Abstract
Excessive body fat is associated with various comorbidities including cardiovascular disease, type 2 diabetes mellitus and certain types of cancer. The search for effective, relatively easy to maintain body-fat reduction interventions has been ongoing. We aimed to review the current literature to assess the effectiveness of high-intensity interval training with and without dietary supplementation on body fat loss, concentration of markers of metabolic health and aerobic capacity of adults with overweight and obesity. Seventy full-text articles were assessed to determine their eligibility and thirteen were included in the review. The methodology of this systematic review was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Almost all studies (93%) demonstrated effectiveness of high-intensity interval training of various protocols in reducing body fat, improving metabolic health and aerobic capacity of adults with overweight and obesity. These effects were enhanced by an addition of a dietary supplement, such as green tea or ginger or other. Although combining HIIT with dietary supplementation seem to improve body composition, metabolic health and aerobic capacity in adults with overweight and obesity in some instances to a greater extent than HIIT alone, it does not seem to be necessary to combine these two interventions.
1. Introduction
The prevalence of overweight (BMI ≥ 25 kg/m2) and obesity (BMI ≥ 30 kg/m2) has been dramatically increasing since the last century and these disorders are now affecting 59% of adults and almost 1 in 3 children in Europe [1,2]. Worldwide, approximately 2 billion adults are overweight and of these around 650 million are obese [3]. It is expected that 2.7 billion adults will be overweight and over 1 billion will be obese by 2025 [4].
An abnormal or excessive body fat (BF) accumulation is associated with impaired cellular metabolism [1] and various comorbidities. These include cardiovascular disease [5], type 2 diabetes mellitus [6], non-alcoholic fatty liver disease [6], certain types of cancer [5] and mental disorders [7]. The BF accumulation and its related comorbidities involve complex pathogenesis, including adipokines dysregulation (pro-inflammatory > anti-inflammatory profile) [8] and inhibition of browning of the white adipose tissue, which leads to reduced dissipation and increased storage of chemical energy [9]. Microbiota dysbiosis characterised by a depletion of probiotics that may increase the risk of colorectal cancer [10] and immune dysregulation with immune cells shifting from the anti-inflammatory to pro-inflammatory phenotype are other hallmarks of BF accumulation [8,11].
A sedentary lifestyle and reduced physical activity in conjunction with unhealthy hypercaloric diet [12], rich in glycaemic (digestible) carbohydrates (CHO) such as sugar and refined CHO [13,14] and fat [14] and genetic, endocrine, metabolic and environmental factors are viewed as the main causes of the excessive BF [15]. Reducing BF is generally achievable for a person with overweight or obesity; however, maintaining the reduced BF level has been proven to be challenging and only a very small percentage of these individuals succeed in maintaining the results [15]. Therefore, the quest for finding effective and relatively easy to adhere to and to maintain therapeutic interventions has been ongoing.
Since compliance with standard body mass management programmes is notoriously poor [16], various dietary strategies are recommended to decrease BF and amongst these are dietary supplements (DS). DS for BF management can be classified into herbs and botanicals, vitamins, minerals, and amino acids [17]. A recent excellent systematic review has demonstrated that most DS as aids in reducing BF have a limited, high-quality evidence-based efficacy [18]. For instance, out of twenty-two studies on calcium-vitamin D-supplementation, only three demonstrated significant body mass reduction over time and of the five papers with low bias (23%), none showed significant changes in body mass between groups (experimental vs. placebo). Out of sixteen studies on green tea supplementation with an overall low degree of bias, only two (13%) demonstrated statistically significant improvements in %BF ranging from 1.7 to 2.3%, with no statistical differences between treatment and placebo groups. On the other hand, ephedrine–caffeine (often taken together) [18] supplementation seemed to be more effective as of the ten studies with a low risk of bias, 50% reported significant BF reduction ranging from 0.3 to 4.9 kg but results on inter-group pre/post changes were not reported. The authors concluded that well-designed, randomised, double-blinded controlled trials of sufficient duration are needed to show efficacy of DS in BF loss and suggested that adding DS to lifestyle interventions to enhance efficacy would be helpful to explore [18].
High-intensity interval exercise training (HIIT) has been gaining popularity for its time-saving characteristics, being perceived as more enjoyable and giving a greater sense of accomplishment when compared to traditional moderate intensity exercise training (MICT) [19]. HIIT can be defined as a near-maximal (intensity of 85–95% of maximal heart rate), or maximal or supramaximal, bouts of between ≤ 30 s and 6 min of work, interspersed with 2–5 min of rest [20]. HIIT has been shown to improve a number of cardiovascular and metabolic risks factors in healthy, older and non-obese females [21], sedentary males with overweight [22], patients with coronary artery disease [23] and patients with type 1 diabetes [24]. There is growing evidence that HIIT elicits greater benefits than MICT on a range of health markers in the healthy and those suffering from chronic illnesses [25,26]. A meta-analysis of the effectiveness of HIIT and MICT on BF loss demonstrated that both regimens could induce only modest body composition improvements in individuals with overweight or obesity [27]. However, some studies in people with obesity revealed that HIIT can significantly reduce BF [28,29]. Without the consensus to whether HIIT regimens are effective for BF loss and whether the BF loss can be maintained, other therapeutic interventions such as dietary supplementation (DS) has been used in combination with HIIT to assess their effectiveness in BF reduction and markers of metabolic health.
To the best of the authors’ knowledge, to date, no study has analysed the synthesis of the results of HIIT combined with DS in adults with overweight and obesity. Therefore, the aim of the study was to examine the effectiveness of HIIT combined with DS on BF loss, markers of metabolic health and aerobic capacity in adults with overweight and obesity.
2. Materials and Methods
2.1. Study Design
The methodology of this systematic review was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Prisma—internet) (see Supplementary Materials File S1).
