Nutritional Treatment in a Cohort of Pediatric Patients with Familial Hypercholesterolaemia: Effect on Lipid Profile
Abstract
1. Introduction
2. Materials and Methods
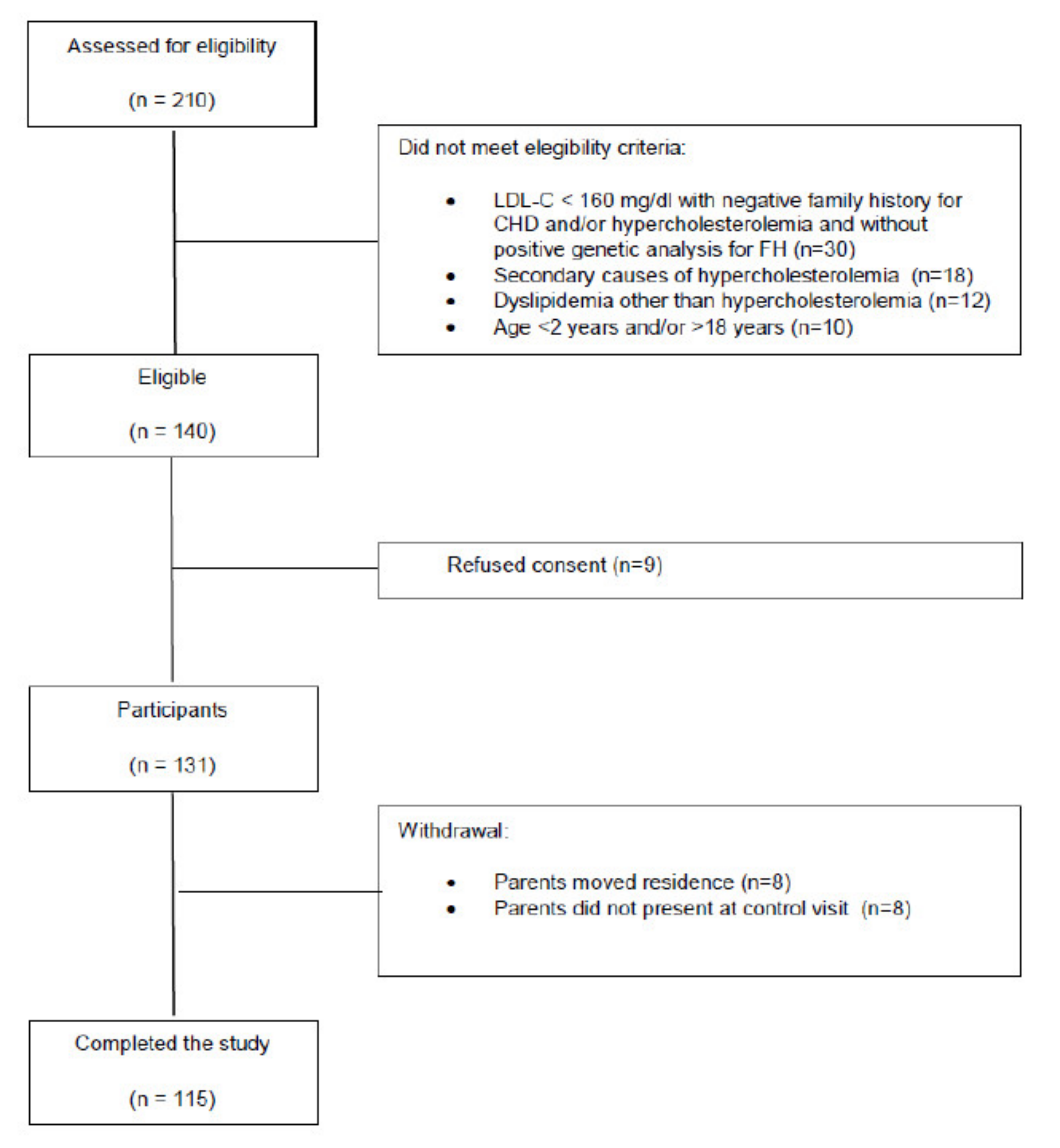
2.1. Study Design and Population
2.2. Study Variables
2.3. Statistic Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
References
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ose, L.; Averna, M.; Boileau, C.; Borén, J.; et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur. Hear. J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, D. The Rationale for Initiating Treatment of Hypercholesterolemia in Young Adulthood. Curr. Atheroscler. Rep. 2013, 15, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pederiva, C.; Capra, M.; Viggiano, C.; Rovelli, V.; Banderali, G.; Biasucci, G. Early Prevention of Atherosclerosis: Detection and Management of Hypercholesterolaemia in Children and Adolescents. Life 2021, 11, 345. [Google Scholar] [CrossRef] [PubMed]
- Capra, M.; Pederiva, C.; Viggiano, C.; De Santis, R.; Banderali, G.; Biasucci, G. Nutritional Approach to Prevention and Treatment of Cardiovascular Disease in Childhood. Nutrients 2021, 13, 2359. [Google Scholar] [CrossRef]
- Arroyo-Olivares, R.; Alonso, R.; Quintana-Navarro, G.; Fuentes-Jiménez, F.; Mata, N.; Muñiz-Grijalvo, O.; Díaz-Díaz, J.L.; Zambón, D.; Arrieta, F.; García-Cruces, J.; et al. Adults with familial hypercholesterolaemia have healthier dietary and lifestyle habits compared with their non-affected relatives: The SAFEHEART study. Public Health Nutr. 2019, 22, 1433–1443. [Google Scholar] [CrossRef]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. S5), S213–S256. [Google Scholar] [CrossRef]
