A Breastfeeding Relaxation Intervention Promotes Growth in Late Preterm and Early Term Infants: Results from a Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
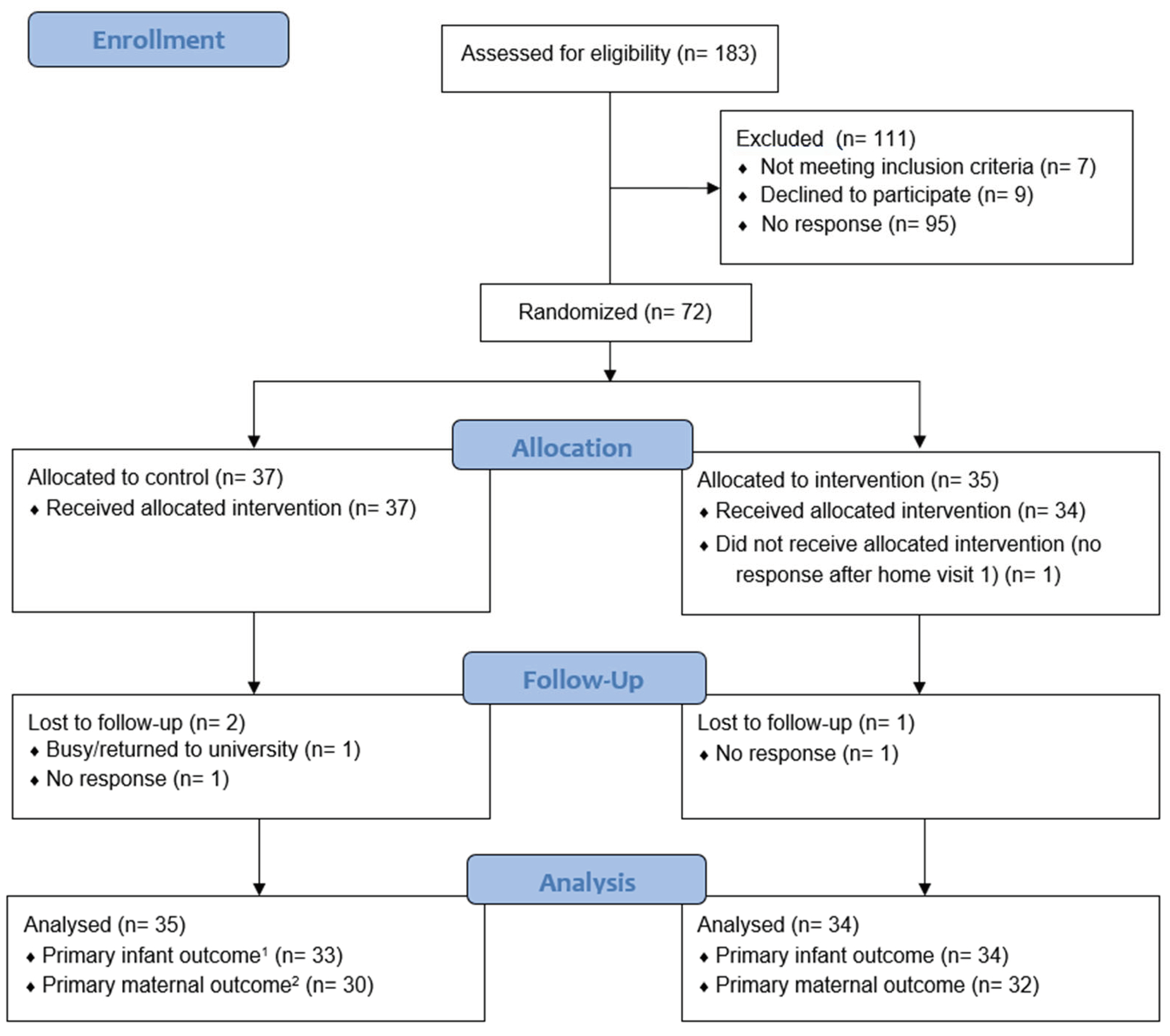
2.1. Study Participants and Design
2.2. Randomization and Masking
2.3. Data Collection
2.4. Changes to Study Methods Due to COVID-19 Pandemic
2.5. Data Analysis
3. Results
3.1. Primary Outcomes
3.2. Secondary Outcomes
3.3. Further Exploratory Analysis
3.4. Dose-Response Associations
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davidoff, M.J.; Dias, T.; Damus, K.; Russell, R.; Bettegowda, V.R.; Dolan, S.; Schwarz, R.H.; Green, N.S.; Petrini, J. Changes in the gestational age distribution among US singleton births: Impact on rates of late preterm birth, 1992 to 2002. Semin. Perinatol. 2006, 30, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.L.; Dorer, D.J.; Fleming, M.P.; Catlin, E.A. Clinical outcomes of near-term infants. Pediatrics 2004, 114, 372–376. [Google Scholar] [CrossRef]
- Zanardo, V.; Gambina, I.; Begley, C.; Litta, P.; Cosmi, E.; Giustardi, A.; Trevisanuto, D. Psychological distress and early lactation performance in mothers of late preterm infants. Early Hum. Dev. 2011, 87, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Engle, W.A. Morbidity and mortality in late preterm and early term newborns: A continuum. Clin. Perinatol. 2011, 38, 493–516. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.K.; Speechley, K.N.; Macnab, J.; Natale, R.; Campbell, M.K. Neonatal morbidity associated with late preterm and early term birth: The roles of gestational age and biological determinants of preterm birth. Int. J. Epidemiol. 2014, 43, 802–814. [Google Scholar] [CrossRef]
- Lapillonne, A.; Bronsky, J.; Campoy, C.; Embleton, N.; Fewtrell, M.; Fidler Mis, N.; Gerasimidis, K.; Hojsak, I.; Hulst, J.; Indrio, F.; et al. Feeding the Late and Moderately Preterm Infant: A Position Paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 259–270. [Google Scholar] [CrossRef]
- Victora, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Hackman Nicole, M.; Kjerulff Kristen, H. Reduced breastfeeding rates in firstborn late preterm and early term infants. Breastfeed. Med. 2016, 11, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.K.; Attanasio, L.B.; Kozhimannil, K.B. Hospital care and early breastfeeding outcomes among late preterm, early-term, and term infants. Birth 2014, 41, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Boyle, E.M.; Johnson, S.; Manktelow, B.; Seaton, S.E.; Draper, E.S.; Smith, L.K.; Dorling, J.; Marlow, N.; Petrou, S.; Field, D.J. Neonatal outcomes and delivery of care for infants born late preterm or moderately preterm: A prospective population-based study. Arch. Dis. Child. Fetal. Neonatal. Ed. 2015, 100, F479–F485. [Google Scholar] [CrossRef]
