Dietary Models and Cardiovascular Risk Prevention in Pediatric Patients
Abstract
:1. Introduction
2. Mediterranean Diet
2.1. Mediterranean Diet and CVD Prevention in Adult Population
2.2. Mediterranean Diet and CVD Prevention in Pediatric Population
3. Plant-Based Diets
3.1. Plant-Based Diets and CVD Prevention in Adult Population
3.2. Plant-Based Diets and CVD Prevention in Pediatric Population
4. DASH Diet
4.1. DASH Diet and CVD Prevention in Adult Population
4.2. DASH Diet and CVD Prevention in Pediatric Population
5. Nordic Diet
5.1. Nordic Diet and CVD Prevention in Adult Population
5.2. Nordic Diet and CVD Prevention in Pediatric Population
6. Low-Carb Diet
6.1. Low Carbohydrate Diet and CVD Prevention in Adult Population
6.2. Low Carbohydrate Diet and CVD Prevention in Pediatric Population
7. Ketogenic Diet
7.1. Ketogenic Diet and CVD Prevention in Adult Population
7.2. Ketogenic Diet and CVD Prevention in Pediatric Populaton
8. Paleolithic Diet
8.1. Paleolithic Diet and CVD Prevention in Adult Population
8.2. Paleolithic Diet and CVD Prevention in Pediatric Population
9. High protein Diet
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAND | American Academy of Nutrition and Dietetics |
| AHA | American Heart Association |
| ApoB | Apolipoprotein B |
| BBB | Blood Brain Barrier |
| BMI | Body Mass Index |
| BP | Blood Pressure |
| BNP | Brain Natriuretic Peptide |
| BSDS | Baltic Sea Diet Score |
| CHO | Carbohydrate |
| CVD | Cardiovascular Disease |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | Diastolic Blood Pressure |
| DHA | Docosahexaenoic Acid |
| DMT1 | Diabetes Mellitus Type 1 |
| DMT2 | Diabetes Mellitus Type 2 |
| EPA | Eicosapentaenoic Acid |
| EVOO | Extra Virgin Olive Oil |
| GI | Glycemic Index |
| HDL | High Density Lipoprotein |
| HOMA-IR | Homeostasis Model Assessment Insulin Resistance |
| KD | Ketogenic Diet |
| LCD | Low Carbohydrate Diet |
| LCPUFA | Long Chain Polyunsaturated Fatty Acids |
| LDL | Low Density Lipoprotein |
| MAD | Modified Atkins Diet |
| MAFLD | Metabolic dysfunction-Associated Fatty Liver Disease |
| MAP | Mean Arterial Pressure |
| MCTD | Medium Chain Triglycerides Diet |
| MED | Mediterranean |
| MPO | Myeloperoxidase |
| MUFA | Monounsaturated Fatty Acids |
| red | Relative Mediterranean Diet Score |
| NAFLD | Non-Alcoholic Fatty Liver Disease |
| ND | Nordic Diet |
| NND | New Nordic Diet |
| PBD | Plant Based Diets |
| PD | Palaeolithic Diet |
| ROS | Reactive Oxygen Species |
| SBP | Systolic Blood Pressure |
| SFA | Saturated Fatty Acids |
| TDM | Traditional Mediterranean Diet |
| TG | Triglycerides |
| TNF-α | Tumor Necrosis Factor Alfa |
References
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary Report. Pediatrics 2011, 128, S213–S256. [Google Scholar] [CrossRef]
- De Ferranti, S.D.; Steinberger, J.; Urbina, E.M.; Zachariah, J.P.; Zaidi, A.N.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; et al. Cardiovascular Risk Reduction in High-Risk Pediatric Patients: A Scientific Statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef] [PubMed]
- Wiegman, A.; Gidding, S.S.; Watts, G.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ose, L.; Averna, M.; Boileau, C.; Borén, J.; et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur. Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef] [PubMed]
- Capra, M.E.; Pederiva, C.; Viggiano, C.; De Santis, R.; Banderali, G.; Biasucci, G. Nutritional Approach to Prevention and Treatment of Cardiovascular Disease in Childhood. Nutrients 2021, 13, 2359. [Google Scholar] [CrossRef]
- Gardner, C.D.; Vadiveloo, M.K.; Petersen, K.S.; Anderson, C.A.M.; Springfield, S.; Van Horn, L.; Khera, A.; Lamendola, C.; Mayo, S.M.; Joseph, J.J. American Heart Association Council on Lifestyle and Cardiometabolic Health. Popular Dietary Patterns: Alignment with American Heart Association 2021 Dietary Guidance: A Scientific Statement From the American Heart Association. Circulation 2023, 147, 1715–1730. [Google Scholar] [CrossRef]
- Chait, A.; Brunzell, J.; Denke, M.; Eisenberg, D.; Ernst, N.; Franklin, F., Jr.; Ginsberg, H.; Kotchen, T.; Kuller, L.; Mullis, R. Rationale of the diet-heart statement of the American Heart Association: Report of the Nutrition Committee. Circulation 1993, 88, 3008–3029. [Google Scholar] [CrossRef] [PubMed]
- Krauss, R.M.; Eckel, R.H.; Howard, B.; Appel, L.J.; Daniels, S.R.; Deckelbaum, R.J.; Erdman, J.W., Jr.; Kris-Etherton, P.; Goldberg, I.J.; Kotchen, T.A.; et al. AHA dietary guidelines: Revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation 2000, 102, 2284–2299. [Google Scholar] [CrossRef]
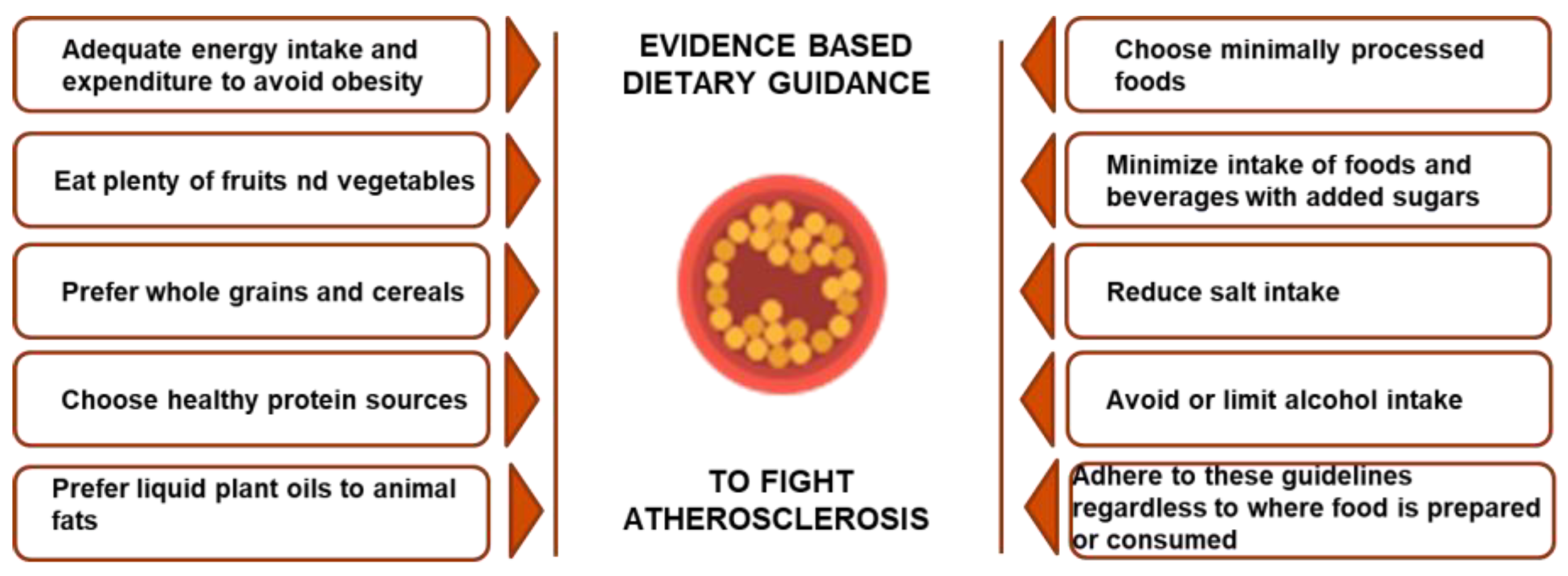
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J.; et al. 2021 Dietary guidance to improve cardiovascular health: A scientific statement from the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef]
- Pederiva, C.; Capra, M.E.; Viggiano, C.; Rovelli, V.; Banderali, G.; Biasucci, G. Early Prevention of Atherosclerosis: Detection and Management of Hypercholesterolaemia in Children and Adolescents. Life 2021, 11, 345. [Google Scholar] [CrossRef]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Dussaillant, C.; Echeverría, G.; Urquiaga, I.; Velasco, N.; Rigotti, A. Current Evidence on Health Benefits of the Mediterranean Diet. Rev. Med. Child. 2016, 144, 1044–1052. [Google Scholar]
- Bonaccio, M.; Iacoviello, L.; Donati, M.B.; de Gaetano, G. The Tenth Anniversary as a UNESCO World Cultural Heritage: An Unmissable Opportunity to Get Back to the Cultural Roots of the Mediterranean Diet. Eur. J. Clin. Nutr. 2022, 76, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Lacoba, R.; Pardo-Garcia, I.; Amo-Saus, E.; Escribano-Sotos, F. Mediterranean diet and health outcomes: A systematic meta-review. Eur. J. Public Health 2018, 28, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Fitó, M.; Estruch, R.; Salas-Salvadó, J.; Martínez-Gonzalez, M.A.; Arós, F.; Vila, J.; Corella, D.; Díaz, O.; Sáez, G.; de la Torre, R.; et al. Effect of the Mediterranean diet on heart failure biomarkers: A randomized sample from the PREDIMED trial. Eur. J. Heart Fail. 2014, 16, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Castillejo, S.; Pedret, A.; Catalán, Ú.; Valls, R.M.; Farràs, M.; Rubió, L.; Castañer, O.; Macià, A.; Fitó, M.; Motilva, M.J.; et al. Virgin Olive Oil Phenolic Compounds Modulate the HDL Lipidome in Hypercholesterolaemic Subjects: A Lipidomic Analysis of the VOHF Study. Mol. Nutr. Food Res. 2021, 65, e2001192. [Google Scholar] [CrossRef] [PubMed]