- Capra, M.E.; Pederiva, C.; Banderali, G.; Biasucci, G. Prevention starts from the crib: The pediatric point of view on detection of families at high cardiovascular risk. Ital. J. Pediatr. 2021, 47, 1–6. [Google Scholar] [CrossRef]
- Gidding, S.S.; Dennison, B.A.; Birch, L.L.; Daniels, S.R.; Gilman, M.W.; Lichtenstein, A.H.; Rattay, K.T.; Steinberger, J.; Stettler, N.; Van Horn, L. Dietary Recommendations for Children and Adolescents. Circulation 2005, 112, 2061–2075, Erratum in: Circulation 2005, 112, 2375. Erratum in: Circulation 2006, 113, e857. [Google Scholar] [CrossRef]
- Giovannini, M.; De Carlis, S. Raccomandazioni per la prevenzione in età pediatrica dell’aterosclerosi. Riv. Ital. Pediatr. 2000, 26, 13–28. [Google Scholar]
- Bel-Serrat, S.; Mouratidou, T.; Pala, V.; Huybrechts, I.; Börnhorst, C.; Fernández-Alvira, J.M.; Hadjigeorgiou, C.; Eiben, G.; Hebestreit, A.; Lissner, L.; et al. Relative validity of the Children’s Eating Habits Questionnaire–food frequency section among young European children: The IDEFICS Study. Public Health Nutr. 2014, 17, 266–276. [Google Scholar] [CrossRef]
- Polonsky, S.M.; Bellet, P.S.; Sprecher, D.L. Primary Hyperlipidemia in a Pediatric Population: Classification and Effect of Dietary Treatment. Pediatrics 1993, 91, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.A.; Shapero, J.; McNerney, C.; Glueck, C.J.; Tracy, T.; Gartside, P. Changes in plasma lipid and lipoprotein fractions after alteration in dietary cholesterol, polyunsaturated, saturated, and total fat in free-living normal and hypercholesterolemic children. Am. J. Clin. Nutr. 1982, 35, 1375–1390. [Google Scholar] [CrossRef] [PubMed]
