Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review
Abstract
1. Introduction
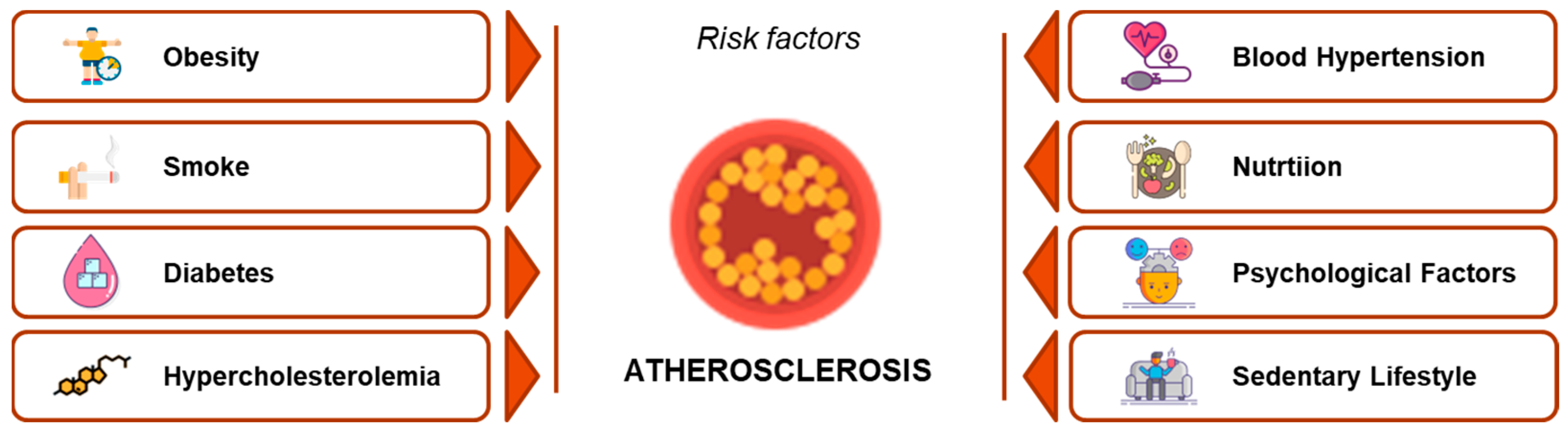
2. Cardiovascular Risk in Developmental Age
3. Long-Chain Polyunsaturated Fatty Acids (LCPUFAs)
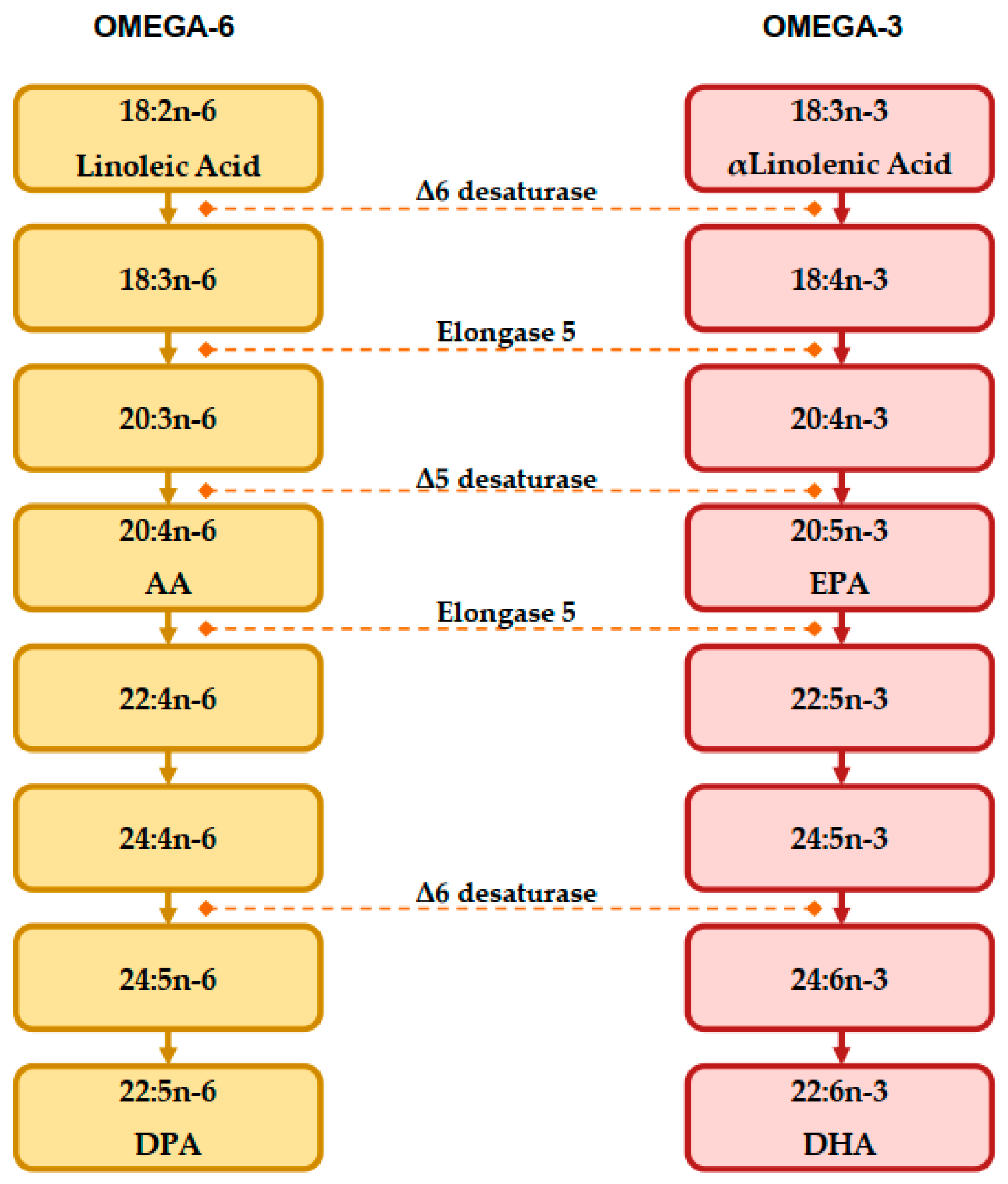
3.1. Omega-3 and Omega-6 Series
3.2. Nutritional Sources of LCPUFAs
3.3. LCPUFAs in Pregnancy and Lactation
4. Long-Chain Polyunsaturated Fatty Acids (LCPUFAs) in Cardiovascular Prevention in Adult Population
5. Long-Chain Polyunsaturated Fatty Acids (LCPUFAs) in Cardiovascular Prevention in the Pediatric Population
5.1. Non-Alcoholic Fatty Liver Disease
5.2. Hypercholesterolemia
5.3. Hypertriglyceridemia
5.4. Blood Pressure
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AA | Arachidonic Acid |
| ALA | Alfa-Linolenic Acid |
| ALT | Alanine AminoTransferase |
| Apo-B | Apolipoprotein B |
| ASCVD | Atherosclerotic Cardiovascular Disease |
| AST | Aspartate AminoTransferase |
| BMI | Body Mass Index |
| CHD | Coronary Heart Disease |
| DHA | DocosaHexaenoic Acid |
| DNA | DesoxyriboNucleic Acid |
| DPA | DocosaPentaenoic Acid |
| EPA | EicosaPentaenoic Acid |
| ESPGHAN | European Society for Paediatric Gastroenterology Hepatology and Nutrition |
| FA | Fatty Acid |
| FH | Familial Hypercholesterolemia |
| GGT | Gamma-Glutamyl Transpeptidase |
| HOMA.IR | Homestasis Model Assessment Insulin Resistance |
| HDL | High-Density Lipoprotein |
| HDL-C | High-Density Lipoprotein-Cholesterol |
| HSC | Hepatic Stellate Cells |
| IDF | International Diabetes Federation |
| IDL-1 | Intermediate Density Lipoprotein 1 |
| IDL-2 | Intermediate Density Lipoprotein 2 |
| LA | Linoleic Acid |
| LCPUFAs | Long-Chain Polyunsaturated Fatty Acids |
| LDL | Low-Density Lipoproteins |
| LDL-C | Low-Density Lipoproteins-Cholesterol |
| MAFLD | Metabolic dysfunction-Associated Fatty Liver Disease |
| miRNA | micro RiboNucleic Acid |
| MRI | Magnetic Resonance Imaging |
| NAFL | Non-Alcoholic Fatty Liver |
| NAFLD | Non-Alcoholic Fatty Liver Disease |
| NASH | Non-Alcoholic SteatoHepatitis |
| NASPGHAN | North American Society for Pediatric Gastroenterology, Hepatology and Nutrition |
| PGs | ProstaGlandins |
| PGI | Prostacyclin |
| PPAR | Peroxisome Proliferator-Activated Receptor |
| PUFAs | PolyUnsaturated Fatty Acids |
| TAG | Triacylglyceride |
| TC | Total Cholesterol |
| TONIC | Treatment Of Nonalcoholic fatty liver disease In Children |
| TX | ThromboXane |
| UDCA | UrsoDeoxyCholic Acid |
| VLDL | Very Low Density Lipoprotein |
References
- Authors/Task Force Members; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis 2019, 290, 140–205. [Google Scholar] [CrossRef]
- Agostoni, C. Docosahexaenoic acid (DHA): From the maternal–foetal dyad to the complementary feeding period. Early Hum. Dev. 2010, 86, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Bairey Merz, C.N.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation 2014, 129, S1–S45. [Google Scholar] [CrossRef]
- Napoli, C.; D’Armiento, F.P.; Mancini, F.P.; Postiglione, A.; Witztum, J.L.; Palumbo, G.; Palinski, W. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J. Clin. Investig. 1997, 100, 2680–2690. [Google Scholar] [CrossRef] [PubMed]
- Napoli, C.; Glass, C.K.; Witztum, J.L.; Deutsch, R.; D’Armiento, F.P.; Palinski, W. Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: Fate of Early Lesions in Children (FELIC) study. Lancet 1999, 354, 1234–1241. [Google Scholar] [CrossRef]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. S5), S213–S256. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar]
- Capra, M.; Pederiva, C.; Viggiano, C.; De Santis, R.; Banderali, G.; Biasucci, G. Nutritional Approach to Prevention and Treatment of Cardiovascular Disease in Childhood. Nutrients 2021, 13, 2359. [Google Scholar] [CrossRef]
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ose, L.; Averna, M.; Boileau, C.; Borén, J.; et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur. Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol. Nutr. Food Res. 2008, 52, 885–897. [Google Scholar] [CrossRef]
- Hughes, C.L.; Dhiman, T.R.; Burdock, R.P.; Crawford, J.W.; Venturelli, B.C.; Júnior, J.E.D.F.; Takiya, C.S.; de Araújo, A.P.C.; Santos, M.C.B.; Calomeni, G.D.; et al. Dietary Compounds in Relation to Dietary Diversity and Human Health. J. Med. Food 2002, 5, 51–68. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.; Wall, R.; Fitzgerald, G.F.; Ross, R.; Stanton, C. Health Implications of High Dietary Omega-6 Polyunsaturated Fatty Acids. J. Nutr. Metab. 2012, 2012, 539426. [Google Scholar] [CrossRef] [PubMed]
- Das, U.N. Essential Fatty Acids—Biochemistry, Physiology and Clinical Significance. In Molecular Basis of Health and Disease, 1st ed.; Das, U., Ed.; Springer: Dordrecht, The Netherlands, 2011; pp. 101–151. [Google Scholar]