- Zock, P.L.; Blom, W.A.M.; Nettleton, J.A.; Hornstra, G. Progressing Insights into the Role of Dietary Fats in the Prevention of Cardiovascular Disease. Curr. Cardiol. Rep. 2016, 18, 111. [Google Scholar] [CrossRef] [PubMed]
- Zhong, V.W.; Lamichhane, A.P.; Crandell, J.L.; Couch, S.C.; Liese, A.D.; The, N.S.; Tzeel, B.A.; Dabelea, D.; Lawrence, J.M.; Marcovina, S.M.; et al. Association of adherence to a Mediterranean diet with glycemic control and cardiovascular risk factors in youth with type I diabetes: The SEARCH Nutrition Ancillary Study. Eur. J. Clin. Nutr. 2016, 70, 802–807. [Google Scholar] [CrossRef]
- Vitale, M.; Masulli, M.; Calabrese, I.; Rivellese, A.A.; Bonora, E.; Signorini, S.; Perriello, G.; Squatrito, S.; Buzzetti, R.; Sartore, G.; et al. Impact of a Mediterranean Dietary Pattern and Its Components on Cardiovascular Risk Factors, Glucose Control, and Body Weight in People with Type 2 Diabetes: A Real-Life Study. Nutrients 2018, 10, 1067. [Google Scholar] [CrossRef]
- Chiuve, S.E.; McCullough, M.L.; Sacks, F.M.; Rimm, E.B. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation 2006, 114, 160–167. [Google Scholar] [CrossRef]
- Zurbau, A.; Au-Yeung, F.; Blanco Mejia, S.; Khan, T.A.; Vuksan, V.; Jovanovski, E.; Leiter, L.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Sievenpiper, J.L. Relation of Different Fruit and Vegetable Sources with Incident Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2020, 9, e017728. [Google Scholar] [CrossRef] [PubMed]
- La Torre, G.; Saulle, R.; Di Murro, F.; Siliquini, R.; Firenze, A.; Maurici, M.; Mannocci, A.; Colamesta, V.; Barillà, F.; Ferrante, F.; et al. Mediterranean diet adherence and synergy with acute myocardial infarction and its determinants: A multicenter case-control study in Italy. PLoS ONE 2018, 13, e0193360. [Google Scholar] [CrossRef] [PubMed]
- Kistorp, C.; Raymond, I.; Pedersen, F.; Gustafsson, F.; Faber, J.; Hildebrandt, P. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA 2005, 293, 1609–1616. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Dinu, M.; Pagliai, G.; Cesari, F.; Gori, A.M.; Sereni, A.; Becatti, M.; Fiorillo, C.; Marcucci, R.; Casini, A. Low-Calorie Vegetarian Versus Mediterranean Diets for Reducing Body Weight and Improving Cardiovascular Risk Profile: CARDIVEG Study (Cardiovascular Prevention With Vegetarian Diet). Circulation 2018, 137, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Pagliai, G.; Russo, E.; Niccolai, E.; Dinu, M.; Di Pilato, V.; Magrini, A.; Bartolucci, G.; Baldi, S.; Menicatti, M.; Giusti, B.; et al. Influence of a 3-month low-calorie Mediterranean diet compared to the vegetarian diet on human gut microbiota and SCFA: The CARDIVEG Study. Eur. J. Nutr. 2020, 59, 2011–2024. [Google Scholar] [CrossRef]
- Velázquez-López, L.; Santiago-Díaz, G.; Nava-Hernández, J.; Muñoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014, 14, 175. [Google Scholar] [CrossRef]
- Mozzillo, E.; Zito, E.; Maffeis, C.; De Nitto, E.; Maltoni, G.; Marigliano, M.; Zucchini, S.; Franzese, A.; Valerio, G. Unhealthy lifestyle habits and diabetes-specific health-related quality of life in youths with type 1 diabetes. Acta Diabetol. 2017, 54, 1073–1080. [Google Scholar] [CrossRef]
- Della Corte, C.; Mosca, A.; Vania, A.; Alterio, A.; Iasevoli, S.; Nobili, V. Good adherence to the Mediterranean diet reduces the risk for NASH and diabetes in pediatric patients with obesity: The results of an Italian Study. Nutrition 2017, 39–40, 8–14. [Google Scholar] [CrossRef]
- Feldstein, A.E.; Charatcharoenwitthaya, P.; Treeprasertsuk, S.; Benson, J.T.; Enders, F.B.; Angulo, P. The natural history of nonalcoholic fatty liver disease in children: A follow-up study for up to 20-years. Gut 2010, 58, 1538–1544. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Diehl, A.M.; Brunt, E.M.; Cusi, K.; Charlton, M.; Sanyal, A.J. The Diagnosis and Management of Non-alcoholic Fatty Liver Disease: Practice Guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012, 142, 1592–1609. [Google Scholar] [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J.; on behalf of the International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1991. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Alkhouri, N.; Vajro, P.; Baumann, U.; Weiss, R.; Socha, P.; Marcus, C.; Lee, W.S.; Kelly, D.; Porta, G.; et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: An international expert consensus statement. Lancet Gastroenterol. Hepatol. 2021, 6, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Martíncrespo-Blanco, M.C.; Varillas-Delgado, D.; Blanco-Abril, S.; Cid-Exposito, M.G.; Robledo-Martín, J. Effectiveness of an Intervention Programme on Adherence to the Mediterranean Diet in a Preschool Child: A Randomised Controlled Trial. Nutrients 2022, 14, 1536. [Google Scholar] [CrossRef] [PubMed]
- Desmond, M.A.; Sobiecki, J.G.; Jaworski, M.; Płudowski, P.; Antoniewicz, J.; Shirley, M.K.; Eaton, S.; Książyk, J.; Cortina-Borja, M.; De Stavola, B.; et al. Growth, body composition, and cardiovascular and nutritional risk of 5- to 10-y-old children consuming vegetarian, vegan, or omnivore diets. Am. J. Clin. Nutr. 2021, 113, 1565–1577. [Google Scholar] [CrossRef] [PubMed]
- Weder, S.; Hoffmann, M.; Becker, K.; Alexy, U.; Keller, M. Energy, Macronutrient Intake, and Anthropometrics of Vegetarian, Vegan, and Omnivorous Children (1–3 Years) in Germany (VeChi Diet Study). Nutrients 2019, 11, 832. [Google Scholar] [CrossRef] [PubMed]
- Craig, W.J.; Mangels, A.R.; Fresán, U.; Marsh, K.; Miles, F.L.; Saunders, A.V.; Haddad, E.H.; Heskey, C.E.; Johnston, P.; Larson-Meyer, E.; et al. The Safe and Effective Use of Plant-Based Diets with Guidelines for Health Professionals. Nutrients 2021, 13, 4144. [Google Scholar] [CrossRef] [PubMed]
- Gan, Z.H.; Cheong, H.C.; Tu, Y.-K.; Kuo, P.-H. Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3952. [Google Scholar] [CrossRef] [PubMed]
- Ferdowsian, H.R.; Barnard, N.D. Effects of plant-based diets on plasma lipids. Am. J. Cardiol. 2009, 104, 947–956. [Google Scholar] [CrossRef]
- Boeing, H.; Bechthold, A.; Bub, A.; Ellinger, S.; Haller, D.; Kroke, A.; Leschik-Bonnet, E.; Müller, M.J.; Oberritter, H.; Schulze, M.; et al. Critical review: Vegetables and fruit in the prevention of chronic diseases. Eur. J. Nutr. 2012, 51, 637–663. [Google Scholar] [CrossRef]
- Fujioka, N.; Fritz, V.; Upadhyaya, P.; Kassie, F.; Hecht, S.S. Research on cruciferous vegetables, indole-3-carbinol, and cancer prevention: A tribute to Lee W. Wattenberg. Mol. Nutr. Food Res. 2016, 60, 1228–1238. [Google Scholar] [CrossRef]