- Shannon, B.M.; Tershakovec, A.M.; Martel, J.R.; Achterberg, C.L.; Cortner, J.A.; Smiciklas-Wright, H.S.; Stallings, V.A.; Stolley, P.D. Reduction of elevated LDL-cholesterol levels of 4 to 10-year-old children through home-based dietary education. Pediatrics 1994, 94, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.R.; Moore, L.L.; Garrahie, E.J.; Ellison, R.C. The tracking of nutrient intake in young children: The Framingham Children’s Study. Am. J. Public Health 1995, 85, 1673–1677. [Google Scholar] [CrossRef] [PubMed]
- Tonstad, S.; Leren, T.P.; Sivertsen, M.; Ose, L. Determinants of Lipid Levels Among Children with Heterozygous Familial Hypercholesterolemia in Norway. Arter. Thromb. Vasc. Biol. 1995, 15, 1009–1014. [Google Scholar] [CrossRef]
- Kwiterovich, P.O.; Hartmuller, G.; Van Horn, L.; Christoffel, K.K.; Gernhoffer, N.; Gidding, S.; Lavigne, J.V.; Lauer, R.M.; Snetselaar, L.; Steinmuller, P.; et al. Efficacy and Safety of Lowering Dietary Intake of Fat and Cholesterol in Children with Elevated Low-Density Lipoprotein Cholesterol. The Dietary Intervention Study in Children (DISC). JAMA 1995, 273, 1429–1435. [Google Scholar] [CrossRef]
- Torvik, K.; Narverud, I.; Ottestad, I.; Svilaas, A.; Gran, J.M.; Retterstøl, K.; Ellingvåg, A.; Strøm, E.; Ose, L.; Veierød, M.B.; et al. Dietary counseling is associated with an improved lipid profile in children with familial hypercholesterolemia. Atherosclerosis 2016, 252, 21–27. [Google Scholar] [CrossRef][Green Version]
- Cicero, A.F.; Fogacci, F.; Giovannini, M.; Bove, M.; Debellis, G.; Borghi, C. Effect of quantitative and qualitative diet prescription on children behavior after diagnosis of heterozygous familial hypercholesterolemia. Int. J. Cardiol. 2019, 293, 193–196. [Google Scholar] [CrossRef]