- Richter, C.K.; Bowen, K.; Mozaffarian, D.; Kris-Etherton, P.M.; Skulas-Ray, A.C. Total Long-Chain n-3 Fatty Acid Intake and Food Sources in the United States Compared to Recommended Intakes: NHANES 2003–2008. Lipids 2017, 52, 917–927. [Google Scholar] [CrossRef]
- Nakamura, M.; Nara, T. Essential fatty acid synthesis and its regulation in mammals. Prostaglandins Leukot. Essent. Fat. Acids 2003, 68, 145–150. [Google Scholar] [CrossRef]
- Shahidi, F.; Ambigaipalan, P. Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu. Rev. Food Sci. Technol. 2018, 9, 345–381. [Google Scholar] [CrossRef]
- Couëdelo, L.; Amara, S.; Lecomte, M.; Meugnier, E.; Monteil, J.; Fonseca, L.; Pineau, G.; Cansell, M.; Carrière, F.; Michalski, M.C.; et al. Impact of various emulsifiers on ALA bioavailability and chylomicron synthesis through changes in gastrointestinal lipolysis. Food Funct. 2015, 6, 1726–1735. [Google Scholar] [CrossRef]
- Burdge, G.C.; Wootton, S.A. Conversion of α-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br. J. Nutr. 2002, 88, 411–420. [Google Scholar] [CrossRef]
- Abedi, E.; Sahari, M.A. Long-chain polyunsaturated fatty acid sources and evaluation of their nutritional and functional properties. Food Sci. Nutr. 2014, 2, 443–463. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Stapleton, R.D. Parenteral and Enteral Nutrition with Omega-3 Fatty Acids. In Diet and Nutrition in Critical Care, 1st ed.; Rajendram, R., Preedy, V.R., Patel, V.B., Eds.; Springer: New York, NY, USA, 2015; Volume 2, pp. 1695–1710. [Google Scholar]
- Linseisen, J.A.; Welch, A.; Ocké, M.; Amiano, P.; Agnoli, C.; Ferrari, P.; Sonestedt, E.; Chajès, V.; Bueno-De-Mesquita, H.B.; Kaaks, R.; et al. Dietary fat intake in the European Prospective Investigation into Cancer and Nutrition: Results from the 24-h dietary recalls. Eur. J. Clin. Nutr. 2009, 63, S61–S80. [Google Scholar] [CrossRef]
- Eaton, S.B.; Konner, M.J.; Cordain, L. Diet-dependent acid load, Paleolithic nutrition, and evolutionary health promotion. Am. J. Clin. Nutr. 2010, 91, 295–297. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. n−3 fatty acids and human health: Defining strategies for public policy. Lipids 2001, 36, S83–S89. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. Evolutionary Aspects of Diet: The Omega-6/Omega-3 Ratio and the Brain. Mol. Neurobiol. 2011, 44, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.J.; Miles, E.A.; Burdge, G.C.; Yaqoob, P.; Calder, P.C. Metabolism and functional effects of plant-derived omega-3 fatty acids in humans. Prog. Lipid Res. 2016, 64, 30–56. [Google Scholar] [CrossRef]
- Burdge, G.C.; Calder, P.C. Conversion of α-linolenic acid to longer-chain polyunsaturated fatty acids in human adults. Reprod. Nutr. Dev. 2005, 45, 581–597. [Google Scholar] [CrossRef]
- Spector, A.A.; Kim, H.-Y. Discovery of essential fatty acids. J. Lipid Res. 2015, 56, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, F.; Ambigaipalan, P. Novel functional food ingredients from marine sources. Curr. Opin. Food Sci. 2015, 2, 123–129. [Google Scholar] [CrossRef]
- Shahidi, F.; Ambigaipalan, P. Beverages fortified with omega 3 fatty acids, dietary fiber, minerals and vitamins. In Handbook of Functional Beverages and Human Health; Shahidi, F., Alsalvar, C., Eds.; CRC Press: Boca Raton, FL, USA, 2016; pp. 801–813. [Google Scholar]
- Shahidi, F.; Miraliakbari, H. Omega-3 (n-3) Fatty Acids in Health and Disease: Part 1—Cardiovascular Disease and Cancer. J. Med. Food 2004, 7, 387–401. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. Fats and fatty acids in human nutrition. Report of an expert consultation. FAO Food Nutr. Pap. 2010, 91, 1–166. [Google Scholar]
- Pérez-Gálveza, A.; Garrido-Fernándeza, J.; Mínguez-Mosqueraa, M.I.; Lozano-Ruizb, M.; Montero-de-Espinosab, V. Fatty acid composition of two new pepper varieties (Capsicum annuum L. cv. Jaranda and Jariza). Effect of drying process and nutritional aspects. J. Am. Oil Chem. Soc. 1999, 76, 205–208. [Google Scholar]
- Yang, J.; Zhou, C.; Yuan, G.; Li, D. Effects of Geographical Origin on the Conjugated Linolenic Acid of Trichosanthes kirilowii Maxim Seed Oil. J. Am. Oil Chem. Soc. 2012, 89, 401–407. [Google Scholar] [CrossRef]
- Jin, F.; Nieman, D.C.; Sha, W.; Xie, G.; Qiu, Y.; Jia, W. Supplementation of Milled Chia Seeds Increases Plasma ALA and EPA in Postmenopausal Women. Plant Foods Hum. Nutr. 2012, 67, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.L.; Martínez, F.P.; Ferreira, S.B.; Kaiser, C.R. A complete evaluation of thermal and oxidative stability of chia oil. J. Therm. Anal. Calorim. 2017, 130, 1307–1315. [Google Scholar] [CrossRef]
- Linee Guida per Una Sana Alimentazione Revisione 2018. ISBN 9788833850375. Available online: https://www.Crea.Gov.It/En/Web/Alimenti-e-Nutrizione/-/Linee-Guida-per-Una-Sana-Alimentazione-2018 (accessed on 28 February 2023).