- Lee, A.; Beaubernard, L.; Lamothe, V.; Bennetau-Pelissero, C. New Evaluation of Isoflavone Exposure in the French Population. Nutrients 2019, 11, 2308. [Google Scholar] [CrossRef] [PubMed]
- Verneau, F.; La Barbera, F.; Furno, M. The Role of Health Information in Consumers’ Willingness to Pay for Canned Crushed Tomatoes Enriched with Lycopene. Nutrients 2019, 11, 2173. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Solmi, M.; Caruso, M.G.; Giannelli, G.; Osella, A.R.; Evangelou, E.; Maggi, S.; Fontana, L.; Stubbs, B.; Tzoulaki, I. Dietary fiber and health outcomes: An umbrella review of systematic reviews and meta-analyses. Am. J. Clin. Nutr. 2018, 107, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Viguiliouk, E.; Glenn, A.J.; Nishi, S.K.; Chiavaroli, L.; Seider, M.; Khan, T.; Bonaccio, M.; Iacoviello, L.; Mejia, S.B.; Jenkins, D.J.A.; et al. Associations between Dietary Pulses Alone or with Other Legumes and Cardiometabolic Disease Outcomes: An Umbrella Review and Updated Systematic Review and Meta-analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, S308–S319. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, A.J.; de Souza, R.J.; Meyre, D.; Anand, S.S.; Mente, A. A systematic review and meta-analysis of nut consumption and incident risk of CVD and all-cause mortality. Br. J. Nutr. 2016, 115, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated fatty acids, olive oil and health status: A systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef]
- Qian, F.; Liu, G.; Hu, F.B.; Bhupathiraju, S.N.; Sun, Q. Association between Plant-Based Dietary Patterns and Risk of Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2019, 179, 1335–1344. [Google Scholar] [CrossRef]
- Neuenschwander, M.; Ballon, A.; Weber, K.S.; Norat, T.; Aune, D.; Schwingshackl, L.; Schlesinger, S. Role of diet in type 2 diabetes incidence: Umbrella review of meta-analyses of prospective observational studies. BMJ 2019, 366, l2368. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern. Med. 2014, 174, 577–587. [Google Scholar] [CrossRef]
- Le, L.T.; Sabaté, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef]
- Barnard, N.D.; Levin, S.M.; Yokoyama, Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J. Acad. Nutr. Diet. 2015, 115, 954–969. [Google Scholar] [CrossRef] [PubMed]
- Poore, J.; Nemecek, T. Reducing food’s environmental impacts through producers and consumers. Science 2018, 360, 987–992, Erratum in Science 2019, 22, 363. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492, Erratum in Lancet 2019, 393, 530. Erratum in Lancet 2019, 393, 2590. Erratum in Lancet 2020, 395, 338. Erratum in Lancet 2020, 396, e56. [Google Scholar] [CrossRef] [PubMed]
- Jardine, M.A.; Kahleova, H.; Levin, S.M.; Ali, Z.; Trapp, C.B.; Barnard, N.D. Perspective: Plant-Based Eating Pattern for Type 2 Diabetes Prevention and Treatment: Efficacy, Mechanisms, and Practical Considerations. Adv. Nutr. 2021, 12, 2045–2055. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A. The Role of Vegan Diets in Lipotoxicity-induced Beta-cell Dysfunction in Type-2-Diabetes: A Narrative Review. J. Popul. Ther. Clin. Pharmacol. 2020, 27 Pt 2, e22–e38. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, J.; van Daalen, K.R.; Thayyil, A.; Cocco, M.T.A.R.R.; Caputo, D.; Oliver-Williams, C. A Systematic Review of the Association Between Vegan Diets and Risk of Cardiovascular Disease. J. Nutr. 2021, 151, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Jabri, A.; Kumar, A.; Verghese, E.; Alameh, A.; Kumar, A.; Khan, M.S.; Khan, S.U.; Michos, E.D.; Kapadia, S.R.; Reed, G.W.; et al. Meta-analysis of effect of vegetarian diet on ischemic heart disease and all-cause mortality. Am. J. Prev. Cardiol. 2021, 7, 100182. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Appleby, P.N.; Bradbury, K.E.; Perez-Cornago, A.; Travis, R.C.; Clarke, R.; Key, T.J. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: Results from the prospective EPIC-Oxford study. BMJ 2019, 366, l4897. [Google Scholar] [CrossRef]
- Storz, M.A.; Helle, P. Atrial fibrillation risk factor management with a plant-based diet: A review. J. Arrhythm. 2019, 35, 781–788. [Google Scholar] [CrossRef]
- Müller, A.; Zimmermann-Klemd, A.M.; Lederer, A.K.; Hannibal, L.; Kowarschik, S.; Huber, R.; Storz, M.A. A Vegan Diet Is Associated with a Significant Reduction in Dietary Acid Load: Post Hoc Analysis of a Randomized Controlled Trial in Healthy Individuals. Int. J. Environ. Res. Public Health 2021, 18, 9998. [Google Scholar] [CrossRef]
- Dressler, J.; Storz, M.A.; Müller, C.; Kandil, F.I.; Kessler, C.S.; Michalsen, A.; Jeitler, M. Does a Plant-Based Diet Stand Out for Its Favorable Composition for Heart Health? Dietary Intake Data from a Randomized Controlled Trial. Nutrients 2022, 14, 4597. [Google Scholar] [CrossRef] [PubMed]
- Viguiliouk, E.; Kendall, C.W.; Kahleová, H.; Rahelić, D.; Salas-Salvadó, J.; Choo, V.L.; Mejia, S.B.; Stewart, S.E.; Leiter, L.A.; Jenkins, D.J.; et al. Effect of vegetarian dietary patterns on cardiometabolic risk factors in diabetes: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. 2019, 38, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Al-Khudairy, L.; Takeda, A.; Stranges, S. Vegan dietary pattern for the primary and secondary prevention of cardiovascular diseases. Cochrane Database Syst. Rev. 2021, 2, CD013501. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Boeing, H.; Grünewald-Funk, D.; Heseker, H.; Kroke, A.; Leschik-Bonnet, E.; Oberritter, H.; Strohm, D.; Watzl, B. For the German Nutrition Society. Vegan diet. Position of the German Nutrition Society (DGE). Ernähr. Umsch. 2016, 63, 92–102. [Google Scholar]
- Weaver, C.M.; Gordon, C.M.; Janz, K.F.; Kalkwarf, H.J.; Lappe, J.M.; Lewis, R.; O’Karma, M.; Wallace, T.C.; Zemel, B.S. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporos. Int. 2016, 27, 1281–1386, Erratum in Osteoporos. Int. 2016, 27, 1387. [Google Scholar] [CrossRef] [PubMed]
- Alexy, U.; Fischer, M.; Weder, S.; Längler, A.; Michalsen, A.; Sputtek, A.; Keller, M. Nutrient Intake and Status of German Children and Adolescents Consuming Vegetarian, Vegan or Omnivore Diets: Results of the VeChi Youth Study. Nutrients 2021, 13, 1707. [Google Scholar] [CrossRef] [PubMed]
- Hovinen, T.; Korkalo, L.; Freese, R.; Skaffari, E.; Isohanni, P.; Niemi, M.; Nevalainen, J.; Gylling, H.; Zamboni, N.; Erkkola, M.; et al. Vegan diet in young children remodels metabolism and challenges the statuses of essential nutrients. EMBO Mol. Med. 2021, 13, e13492. [Google Scholar] [CrossRef]