2.2. Inclusion and Exclusion Criteria
In this systematic review, the inclusion criteria for the study were as follows: (1) randomised controlled trials (RCTs) (including double-blind RCTs), (2) males and females 18–50 years old, (3) individuals with overweight/obesity diagnosed based on the WHO guidelines (BMI ≥ 24.99 kg/m2) [1,2], (4) no other health conditions, (5) HIIT combined with DS.
The exclusion criteria were: (1) a study design different than RCT (2) a study group including children, adolescents or people aged over 50 years old, (3) a poor methodological design, (4) no full text available, (5) manuscript written in a language other than English, (6) lack of data, (7) HIIT not combined with DS or DS not combined with HIIT.
2.3. Literature Search
A search of the selected electronic databases (Pubmed, SCOPUS, ScienceDirect) was conducted by two authors (SS, AG). They identified all studies on HIIT combined with DS and their effects on BF in individuals with overweight and obesity conducted between November 2013 and November 2023. The following methods were used during the search: (a) data mining, and (b) data discovery and classification. The search terms were combined by Boolean logic (AND/OR) in PubMed, SCOPUS and ScienceDirect databases. The search was undertaken using the following 7 prioritised keyword combinations in English: ‘HIIT’, ‘adiposity, ‘supplementation, ‘overweight’, ‘obesity’, ‘adipose tissue’, ‘body fat’ and ‘reduction’. Furthermore, two other authors (EG, BH) with expertise in somatic analysis, overweight and obesity, HIIT and DS reviewed the reference lists of the included studies and screened Google Scholar for additional studies. The corresponding authors of the selected publications were also contacted directly if the crucial data were not available in the original articles.
2.4. Methodological Quality of the Included Studies (Risk of Bias)
The methodological quality of the included studies was evaluated based on a revised Cochrane risk of bias tool—RoB 2.0 tool (version of 22 August 2019) that is known to be suitable for individually-randomised, parallel-group and cluster RCT [30]. RoB 2.0 tool is also known to be the most recommended risk of bias tool for RCT [30]. The tool consist of five bias domains: (1) risk of bias arising from the randomisation process, (2) risk of bias due to deviations from the intended interventions (effect of assignment interventions/adhering the intervention), (3) missing outcome data, (4) risk of bias in measurement of the outcome and (5) risk of bias in the selection of the reported results, that is followed by an ‘overall risk of bias’ assessment [31]. Each study was read and ranked by two independent investigators (EG, SS) with one of the following response options: (1) ‘yes’ (2) ‘probably yes’, (3) ‘probably no’, (4) ‘no’, (5) ‘no information’, (6) ‘no applicable’ to a series of signalling questions in each of the five domains. Moreover, an independent co-author (AZ) was designated to resolve all discrepancies that could occur among investigators during the assessment. Based on the original RoB 2.00 tool, the responses that were underlined in green were believed to have a low risk of bias, while the responses underlined in red were believed to have a high risk of bias [31]. Next, based on the obtained responses, each investigator (in each of the domains) chose one of the following risk of bias judgment options, i.e., (i) ‘low’, (ii) ‘high’ or (iii) ‘some concerns’ [31]. According to the recommendations for the overall risk of bias judgement, if all domains were judged as ‘low’ risk of bias, the overall risk of bias was low, while if one domain was judged as a ‘high’ risk of bias, or if several domains were judged to have ‘some concerns’, the overall risk of bias was high. Moreover, if at least one domain was judged as ‘some concerns’, but simultaneously there was no domain judged as ‘high’ risk of bias, the overall risk of bias was judged to have some concerns [31]. Furthermore, based on the original recommendations from Sterne et al. [31], RoB 2.0 tool was used to assess the risk of bias based on a given outcome, rather than for a whole RCT.
3. Results
3.1. Study Selection
The flow of the systematic review is presented in Figure 1. Seventy full-text articles were assessed to determine their eligibility, while fifteen met the inclusion criteria and were subjected to a detailed analysis and assessment of their methodological quality (see Table 1).
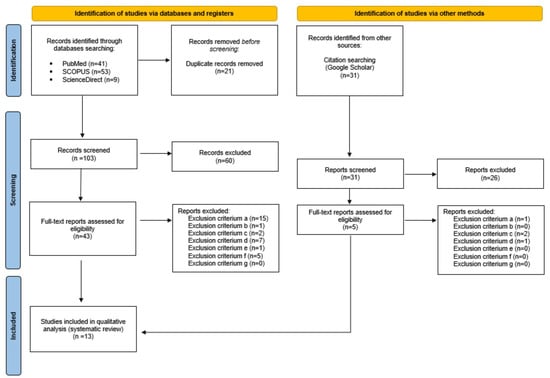
Figure 1.
PRISMA flow diagram detailing the study inclusion process (PRISMA—internet).

Table 1.
The assessment of the methodological quality of the included studies (risk of bias) using the Cochrane RoB 2.0 tool (version of 22 August 2019) for RCT. Studies are presented in order of the publication year.
The majority of the reports that were assessed for their methodological quality were considered to have a low overall risk of bias and were judged eligible to be included in the systematic review, while some of the publications were considered to have some concerns of eligibility and none of the reports were judged with a high risk of bias. The initial agreement of the two independent investigators (EG, BH) was 90%. All discrepancies among the investigators were resolved by an expert evaluation by an independent co-author (AZ). Thirteen full-text articles were finally included in the systematic review (see Table 2).

Table 2.
The summary of the studies from 2014 to 2023 evaluating the effects of HIIT and supplementation on reduction of body fat in individuals with overweight and obesity. Presented based on DS classification [17].