- Ledger, H.P. Body composition as a basis for a comparative study of some East African animals. Symp. Zool Soc. Lond. 1968, 21, 289–310. [Google Scholar]
- Eaton, S., 3rd; Iii, S.E.; Sinclair, A.; Cordain, L.; Mann, N.J. Dietary Intake of Long-Chain Polyunsaturated Fatty Acids during the Paleolithic. World Rev. Nutr. Diet. 1998, 83, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 2002, 56, 365–379. [Google Scholar] [CrossRef]
- Mori, T.A. Marine OMEGA-3 fatty acids in the prevention of cardiovascular disease. Fitoterapia 2017, 123, 51–58. [Google Scholar] [CrossRef]
- Fialkow, J. Omega-3 Fatty Acid Formulations in Cardiovascular Disease: Dietary Supplements are Not Substitutes for Prescription Products. Am. J. Cardiovasc. Drugs 2016, 16, 229–239. [Google Scholar] [CrossRef]
- Monroig, Ó.; Tocher, D.R.; Navarro, J.C. Biosynthesis of Polyunsaturated Fatty Acids in Marine Invertebrates: Recent Advances in Molecular Mechanisms. Mar. Drugs 2013, 11, 3998–4018. [Google Scholar] [CrossRef]
- Senanayake, S.P.J.N.; Fichtali, J. Marine oils: Single cell oil as a sources of nutraceuticals and speciality lipids: Processing technologies and application. In Nutraceutical and Speciality Lipids and Their Co-Products; Shahidi, F., Ed.; CRC Press: Boca Raton, FL, USA, 2006; pp. 251–280. [Google Scholar]
- Copeman, L.A.; Parrish, C.C. Lipids Classes, Fatty Acids, and Sterols in Seafood from Gilbert Bay, Southern Labrador. J. Agric. Food Chem. 2004, 52, 4872–4881. [Google Scholar] [CrossRef]
- Budge, S.M.; Iverson, S.J.; Bowen, W.D.; Ackman, R.G. Among- and within-species variability in fatty acid signatures of marine fish and invertebrates on the Scotian Shelf, Georges Bank, and southern Gulf of St. Lawrence. Can. J. Fish. Aquat. Sci. 2002, 59, 886–898. [Google Scholar] [CrossRef]
- Aursand, M.; Bleivik, B.; Rainuzzo, J.R.; Leif, J.; Mohr, V. Lipid distribution and composition of commercially farmed Atlantic salmon (Salmo salar). J. Sci. Food Agric. 1994, 64, 239–248. [Google Scholar] [CrossRef]
- Schuchardt, J.P.; Hahn, A. Bioavailability of long-chain omega-3 fatty acids. Prostaglandins Leukot. Essent. Fat. Acids 2013, 89, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Maki, K.C.; Johns, C.; Harris, W.S.; Puder, M.; Freedman, S.D.; Thorsteinsson, T.; Daak, A.; Rabinowicz, A.L.; Sancilio, F.D. Bioequivalence Demonstration for Ω-3 Acid Ethyl Ester Formulations: Rationale for Modification of Current Guidance. Clin. Ther. 2017, 39, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Rodríguez, N.; Beltrán, S.; Jaime, I.; de Diego, S.M.; Sanz, M.T.; Carballido, J.R. Production of omega-3 polyunsaturated fatty acid concentrates: A review. Innov. Food Sci. Emerg. Technol. 2010, 11, 1–12. [Google Scholar] [CrossRef]
- SINU, Società Italiana di Nutrizione Umana. LARN—Livelli di Assunzione di Riferimento di Nutrienti ed Energia per la Popolazione Italiana; IV Revisione; Coordinamento Editoriale SINU-INRAN; SICS: Milan, Italy, 2014. [Google Scholar]
- Puri, R.; Mahajan, M.; Sahajpal, N.S.; Singh, H.; Singh, H.; Jain, S.K. Self-nanoemulsifying drug delivery system of docosahexanoic acid: Development, in vitro, in vivo characterization. Drug Dev. Ind. Pharm. 2016, 42, 1032–1041. [Google Scholar] [CrossRef]
- Jensen, R.G. The lipids in human milk. Prog. Lipid Res. 1996, 35, 53–92. [Google Scholar] [CrossRef] [PubMed]
- Marangoni, F.; Agostoni, C.; Lammardo, A.M.; Giovannini, M.; Galli, C.; Riva, E. Polyunsaturated fatty acid concentrations in human hindmilk are stable throughout 12-months of lactation and provide a sustained intake to the infant during exclusive breast-feeding: An Italian study. Br. J. Nutr. 2000, 84, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Farquharson, J.; Cockburn, F.A.; Patrick, W.; Jamieson, E.C.; Logan, R.W. Infant cerebral cortex phospholipid fatty-acid composition and diet. Lancet 1992, 340, 810–813. [Google Scholar] [CrossRef]
- Makrides, M.; Neumann, M.; Byard, R.; Simmer, K.; Gibson, R. Fatty acid composition of brain, retina, and erythrocytes in breast- and formula-fed infants. Am. J. Clin. Nutr. 1994, 60, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Innis, S.M. Polyunsaturated fatty acids in human milk: An essential role in infant development. Adv. Exp. Med. Biol. 2004, 554, 27–43. [Google Scholar] [CrossRef]
- Reynolds, A. Breastfeeding and Brain Development. Pediatr. Clin. N. Am. 2001, 48, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Decsi, T. Effects of supplementing LCPUFA to the diet of pregnant women: Data from RCT. Adv. Exp. Med. Biol. 2009, 646, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.F.; Østerdal, M.L.; Salvig, J.D.; Mortensen, L.M.; Rytter, D.; Secher, N.J.; Henriksen, T.B. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am. J. Clin. Nutr. 2008, 88, 167–175. [Google Scholar] [CrossRef]