- Barkas, F.; Nomikos, T.; Liberopoulos, E.; Panagiotakos, D. Diet and Cardiovascular Disease Risk Among Individuals with Familial Hypercholesterolemia: Systematic Review and Meta-Analysis. Nutrients 2020, 12, 2436. [Google Scholar] [CrossRef]
- Helk, O.; Widhalm, K. Effects of a low-fat dietary regimen enriched with soy in children affected with heterozygous familial hypercholesterolemia. Clin. Nutr. Espen 2019, 36, 150–156. [Google Scholar] [CrossRef]
- Banderali, G.; Capra, M.E.; Viggiano, C.; Biasucci, G.; Pederiva, C. Nutraceuticals in Paediatric Patients with Dyslipidaemia. Nutrients 2022, 14, 569. [Google Scholar] [CrossRef] [PubMed]
- Shafiq, N.; Singh, M.; Kaur, S.; Khosla, P.; Malhotra, S. Dietary treatment for familial hypercholesterolaemia. Cochrane Database Syst. Rev. 2010, 12, 2436. [Google Scholar] [CrossRef]
- Roy, G.; Boucher, A.; Couture, P.; Drouin-Chartier, J.-P. Impact of Diet on Plasma Lipids in Individuals with Heterozygous Familial Hypercholesterolemia: A Systematic Review of Randomized Controlled Nutritional Studies. Nutrients 2021, 13, 235. [Google Scholar] [CrossRef] [PubMed]
- Ference, B.A.; Yoo, W.; Alesh, I.; Mahajan, N.; Mirowska, K.K.; Mewada, A.; Kahn, J.; Afonso, L.; Williams, K.A.; Flack, J.M. Effect of Long-Term Exposure to Lower Low-Density Lipoprotein Cholesterol Beginning Early in Life on the Risk of Coronary Heart Disease: A Mendelian Randomization Analysis. J. Am. Coll. Cardiol. 2012, 60, 2631–2639. [Google Scholar] [CrossRef] [PubMed]
- The Myocardial Infarction Genetics Consortium Investigators Inactivating Mutations in NPC1L1 and Protection from Coronary Heart Disease. N. Engl. J. Med. 2014, 371, 2072–2082. [CrossRef] [PubMed]