- Carpay, N.C.; Kakaroukas, A.; Embleton, N.D.; van Elburg, R.M. Barriers and Facilitators to Breastfeeding in Moderate and Late Preterm Infants: A Systematic Review. Breastfeed. Med. 2021, 16, 370–384. [Google Scholar] [CrossRef] [PubMed]
- Cartwright, J.; Atz, T.; Newman, S.; Mueller, M.; Demirci, J.R. Integrative Review of Interventions to Promote Breastfeeding in the Late Preterm Infant. J. Obs. Gynecol. Neonatal Nurs. 2017, 46, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Dib, S.; Kittisakmontri, K.; Wells, J.C.; Fewtrell, M. Interventions to Improve Breastfeeding Outcomes in Late Preterm and Early Term Infants. Breastfeed Med 2022, 17, 781–792. [Google Scholar] [PubMed]
- Keith, D.R.; Weaver, B.S.; Vogel, R.L. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Adv. Neonat. Care 2012, 12, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Feher, S.D.; Berger, L.R.; Johnson, J.D.; Wilde, J.B. Increasing breast milk production for premature infants with a relaxation/imagery audiotape. Pediatrics 1989, 83, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Mohd Shukri, N.H.; Wells, J.; Eaton, S.; Mukhtar, F.; Petelin, A.; Jenko-Pražnikar, Z.; Fewtrell, M. Randomized controlled trial investigating the effects of a breastfeeding relaxation intervention on maternal psychological state, breast milk outcomes, and infant behavior and growth. Am. J. Clin. Nutr. 2019, 110, 121–130. [Google Scholar] [CrossRef]
- Trivers, R.L. Parent-offspring conflict. Integr. Comp. Biol. 1974, 14, 249–264. [Google Scholar] [CrossRef]
- Hill, K. Life history theory and evolutionary anthropology. Evol. Anthropol. Issues News Rev. 1993, 2, 78–88. [Google Scholar] [CrossRef]
- Wells, J.C.; Cole, T.J.; Cortina-Borja, M.; Sear, R.; Leon, D.A.; Marphatia, A.A.; Murray, J.; Wehrmeister, F.C.; Oliveira, P.D.; Gonçalves, H. Low maternal capital predicts life history trade-offs in daughters: Why adverse outcomes cluster in individuals. Front. Public Health 2019, 7, 206. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.; Nesse, R.M.; Sear, R.; Johnstone, R.A.; Stearns, S.C. Evolutionary public health: Introducing the concept. Lancet 2017, 390, 500–509. [Google Scholar] [CrossRef]
- Dib, S.; Wells, J.C.K.; Fewtrell, M. Mother And late Preterm Lactation Study (MAPLeS): A randomised controlled trial testing the use of a breastfeeding meditation by mothers of late preterm infants on maternal psychological state, breast milk composition and volume, and infant behaviour and growth. Trials 2020, 21, 318. [Google Scholar] [PubMed]