3.2. Study Characteristics
A comparison of the effects of HIIT combined with DS on the selected variables analysed in the reviewed articles (see Table 1) is presented in Figure 2. It was found that body build and composition (52%) were the variables most frequently impacted by the interventions.
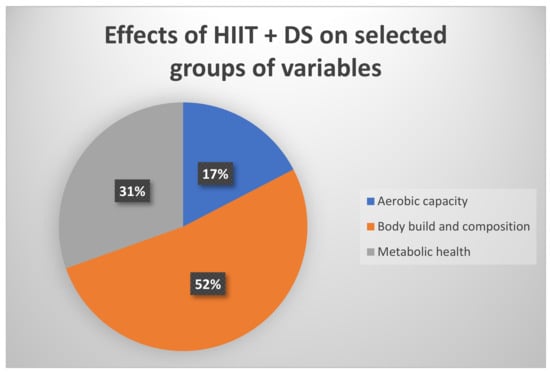
Figure 2.
Effects of HIIT and DS (%) on selected groups of analysed variables, i.e., aerobic capacity, body build and composition, metabolic health.
4. Discussion
A careful examination of the current scientific studies on the HIIT combined with DS on BF loss, aerobic fitness, and selected indices of metabolic health in adults with overweight and obesity yielded partially inconsistent findings. Nevertheless, this qualitative analysis found that HIIT combined with adequate DS can induce BF loss, reduce or increase blood concentration of metabolic health markers and improve aerobic capacity to a greater extent rather than DS or HIIT alone (see Table 2) in adults with overweight and obesity.
4.1. Effects of HIIT Combined with Supplementation on BF
The majority of the analysed scientific articles demonstrated statistically significant effects of HIIT and DS on BF and induced a reduction of %FAT, body fat mass, BMI, or waist-to-hip ratio [32,33,36,39,40,41,42,43,44]. On the contrary, two investigations [35,37] did not find any effects of HIIT combined with DS on BF in older adults with overweight and obesity. These inconsistencies could be explained mainly by the differences in the (1) HIIT protocol, (2) type, daily dose and duration of DS and (3) characteristics of the participants (sex, age, anthropometric measurements).
4.1.1. HIIT: The Most Popular Protocol
Among different HIIT protocols, the 40-m shuttle run test was implemented most frequently [33,34,36,38,41] and was combined with ginger (3000 mg/daily) [33,34] or green tea supplementation [36,38], which proved to be effective in reducing BF of participants with overweight and obesity to a greater extent than HIIT or DS alone [33,36,38]. Conversely, Sheikholeslami-Vatani et al. [41] found that the 40-m shuttle run protocol combined with vitamin D3 (2000 IU/daily) or placebo supplementation both had a similar effect on the indicators of body fat loss: %FAT, BM and BMI, whereas Saghebjoo et al. [37] demonstrated that the 40-m shuttle run HIIT combined with L-arginine (6 g/daily) did not cause a significant reduction of the BF mass. The above-mentioned synthesis of the results allowed us to conclude that a 40-m shuttle run test as a HIIT protocol may be effective in inducing BF loss both alone and in combination with DS, especially with green tea.
4.1.2. HIIT: Other Protocols
Apart from the 40-m shuttle run, other HIIT protocols had been implemented in the reviewed studies. Some of them used longer HIIT sessions, lasting between 30 and 60 min [42,43,44], whilst others focused on much shorter sessions [32,40] lasting between 8 and 30 s. Regardless of its duration, each HIIT session combined with DS (see Table 2) has been found effective in improving the body composition of participants with overweight and obesity, especially in reducing their BF. Regarding the duration of HIIT, shorter (6-week) and longer (up to 12 week) HIIT programmes were as effective in reducing BF in individuals with overweight and obesity.
4.1.3. DS: Type and Dose Effect on BF
However, the effectiveness of a combined HIIT + DS intervention on body composition improvement seemed to depend on the type and dose of the DS. For instance, Lithgow et al. [35] demonstrated that a 6-week HIIT alone significantly reduced the waist and hip circumference of adults with overweight and obesity, with vitamin D3 (100 μg/day = 4000 IU/day) not proffering any additional effects. Similar observations were made by Sheikholeslami-Vatani et al. [41] who implemented a two-times lower dose of vitamin D3 (2000 IU/day) supplementation but a longer by two weeks intervention compared to Lithgow et al. [35]. The authors observed that both HIIT + vitamin D3 and HIIT + placebo reduced %FAT and BMI significantly (p < 0.05) and to a similar extent in males with overweight.
4.1.4. HIIT + DS: Sex-Based Differences in BF Responses
Minor sex-based differences in the intrinsic responses to HIIT and DS were observed. Hirsch et al. [39] demonstrated that compared to females, males tended to have greater muscular adaptations (i.e., thigh muscle size and muscle quality) to HIIT alone and HIIT combined with essential-amino acid DS compared to females. In females, HIIT + EEA induced greater improvements in the muscle mass than HIIT alone, which suggests that EAA may support greater increases in muscle mass, especially in females. The sex-based dissimilarities could be attributed to hormonal differences between males and females, especially in the secretion of anabolic hormones and growth factors that induce muscle mass grow and in the skeletal muscle fibre-type composition [45] that could contribute to the body’s biochemical responses to HIIT and EAA supplementation.
Unfortunately, the currently available scientific literature that has examined the effects of HIIT combined with DS did not provide enough data to indicate the best supplement for a reduction of BF mass. Nevertheless, based on the detailed examination of the current scientific studies a direct effect of HIIT combined with several supplements on the improvement of body composition, especially BF reduction can be confirmed (see Table 2).
4.2. Effects of HIIT Combined with Supplementation on Metabolic Markers
The reviewed studies have analysed various markers of metabolic health in participants with overweight and obesity. In the current study, the effects of HIIT + DS on the most relevant metabolic markers are being discussed.