- Molven, I.; Retterstøl, K.; Andersen, L.F.; Veierød, M.B.; Narverud, I.; Ose, L.; Svilaas, A.; Wandel, M.; Holven, K.B. Children and young adults with familial hypercholesterolaemia (FH) have healthier food choices particularly with respect to dietary fat sources compared with non-FH children. J. Nutr. Sci. 2013, 2, e32. [Google Scholar] [CrossRef]
- Millen, B.E.; Abrams, S.; Adams-Campbell, L.; Anderson, C.A.; Brenna, J.T.; Campbell, W.W.; Clinton, S.; Hu, F.; Nelson, M.; Neuhouser, M.L.; et al. The 2015 Dietary Guidelines Advisory Committee Scientific Report: Development and Major Conclusions. Adv. Nutr. Int. Rev. J. 2016, 7, 438–444. [Google Scholar] [CrossRef]
- Brandhorst, S.; Longo, V.D. Dietary Restrictions and Nutrition in the Prevention and Treatment of Cardiovascular Disease. Circ. Res. 2019, 124, 952–965. [Google Scholar] [CrossRef]
- Guasch-Ferré, M.; Babio, N.; Martínez-González, M.A.; Corella, D.; Ros, E.; Martín-Peláez, S.; Estruch, R.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; et al. Dietary Fat Intake and Risk of Cardiovascular Disease and All-Cause Mortality in a Population at High Risk of Cardiovascular Disease. Am. J. Clin. Nutr. 2015, 102, 1563–1573. [Google Scholar] [CrossRef]
| All Patients | Male | Female | |
|---|---|---|---|
| Number | 115 | 57 | 58 |
| Age (years, mean ± sd) | 9.40 ± 4.11 | 9.40 ± 3.40 | 9.31 ± 4.62 |
| BMI (n, %) | |||
| 1: normal weight | 82 (71.30%) | 40 (70.17%) | 42 (72.41%) |
| 2: overweight | 18 (15.65%) | 9 (15.79%) | 9 (15.50%) |
| 3: obese | 11 (9.58%) | 6 (10.52%) | 5 (8.62%) |
| 4: underweight | 4 (3.47%) | 2 (3.51%) | 2 (3.47%) |
| Genetic analysis for FH (positive, %) | 85 (73.91%) | 43 (75.43%) | 42 (72.41%) |
| Total cholesterol (mg/dL, mean ± sd) | 285.87 ± 51.11 | 281.19 ± 55.78 | 290.46 ± 46.09 |
| LDL cholesterol (mg/dL, mean ± sd) | 214.94 ± 47.73 | 210.72 ± 51.07 | 219.08 ± 44.27 |