- Macknin, M.; Kong, T.; Weier, A.; Worley, S.; Tang, A.S.; Alkhouri, N.; Golubic, M. Plant-based, no-added-fat or American Heart Association diets: Impact on cardiovascular risk in obese children with hypercholesterolemia and their parents. J. Pediatr. 2015, 166, e1–e3. [Google Scholar] [CrossRef]
- Macknin, M.; Stegmeier, N.; Thomas, A.; Worley, S.; Li, L.; Hazen, S.L.; Tang, W.H.W. Three Healthy Eating Patterns and Cardiovascular Disease Risk Markers in 9 to 18 Year Olds With Body Mass Index >95%: A Randomized Trial. Clin Pediatr. 2021, 60, 474–484. [Google Scholar] [CrossRef]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.; Fidler Mis, N.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Li, N.; Yang, R.; Liao, X.Y.; Zhang, Y.; Zhu, B.F.; Zhao, Q.; Chen, L.; Zhang, Y.G.; Lei, Y. Effects of the Modified DASH Diet on Adults with Elevated Blood Pressure or Hypertension: A Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 725020, Erratum in Front. Nutr. 2021, 8, 778414. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute. Your Guide to Lowering Your Blood Pressure with DASH; NIH Publication no. 06-4082; NIH, National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2006. [Google Scholar]
- He, F.J.; Markandu, N.D.; Coltart, R.; Barron, J.; MacGregor, G.A. Effect of shortterm supplementation of potassium chloride and potassium citrate on blood pressure in hypertensives. Hypertension 2005, 45, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Streppel, M.T.; Arends, L.R.; van’t Veer, P.; Grobbee, D.E.; Geleijnse, J.M. Dietary fiber and blood pressure: A meta-analysis of randomized placebo-controlled trials. Arch. Intern. Med. 2005, 165, 150–156. [Google Scholar] [CrossRef]
- Bucher, H.C.; Cook, R.J.; Guyatt, G.H.; Lang, J.D.; Cook, D.J.; Hatala, R.; Hunt, D.L. Effects of dietary calcium supplementation on blood pressure. A meta-analysis of randomized controlled trials. JAMA 1996, 275, 1016–1022. [Google Scholar] [CrossRef]
- Ward, N.C.; Hodgson, J.M.; Croft, K.D.; Burke, V.; Beilin, L.J.; Puddey, I.B. The combination of vitamin C and grape-seed polyphenols increases blood pressure: A randomized, double-blind, placebo-controlled trial. J. Hypertens. 2005, 23, 427–434. [Google Scholar] [CrossRef] [PubMed]
- McEneny, J.; Couston, C.; McKibben, B.; Young, I.S.; Woodside, J.V. Folate: In vitro and in vivo effects on VLDL and LDL oxidation. Int. J. Vitam. Nutr. Res. 2007, 77, 66–72. [Google Scholar] [CrossRef]
- Saneei, P.; Hashemipour, M.; Kelishadi, R.; Rajaei, S.; Esmaillzadeh, A. Effects of recommendations to follow the Dietary Approaches to Stop Hypertension (DASH) diet v. usual dietary advice on childhood metabolic syndrome: A randomised cross-over clinical trial. Br. J. Nutr. 2013, 110, 2250–2259. [Google Scholar] [CrossRef]
- Appel, L.J.; Brands, M.W.; Daniels, S.R.; Karanja, N.; Elmer, P.J.; Sacks, F.M.; American Heart Association. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension 2006, 47, 296–308. [Google Scholar] [CrossRef]
- Azadbakht, L.; Surkan, P.J.; Esmaillzadeh, A.; Willett, W.C. The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J. Nutr. 2011, 141, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Asemi, Z.; Samimi, M.; Tabassi, Z.; Sabihi, S.S.; Esmaillzadeh, A. A randomized controlled clinical trial investigating the effect of DASH diet on insulin resistance, inflammation, and oxidative stress in gestational diabetes. Nutrition 2013, 29, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Maruthur, N.M.; Appel, L.J. The effect of dietary patterns on estimated coronary heart disease risk: Results from the Dietary Approaches to Stop Hypertension (DASH) trial. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2015, 113, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Tiong, X.T.; Nursara Shahirah, A.; Pun, V.C.; Wong, K.Y.; Fong, A.Y.Y.; Sy, R.G.; Castillo-Carandang, N.T.; Nang, E.E.K.; Woodward, M.; van Dam, R.M.; et al. The association of the dietary approach to stop hypertension (DASH) diet with blood pressure, glucose and lipid profiles in Malaysian and Philippines populations. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, D.; Kay, M.; Burroughs, J.; Svetkey, L.P.; Bennett, G.G. The Effect of a Digital Behavioral Weight Loss Intervention on Adherence to the Dietary Approaches to Stop Hypertension (DASH) Dietary Pattern in Medically Vulnerable Primary Care Patients: Results from a Randomized Controlled Trial. J. Acad. Nutr. Diet. 2019, 119, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Kucharska, A.; Gajewska, D.; Kiedrowski, M.; Sińska, B.; Juszczyk, G.; Czerw, A.; Augustynowicz, A.; Bobiński, K.; Deptała, A.; Niegowska, J. The impact of individualised nutritional therapy according to DASH diet on blood pressure, body mass, and selected biochemical parameters in overweight/obese patients with primary arterial hypertension: A prospective randomised study. Kardiol. Pol. 2018, 76, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Couch, S.C.; Saelens, B.E.; Levin, L.; Dart, K.; Falciglia, G.; Daniels, S.R. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J. Pediatr. 2008, 152, 494–501. [Google Scholar] [CrossRef]
- Mahdavi, A.; Mohammadi, H.; Foshati, S.; Shokri-Mashhadi, N.; Clark, C.C.T.; Moafi, A.; Rouhani, M.H. Effects of the dietary approach to stop hypertension (DASH) diet on blood pressure, blood glucose, and lipid profile in adolescents with hemophilia: A randomized clinical trial. Food Sci. Nutr. 2020, 9, 145–153. [Google Scholar] [CrossRef]
- Mithril, C.; Dragsted, L.O.; Meyer, C.; Blauert, E.; Holt, M.K.; Astrup, A. Guidelines for the New Nordic Diet. Public Health Nutr. 2012, 15, 1941–1947. [Google Scholar] [CrossRef] [PubMed]
- Slimani, N.; Fahey, M.; Welch, A.A.; Wirfält, E.; Stripp, C.; Bergström, E.; Linseisen, J.; Schulze, M.B.; Bamia, C.; Chloptsios, Y.; et al. Diversity of dietary patterns observed in the European Prospective Investigation into Cancer and Nutrition (EPIC) project. Public Health Nutr. 2002, 5, 1311–1328. [Google Scholar] [CrossRef] [PubMed]
- Kanerva, N.; Kaartinen, N.E.; Schwab, U.; Lahti-Koski, M.; Männistö, S. The Baltic Sea Diet Score: A tool for assessing healthy eating in Nordic countries. Public Health Nutr. 2014, 17, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Adamsson, V.; Reumark, A.; Cederholm, T.; Vessby, B.; Risérus, U.; Johansson, G. What is a healthy Nordic diet? Foods and nutrients in the NORDIET study. Food Nutr. Res. 2012, 56, 18189. [Google Scholar] [CrossRef]