4.2.1. Adipokines and Insulin
Adipokines are cytokines secreted by white and brown adipocytes that signal the functional status of these cells to targets in the muscle, blood vessels, liver, pancreas, brain and other tissues [46]. Adipokines exert numerous functions, including regulation of carbohydrate and lipid metabolism, appetite, immune functions (pro-and anti-inflammatory adipokines), development and maintenance of muscle mass, and many others [47,48]. Enhanced expression of pro-inflammatory cytokines in obesity plays a role in inducing insulin resistance [49], the state characterised by impaired insulin-stimulated glucose uptake by myocytes and adipocytes, with reduced inhibition of liver glucose production [50]. Consequently, elevated fasting glucose levels and the inability to effectively clear glucose from the circulation during the post-prandial state will occur [51], eventually leading to type 2 diabetes characterised by chronic hyperglycaemia and hyperinsulinaemia [52]. Adipokine dysregulation is observed in obesity and contributes to obesity-related disorders [46]. In the current review, five studies [32,37,42,43,44] assessed the effects of HIIT + DS on blood adipokines and insulin homeostasis and four of them found beneficial modifications [32,42,43,44]. Whereas the effects of HIIT alone or in combination with DS on fasting glucose and insulin, as the indicators of insulin resistance, without the effects of HIIT + DS on adipokines were assessed by two studies [35,41], which, interestingly, had chosen similar HIIT protocols and vitamin D3 supplementation.
Adipokines
Dunn et al. [32] demonstrated that a 12-week intervention consisting of 8-s sprint on a manual cycle ergometer + 12-s rest, 3 × a week combined with the ω-3 fatty-acids supplementation and a low-glycaemic diet, significantly reduced serum IL-6. This is an important finding as IL-6 is a pro-inflammatory cytokine that plays a role in insulin resistance [53]. The authors also observed a tendency for adiponectin to rise in response to the intervention. In contrast to IL-6, higher levels of adiponectin, an insulin-sensitising cytokine, are associated with augmented glucose and lipid metabolism preventing hyperinsulinaemia [46]. Indeed, this observation was accompanied by a significant reduction in fasting insulin and a tendency for improved insulin resistance index (HOMA IR), suggesting increased sensitivity of the insulin-target cells and better metabolic health. Conversely, Saghebjoo et al. [37] did not observe any significant effects of HIIT (30-s sprint, repeated 4–6 times depending on the week of HIIT) + L-arginine supplementation on serum adiponectin in males with overweight.
Leptin is one of the key adipokines produced by white fat cells and is concerned with suppression of appetite, hence, energy homeostasis, and inflammation [46,54]. Its serum concentration positively correlates with BF mass, and leptin resistance is another feature of obesity and type 2 diabetes [55]. In the current review, only one study assessed the effects of HIIT + DS on leptin [44]. The authors found that HIIT consisting of 30 min exercise sessions combined with citrulline (an amino acid) significantly reduced serum leptin in older adults with obesity and HIIT+ citrulline-induced effects were more profound compared to HIIT alone [44]. Reduction of leptin in response to HIIT + citrulline was accompanied by a significant reduction in the total android BF mass and a tendency for increased adiponectin, the results not observed in response to HIIT alone.
In their two studies, Saeidi et al. [42,43] observed beneficial effects of a 12-week high-intensity functional training Cross-fit®, a form of HIIT [56], combined with either astaxanthin [42] or spinach-derived thylakoid [43] on selected markers of metabolic health. Cross-fit® + astaxanthin significantly reduced CTRP2, CTRP9, myostatin and growth differentiation factor-15 (GDF15) [42]. In obesity, these adipokines have been shown to be elevated and to negatively affect lipid and glucose metabolism, and skeletal muscle homeostasis [57,58,59,60]. Whereas Cross-fit® + spinach-derived thylakoid decreased the proinflammatory leptin and resistin and increased the anti-inflammatory adiponectin and omentin in males with obesity, suggesting a reduction of inflammation, a feature of BF accumulation [8,11]. These findings were accompanied by reduced insulin resistance [42,43] and the beneficial metabolic effects were greater in the combined intervention demonstrating a synergistic effect of HIIT and astaxanthin/spinach-derived thylakoid.
Insulin
Lithgow et al. [35] demonstrated that HIIT (cycling for 1 min × 10 repetitions, 3 × week for 6 weeks) significantly reduced fasting insulin and glucose plasma levels, improving insulin sensitivity in males and females with overweight and obesity, whilst, interestingly, the addition of vitamin D3 appeared to attenuate the HIIT-induced improvement in glucose tolerance.
Sheikholeslami-Vatani et al. [41] revealed reduced fasting insulin, but not fasting glucose, in response to HIIT of a similar protocol [35], but a slightly longer duration of the investigation and a lower dose of vitamin D3 supplementation (2000 IU/day vs. 4000 IU/day compared to Lithgow et al. [31]. Similarly, vitamin D3 supplementation did not proffer any additional positive effects on glucose tolerance during an oral glucose tolerance test or fasting insulin levels suggesting a superior role of HIIT in achieving such improvements.
4.2.2. Aerobic Capacity
Overweight and obesity are associated with reduced aerobic capacity and exercise tolerance which will negatively affect daily energy expenditure associated with physical activity and/or exercise and will further augment BF accumulation [61]. Therefore, improvements in aerobic capacity are of significant health importance and indicate improvement in the cardio-respiratory systems [62]. In the present review, nearly a half of studies assessed the effects of HIIT with or without DS on VO2max of adults with overweight and obesity. Maximal oxygen uptake (VO2max or VO2peak in patients with reduced exercise tolerance) is considered the golden standard of cardiopulmonary and muscle cell fitness [62]. VO2max increased in response to HIIT alone or combined with ω-3 fatty acids and low-glycaemic diet [32], green tea [38], ginger [33,34], astaxanthin [42] and spinach-derived thylakoid [43]. Ghasemi et al. [38] also found a significant elevation of PGC-1α, a key regulator of mitochondrial biogenesis in muscle, in response to HIIT + green tea, suggesting an improvement of cellular aerobic metabolism [63]. Apart from one [33], all studies demonstrated greater improvements in VO2max when HIIT was combined with DS.