| HDL cholesterol (mg/dL, mean ± sd) | 52.85 ± 13.10 | 53.02 ± 12.26 | 52.70 ± 13.72 |
| Triglycerides (mg/dL, mean ± sd) | 87.03 ± 46.75 | 78.23 ± 34.18 | 95.67 ± 55.32 |
| Non-HDL cholesterol (mg/dL, mean ± sd) | 233.02 ± 51.44 | 228.19 ± 55.21 | 237.76 ± 47.40 |
| T0 | T1 | p Value | |
|---|---|---|---|
| Breakfast (yes, n, %) | 106 (92%) | 109 (95%) | 0.37 |
| Fruit and vegetables (weekly portions, mean ± sd) | 16.0 ± 11.4 | 22.3 ± 10.1 | <0.01 * |
| Meat (weekly portions, mean ± sd) | 4.5 ± 2.4 | 3.7 ± 1.2 | <0.01 * |
| Sausages (weekly portions, mean ± sd) | 2.7 ± 1.9 | 1.6 ± 1.2 | <0.01 * |
| Fish (weekly portions, mean ± sd) | 1.8 ± 1.2 | 2.4 ± 1.1 | <0.01 * |
| Pulses (weekly portions, mean ± sd) | 1.5 ± 1.6 | 1.8 ± 1.2 | 0.01 * |
| Cheese (weekly portions, mean ± sd) | 2.9 ± 2.3 | 1.5 ± 1.3 | <0.01 * |
| Eggs (weekly portions, mean ± sd) | 0.7 ± 0.7 | 0.9 ± 0.6 | 0.01 * |
| Whole foods (weekly portions, mean ± sd) | 1.4 ± 3.5 | 2.6 ± 4 | <0.01 * |
| Junk foods (weekly portions, mean ± sd) | 8.2 ± 6.5 | 4.3 ± 3.6 | <0.01 * |
| Screen time (daily hours, mean ± sd) | 2.7 ± 1.5 | 2.5 ± 1.5 | <0.01 * |
| Physical activity (daily hours, mean ± sd) | 1.6 ± 0.7 | 1.6 ± 0.3 | 0.11 |
| Sport (weekly hours, mean ± sd) | 1.36 ± 1.5 | 1.42 ± 1.5 | 0.02 |
| T0 | T1 | p Value | |
|---|---|---|---|
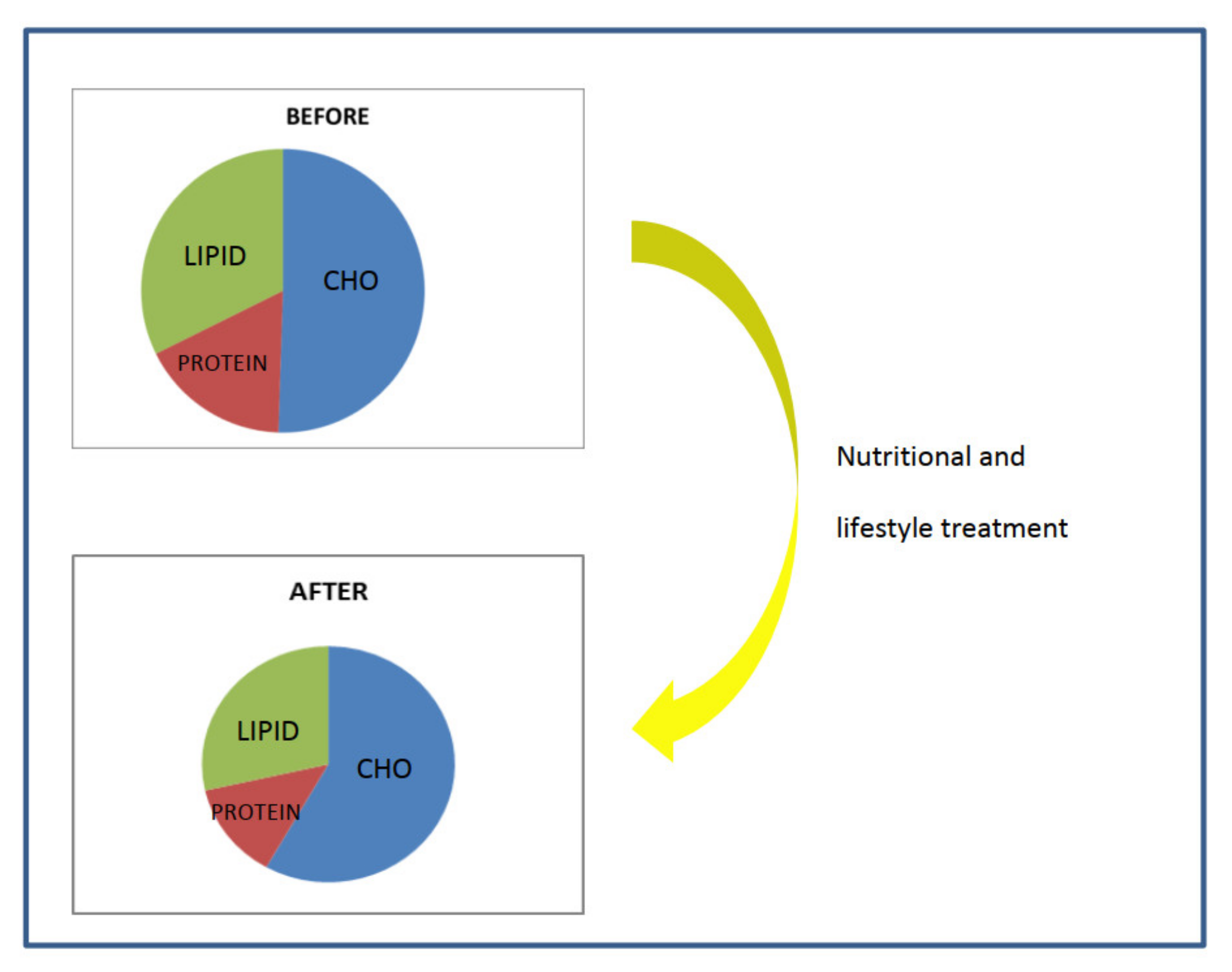
| Carbohydrates (Energy %) | 50.1 ± 2.3 | 57.2 ± 2.7 | <0.01 * |
| Fiber (g/day) | 3.8 ± 2.4 | 5.5 ± 1.2 | 0.08 |
| Protein (Energy %) | 17.3 ± 1.6 | 13.8 ± 1.2 | <0.01 * |
| Fat (Energy %) | 32.8 ± 2.3 | 29.3 ± 2.5 | <0.01 * |
| T0 | T1 | p Value | |
|---|---|---|---|
| Total cholesterol | 283.47 ± 48.84 | 279.17 ± 48.03 | 0.31 |
| LDL cholesterol | 214.62 ± 48.69 | 209.41 ± 47.38 | 0.23 |