- Dib, S.; Wells, J.C.K.; Fewtrell, M. A within-subject comparison of different relaxation therapies in eliciting physiological and psychological changes in young women. PeerJ 2020, 8, e9217. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Altman, D.; Purwar, M.; Noble, J.; Knight, H.; Ruyan, P.; Cheikh Ismail, L.; Barros, F.; Lambert, A.; Papageorghiou, A. The objectives, design and implementation of the INTERGROWTH-21st Project. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 9–26. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Leerkes, E.; Qu, J. The Maternal (Non) Responsiveness Questionnaire: Initial Factor Structure and Validation. Infant Child Dev. 2017, 26, e1992. [Google Scholar] [CrossRef]
- Muller, M.E. A questionnaire to measure mother-to-infant attachment. J. Nurs. Meas. 1994, 2, 129–141. [Google Scholar] [CrossRef]
- Llewellyn, C.H.; van Jaarsveld, C.H.; Johnson, L.; Carnell, S.; Wardle, J. Development and factor structure of the Baby Eating Behaviour Questionnaire in the Gemini birth cohort. Appetite 2011, 57, 388–396. [Google Scholar] [CrossRef]
- Barr, R.G.; Kramer, M.S.; Boisjoly, C.; McVey-White, L.; Pless, I.B. Parental diary of infant cry and fuss behaviour. Arch. Dis. Child 1988, 63, 380–387. [Google Scholar] [CrossRef]
- Estevez-Gonzalez, A.; Kulisevsky, J.; Boltes, A.; Otermin, P.; Garcia-Sanchez, C. Rey verbal learning test is a useful tool for differential diagnosis in the preclinical phase of Alzheimer’s disease: Comparison with mild cognitive impairment and normal aging. Int. J. Geriatr. Psychiatry 2003, 18, 1021–1028. [Google Scholar] [CrossRef]
- Reilly, J.J.; Ashworth, S.; Wells, J.C. Metabolisable energy consumption in the exclusively breast-fed infant aged 3–6 months from the developed world: A systematic review. Br. J. Nutr. 2005, 94, 56–63. [Google Scholar] [CrossRef]
- Fenton, T.R.; Anderson, D.; Groh-Wargo, S.; Hoyos, A.; Ehrenkranz, R.A.; Senterre, T. An attempt to standardize the calculation of growth velocity of preterm infants—Evaluation of practical bedside methods. J. Pediatr. 2018, 196, 77–83. [Google Scholar] [CrossRef]
- Ong, K.K.; Ahmed, M.L.; Emmett, P.M.; Preece, M.A.; Dunger, D.B. Association between postnatal catch-up growth and obesity in childhood: Prospective cohort study. BMJ 2000, 320, 967–971. [Google Scholar] [CrossRef]
- Varişoğlu, Y.; Güngör Satilmiş, I. The Effects of Listening to Music on Breast Milk Production by Mothers of Premature Newborns in the Neonatal Intensive Care Unit: A Randomized Controlled Study. Breastfeed. Med. 2020, 15, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Jayamala, A.; Lakshmanagowda, P.B.; Pradeep, G.; Goturu, J. Impact of music therapy on breast milk secretion in mothers of premature newborns. J. Clin. Diagn. Res. JCDR 2015, 9, CC04. [Google Scholar]