It is worth noting that the type, dose and duration of dietary supplementation as well as participants’ characteristics, including sex, age and anthropometric indices could be responsible for the variability of the findings of the reviewed studies. In order to fully understand the complexity of interactions that occur between the intrinsic biochemical processes further studies are needed, including meta-analysis, to evaluate the effects of HIIT and DS on the reduction of BF, improvement of metabolic markers and aerobic capacity of adults with overweight and obesity.
5. Limitations and Strengths
While this qualitative analysis contributes to the current body of literature, there are some limitations that need to be addressed. The main limitation of the current study is a small number of studies that have investigated HIIT combined with DS in population of people with overweight and obesity, which did not allow for conducting a quantitative analysis that would allow for general interference. Moreover, the analysed studies were conducted with various number of participants including age and sex differences. Moreover, HIIT protocols differed in duration. In addition, various types and doses of dietary supplements make generalisation impossible. Therefore, further research is needed to fully understand the complexity of DS combined with HIIT that should be focused on delivering knowledge on an adequate type and dose of DS for people with overweight and obesity, that can be applied for healthy reduction of the adipose tissue. Moreover, there is still a need for studies to develop a universal model of HIIT protocol that can be combined with DS and applied to individuals with overweight and obesity. The main strength of the present study is the systematic review of the latest reports from the last decade that have examined the HIIT combined with DS in adults with overweight and obesity (similar age range). Moreover, the majority of the included studies were evaluated to be perfectly eligible for this analysis. The authors believe that the novelty of the presented research problem and undertaking the hitherto unexplored aspects in scientific research will enable a better understanding of the process of implementing HIIT in this population. It may also help to optimise HIIT programmes by using interventions based on sex-based strengths combined with specific DS.
6. Conclusions
- In general, HIIT combined with DS seems to induce the reduction of BF mass and improve metabolic health in adults with overweight and obesity; however, its effectiveness is related to several variables, including sex, type and dose of DS and HIIT protocol;
- The 40-m shuttle run test could be recommended as an effective form of HIIT for targeting overweight and obesity;
- It is difficult to point out the best type of DS for the reduction of BF in population with overweight and obesity; however, green tea seems to be effective.
- HIIT seems to be effective in reducing insulin resistance and does not seem to require being combined with DS;
- HIIT combined with DS green tea, ginger, astaxanthin or spinach-derived thylakoid may be more effective in improving aerobic capacity of adults with overweight and obesity than HIIT alone;
- Although combining HIIT with dietary supplementation seems to improve body composition, metabolic health and aerobic capacity in adults with overweight and obesity to a greater extent than HIIT alone, but it does not seem to be necessary to combine these two interventions.
7. Practical Implications
Individuals with overweight and obesity can face different barriers to exercise, including lack of time, feelings of negative body image and lack of confidence in exercising in front of others [64]. Therefore, HIIT with its time-consuming characteristics and its adaptability to a person’s level of exercise tolerance, may be a good solution for BF loss, improvement of metabolic health and aerobic capacity intervention. Some of these effects (i.e., profile of adipokines and aerobic capacity) may be enhanced by the addition of DS.
For instance, HIIT could be implemented into a daily routine by running instead of walking to a bus stop or up the stairs, skipping, hopping, performing jumping jacks at home or during a break at work, or interspersing moderate-intensity exercise such as jogging, swimming or cycling with intense, short bouts of the exercise. DS, such as green tea could be consumed prior to a HIIT session to enhance its BF lowering effects, potentially improve the profile of adipokines and aerobic capacity. Although, it was not within the scope of the current work, it would also be interesting to evaluate whether adding green tea, ginger, spinach or astaxanthin-rich algae, yeast, salmon, trout, krill, shrimp or crayfish [65].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu16030355/s1, File S1: PRISMA 2020 Checklist. Reference [66] is cited in the Supplementary Materials.
Author Contributions
Conceptualisation, E.G., B.H. and S.S.; methodology, E.G. and A.Z.; software, S.S.; validation, A.Z.; formal analysis, E.G., investigation, E.G., B.H. and S.S.; resources, S.S. and A.G.; data curation, S.S.; writing—original draft preparation, E.G., writing—review and editing, B.H.; visualisation, E.G., supervision, A.Z.; project administration, E.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. World Health Organ. Tech. Rep. Ser. 2000, 894, 1–253. [Google Scholar]
- World Health Organization. WHO European Regional Obesity Report 2022; WHO Regional Office for Europe: Copenhagen, Denmark, 2022; Available online: https://iris.who.int/bitstream/handle/10665/353747/9789289057738-eng.pdf (accessed on 14 December 2023).
- World Health Organization. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 January 2024).