- Dunstan, J.A.; Simmer, K.; Dixon, G.; Prescott, S.L. Cognitive assessment of children at age 2½ years after maternal fish oil supplementation in pregnancy: A randomised controlled trial. Arch. Dis. Child.-Fetal Neonatal Ed. 2008, 93, F45–F50. [Google Scholar] [CrossRef]
- Helland, I.B.; Smith, L.; Saarem, K.; Saugstad, O.D.; Drevon, C.A. Maternal Supplementation with Very-Long-Chain n-3 Fatty Acids during Pregnancy and Lactation Augments Children’s IQ at 4 Years of Age. Pediatrics 2003, 111, e39–e44. [Google Scholar] [CrossRef]
- Helland, I.B.; Smith, L.; Blomén, B.; Saarem, K.; Saugstad, O.D.; Drevon, C.A. Effect of Supplementing Pregnant and Lactating Mothers with n-3 Very-Long-Chain Fatty Acids on Children’s IQ and Body Mass Index at 7 Years of Age. Pediatrics 2008, 122, e472–e479. [Google Scholar] [CrossRef] [PubMed]
- Innis, S.M.; Friesen, R.W. Essential n−3 fatty acids in pregnant women and early visual acuity maturation in term infants. Am. J. Clin. Nutr. 2008, 87, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Malcolm, C.A.; McCulloch, D.L.; Montgomery, C.; Shepherd, A.; Weaver, L.T. Maternal docosahexaenoic acid supplementation during pregnancy and visual evoked potential development in term infants: A double blind, prospective, randomised trial. Arch. Dis. Child.-Fetal Neonatal Ed. 2003, 88, 383–390. [Google Scholar] [CrossRef]
- Martinez, M. Tissue levels of polyunsaturated fatty acids during early human development. J. Pediatr. 1992, 120, S129–S138. [Google Scholar] [CrossRef]
- Burr, M.L.; Fehily, A.M.; Gilbert, J.F.; Rogers, S.; Holliday, R.M.; Sweetnam, P.M.; Elwood, P.C.; Deadman, N.M. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet and reinfarction trial (DART). Lancet 1989, 334, 757–761. [Google Scholar] [CrossRef]
- Yokoyama, M.; Origasa, H.; Matsuzaki, M.; Matsuzawa, Y.; Saito, Y.; Ishikawa, Y.; Oikawa, S.; Sasaki, J.; Hishida, H.; Itakura, H.; et al. Effects of eicosapentaenoic acid on major coronary events in hy-percholesterolaemic patients (JELIS): A randomised open-label, blinded endpoint analysis. Lancet 2007, 369, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- GISSI-Prevenzione Investigators (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico). Dietary supplementation with n-3 polyunsatured fatty acids and vitamin E after myocardial infarcion: Results of the GISSI-Prevenzione trial. Lancet 1999, 354, 447–455. [Google Scholar] [CrossRef]
- Ballantyne, C.M.; Bays, H.E.; Kastelein, J.J.; Stein, E.; Isaacsohn, J.L.; Braeckman, R.A.; Soni, P.N. Efficacy and Safety of Eicosapentaenoic Acid Ethyl Ester (AMR101) Therapy in Statin-Treated Patients with Persistent High Triglycerides (from the ANCHOR Study). Am. J. Cardiol. 2012, 110, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Bays, H.E.; Ballantyne, C.M.; Kastelein, J.J.; Isaacsohn, J.L.; Braeckman, R.A.; Soni, P.N. Eicosapentaenoic Acid Ethyl Ester (AMR101) Therapy in Patients With Very High Triglyceride Levels (from the Multi-center, plAcebo-controlled, Randomized, double-blINd, 12-week study with an open-label Extension [MARINE] Trial). Am. J. Cardiol. 2011, 108, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Kastelein, J.J.; Maki, K.C.; Susekov, A.; Ezhov, M.; Nordestgaard, B.G.; Machielse, B.N.; Kling, D.; Davidson, M.H. Omega-3 free fatty acids for the treatment of severe hypertriglyceridemia: The EpanoVa fOr Lowering Very high triglyceridEs (EVOLVE) trial. J. Clin. Lipidol. 2014, 8, 94–106. [Google Scholar] [CrossRef] [PubMed]
- The Look AHEAD Research Group; Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; et al. Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes. N. Engl. J. Med. 2013, 369, 145–154. [Google Scholar] [CrossRef]
- Budoff, M.J.; Bhatt, D.L.; Kinninger, A.; Lakshmanan, S.; Muhlestein, J.B.; Le, V.T.; May, H.T.; Shaikh, K.; Shekar, C.; Roy, S.K.; et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: Final results of the EVAPORATE trial. Eur. Heart J. 2020, 41, 3925–3932. [Google Scholar] [CrossRef]
- Nicholls, S.J.; Lincoff, A.M.; Garcia, M.; Bash, D.; Ballantyne, C.M.; Barter, P.J.; Davidson, M.H.; Kastelein, J.J.P.; Koenig, W.; McGuire, D.K.; et al. Effect of High-Dose Omega-3 Fatty Acids vs Corn Oil on Major Adverse Cardiovascular Events in Patients at High Cardiovascular Risk. JAMA 2020, 324, 2268. [Google Scholar] [CrossRef]
- Averna, M.; Banach, M.; Bruckert, E.; Drexel, H.; Farnier, M.; Gaita, D.; Magni, P.; März, W.; Masana, L.; e Silva, A.M.; et al. Practical guidance for combination lipid-modifying therapy in high- and very-high-risk patients: A statement from a European Atherosclerosis Society Task Force. Atherosclerosis 2021, 325, 99–109. [Google Scholar] [CrossRef]