- Zampelas, A.; Magriplis, E. Dietary patterns and risk of cardiovascular diseases: A review of the evidence. Proc. Nutr. Soc. 2020, 79, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Summerbell, C.D.; Thompson, R.; Sills, D.; Roberts, F.G.; Moore, H.J.; Smith, G.D. Reduced or modified dietary fat for preventing cardiovascular disease. Sao Paulo Med. J. 2016, 134, 182–183. [Google Scholar] [CrossRef]
- Puska, P.; Vartiainen, E.; Tuomilehto, J.; Salomaa, V.; Nissinen, A. Changes in premature deaths in Finland: Successful long-term prevention of cardiovascular diseases. Bull. World Health Organ. 1998, 76, 419–425. [Google Scholar]
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. CMAJ 2020, 192, E875–E891. [Google Scholar] [CrossRef]
- Sievenpiper, J.L.; Chan, C.B.; Dworatzek, P.D.; Freeze, C.; Williams, S.L.; Diabetes Canada Clinical Practice Guidelines Expert Committee. Nutrition Therapy. Can. J. Diabetes 2018, 42 (Suppl. S1), S64–S79. [Google Scholar] [CrossRef]
- Dyson, P.A.; Twenefour, D.; Breen, C.; Duncan, A.; Elvin, E.; Goff, L.; Hill, A.; Kalsi, P.; Marsland, N.; McArdle, P.; et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet. Med. 2018, 35, 541–547. [Google Scholar] [CrossRef]
- Helsedirektoratet. Diagnostikk av diabetes, risikovurdering ognoppfølging av personer med høy risiko for å utvikle diabetes. [1. Diagnosis of diabetes, risk assessment and follow-up of people athigh risk of developing diabetes]. In Diabetes—National Professional Guideline; Helsedirektoratet: Oslo, Norway, 2016. [Google Scholar]
- Pohjolainen, T.; Leinonen, V.; Frantén, J.; Haanpää, M.; Jousimaa, J.; Karppinen, J.; Kuukkanen, T.; Luoma, K.; Salmenkivi, J.; Osterman, H.; et al. Update on Current Care Guideline. Diabetes Duodecim. 2016, 132, 881–882. [Google Scholar]
- Massara, P.; Zurbau, A.; Glenn, A.J.; Chiavaroli, L.; Khan, T.A.; Viguiliouk, E.; Mejia, S.B.; Comelli, E.M.; Chen, V.; Schwab, U.; et al. Nordic dietary patterns and cardiometabolic outcomes: A systematic review and meta-analysis of prospective cohort studies and randomised controlled trials. Diabetologia 2022, 65, 2011–2031. [Google Scholar] [CrossRef] [PubMed]
- Niinikoski, H.; Lagström, H.; Jokinen, E.; Siltala, M.; Rönnemaa, T.; Viikari, J.; Raitakari, O.T.; Jula, A.; Marniemi, J.; Näntö-Salonen, K.; et al. Impact of Repeated Dietary Counseling Between Infancy and 14 Years of Age on Dietary Intakes and Lipids and Lipoproteins The STRIP Study. Circulation 2007, 116, 1032–1040. [Google Scholar] [CrossRef]
- Simell, O.; Niinikoski, H.; Rönnemaa, T.; Raitakari, O.T.; Lagström, H.; Laurinen, M.; Aromaa, M.; Hakala, P.; Jula, A.; Jokinen, E.; et al. STRIP Study GroupCohort Profile: The STRIP Study (Special Turku Coronary Risk Factor Intervention Project), an Infancy-onset Dietary and Life-style Intervention Trial. Int. J. Epidemiol. 2009, 38, 650–655. [Google Scholar] [CrossRef]
- Pahkala, K.; Tomi TLaitinen, T.T.; Harri Niinikoski, H.; Noora Kartiosuo, N.; Suvi PRovio, S.P.; Hanna Lagström, H.; Loo, B.M.; Salo, P.; Jokinen, E.; Magnussen, C.G.; et al. Effects of 20-year infancy-onset dietary counselling on cardiometabolic risk factors in the Special Turku Coronary Risk Factor Intervention Project (STRIP): 6-year post-intervention follow-up. Lancet Child. Adolesc. Health 2020, 4, 359–369. [Google Scholar] [CrossRef]
- Andersen, R.; Biltoft-Jensen, A.; Christensen, T.; Andersen, E.W.; Ege, M.; Thorsen, A.V.; Dalskov, S.M.; Damsgaard, C.T.; Astrup, A.; Michaelsen, K.F.; et al. Dietary effects of introducing school meals based on the New Nordic Diet—A randomised controlled trial in Danish children. The OPUS School Meal Study. Br. J. Nutr. 2014, 111, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, L.B.; Damsgaard, C.T.; Dalskov, S.M.; Petersen, R.A.; Egelund, N.; Dyssegaard, C.B.; Stark, K.D.; Andersen, R.; Tetens, I.; Astrup, A.; et al. Diet-induced changes in iron and n-3 fatty acid status and associations with cognitive performance in 8–11-year-old Danish children: Secondary analyses of the Optimal Well-Being, Development and Health for Danish Children through a Healthy New Nordic Diet School Meal Study. Br. J. Nutr. 2015, 114, 1623–1637. [Google Scholar] [CrossRef]
- Capra, M.E.; Stanyevic, B.; Giudice, A.; Monopoli, D.; Decarolis, N.M.; Esposito, S.; Biasucci, G. Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review. Nutrients 2023, 15, 1661. [Google Scholar] [CrossRef]
- Agnihotri, N.; Øverby, N.C.; Bere, E.; Wills, A.K.; Brantsaeter, A.L.; Hillesund, E.R. Childhood adherence to a potentially healthy and sustainable Nordic diet and later overweight: The Norwegian Mother, Father and Child Cohort Study (MoBa). Matern. Child. Nutr. 2021, 17, e13101. [Google Scholar] [CrossRef]
- Kanerva, N.; Kaartinen, N.E.; Rissanen, H.; Knekt, P.; Eriksson, J.G.; Sääksjärvi, K.; Sundvall, J.; Männistö, S. Associations of the Baltic Sea diet with cardiometabolic risk factors--a meta-analysis of three Finnish studies. Br. J. Nutr. 2014, 112, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Ramezani-Jolfaie, N.; Mohammadi, M.; Salehi-Abargouei, A. The effect of healthy Nordic diet on cardio-metabolic markers: A systematic review and meta-analysis of randomized controlled clinical trials. Eur. J. Nutr. 2019, 58, 2159–2174. [Google Scholar] [CrossRef]
- Zhang, Z.; Kris-Etherton, P.M.; Hartman, T.J. Birth weight and risk factors for cardiovascular disease and type 2 diabetes in US children and adolescents: 10 year results from NHANES. Matern. Child. Health J. 2014, 18, 1423–1432. [Google Scholar] [CrossRef]
- Meinilä, J.; Perälä, M.M.; Kanerva, N.; Männistö, S.; Wasenius, N.; Kajantie, E.; Salonen, M.; Eriksson, J.G. Birth weight modifies the association between a healthy Nordic diet and office blood pressure in old age. J. Hum. Hypertens. 2021, 35, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Borjabad, C.; Narveud, I.; Christensen, J.J.; Ulven, S.M.; Malo, A.I.; Ibarretxe, D.; Girona, J.; Torvik, K.; Bogsrud, M.P.; Retterstøl, K.; et al. Dietary intake and lipid levels in Norwegian and Spanish children with familial hypercholesterolemia. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1299–1307. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Imamura, F.; Monsivais, P.; Brage, S.; Griffin, S.J.; Wareham, N.J.; Forouhi, N.G. Dietary cost associated with adherence to the Mediterranean diet, and its variation by socio-economic factors in the UK Fenland Study. Br. J. Nutr. 2018, 119, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.E.; McEvoy, C.T.; Prior, L.; Lawton, J.; Patterson, C.C.; Kee, F.; Cupples, M.; Young, I.S.; Appleton, K.; McKinley, M.C.; et al. Barriers to adopting a Mediterranean diet in Northern European adults at high risk of developing cardiovascular disease. J. Hum. Nutr. Diet. 2018, 31, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Stoica, R.A.; Diaconu, C.C.; Rizzo, M.; Toth, P.P.; Stefan, S.D.; Serafinceanu, C.; Nikolic, D.; Poiana, C.; Ionescu-Tirgoviste, C.; Pantea-Stoian, A. Weight loss programmes using low carbohydrate diets to control the cardiovascular risk in adolescents (Review). Exp. Ther. Med. 2021, 21, 90. [Google Scholar] [CrossRef]