- Boutari, C.; Mantzoros, C.S. A 2022 update on the epidemiology of obesity and a call to action: As its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism 2022, 133, 155217. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Leitner, D.R.; Frühbeck, G.; Yumuk, V.; Schindler, K.; Micic, D.; Woodward, E.; Toplak, H. Obesity and Type 2 Diabetes: Two Diseases with a Need for Combined Treatment Strategies—EASO Can Lead the Way. Obes. Facts 2017, 10, 483–492. [Google Scholar] [CrossRef]
- Alford, S.; Patel, D.; Perakakis, N.; Mantzoros, C.S. Obesity as a Risk Factor for Alzheimer’s Disease: Weighing the Evidence. Obes. Rev. 2018, 19, 269–280. [Google Scholar] [CrossRef]
- Jung, U.J.; Choi, M.-S. Obesity and Its Metabolic Complications: The Role of Adipokines and the Relationship between Obesity, Inflammation, Insulin Resistance, Dyslipidemia and Nonalcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2014, 15, 6184–6223. [Google Scholar] [CrossRef]
- Zhang, X.; Ha, S.; Lau, H.C.-H.; Yu, J. Excess Body Weight: Novel Insights into Its Roles in Obesity Comorbidities. Semin. Cancer Biol. 2023, 92, 16–27. [Google Scholar] [CrossRef]
- Cani, P.D.; Van Hul, M.; Lefort, C.; Depommier, C.; Rastelli, M.; Everard, A. Microbial Regulation of Organismal Energy Homeostasis. Nat. Metab. 2019, 1, 34–46. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Bodzin, J.L.; Saltiel, A.R. Obesity Induces a Phenotypic Switch in Adipose Tissue Macrophage Polarization. J. Clin. Investig. 2007, 117, 175–184. [Google Scholar] [CrossRef]
- Hall, K.D.; Farooqi, I.S.; Friedman, J.M.; Klein, S.; Loos, R.J.F.; Mangelsdorf, D.J.; O’Rahilly, S.; Ravussin, E.; Redman, L.M.; Ryan, D.H.; et al. The Energy Balance Model of Obesity: Beyond Calories in, Calories Out. Am. J. Clin. Nutr. 2022, 115, 1243–1254. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond ‘Calories In, Calories Out’. JAMA Intern. Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef]
- Wali, J.A.; Ni, D.; Facey, H.J.W.; Dodgson, T.; Pulpitel, T.J.; Senior, A.M.; Raubenheimer, D.; Macia, L.; Simpson, S.J. Determining the Metabolic Effects of Dietary Fat, Sugars and Fat-Sugar Interaction Using Nutritional Geometry in a Dietary Challenge Study with Male Mice. Nat. Commun. 2023, 14, 4409. [Google Scholar] [CrossRef]
- Hall, K.D.; Kahan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Mann, T.; Tomiyama, A.J.; Westling, E.; Lew, A.M.; Samuels, B.; Chatman, J. Medicare’s search for effective obesity treatments: Diets are not the answer. Am. Psychol. 2007, 62, 220–233. [Google Scholar] [CrossRef]
- National Institutes of Health, Office of Dietary Supplements. Background Information: Dietary Supplements; National Institutes of Health, Office of Dietary Supplements: Bethesda, MD, USA, 2011. Available online: https://ods.od.nih.gov/factsheets/DietarySupplements-HealthProfessional/ (accessed on 7 January 2024).
- Batsis, J.A.; Apolzan, J.W.; Bagley, P.J.; Blunt, H.B.; Divan, V.; Gill, S.; Golden, A.; Gundumraj, S.; Heymsfield, S.B.; Kahan, S.; et al. A Systematic Review of Dietary Supplements and Alternative Therapies for Weight Loss. Obesity 2021, 29, 1102–1113. [Google Scholar] [CrossRef]
- Koh, Y.S.; Asharani, P.V.; Devi, F.; Roystonn, K.; Wang, P.; Vaingankar, J.A.; Abdin, E.; Sum, C.F.; Lee, E.S.; Müller-Riemenschneider, F.; et al. A Cross-Sectional Study on the Perceived Barriers to Physical Activity and Their Associations with Domain-Specific Physical Activity and Sedentary Behaviour. BMC Public Health 2022, 22, 1051. [Google Scholar] [CrossRef]
- MacInnis, M.J.; Gibala, M.J. Physiological Adaptations to Interval Training and the Role of Exercise Intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef]
- DiPietro, L.; Dziura, J.; Yeckel, C.W.; Neufer, P.D. Exercise and Improved Insulin Sensitivity in Older Women: Evidence of the Enduring Benefits of Higher Intensity Training. J. Appl. Physiol. 2006, 100, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Whyte, L.J.; Gill, J.M.R.; Cathcart, A.J. Effect of 2 Weeks of Sprint Interval Training on Health-Related Outcomes in Sedentary Overweight/Obese Men. Metabolism 2010, 59, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Amundsen, B.H.; Rognmo, Ø.; Hatlen-Rebhan, G.; Slørdahl, S.A. High-Intensity Aerobic Exercise Improves Diastolic Function in Coronary Artery Disease. Scand. Cardiovasc. J. 2008, 42, 110–117. [Google Scholar] [CrossRef]
- Hall, B.; Żebrowska, A.; Sikora, M.; Siatkowski, S.; Robins, A. The Effect of High-Intensity Interval Exercise on Short-Term Glycaemic Control, Serum Level of Key Mediator in Hypoxia and Pro-Inflammatory Cytokines in Patients with Type 1 Diabetes-An Exploratory Case Study. Nutrients 2023, 15, 3749. [Google Scholar] [CrossRef] [PubMed]
- Bacon, A.P.; Carter, R.E.; Ogle, E.A.; Joyner, M.J. VO2max Trainability and High Intensity Interval Training in Humans: A Meta-Analysis. PLoS ONE 2013, 8, e73182. [Google Scholar] [CrossRef] [PubMed]