- Manson, J.E.; Bassuk, S.S.; Lee, I.-M.; Cook, N.R.; Albert, M.A.; Gordon, D.; Zaharris, E.; MacFadyen, J.G.; Danielson, E.; Lin, J.; et al. The VITamin D and OmegA-3 TriaL (VITAL): Rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp. Clin. Trials 2012, 33, 159–171. [Google Scholar] [CrossRef]
- Bassuk, S.S.; Manson, J.E.; for the VITAL Research Group. Marine omega-3 fatty acid supplementation and prevention of cardiovascular disease: Update on the randomized trial evidence. Cardiovasc. Res. 2022. [Google Scholar] [CrossRef]
- Abdelhamid, A.S.; Brown, T.J.; Brainard, J.S.; Biswas, P.; Thorpe, G.C.; Moore, H.J.; Deane, K.H.; AlAbdulghafoor, F.K.; Summerbell, C.D.; Worthington, H.V.; et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2018, 7, CD003177. [Google Scholar] [CrossRef]
- De Cosmi, V.; Mazzocchi, A.; D’Oria, V.; Re, A.; Spolidoro, G.C.I.; Milani, G.P.; Berti, C.; Scaglioni, S.; Giavoli, C.; Bergamaschi, S.; et al. Effect of Vitamin D and Docosahexaenoic Acid Co-Supplementation on Vitamin D Status, Body Composition, and Metabolic Markers in Obese Children: A Randomized, Double Blind, Controlled Study. Nutrients 2022, 14, 1397. [Google Scholar] [CrossRef]
- Borasio, F.; Syren, M.-L.; Turolo, S.; Agostoni, C.; Molteni, M.; Antonietti, A.; Lorusso, M.L. Direct and Indirect Effects of Blood Levels of Omega-3 and Omega-6 Fatty Acids on Reading and Writing (Dis)Abilities. Brain Sci. 2022, 12, 169. [Google Scholar] [CrossRef]
- Demmelmair, H.; MacDonald, A.; Kotzaeridou, U.; Burgard, P.; Gonzalez-Lamuno, D.; Verduci, E.; Ersoy, M.; Gokcay, G.; Alyanak, B.; Reischl, E.; et al. Determinants of Plasma Docosahexaenoic Acid Levels and Their Relationship to Neurological and Cognitive Functions in PKU Patients: A Double Blind Randomized Supplementation Study. Nutrients 2018, 10, 1944. [Google Scholar] [CrossRef] [PubMed]
- ESPGHAN Committee on Nutrition; Agostoni, C.; Braegger, C.; Decsi, T.; Kolacek, S.; Mihatsch, W.; Moreno, L.A.; Puntis, J.; Shamir, R.; Szajewska, H.; et al. Supplementation of N-3 LCPUFA to the Diet of Children Older than 2 Years: A Commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Craniofacial Surg. 2017, 64, 319–334. [Google Scholar] [CrossRef]
- Mann, J.P.; Valenti, L.; Scorletti, E.; Byrne, C.D.; Nobili, V. Nonalcoholic Fatty Liver Disease in Children. Semin. Liver Dis. 2018, 38, 001–013. [Google Scholar] [CrossRef]
- Dietrich, P.; Hellerbrand, C. Non-alcoholic fatty liver disease, obesity and the metabolic syndrome. Best Pract. Res. Clin. Gastroenterol. 2014, 28, 637–653. [Google Scholar] [CrossRef] [PubMed]
- Zimmet, P.; Alberti, K.G.M.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennett, P.; Shaw, J.; Caprio, S.; et al. The metabolic syndrome in children and adolescents? an IDF consensus report. Pediatr. Diabetes 2007, 8, 299–306. [Google Scholar] [CrossRef]
- Pacifico, L.; Perla, F.M.; Roggini, M.; Andreoli, G.; D’Avanzo, M.; Chiesa, C. A Systematic Review of NAFLD-Associated Extrahepatic Disorders in Youths. J. Clin. Med. 2019, 8, 868. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Sanyal, A.J.; George, J.; on behalf of theInternational Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Alkhouri, N.; Vajro, P.; Baumann, U.; Weiss, R.; Socha, P.; Marcus, C.; Lee, W.S.; Kelly, D.; Porta, G.; et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: An international expert consensus statement. Lancet Gastroenterol. Hepatol. 2021, 6, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Cholongitas, E.; Pavlopoulou, I.; Papatheodoridi, M.; Markakis, G.E.; Bouras, E.; Haidich, A.B.; Papatheodoridis, G. Epidemiology of nonalcoholic fatty liver disease in Europe: A systematic review and meta-analysis. Ann. Gastroenterol. 2021, 34, 404–414. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Wu, C.-C.; Ni, Y.-H. New Perspectives on Genetic Prediction for Pediatric Metabolic Associated Fatty Liver Disease. Front. Pediatr. 2020, 8, 603654. [Google Scholar] [CrossRef]
- Smith, S.K.; Perito, E.R. Nonalcoholic Liver Disease in Children and Adolescents. Clin. Liver Dis. 2018, 22, 723–733. [Google Scholar] [CrossRef]
- Alisi, A.; Feldstein, A.E.; Villani, A.; Raponi, M.; Nobili, V. Pediatric nonalcoholic fatty liver disease: A multidisciplinary approach. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 152–161. [Google Scholar] [CrossRef]
- Shaunak, M.; Byrne, C.D.; Davis, N.; Afolabi, P.; Faust, S.; Davies, J.H. Non-alcoholic fatty liver disease and childhood obesity. Arch. Dis. Child. 2020, 106, 3–8. [Google Scholar] [CrossRef]