| HDL cholesterol | 53.01 ± 12.84 | 53.65 ± 10.89 | 0.37 |
| Triglycerides | 82.36 ± 39.71 | 78.15 ± 29.19 | 0.39 |
| Non-HDL cholesterol | 230.47 ± 50.23 | 225.52 ± 49.80 | 0.22 |
| T0 | T1 | p Value | |
|---|---|---|---|
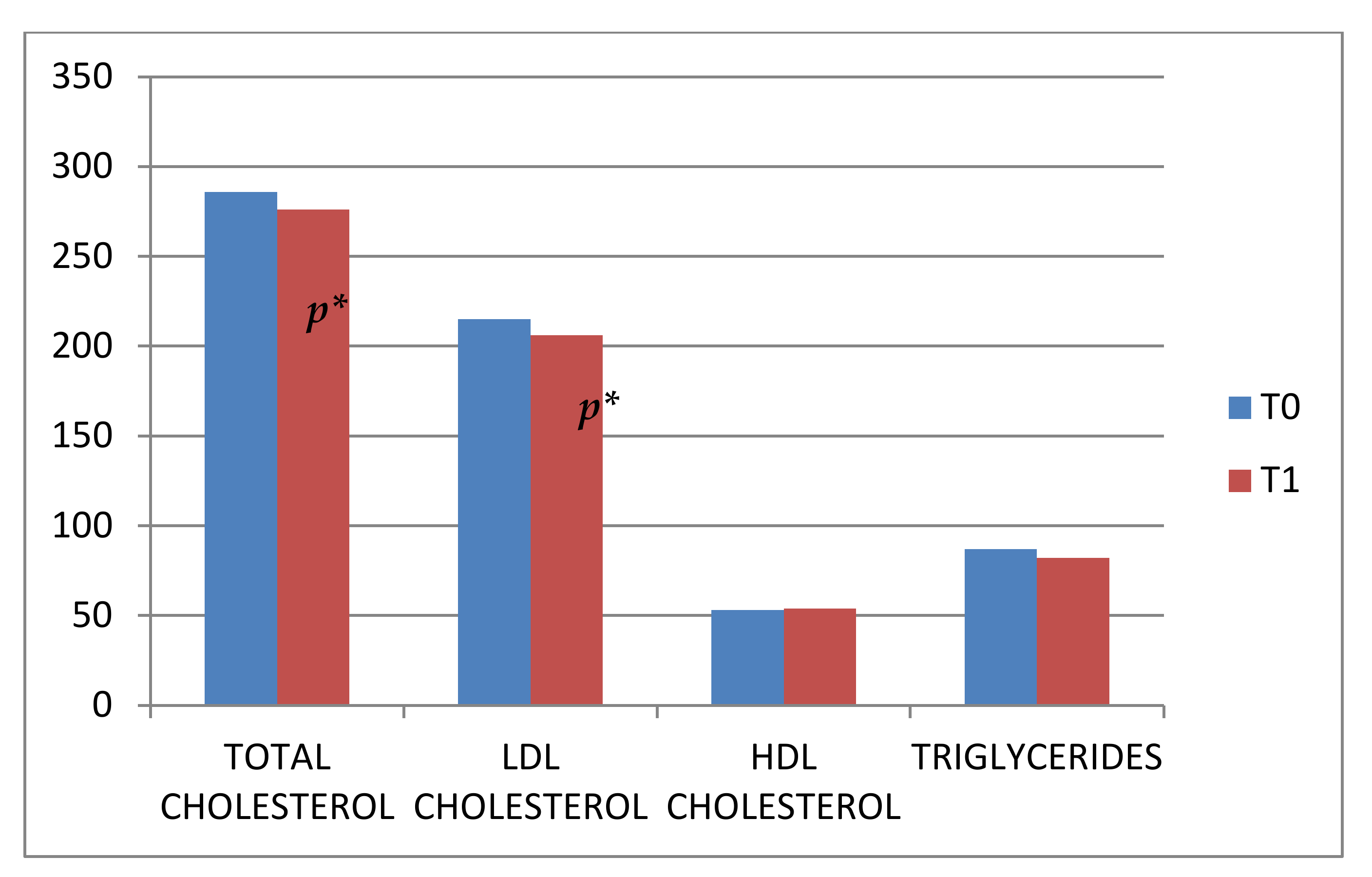
| Total cholesterol | 289.10 ± 54.37 | 273.22 ± 45.36 | <0.01 * |
| LDL cholesterol | 215.37 ± 46.93 | 202.43 ± 45.70 | <0.01 * |
| HDL cholesterol | 52.65 ± 13.26 | 55.47 ± 12.31 | 0.08 |
| Triglycerides | 93.31 ± 54.54 | 87.55 ± 47.93 | 0.78 |
| Non-HDL cholesterol | 236.45 ± 53.31 | 217.76 ± 44.16 | <0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capra, M.E.; Pederiva, C.; Viggiano, C.; Fabrizi, E.; Banderali, G.; Biasucci, G. Nutritional Treatment in a Cohort of Pediatric Patients with Familial Hypercholesterolaemia: Effect on Lipid Profile. Nutrients 2022, 14, 2817. https://doi.org/10.3390/nu14142817
Capra ME, Pederiva C, Viggiano C, Fabrizi E, Banderali G, Biasucci G. Nutritional Treatment in a Cohort of Pediatric Patients with Familial Hypercholesterolaemia: Effect on Lipid Profile. Nutrients. 2022; 14(14):2817. https://doi.org/10.3390/nu14142817
Chicago/Turabian StyleCapra, Maria Elena, Cristina Pederiva, Claudia Viggiano, Enrico Fabrizi, Giuseppe Banderali, and Giacomo Biasucci. 2022. "Nutritional Treatment in a Cohort of Pediatric Patients with Familial Hypercholesterolaemia: Effect on Lipid Profile" Nutrients 14, no. 14: 2817. https://doi.org/10.3390/nu14142817
APA StyleCapra, M. E., Pederiva, C., Viggiano, C., Fabrizi, E., Banderali, G., & Biasucci, G. (2022). Nutritional Treatment in a Cohort of Pediatric Patients with Familial Hypercholesterolaemia: Effect on Lipid Profile. Nutrients, 14(14), 2817. https://doi.org/10.3390/nu14142817