- Milanović, Z.; Sporiš, G.; Weston, M. Effectiveness of High-Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta-Analysis of Controlled Trials. Sports Med. 2015, 45, 1469–1481. [Google Scholar] [CrossRef] [PubMed]
- Wewege, M.; van den Berg, R.; Ward, R.E.; Keech, A. The Effects of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Body Composition in Overweight and Obese Adults: A Systematic Review and Meta-Analysis. Obes. Rev. 2017, 18, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, B.J.; Tucker, W.J.; Bhammar, D.M.; Ryder, J.R.; Sweazea, K.L.; Gaesser, G.A. Effects of High-Intensity Interval Training and Moderate-Intensity Continuous Training on Endothelial Function and Cardiometabolic Risk Markers in Obese Adults. J. Appl. Physiol. 2016, 121, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Colpitts, B.H.; Rioux, B.V.; Eadie, A.L.; Brunt, K.R.; Sénéchal, M. Irisin response to acute moderate intensity exercise and high intensity interval training in youth of different obesity statuses: A randomized crossover trial. Physiol. Rep. 2022, 10, e15198. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological Quality (Risk of Bias) Assessment Tools for Primary and Secondary Medical Studies: What Are They and Which Is Better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Dunn, S.L.; Siu, W.; Freund, J.; Boutcher, S.H. The Effect of a Lifestyle Intervention on Metabolic Health in Young Women. Diabetes Metab. Syndr. Obes. 2014, 7, 437–444. [Google Scholar] [CrossRef]
- Nayebifar, S.; Afzalpour, M.E.; Kazemi, T.; Eivary, S.H.A.; Mogharnasi, M. The Effect of a 10-Week High-Intensity Interval Training and Ginger Consumption on Inflammatory Indices Contributing to Atherosclerosis in Overweight Women. J. Res. Med. Sci. 2016, 21, 116. [Google Scholar] [CrossRef]
- Afzalpour, M.E.; Ghasemi, E.; Zarban, A. Effects of 10 Weeks of High Intensity Interval Training and Green Tea Supplementation on Serum Levels of Sirtuin-1 and Peroxisome Proliferator-Activated Receptor Gamma Co-Activator 1-Alpha in Overweight Women. Sci. Sports 2017, 32, 82–90. [Google Scholar] [CrossRef]
- Lithgow, H.M.; Florida-James, G.; Leggate, M. The Combined Effect of High-intensity Intermittent Training and Vitamin D Supplementation on Glycemic Control in Overweight and Obese Adults. Physiol. Rep. 2018, 6, e13684. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, E.; Nayebifar, S. Benefits of 10 Weeks of High-Intensity Interval Training and Green Tea Supplementation on Cardiovascular Risk Factors and VO2max in Overweight Women. J. Res. Med. Sci. 2019, 24, 79. [Google Scholar] [CrossRef] [PubMed]
- Saghebjoo, M.; Farrokhi-Fard, M.; Hedayati, M.; Sadeghi-Tabas, S. The Effect of High-Intensity Interval Training and L-Arginine Supplementation on the Serum Levels of Adiponectin and Lipid Profile in Overweight and Obese Young Men. Obes. Med. 2019, 16, 100139. [Google Scholar] [CrossRef]
- Ghasemi, E.; Afzalpour, M.E.; Nayebifar, S. Combined High-Intensity Interval Training and Green Tea Supplementation Enhance Metabolic and Antioxidant Status in Response to Acute Exercise in Overweight Women. J. Physiol. Sci. 2020, 70, 31. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, K.R.; Greenwalt, C.E.; Saylor, H.E.; Gould, L.M.; Harrison, C.H.; Brewer, G.J.; Blue, M.N.M.; Ferrando, A.A.; Huffman, K.M.; Mayer-Davis, E.J.; et al. High-Intensity Interval Training and Essential Amino Acid Supplementation: Effects on Muscle Characteristics and Whole-Body Protein Turnover. Physiol. Rep. 2021, 9, e14655. [Google Scholar] [CrossRef] [PubMed]
- Nobari, H.; Gandomani, E.E.; Reisi, J.; Vahabidelshad, R.; Suzuki, K.; Volpe, S.L.; Pérez-Gómez, J. Effects of 8 Weeks of High-Intensity Interval Training and Spirulina Supplementation on Immunoglobin Levels, Cardio-Respiratory Fitness, and Body Composition of Overweight and Obese Women. Biology 2022, 11, 196. [Google Scholar] [CrossRef]
- Sheikholeslami-Vatani, D.; Rostamzadeh, N. Changes in Appetite-Dependent Hormones and Body Composition After 8 Weeks of High-Intensity Interval Training and Vitamin D Supplementation in Sedentary Overweight Men. Front. Nutr. 2022, 9, 827630. [Google Scholar] [CrossRef]
- Saeidi, A.; Nouri-Habashi, A.; Razi, O.; Ataeinosrat, A.; Rahmani, H.; Mollabashi, S.S.; Bagherzadeh-Rahmani, B.; Aghdam, S.M.; Khalajzadeh, L.; Al Kiyumi, M.H.; et al. Astaxanthin Supplemented with High-Intensity Functional Training Decreases Adipokines Levels and Cardiovascular Risk Factors in Men with Obesity. Nutrients 2023, 15, 286. [Google Scholar] [CrossRef]
- Saeidi, A.; Saei, M.A.; Mohammadi, B.; Zarei, H.R.A.; Vafaei, M.; Mohammadi, A.S.; Barati, M.; Montazer, M.; Razi, O.; Kiyumi, M.H.A.; et al. Supplementation with Spinach-Derived Thylakoid Augments the Benefits of High Intensity Training on Adipokines, Insulin Resistance and Lipid Profiles in Males with Obesity. Front. Endocrinol. 2023, 14, 1141796. [Google Scholar] [CrossRef]