- Fang, Y.-L.; Chen, H.; Wang, C.-L.; Liang, L. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: From “two hit theory” to “multiple hit model”. World, J. Gastroenterol. 2018, 24, 2974–2983. [Google Scholar] [CrossRef]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Mandala, A.; Janssen, R.C.; Palle, S.; Short, K.R.; Friedman, J.E. Pediatric Non-Alcoholic Fatty Liver Disease: Nutritional Origins and Potential Molecular Mechanisms. Nutrients 2020, 12, 3166. [Google Scholar] [CrossRef] [PubMed]
- Vajro, P.; Lenta, S.; Socha, P.; Dhawan, A.; McKiernan, P.; Baumann, U.; Durmaz, O.; Lacaille, F.; McLin, V.; Nobili, V. Diagnosis of Nonalcoholic Fatty Liver Disease in Children and Adolescents: Position paper of the ESPGHAN Hepatology Committee. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 700–713. [Google Scholar] [CrossRef]
- Nobili, V.; Alisi, A.; Valenti, L.; Miele, L.; Feldstein, A.E.; Alkhouri, N. NAFLD in children: New genes, new diagnostic modalities and new drugs. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Goldner, D.; Lavine, J.E. Nonalcoholic Fatty Liver Disease in Children: Unique Considerations and Challenges. Gastroenterology 2020, 158, 1967–1983.e1. [Google Scholar] [CrossRef]
- Yang, M.; Gong, S.; Ye, S.Q.; Lyman, B.; Geng, L.; Chen, P.; Li, D.-Y. Non-Alcoholic Fatty Liver Disease in Children: Focus on Nutritional Interventions. Nutrients 2014, 6, 4691–4705. [Google Scholar] [CrossRef]
- Crudele, A.; Panera, N.; Braghini, M.R.; Balsano, C.; Alisi, A. The pharmacological treatment of nonalcoholic fatty liver disease in children. Expert Rev. Clin. Pharmacol. 2020, 13, 1219–1227. [Google Scholar] [CrossRef]
- Amatruda, M.; Ippolito, G.; Vizzuso, S.; Vizzari, G.; Banderali, G.; Verduci, E. Epigenetic Effects of n-3 LCPUFAs: A Role in Pediatric Metabolic Syndrome. Int. J. Mol. Sci. 2019, 20, 2118. [Google Scholar] [CrossRef]
- Scorletti, E.; Byrne, C.D. Omega-3 fatty acids and non-alcoholic fatty liver disease: Evidence of efficacy and mechanism of action. Mol. Asp. Med. 2018, 64, 135–146. [Google Scholar] [CrossRef]
- Nobili, V.; Bedogni, G.; Alisi, A.; Pietrobattista, A.; Risé, P.; Galli, C.; Agostoni, C. Docosahexaenoic acid supplementation decreases liver fat content in children with non-alcoholic fatty liver disease: Double-blind randomised controlled clinical trial. Arch. Dis. Child. 2011, 96, 350–353. [Google Scholar] [CrossRef]
- St-Jules, D.E.; Watters, C.A.; Brunt, E.M.; Wilkens, L.R.; Novotny, R.; Belt, P.; Lavine, J.E.; Nonalcoholic Steatohepatitis Clinical Research Network. Estimation of Fish and ω-3 Fatty Acid Intake in Pediatric Nonalcoholic Fatty Liver Disease. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Kris-Etherton, P.M.; Grieger, J.A.; Etherton, T.D. Dietary reference intakes for DHA and EPA. Prostaglandins Leukot. Essent. Fat. Acids 2009, 81, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Boyraz, M.; Pirgon, Ö.; Dündar, B.; Çekmez, F.; Hatipoğlu, N. Long-Term Treatment with n-3 Polyunsaturated Fatty Acids as a Monotherapy in Children with Nonalcoholic Fatty Liver Disease. J. Clin. Res. Pediatr. Endocrinol. 2015, 7, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Della Corte, C.; Carpino, G.; De Vito, R.; De Stefanis, C.; Alisi, A.; Cianfarani, S.; Overi, D.; Mosca, A.; Stronati, L.; Cucchiara, S.; et al. Docosahexanoic Acid Plus Vitamin D Treatment Improves Features of NAFLD in Children with Serum Vitamin D Deficiency: Results from a Single Centre Trial. PLoS ONE 2016, 11, e0168216. [Google Scholar] [CrossRef]
- Pacifico, L.; Bonci, E.; Di Martino, M.; Versacci, P.; Andreoli, G.; Silvestri, L.; Chiesa, C. A double-blind, placebo-controlled randomized trial to evaluate the efficacy of docosahexaenoic acid supplementation on hepatic fat and associated cardiovascular risk factors in overweight children with nonalcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 734–741. [Google Scholar] [CrossRef]
- Janczyk, W.; Lebensztejn, D.; Wierzbicka-Rucińska, A.; Mazur, A.; Neuhoff-Murawska, J.; Matusik, P.; Socha, P. Omega-3 Fatty Acids Therapy in Children with Nonalcoholic Fatty Liver Disease: A Randomized Controlled Trial. J. Pediatr. 2015, 166, 1358–1363.e3. [Google Scholar] [CrossRef]
- Capra, M.E.; Stanyevic, B.; Giudice, A.; Monopoli, D.; Decarolis, N.M.; Esposito, S.; Biasucci, G. The Effects of COVID-19 Pandemic and Lockdown on Pediatric Nutritional and Metabolic Diseases: A Narrative Review. Nutrients 2022, 15, 88. [Google Scholar] [CrossRef]
- Pederiva, C.; Capra, M.; Viggiano, C.; Rovelli, V.; Banderali, G.; Biasucci, G. Early Prevention of Atherosclerosis: Detection and Management of Hypercholesterolaemia in Children and Adolescents. Life 2021, 11, 345. [Google Scholar] [CrossRef]
- Engler, M.; Malloy, M.; Chiu, E.; Besio, D.; Paul, S.; Stuehlinger, M.; Morrow, J.; Ridker, P.; Rifai, N.; Mietus-Snyder, M.; et al. Docosahexaenoic acid restores endothelial function in children with hyperlipidemia: Results from the EARLY Study. Int. J. Clin. Pharmacol. Ther. 2004, 42, 672–679. [Google Scholar] [CrossRef]
