80] | 0.04 [−3.27; 3.34] |
| Dietary habits—Pastry, chocolate, sweets, soda | |||
| Stable vs. worsened | 0.90 [−1.24; 3.05] | 2.81 [0.095; 5.53] * | −1.94 [−4.70; 0.83] |
| Improved vs. worsened | 2.31 [0.16; 4.45] * | 3.68 [1.02; 6.35] ** | −0.58 [−3.34; 2.23] |
| Intervention vs. control | 3.34 [2.09; 4.60] ** | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahin, L.; Olesen, T.B.; Olsen, M.H.; Laursen, D.H.; Christensen, J.R.; Brandt, C.J. The Impact of Education Level on Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program in Denmark: A Randomized Controlled Trial. Nutrients 2024, 16, 795. https://doi.org/10.3390/nu16060795
Shahin L, Olesen TB, Olsen MH, Laursen DH, Christensen JR, Brandt CJ. The Impact of Education Level on Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program in Denmark: A Randomized Controlled Trial. Nutrients. 2024; 16(6):795. https://doi.org/10.3390/nu16060795
Chicago/Turabian StyleShahin, Luma, Thomas Bastholm Olesen, Michael Hecht Olsen, Ditte Hjorth Laursen, Jeanette Reffstrup Christensen, and Carl J. Brandt. 2024. "The Impact of Education Level on Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program in Denmark: A Randomized Controlled Trial" Nutrients 16, no. 6: 795. https://doi.org/10.3390/nu16060795
APA StyleShahin, L., Olesen, T. B., Olsen, M. H., Laursen, D. H., Christensen, J. R., & Brandt, C. J. (2024). The Impact of Education Level on Weight Loss in a Primary Care-Anchored eHealth Lifestyle Coaching Program in Denmark: A Randomized Controlled Trial. Nutrients, 16(6), 795. https://doi.org/10.3390/nu16060795