- Mizuhata, K.; Taniguchi, H.; Shimada, M.; Hikita, N.; Morokuma, S. Effects of Breastfeeding on Stress Measured by Saliva Cortisol Level and Perceived Stress. Asian/Pac. Isl. Nurs. J. 2020, 5, 128. [Google Scholar] [CrossRef] [PubMed]
- Joëls, M.; Krugers, H.J. LTP after stress: Up or down? Neural Plast. 2007, 2007, 093202. [Google Scholar] [CrossRef]
- Lupien, S.J.; Maheu, F.; Tu, M.; Fiocco, A.; Schramek, T.E. The effects of stress and stress hormones on human cognition: Implications for the field of brain and cognition. Brain Cogn. 2007, 65, 209–237. [Google Scholar] [CrossRef] [PubMed]
- Wirth, M.M. Hormones, stress, and cognition: The effects of glucocorticoids and oxytocin on memory. Adapt. Hum. Behav. Physiol. 2015, 1, 177–201. [Google Scholar] [CrossRef] [PubMed]
- Thureen, P.J.; Phillips, R.E.; Baron, K.A.; DeMarie, M.P.; Hay, W.W., Jr. Direct measurement of the energy expenditure of physical activity in preterm infants. J. Appl. Physiol. 1998, 85, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.K.; Davies, P.S.W. Relationship between behavior and energy expenditure in 12-week-old infants. Am. J. Hum. Biol. Off. J. Hum. Biol. Counc. 1996, 8, 465–472. [Google Scholar] [CrossRef]
- Manser, M.B.; Avey, G. The effect of pup vocalisations on food allocation in a cooperative mammal, the meerkat (Suricata suricatta). Behav. Ecol. Sociobiol. 2000, 48, 429–437. [Google Scholar] [CrossRef]
- Weary, D.M.; Fraser, D. Calling by domestic piglets: Reliable signals of need? Anim. Behav. 1995, 50, 1047–1055. [Google Scholar] [CrossRef][Green Version]
- Smith, H.G.; Montgomerie, R. Nestling American robins compete with siblings by begging. Behav. Ecol. Sociobiol. 1991, 29, 307–312. [Google Scholar] [CrossRef]
- Kilner, R. When do canary parents respond to nestling signals of need? Proc. R. Soc. Lond. Ser. B Biol. Sci. 1995, 260, 343–348. [Google Scholar]
| Whole Sample (n = 69) | Control (n = 35) | Relaxation (n = 34) | |
|---|---|---|---|
| Maternal age, years (mean ± SD) | 33.1 ± 4.9 | 34.0 ± 4.8 | 32.3 ± 5.0 |
| Infant gestation, weeks (mean ± SD) | 36.5 ± 1.0 | 36.7 ± 1.1 | 36.3 ± 0.9 |
| Birth weight, kg (mean ± SD) | 2.6 ± 0.4 | 2.7 ± 0.4 | 2.6 ± 0.4 |
| Male infant (n, %) | 42 (60.9) | 19 (54.3) | 23 (67.6) |
| Primiparous (n, %) | 47 (68.1) | 23 (65.7) | 24 (70.6) |
| Breastfeeding plan, months (mean ± SD) | 9.7 ± 4.7 | 9.9 ± 5.8 | 9.4 ± 3.4 |
| Late Preterm Infants 1 (n, %) | 48 (69.6) | 22 (62.9) | 26 (76.5) |
| Maternal Ethnicity (n, %) | |||
| White | 38 (55.1) | 19 (54.3) | 19 (55.9) |
| Mixed/Multiple ethnic groups | 2 (2.9) | 1 (2.9) | 1 (2.9) |
| Black/African/Caribbean/Black British | 11 (15.9) | 7 (20.0) | 4 (11.8) |
| Asian/Asian British | 12 (17.4) | 5 (14.3) | 7 (20.6) |