- Bravata, D.M.; Sanders, L.; Huang, J.; Krumholz, H.M.; Olkin, I.; Gardner, C.D.; Bravata, D.M. Efficacy and safety of low-carbohydrate diets: A systematic review. JAMA 2003, 289, 1837–1850. [Google Scholar] [CrossRef]
- Swan, G.E.; Powell, N.A.; Knowles, B.L.; Bush, M.T.; Levy, L.B. A definition of free sugars for the UK. Public Health Nutr. 2018, 21, 1636–1638. [Google Scholar] [CrossRef]
- Dowla, S.; Pendergrass, M.; Bolding, M.; Gower, B.; Fontaine, K.; Ashraf, A.; Soleymani, T.; Morrison, S.; Goss, A. Effectiveness of a carbohydrate restricted diet to treat non-alcoholic fatty liver disease in adolescents with obesity: Trial design and methodology. Contemp. Clin. Trials 2018, 68, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, A.J.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S., Jr.; Brehm, B.J.; Bucher, H.C. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 285–293, Erratum in Arch. Intern. Med. 2006, 166, 932. [Google Scholar] [CrossRef] [PubMed]
- Bailes, J.R.; Strow, M.T.; Werthammer, J.; McGinnis, R.A.; Elitsur, Y. Effect of low-carbohydrate, unlimited calorie diet on the treatment of childhood obesity: A prospective controlled study. Metab. Syndr. Relat. Disord. 2003, 1, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Demol, S.; Yackobovitch-Gavan, M.; Shalitin, S.; Nagelberg, N.; Gillon-Keren, M.; Phillip, M. Low-carbohydrate (low & high-fat) versus high-carbohydrate low-fat diets in the treatment of obesity in adolescents. Acta Paediatr. 2009, 98, 346–351. [Google Scholar] [CrossRef]
- Noble, C.A.; Kushner, R.F. An update on low-carbohydrate, high-protein diets. Curr. Opin. Gastroenterol. 2006, 22, 153–159. [Google Scholar] [CrossRef]
- Stern, L.; Iqbal, N.; Seshadri, P.; Chicano, K.L.; Daily, D.A.; McGrory, J.; Williams, M.; Gracely, E.J.; Samaha, F.F. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: One-year follow-up of a randomized trial. Ann. Intern. Med. 2004, 140, 778–785. [Google Scholar] [CrossRef]
- Zeybek, C.; Celebi, A.; Aktuglu-Zeybek, C.; Onal, H.; Yalcin, Y.; Erdem, A.; Akdeniz, C.; Imanov, E.; Altay, S.; Aydin, A. The effect of low-carbohydrate diet on left ventricular diastolic function in obese children. Pediatr. Int. 2010, 52, 218–223. [Google Scholar] [CrossRef]
- Zeybek, C.; Aktuglu-Zeybek, C.; Onal, H.; Altay, S.; Erdem, A.; Celebi, A. Right ventricular subclinical diastolic dysfunction in obese children: The effect of weight reduction with a low-carbohydrate diet. Pediatr. Cardiol. 2009, 30, 946–953. [Google Scholar] [CrossRef]
- Sondike, S.B.; Copperman, N.; Jacobson, M.S. Effects of a low-carbohydrate diet on weight loss and cardiovascular risk factor in overweight adolescents. J. Pediatr. 2003, 142, 253–258. [Google Scholar] [CrossRef]
- Gow, M.L.; Ho, M.; Burrows, T.L.; Baur, L.A.; Stewart, L.; Hutchesson, M.J.; Cowell, C.T.; Collins, C.E.; Garnett, S.P. Impact of dietary macronutrient distribution on BMI and cardiometabolic outcomes in overweight and obese children and adolescents: A systematic review. Nutr. Rev. 2014, 72, 453–470. [Google Scholar] [CrossRef]
- Meckling, K.A.; O’Sullivan, C.; Saari, D. Comparison of a low-fat diet to a low-carbohydrate diet on weight loss, body composition, and risk factors for diabetes and cardiovascular disease in free-living, overweight men and women. J. Clin. Endocrinol. Metab. 2004, 89, 2717–2723. [Google Scholar] [CrossRef] [PubMed]
- Brinkworth, G.D.; Noakes, M.; Keogh, J.B.; Luscombe, N.D.; Wittert, G.A.; Clifton, P.M. Long-term effects of a high-protein, low-carbohydrate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 661–670, Erratum in Int. J. Obes. Relat. Metab. Disord. 2004, 28, 1187. [Google Scholar] [CrossRef] [PubMed]
- Veggiotti, P.; Burlina, A.; Coppola, G.; Cusmai, R.; De Giorgis, V.; Guerrini, R.; Tagliabue, A.; Dalla Bernardina, B. The ketogenic diet for Dravet syndrome and other epileptic encephalopathies: An Italian consensus. Epilepsia 2011, 52, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Kossoff, E.H.; Zupec-Kania, B.A.; Auvin, S.; Ballaban-Gil, K.R.; Christina Bergqvist, A.G.; Blackford, R.; Buchhalter, J.R.; Caraballo, R.H.; Cross, J.H.; Dahlin, M.G.; et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open 2018, 3, 175–192. [Google Scholar] [CrossRef]
- Amar, A.; Abulhassan, A.; Nagham, K.; Pramath, K. Ketogenic Diet: Biochemistry, Weight Loss and Clinical Applications. Nutr. Food Sci. Int. J. 2020, 10, 555782. [Google Scholar] [CrossRef]
- Muscogiuri, G.; El Ghoch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L.; Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO). European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Facts 2021, 14, 222–245. [Google Scholar] [CrossRef] [PubMed]
- Dowis, K.; Banga, S. The Potential Health Benefits of the Ketogenic Diet: A Narrative Review. Nutrients 2021, 13, 1654. [Google Scholar] [CrossRef]
- Athinarayanan, S.J.; Adams, R.N.; Hallberg, S.J.; McKenzie, A.L.; Bhanpuri, N.H.; Campbell, W.W.; Volek, J.S.; Phinney, S.D.; McCarter, J.P. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-Year Non-randomized Clinical Trial. Front. Endocrinol. 2019, 10, 348. [Google Scholar] [CrossRef]
- Carmen, M.; Safer, D.L.; Saslow, L.R.; Kalayjian, T.; Mason, A.E.; Westman, E.C.; Sethi Dalai, S. Treating binge eating and food addiction symptoms with low-carbohydrate Ketogenic diets: A case series. J. Eat Disord. 2020, 8, 2. [Google Scholar] [CrossRef]
- Choi, H.R.; Kim, J.; Lim, H.; Park, Y.K. Two-Week Exclusive Supplementation of Modified Ketogenic Nutrition Drink Reserves Lean Body Mass and Improves Blood Lipid Profile in Obese Adults: A Randomized Clinical Trial. Nutrients 2018, 10, 1895. [Google Scholar] [CrossRef]
- Bhanpuri, N.H.; Hallberg, S.J.; Williams, P.T.; McKenzie, A.L.; Ballard, K.D.; Campbell, W.W.; McCarter, J.P.; Phinney, S.D.; Volek, J.S. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: An open label, non-randomized, controlled study. Cardiovasc. Diabetol. 2018, 17, 56. [Google Scholar] [CrossRef] [PubMed]
- Van der Louw, E.; van den Hurk, D.; Neal, E.; Leiendecker, B.; Fitzsimmon, G.; Dority, L.; Thompson, L.; Marchió, M.; Dudzińska, M.; Dressler, A.; et al. Ketogenic diet guidelines for infants with refractory epilepsy. Eur. J. Paediatr. Neurol. 2016, 20, 798–809. [Google Scholar] [CrossRef] [PubMed]