- Barkas, F.; Nomikos, T.; Liberopoulos, E.; Panagiotakos, D. Diet and Cardiovascular Disease Risk Among Individuals with Familial Hypercholesterolemia: Systematic Review and Meta-Analysis. Nutrients 2020, 12, 2436. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Wu, J.H.Y. Omega-3 Fatty Acids and Cardiovascular Disease: Effects on risk factors, molecular pathways, and clinical events. J. Am. Coll. Cardiol. 2011, 58, 2047–2067. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Yu, D.; Demark-Wahnefried, W.; Franco, O.H.; Lin, X. Meta-analysis of the effects of flaxseed interventions on blood lipids. Am. J. Clin. Nutr. 2009, 90, 288–297. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Steg, P.G.; Miller, M.; Brinton, E.A.; Jacobson, T.A.; Ketchum, S.B.; Doyle, R.T., Jr.; Juliano, R.A.; Jiao, L.; Granowitz, C.; et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N. Engl. J. Med. 2019, 380, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Zhu, C.; Wang, Z.; Wang, S.; Yuan, P.; Song, T.; Hou, X.; Lei, Z. Effects of Fish Oil Supplementation on Cardiometabolic Risk Factors in Overweight or Obese Children and Adolescents: A Meta-Analysis of Randomized Controlled Trials. Front. Pediatr. 2021, 9, 604469. [Google Scholar] [CrossRef]
- Garaiova, I.; Muchová, J.; Nagyová, Z.; Mišľanová, C.; Oravec, S.; Dukát, A.; Wang, D.; Plummer, S.F.; Ďuračková, Z. Effect of a plant sterol, fish oil and B vitamin combination on cardiovascular risk factors in hypercholesterolemic children and adolescents: A pilot study. Nutr. J. 2013, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Calpe-Berdiel, L.; Escolà-Gil, J.C.; Blanco-Vaca, F. New insights into the molecular actions of plant sterols and stanols in cholesterol metabolism. Atherosclerosis 2009, 203, 18–31. [Google Scholar] [CrossRef]
- Dumont, J.; Huybrechts, I.; Spinneker, A.; Gottrand, F.; Grammatikaki, E.; Bevilacqua, N.; Vyncke, K.; Widhalm, K.; Kafatos, A.; Molnar, D.; et al. FADS1 Genetic Variability Interacts with Dietary a-Linolenic Acid Intake to Affect Serum Non-HDL–Cholesterol Concentrations in European Adolescents. J. Nutr. 2011, 141, 1247–1253. [Google Scholar] [CrossRef]
- Valaiyapathi, B.; Sunil, B.; Ashraf, A.P. Approach to Hypertriglyceridemia in the Pediatric Population. Pediatr. Rev. 2017, 38, 424–434. [Google Scholar] [CrossRef]
- Blackett, P.R.; Wilson, D.P.; McNeal, C.J. Secondary hypertriglyceridemia in children and adolescents. J. Clin. Lipidol. 2015, 9, S29–S40. [Google Scholar] [CrossRef]
- Capra, M.E.; Biasucci, G.; Banderali, G.; Pederiva, C. Nutritional Treatment of Hypertriglyceridemia in Childhood: From Healthy-Heart Counselling to Life-Saving Diet. Nutrients 2023, 15, 1088. [Google Scholar] [CrossRef]
- Benuck, I.; Wilson, D.P.; McNeal, C. Secondary Hypertriglyceridemia. 2020 Jun 1. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Shah, A.S.; Wilson, D.P. Genetic Disorders Causing Hypertriglyceridemia in Children and Adolescents. 2020 Jan 22. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Bálint, E.R.; Fűr, G.; Kiss, L.; Németh, D.I.; Soós, A.; Hegyi, P.; Szakács, Z.; Tinusz, B.; Varjú, P.; Vincze, Á.; et al. Assessment of the course of acute pancreatitis in the light of aetiology: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 17936. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.K.; Yoo, E.-G. Hypertriglyceridemia in Obese Children and Adolescents. J. Obes. Metab. Syndr. 2018, 27, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Bamba, V. Update on Screening, Etiology, and Treatment of Dyslipidemia in Children. J. Clin. Endocrinol. Metab. 2014, 99, 3093–3102. [Google Scholar] [CrossRef] [PubMed]
- Colletti, R.B.; Roff, N.K.; Neufeld, E.J.; Baker, A.L.; Newburger, J.W.; McAuliffe, T.L. Niacin Treatment of Hypercholesterolemia in Children. Pediatrics 1993, 92, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Balk, E.; Chung, M.; Lichtenstein, A.; Chew, P.; Kupelnick, B.; Lawrence, A.; DeVine, D.; Lau, J. Effects of omega-3 fatty acids on cardi-ovascular risk factors and intermediate markers of cardiovascular disease. Evid. Rep. Technol. Assess (Summ.) 2004, 93, 1–6. [Google Scholar]
- Lane, K.; Derbyshire, E.; Li, W.; Brennan, C. Bioavailability and Potential Uses of Vegetarian Sources of Omega-3 Fatty Acids: A Review of the Literature. Crit. Rev. Food Sci. Nutr. 2014, 54, 572–579. [Google Scholar] [CrossRef]
- Adkins, Y.; Kelley, D.S. Mechanisms underlying the cardioprotective effects of omega-3 polyunsaturated fatty acids. J. Nutr. Biochem. 2010, 21, 781–792. [Google Scholar] [CrossRef]
- Juárez-López, C.; Klünder-Klünder, M.; Madrigal-Azcárate, A.; Flores-Huerta, S. Omega-3 polyunsaturated fatty acids reduce insulin resistance and triglycerides in obese children and adolescents. Pediatr. Diabetes 2013, 14, 377–383. [Google Scholar] [CrossRef]