| Arab | 3 (4.3) | 1 (2.9) | 2 (5.9) |
| Other ethnic group | 3 (4.3) | 2 (5.7) | 1 (2.9) |
| Maternal education (n, %) | |||
| ≤5 GCSE A-C grade | 3 (4.2) | 1 (3.2) | 2 (6.3) |
| A levels//equivalent | 10 (14.5) | 5 (16.1) | 5 (15.6) |
| Bachelor’s degree | 25 (36.2) | 11 (35.5) | 14 (43.8) |
| Master’s degree | 15 (21.7) | 11 (35.5) | 4 (12.5) |
| PhD/professional qualification | 10 (14.5) | 3 (9.7) | 7 (21.9) |
| Marital Status (n, %) | |||
| Married/Civil Partnership/Cohabitation | 55 (79.7) | 29 (87.9) | 26 (78.8) |
| Single parent- living on own | 4 (5.8) | 2 (6.1) | 2 (6.1) |
| Single parent- living with family | 6 (8.7) | 1 (3.0) | 5 (15.2) |
| Divorced | 1 (1.4) | 1 (3.0) | 0 (0.0) |
| Household income (n, %) | |||
| <£20–30 K | 18 (28.6) | 8 (26.7) | 10 (30.3) |
| <£45 K–75 K | 14 (22.2) | 8 (26.7) | 6 (18.2) |
| <£100 K | 12 (19.0) | 6 (17.1) | 6 (18.2) |
| >£100 K | 19 (30.2) | 8 (26.7) | 11 (33.3) |
| Control Group (n = 35) | Intervention Group (n = 34) | |
|---|---|---|
| Did not attend breastfeeding classes (n, %) | 22 (62.9) | 23 (67.6) |
| Type of Delivery (n, %) | ||
| Vaginal- not induced | 10 (28.6) | 12 (35.3) |
| Vaginal- induced | 8 (22.9) | 5 (14.7) |
| C-section- planned or elective | 3 (8.6) | 2 (5.9) |
| C-section- emergency or unplanned | 14 (40.0) | 15 (44.1) |
| Skin-to-Skin: How Soon (n, %) | ||
| Did not have skin-to-skin | 5 (14.3) | 8 (23.5) |
| Directly | 16 (45.7) | 16 (47.1) |
| Within 30 min after birth | 4 (11.4) | 4 (11.8) |
| More than 30 min after birth | 6 (17.1) | 4 (11.8) |
| More than 1 h after birth | 4 (11.4) | 2 (5.9) |
| Skin-to-Skin: How Long (n, %) | ||
| Did not have skin-to-skin | 5 (14.3) | 8 (23.5) |
| Less than 30 min | 14 (40.0) | 16 (47.1) |
| Between 30 to 60 min | 8 (22.9) | 4 (11.8) |
| More than 1 h | 8 (22.9) | 6 (17.6) |
| Breastfeeding Initiation: How Soon (n, %) | ||
| Less than 30 min after birth | 6 (17.1) | 9 (26.5) |
| More than 30 min after birth | 29 (82.9) | 25 (73.5) |
| Mother and Infant Rooming-In (n, %) | ||
| Did not room-in at all | 2 (5.7) | 3 (8.8) |
| Sometimes | 6 (17.1) | 7 (20.6) |
| At all times | 27 (77.1) | 24 (70.6) |
| Hospital Stay | ||
| Admitted to NICU (n, %) | 7 (20.0) | 11 (32.4) |
| Length of stay at NICU (median [range]) | 5.0 [1,2,3,4,5,6,7,8,9,10,11,12,13,14] | 5.0 [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] |
| Length of hospital stay (median [range]) | 4.0 [1,2,3,4,5,6,7,8,9,10,11,12,13] | 4.0 [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] |
| Supplementation | ||
| Did not supplement infant formula (n, %) | 5 (14.3) | 12 (35.3) |
| <30 mL per feed, on average (n, %) | 21 (60.0) | 13 (38.2) |
| 30–60 mL per feed, on average (n, %) | 9 (25.7) | 9 (26.5) |