- Ułamek-Kozioł, M.; Czuczwar, S.J.; Januszewski, S.; Pluta, R. Ketogenic Diet and Epilepsy. Nutrients 2019, 11, 2510. [Google Scholar] [CrossRef] [PubMed]
- Newmaster, K.; Zhu, Z.; Bolt, E.; Chang, R.J.; Day, C.; Mhanna, A.; Paudel, S.; Farooq, O.; Swaminathan, A.; Acharya, P.; et al. A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy. Children 2022, 9, 1372. [Google Scholar] [CrossRef] [PubMed]
- Kwiterovich, P.O., Jr.; Vining, E.P.; Pyzik, P.; Skolasky, R., Jr.; Freeman, J.M. Effect of a high-fat ketogenic diet on plasma levels of lipids, lipoproteins, and apolipoproteins in children. JAMA 2003, 290, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Zamani, G.R.; Mohammadi, M.; Ashrafi, M.R.; Karimi, P.; Mahmoudi, M.; Badv, R.S.; Tavassoli, A.R.; Azizi Malamiri, R. The effects of classic ketogenic diet on serum lipid profile in children with refractory seizures. Acta Neurol. Belg. 2016, 116, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Azevedo de Lima, P.; Baldini Prudêncio, M.; Murakami, D.K.; Pereira de Brito Sampaio, L.; Figueiredo Neto, A.M.; Teixeira Damasceno, N.R. Effect of classic ketogenic diet treatment on lipoprotein subfractions in children and adolescents with refractory epilepsy. Nutrition 2017, 33, 271–277. [Google Scholar] [CrossRef]
- Liu, Y.M.; Lowe, H.; Zak, M.M.; Kobayashi, J.; Chan, V.W.; Donner, E.J. Can children with hyperlipidemia receive ketogenic diet for medication-resistant epilepsy? J. Child. Neurol. 2013, 28, 479–483. [Google Scholar] [CrossRef]
- Partsalaki, I.; Karvela, A.; Spiliotis, B.E. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2012, 25, 697–704. [Google Scholar] [CrossRef]
- Su, X.; Peng, D. Adipokines as novel biomarkers of cardio-metabolic disorders. Clin. Chim. Acta 2020, 507, 31–38. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Pascuzzi, M.C.; Magenes, V.C.; Fiore, G.; Di Profio, E.; Tenuta, E.; Bosetti, A.; Todisco, C.F.; D’Auria, E.; et al. Metabolic Derangement in Pediatric Patient with Obesity: The Role of Ketogenic Diet as Therapeutic Tool. Nutrients 2021, 13, 2805. [Google Scholar] [CrossRef] [PubMed]
- Kapetanakis, M.; Liuba, P.; Odermarsky, M.; Lundgren, J.; Hallböök, T. Effects of ketogenic diet on vascular function. Eur. J. Paediatr. Neurol. 2014, 18, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, R.; Güzel, O.; Küçük, M.; Karadeniz, C.; Katipoglu, N.; Yılmaz, Ü.; Yılmazer, M.M.; Meşe, T. The Effect of the Ketogenic Diet on the Vascular Structure and Functions in Children With Intractable Epilepsy. Pediatr. Neurol. 2016, 56, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Challa, H.J.; Bandlamudi, M.; Uppaluri, K.R. Paleolithic Diet. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Boers, I.; Muskiet, F.A.; Berkelaar, E.; Schut, E.; Penders, R.; Hoenderdos, K.; Wichers, H.J.; Jong, M.C. Favourable effects of consuming a Palaeolithic-type diet on characteristics of the metabolic syndrome: A randomized controlled pilot-study. Lipids Health Dis. 2014, 13, 160. [Google Scholar] [CrossRef] [PubMed]
- Mellberg, C.; Sandberg, S.; Ryberg, M.; Eriksson, M.; Brage, S.; Larsson, C.; Olsson, T.; Lindahl, B. Long-term effects of a Palaeolithic-type diet in obese postmenopausal women: A 2-year randomized trial. Eur. J. Clin. Nutr. 2014, 68, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Jönsson, T.; Granfeldt, Y.; Ahrén, B.; Branell, U.C.; Pålsson, G.; Hansson, A.; Söderström, M.; Lindeberg, S. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: A randomized cross-over pilot study. Cardiovasc. Diabetol. 2009, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Masharani, U.; Sherchan, P.; Schloetter, M.; Stratford, S.; Xiao, A.; Sebastian, A.; Nolte Kennedy, M.; Frassetto, L. Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. Eur. J. Clin. Nutr. 2015, 69, 944–948. [Google Scholar] [CrossRef]
- Lindeberg, S.; Jönsson, T.; Granfeldt, Y.; Borgstrand, E.; Soffman, J.; Sjöström, K.; Ahrén, B. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease. Diabetologia 2007, 50, 1795–1807. [Google Scholar] [CrossRef]
- Manheimer, E.W.; van Zuuren, E.J.; Fedorowicz, Z.; Pijl, H. Paleolithic nutrition for metabolic syndrome: Systematic review and meta-analysis. Am. J. Clin. Nutr. 2015, 102, 922–932. [Google Scholar] [CrossRef]
- Thom, T.; Haase, N.; Rosamond, W.; Howard, V.J.; Rumsfeld, J.; Manolio, T.; Zheng, Z.J.; Flegal, K.; O’Donnell, C.; Kittner, S.; et al. Heart disease and stroke statistics—2006 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2006, 113, e85–e151. [Google Scholar] [CrossRef]
- Joint WHO/FAO/UNU Expert Consultation. Protein and Amino Acid Requirements in Human Nutrition; World Health Organization: Geneva, Switzerland, 2007; Volume 35, pp. 1–265. [Google Scholar]
- Ko, G.J.; Rhee, C.M.; Kalantar-Zadeh, K.; Joshi, S. The Effects of High-Protein Diets on Kidney Health and Longevity. J. Am. Soc. Nephrol. 2020, 31, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Nan, F.; Wang, L.Y.; Jiang, H.; Chen, W.; Jiang, Y. Effects of high-protein diet on glycemic control, insulin resistance and blood pressure in type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. 2020, 39, 1724–1734. [Google Scholar] [CrossRef] [PubMed]
- Tettamanzi, F.; Bagnardi, V.; Louca, P.; Nogal, A.; Monti, G.S.; Mambrini, S.P.; Lucchetti, E.; Maestrini, S.; Mazza, S.; Rodriguez-Mateos, A.; et al. A High Protein Diet Is More Effective in Improving Insulin Resistance and Glycemic Variability Compared to a Mediterranean Diet-A Cross-Over Controlled Inpatient Dietary Study. Nutrients 2021, 13, 4380. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, L.; Perla, F.M.; Roggini, M.; Andreoli, G.; D’Avanzo, M.; Chiesa, C. A Systematic Review of NAFLD-Associated Extrahepatic Disorders in Youths. J. Clin. Med. 2019, 8, 868. [Google Scholar] [CrossRef]
- Campos-Nonato, I.; Hernandez, L.; Barquera, S. Effect of a High-Protein Diet versus Standard-Protein Diet on Weight Loss and Biomarkers of Metabolic Syndrome: A Randomized Clinical Trial. Obes. Facts 2017, 10, 238–251. [Google Scholar] [CrossRef] [PubMed]
- Dorenbos, E.; Drummen, M.; Adam, T.; Rijks, J.; Winkens, B.; Martínez, J.A.; Navas-Carretero, S.; Stratton, G.; Swindell, N.; Stouthart, P.; et al. Effect of a high protein/low glycaemic index diet on insulin resistance in adolescents with overweight/obesity-A PREVIEW randomized clinical trial. Pediatr. Obes. 2021, 16, e12702. [Google Scholar] [CrossRef]