- Chahal, N.; Manlhiot, C.; Wong, H.; McCrindle, B.W. Effectiveness of Omega-3 Polysaturated Fatty Acids (Fish Oil) Supplementation for Treating Hypertriglyceridemia in Children and Adolescents. Clin. Pediatr. 2014, 53, 645–651. [Google Scholar] [CrossRef]
- de Ferranti, S.D.; Milliren, C.E.; Denhoff, E.R.; Steltz, S.K.; Tierney, E.S.S.; Feldman, H.A.; Osganian, S.K. Using High-Dose Omega-3 Fatty Acid Supplements to Lower Triglyceride Levels in 10- to 19-Year-Olds. Clin. Pediatr. 2014, 53, 428–438. [Google Scholar] [CrossRef]
- Forsyth, J.S.; Carlson, S.E. Long-chain polyunsaturated fatty acids in infant nutrition: Effects on infant development. Curr. Opin. Clin. Nutr. Metab. Care 2001, 4, 123–126. [Google Scholar] [CrossRef] [PubMed]
| Different Types of Prevention | |
|---|---|
| Primordial prevention | Aimed at preventing risk factors |
| Primary prevention | Aimed at early identification and treatment of risk factors |
| Secondary prevention | Aimed at reducing the risk of other CHD events in subjects who have already had CHD events |
| Food | G of Lipids per 100 g of Food | ALA % of Total Lipids |
|---|---|---|
| Beans, dried, raw | 2 | 33.33 |
| Lentils, dried, raw | 1 | 12.82 |
| Walnuts, dried | 68.1 | 11.89 |
| Soya oil | 99.9 | 8.01 |
| Wheat germ Oil | 99.9 | 5.72 |
| Sole, fresh | 1.4 | 5.68 |
| Trout, fresh | 3 | 3.81 |
| Lamb, lean only, raw | 8.8 | 2.62 |
| Milk, cow, partially skimmed | 1.5 | 2.11 |
| Beef, rib, lean only | 6.1 | 2.10 |
| Pecan Nuts | 71.8 | 1.88 |
| Food | G of Lipids per 100 g of Food | EPA % of Total Lipids |
|---|---|---|
| Squid, fresh | 1.7 | 18.24 |
| Sole, fresh | 1.4 | 17.86 |
| Octopus, fresh | 1 | 17.82 |
| Turkey, whole, with skin, raw | 6.9 | 13.61 |
| Sea bass, fresh | 1.5 | 8.57 |
| Salmon, fresh | 12 | 8.43 |
| Cod, deep frozen, raw | 0.6 | 6.94 |
| Trout, fresh | 3 | 5.71 |
| Beef, hind part cuts | 3.4 | 2.74 |
| Beef, in jelly, canned | 1.8 | 2.71 |
| Horse, lean only | 1 | 1.27 |
| Goat, lean only | 2.3 | 1.09 |
| Swine, light, leg | 3.2 | 1.03 |
| Food | G of Lipids per 100 g of Food | DHA % of Total Lipids |
|---|---|---|
| Cod, deep frozen, roasted in oven | 0.9 | 38.65 |
| Tuna, fresh | 8.1 | 26.54 |
| Sole, fresh | 1.4 | 25.97 |
| Trout, deep frozen | 2.3 | 22.98 |
| Octopus, fresh | 1 | 21.78 |
| Salmon, fresh | 12 | 11.27 |
| Liver, chicken, raw | 6.3 | 4.78 |
| Beef, front part cuts | 7 | 1.50 |
| Chicken egg, whole, powder | 36.4 | 0.81 |
| Type of Study | Population | Intervention | Results | Author |
|---|---|---|---|---|
| Randomized controlled trial | 60 children with NAFLD diagnosis Age 8–12 years | DHA 250 mg/day or 500 mg/day for 6 months |
| Nobili et al., 2011 [106] |
| Cross-sectional analysis | 223 children with NAFLD diagnosis 8–17 years | To evaluate fish and omega-3 fatty-acids intake and their effects on ALT and liver histological characteristics |
| St-Jules et al., 2013 [107] |
| Randomized trial | 108 obese children with NAFLD diagnosis 9–17 years | LCPUFAs 1000 mg/day for 12 months |
| Boyraz et al., 2015 [109] |
| Randomized trial | 60 children with NAFLD 4–16 years | DHA (500 mg/day) and Vitamin D (800 UI/day) for 24 weeks |
| Della Corte et al., 2016 [110] |
| Randomized trial | 51 children with NAFLD diagnosis <18 years | DHA 250 mg/day for 6 months |
| Pacifico et al., 2015 [111] |
| Randomized controlled trial | 76 overweight/obese children with NAFLD diagnosis Median age 13 | DHA and EPA 450–1300 mg/day for 6 months |
| Janczyk et al., 2015 [112] |
| Age | Normal | Borderline | High | Very High | Severe | Very Severe |
|---|---|---|---|---|---|---|
| 0–9 years | <75 | ≥75–99 | ≥100–499 | ≥500–999 | ≥1000–1999 | ≥2000 |
| 10–19 years | <90 | ≥90–129 | ≥130–499 | ≥500–999 | ≥1000–1999 | ≥2000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capra, M.E.; Stanyevic, B.; Giudice, A.; Monopoli, D.; Decarolis, N.M.; Esposito, S.; Biasucci, G. Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review. Nutrients 2023, 15, 1661. https://doi.org/10.3390/nu15071661
Capra ME, Stanyevic B, Giudice A, Monopoli D, Decarolis NM, Esposito S, Biasucci G. Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review. Nutrients. 2023; 15(7):1661. https://doi.org/10.3390/nu15071661
Chicago/Turabian StyleCapra, Maria Elena, Brigida Stanyevic, Antonella Giudice, Delia Monopoli, Nicola Mattia Decarolis, Susanna Esposito, and Giacomo Biasucci. 2023. "Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review" Nutrients 15, no. 7: 1661. https://doi.org/10.3390/nu15071661
APA StyleCapra, M. E., Stanyevic, B., Giudice, A., Monopoli, D., Decarolis, N. M., Esposito, S., & Biasucci, G. (2023). Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review. Nutrients, 15(7), 1661. https://doi.org/10.3390/nu15071661