| Times/day expressed breast milk (mean ± SD) | 2.5 ± 3.8 | 2.8 ± 3.4 |
| Support | ||
| Offered support for feeding problems | 28 (80.0) | 26 (76.5) |
| Received enough help with feeding | 20 (58.8) | 23 (67.6) |
| Given details of community support groups | 30 (85.7) | 32 (94.1) |
| Control Group | Relaxation Group | p-Value 1 | MD | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Primary Maternal Outcomes | n | Mean ± SD | n | Mean ± SD | |||
| Perceived Stress HV1 2 | 31 | 15.2 ± 5.2 | 33 | 14.8 ± 5.8 | 0.8 | −0.4 | −3.2, 2.4 |
| Perceived Stress HV2 | 34 | 13.7 ± 5.0 | 33 | 12.0 ± 5.5 | 0.2 | −1.7 | −4.3, 0.9 |
| Change Stress | 30 | −2.7 ± 5.0 | 32 | −2.9 ± 5.3 | 0.9 | −0.2 | −2.8, 2.4 |
| Primary Infant Outcome | |||||||
| Weight Z-Score HV1 | 35 | −0.32 ± 0.95 | 35 | −0.37 ± 0.89 | 0.9 | −0.09 | −0.50, 0.40 |
| Weight Z-Score HV2 | 35 | 0.07 ± 0.97 | 34 | 0.43 ± 0.79 | 0.1 | 0.37 | −0.06, 0.80 |
| Change Weight Z-Score | 33 | 0.37 ± 0.61 | 34 | 0.77 ± 0.66 | 0.01 | 0.40 | 0.09, 0.71 |
| Control Group | Relaxation Group | p-Value 1 | MD | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Psychological State | n | Mean ± SD | n | Mean ± SD | |||
| Depression score HV1 2 | 27 | 7.6 ± 4.7 | 31 | 7.8 ± 4.4 | 0.8 | 0.2 | −2.2, 2.6 |
| Depression score HV2 | 30 | 6.5 ± 3.8 | 31 | 6.2 ± 4.2 | 0.8 | −0.3 | −2.4, 1.8 |
| Change in Depression score | 24 | −2.0 ± 3.2 | 30 | −1.5 ± 3.4 | 0.6 | 0.5 | −1.3, 2.3 |
| Salivary Cortisol (ug/dL) | |||||||
| Cortisol HV1 | 25 | 0.15 ± 0.07 | 26 | 0.22 ± 0.13 | 0.03 | 0.07 | 0.01, 0.13 |
| Cortisol HV2 | 24 | 0.16 ± 0.08 | 25 | 0.18 ± 0.07 | 0.5 | 0.02 | −0.02, 0.06 |
| Change in Cortisol | 20 | 0.05 ± 0.13 | 21 | −0.03 ± 0.10 | 0.03 | −0.08 | −0.15, −0.01 |
| Responsiveness and Attachment | |||||||
| Responsiveness HV1 | 25 | 4.3 ± 0.5 | 28 | 4.2 ± 0.5 | 0.7 | −0.1 | −0.4, 0.2 |
| Responsiveness HV2 | 22 | 4.2 ± 0.3 | 27 | 4.2 ± 0.4 | 0.7 | 0.0 | −0.2, 0.2 |
| Delayed Responsiveness HV1 | 25 | 2.3 ± 0.9 | 28 | 2.5 ± 0.7 | 0.5 | 0.2 | −0.2, 0.6 |
| Delayed Responsiveness HV2 | 22 | 2.7 ± 0.9 | 27 | 2.5 ± 0.7 | 0.5 | −0.2 | −0.7, 0.3 |
| Non-Responsiveness HV1 | 25 | 1.1 ± 0.3 | 28 | 1.1 ± 0.3 | 0.7 | −0.04 | −0.2, 0.1 |
| Non-Responsiveness HV2 | 22 | 1.1 ± 0.2 | 27 | 1.0 ± 0.1 | 0.2 | −0.05 | −0.1, 0.03 |
| Maternal Attachment HV1 | 23 | 70.9 ± 8.1 | 30 | 71.6 ± 6.4 | 0.7 | 0.7 | −3.3, 4.7 |
| Maternal Attachment HV2 | 21 | 71.9 ± 4.2 | 27 | 73.2 ± 4.4 | 0.3 | 1.2 | −1.3, 3.8 |
| Verbal Memory (words) | |||||||
| Immediate Recall HV1 | 31 | 54.3 ± 7.0 | 30 | 56.1 ± 5.5 | 0.3 | 1.8 | −1.4, 5.0 |
| Immediate Recall HV2 | 25 | 59.2 ± 6.3 | 28 | 61.4 ± 6.2 | 0.2 | 2.2 | −1.3, 5.6 |
| Verbal Learning HV1 | 31 | 5.8 ± 1.9 | 30 | 6.1 ± 1.8 | 0.6 | 0.3 | −0.6, 1.3 |