- Youssef, L.; Durand, S.; Aprahamian, F.; Lefevre, D.; Bourgin, M.; Maiuri, M.C.; Dulac, M.; Hajj-Boutros, G.; Marcangeli, V.; Buckinx, F.; et al. Serum metabolomic adaptations following a 12-week high-intensity interval training combined to citrulline supplementation in obese older adults. Eur. J. Sport Sci. 2023, 23, 2157–2169. [Google Scholar] [CrossRef] [PubMed]
- Haizlip, K.M.; Harrison, B.C.; Leinwand, L.A. Sex-Based Differences in Skeletal Muscle Kinetics and Fiber-Type Composition. Physiology 2015, 30, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Fasshauer, M.; Blüher, M. Adipokines in Health and Disease. Trends Pharmacol. Sci. 2015, 36, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Sierawska, O.; Niedźwiedzka-Rystwej, P. Adipokines as Potential Biomarkers for Type 2 Diabetes Mellitus in Cats. Front. Immunol. 2022, 13, 950049. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Beltrán-Velasco, A.I.; Martín-Rodríguez, A.; Martínez-Guardado, I.; Navarro-Jiménez, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Role of Adipokines in Health and Disease. Biomedicines 2023, 11, 1290. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Hassan-Zadeh, V. IL-6 Signalling Pathways and the Development of Type 2 Diabetes. Inflammopharmacology 2018, 26, 685–698. [Google Scholar] [CrossRef] [PubMed]
- Pessin, J.E.; Saltiel, A.R. Signaling Pathways in Insulin Action: Molecular Targets of Insulin Resistance. J. Clin. Investig. 2000, 106, 165–169. [Google Scholar] [CrossRef]
- Kwon, H.; Pessin, J.E. Adipokines Mediate Inflammation and Insulin Resistance. Front. Endocrinol. 2013, 4, 71. [Google Scholar] [CrossRef]
- Reaven, G.M. Compensatory Hyperinsulinemia and the Development of an Atherogenic Lipoprotein Profile: The Price Paid to Maintain Glucose Homeostasis in Insulin-Resistant Individuals. Endocrinol. Metab. Clin. N. Am. 2005, 34, 49–62. [Google Scholar] [CrossRef]
- Henry, S.L.; Bensley, J.G.; Wood-Bradley, R.J.; Cullen-McEwen, L.A.; Bertram, J.F.; Armitage, J.A. White Adipocytes: More than Just Fat Depots. Int. J. Biochem. Cell Biol. 2012, 44, 435–440. [Google Scholar] [CrossRef]
- Grases-Pintó, B.; Abril-Gil, M.; Castell, M.; Rodríguez-Lagunas, M.J.; Burleigh, S.; Fåk Hållenius, F.; Prykhodko, O.; Pérez-Cano, F.J.; Franch, À. Influence of Leptin and Adiponectin Supplementation on Intraepithelial Lymphocyte and Microbiota Composition in Suckling Rats. Front. Immunol. 2019, 10, 2369. [Google Scholar] [CrossRef]
- Friedman, J.M. Leptin and the Endocrine Control of Energy Balance. Nat. Metab. 2019, 1, 754–764. [Google Scholar] [CrossRef]
- Feito, Y.; Burrows, E.K.; Tabb, L.P. A 4-Year Analysis of the Incidence of Injuries Among CrossFit-Trained Participants. Orthop. J. Sports Med. 2018, 6, 2325967118803100. [Google Scholar] [CrossRef]
- McPherron, A.C.; Lawler, A.M.; Lee, S.J. Regulation of Skeletal Muscle Mass in Mice by a New TGF-Beta Superfamily Member. Nature 1997, 387, 83–90. [Google Scholar] [CrossRef]
- Schuelke, M.; Wagner, K.R.; Stolz, L.E.; Hubner, C.; Riebel, T.; Komen, W.; Braun, T.; Tobin, J.F.; Lee, S.J. Myostatin mutation associated with gross muscle hypertrophy in a child. N. Engl. J. Med. 2004, 350, 2682–2688. [Google Scholar] [CrossRef] [PubMed]
- Seldin, M.M.; Tan, S.Y.; Wong, G.W. Metabolic Function of the CTRP Family of Hormones. Rev. Endocr. Metab. Disord. 2014, 15, 111–123. [Google Scholar] [CrossRef]
- Guo, T.; Jou, W.; Chanturiya, T.; Portas, J.; Gavrilova, O.; McPherron, A.C. Myostatin Inhibition in Muscle, but Not Adipose Tissue, Decreases Fat Mass and Improves Insulin Sensitivity. PLoS ONE 2009, 4, e4937. [Google Scholar] [CrossRef]
- Pietiläinen, K.H.; Kaprio, J.; Borg, P.; Plasqui, G.; Yki-Järvinen, H.; Kujala, U.M.; Rose, R.J.; Westerterp, K.R.; Rissanen, A. Physical Inactivity and Obesity: A Vicious Circle. Obesity 2008, 16, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Setty, P.; Padmanabha, B.; Doddamani, B. Correlation between Obesity and Cardio Respiratory Fitness. Int. J. Med. Sci. Public Health 2013, 2, 298–302. [Google Scholar] [CrossRef]
- Cantó, C.; Auwerx, J. PGC-1alpha, SIRT1 and AMPK, an energy sensing network that controls energy expenditure. Curr. Opin. Lipidol. 2009, 20, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Rech, C.C.; de Camargo, E.M.; de Paula Almeida, M.; dos Santos Bronoski, R.; Okuno, N.M.; Reis, R.S. Barriers for physical activity in overweight adults. Rev. Bras. Atividade Fís. Saúde 2016, 21, 272–279. [Google Scholar] [CrossRef]
- Ambati, R.R.; Siew Moi, P.; Ravi, S.; Aswathanarayana, R.G. Astaxanthin: Sources, Extraction, Stability, Biological Activities and Its Commercial Applications—A Review. Mar. Drugs 2014, 12, 128–152. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, M.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).