- Zadi, V.; Esmaillzadeh, A.; Hashemipour, M.; Surkan, P.J.; Azadbakht, L.; Kelishadi, R. High protein diets do not affect anthropometric indexes and cardiometabolic risk factors among children with excess weight: A randomized controlled trial. J. Cardiovasc. Thorac. Res. 2018, 10, 95–103. [Google Scholar] [CrossRef]
- Jiang, Y.F.; Wang, M.Y.; Zhang, J.D. Effects of high protein diet on anthropometric indices and blood lipid in overweight and obese children: A Meta-analysis. Chin. J. Pediatr. 2022, 60, 426–434. (In Chinese) [Google Scholar] [CrossRef]
- Shikany, J.M.; Safford, M.M.; Soroka, O.; Brown, T.M.; Newby, P.K.; Durant, R.W.; Judd, S.E. Mediterranean Diet Score, Dietary Patterns, and Risk of Sudden Cardiac Death in the REGARDS Stud. J. Am. Heart Assoc. 2021, 10, e019158. [Google Scholar] [CrossRef]
| Type of Study | Population | Results | Author |
|---|---|---|---|
| Cross-sectional study | 63 vegetarians, 52 vegans and 72 omnivores after having followed the respective diet for at least 1 year (healthy children) 5–10 years | Compared to the omnivore group, the vegan and vegetarian group was leaner, with lower levels of HDL-, LDL- and Total-cholesterol, but also shorter, with lower BMC and blood levels of vitamin B12 and D. | Desmond MA 2021 [34] |
| Cross-sectional study | 139 vegetarians, 127 vegans and 164 omnivores (healthy children) 1–3 years | Significant differences in macronutrient intake: protein, fat, added sugars (OM > VG > VN). Carbohydrates and fiber (VN > VG > OM). No significant differences in energy intake or density and anthropometrics. | Weder S 2019 [66] |
| Cross-sectional study | 149 vegetarians, 115 vegans and 137 omnivores (healthy children) 6–18 years | Significant differences in macronutrient intake: protein (OM > VN > VG). Carbohydrates (VN > VG > OM). Fat (OM > VN > VG). VG showed the lowest LDL-C and non-HDL-C concentrations compared with VN and OM. No significant differences were found in HDL-C, triglycerides and energy intake. | Alexy U 2021 [67] |
| Cross-sectional study | Omnivores 24, vegetarians 10, vegans 6 who followed their respective diets from birth <4 years (median age 3.5 years old) | Vegans had significantly lower plasma HDL-C, LDL-C and total cholesterol levels than the omnivore group, with a median total cholesterol level of 2.85 mmol/L. | Hovinen T 2021 [68] |
| 4-week prospective randomized trial | 16 vegans, 14 AHA diet hypercholesterolemic and obese children 9–18 years | Children on PB had 9 and children on AHA had 4 statistically significant (p < 0.05) beneficial changes from baseline (mean decreases): BMI Z-scorePB (−0.14), systolic blood pressurePB (−6.43 mm Hg), total cholesterolPB (−22.5 mg/dL), LDLPB (−13.14 mg/dL), hsCRPPB (−2.09 mg/L), insulinPB (−5.42 μU/mL), myeloperoxidasePB/AHA (−75.34/69.23 pmol/L), mid-arm circumferencePB/AHA (−2.02/−1.55 cm), weightPB/AHA (−3.05/ −1.14 kg) and waist circumferenceAHA (−2.96 cm). | Macknin M 2015 [69] |
| 52-week prospective randomized trial | 32 vegans, 32 AHA diet, 32 MED diet, hypercholesterolemic and obese children 9–18 years | Similar statistically significant (p < 0.05 to <0.001) improvements were found in all groups in the CVD risk markers: low-density lipoprotein, myeloperoxidase (MPO), total cholesterol, weight, systolic and diastolic blood pressure. The stabilization of BMI-for-age among participants was also observed. No significant changes in hsCRP, HDL and insulin were detected during the study in all study groups | Macknin M 2021 [70] |
| Type of Study | Population | Results | Author |
|---|---|---|---|
| Randomized controlled trial | 834 children randomly received their usual packed lunch brought from home (control) or the ND school meal over two 3-month periods 8–11 years | During the ND period, children had higher intakes of fish, vegetable, cheese, potatoes, eggs and beverages (excluding milk) and lower intakes of fats (less saturated fat), bread and other cereal products than in the control period (all, p < 0.05). | Andersen 2014 [109] |
| Randomized controlled trial | 726 children randomly received their usual packed lunch brought from home (control) or the ND school meal over a 3-month period 8–11 years | Both baseline EPA + DHA status and the intervention-induced increase in EPA + DHA status was positively associated with school performance. Those who had consumed fish had higher DHA and EPA status (both p < 0.001) and lower n-6:n-3 PUFA ratio (p < 0.001). | Sørensen 2015 [110] |
| Cross-sectional study based on data from a large prospective cohort study | 14.989 children <8 years | In final analysis, child ND adherence up to 7 years of age was not associated with odds of overweight at 8 years after adjusting for potential confounders. | Agnihotri 2021 [112] |
| Cross-sectional study | 960 partecipants born in 1934–1944 | Benefits on SBP and PP can be achieved through ND and the effects are greater among individuals with low birth weight. | Meinilä 2021 [116] |
| Cross-sectional study | 4–18-year-old children with (n = 114) and without (n = 145) FH who followed Nordic and Mediterranean pattern diets | An impact of diet on lipid alterations in children with FH cannot be excluded, even though these are due to a genetic defect. | Rodríguez-Borjabad et al. 2021 [117] |
| Dietary Pattern | Main Characteristics | Main Effects in Adult Subjects | Main Effects in Pediatric Subjects |
|---|---|---|---|
| Mediterranean Diet |
|
|
|
| Plant based Diet |
|
|
|
| DASH Diet |
|
|
|
| Nordic Diet |
|
|
|
| Low-carb Diet |
|
|
|
| Ketogenic Diet |
|
|
|
| Paleolithic Diet |
|
|
|
| High Protein Diet |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capra, M.E.; Monopoli, D.; Decarolis, N.M.; Giudice, A.; Stanyevic, B.; Esposito, S.; Biasucci, G. Dietary Models and Cardiovascular Risk Prevention in Pediatric Patients. Nutrients 2023, 15, 3664. https://doi.org/10.3390/nu15163664
Capra ME, Monopoli D, Decarolis NM, Giudice A, Stanyevic B, Esposito S, Biasucci G. Dietary Models and Cardiovascular Risk Prevention in Pediatric Patients. Nutrients. 2023; 15(16):3664. https://doi.org/10.3390/nu15163664
Chicago/Turabian StyleCapra, Maria Elena, Delia Monopoli, Nicola Mattia Decarolis, Antonella Giudice, Brigida Stanyevic, Susanna Esposito, and Giacomo Biasucci. 2023. "Dietary Models and Cardiovascular Risk Prevention in Pediatric Patients" Nutrients 15, no. 16: 3664. https://doi.org/10.3390/nu15163664
APA StyleCapra, M. E., Monopoli, D., Decarolis, N. M., Giudice, A., Stanyevic, B., Esposito, S., & Biasucci, G. (2023). Dietary Models and Cardiovascular Risk Prevention in Pediatric Patients. Nutrients, 15(16), 3664. https://doi.org/10.3390/nu15163664