| Verbal Learning HV2 | 25 | 3.5 ± 1.9 | 28 | 4.6 ± 1.8 | 0.04 | 1.1 | 0.04, 2.1 |
| Verbal Forgetting HV1 | 31 | −1.7 ± 1.7 | 30 | −1.3 ± 1.8 | 0.4 | 0.4 | −0.5, 1.3 |
| Verbal Forgetting HV2 | 25 | −0.4 ± 1.6 | 28 | −1.0 ± 1.0 | 0.1 | −0.6 | −1.3, 0.2 |
| Control Group | Relaxation Group | p-Value 1 | MD | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Breast Milk Composition | n | Mean ± SD | n | Mean ± SD | |||
| Fat HV1 2 (g/100 mL) | 30 | 4.0 ± 1.0 | 29 | 3.6 ± 1.0 | 0.1 | −0.4 | −0.9, 0.1 |
| Fat HV2 (g/100 mL) | 28 | 4.1 ± 1.1 | 28 | 4.0 ± 1.2 | 0.7 | −0.1 | −0.8, 0.5 |
| Change Fat | 25 | 0.05 ± 1.3 | 22 | 0.4 ± 1.6 | 0.5 | 0.3 | −0.6, 1.2 |
| Protein HV1 (g/100 mL) | 30 | 1.2 ± 0.3 | 29 | 1.1 ± 0.2 | 0.03 | −0.1 | −0.2, −0.01 |
| Protein HV2 (g/100 mL) | 28 | 1.0 ± 0.2 | 28 | 0.9 ± 0.2 | 0.07 | −0.1 | −0.2, 0.01 |
| Change Protein | 25 | −0.3 ± 0.2 | 22 | −0.3 ± 0.1 | 0.8 | 0.01 | −0.07, 0.1 |
| Carbohydrates HV1 (g/100 mL) | 30 | 7.2 ± 0.3 | 29 | 7.2 ± 0.4 | 0.4 | 0.08 | −0.1, 0.3 |
| Carbohydrates HV2 (g/100 mL) | 28 | 7.2 ± 0.4 | 28 | 7.3 ± 0.3 | 0.4 | 0.08 | −0.1, 0.3 |
| Change Carbohydrates | 25 | 0.04 ± 0.3 | 22 | 0.2 ± 0.4 | 0.07 | 0.2 | −0.01, 0.4 |
| Energy HV1 (kcal/100 mL) | 30 | 72.8 ± 9.7 | 29 | 68.7 ± 8.7 | 0.09 | −4.1 | −8.9, 0.7 |
| Energy HV2 (kcal/100 mL) | 28 | 72.7 ± 10.1 | 28 | 71.2 ± 11.0 | 0.6 | −1.5 | −7.2, 4.2 |
| Change Energy | 25 | −0.6 ± 12.6 | 22 | 2.9 ± 14.9 | 0.4 | 3.5 | −4.5, 11.6 |
| Direct Breast Milk Intake | |||||||
| Volume-Test Weighing HV1 | 7 | 419 ± 270 | 10 | 347 ± 168 | 0.6 | −72 | −297, 154 |
| Volume- Test Weighing HV2 | 4 | 439 ± 163 | 3 | 623 ± 194 | 0.2 | 184 | −162, 530 |
| Change Volume-Test Weighing | 4 | 88 ± 451 | 1 | 320 | 0.7 | ||
| Volume- 24 h Diary HV1 | 11 | 501 ± 269 | 14 | 511 ± 251 | 0.9 | 10 | −205, 226 |
| Volume- 24 h Diary HV2 | 9 | 388 ± 250 | 9 | 519 ± 201 | 0.2 | 131 | −96, 358 |
| Change Volume- BF Diary | 5 | −125 ± 136 | 6 | −0.5 ± 82 | 0.1 | 125 | −25, 274 |
| Feeding Patterns | |||||||
| Breastfeeding Frequency HV1 | 13 | 7.5 ± 5.0 | 14 | 8.7 ± 2.5 | 0.4 | 1.2 | −1.9, 4.3 |
| Breastfeeding Frequency HV2 | 9 | 5.9 ± 3.0 | 9 | 9.8 ± 3.0 | 0.01 | 3.9 | 0.9, 6.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dib, S.; Wells, J.C.K.; Eaton, S.; Fewtrell, M. A Breastfeeding Relaxation Intervention Promotes Growth in Late Preterm and Early Term Infants: Results from a Randomized Controlled Trial. Nutrients 2022, 14, 5041. https://doi.org/10.3390/nu14235041
Dib S, Wells JCK, Eaton S, Fewtrell M. A Breastfeeding Relaxation Intervention Promotes Growth in Late Preterm and Early Term Infants: Results from a Randomized Controlled Trial. Nutrients. 2022; 14(23):5041. https://doi.org/10.3390/nu14235041
Chicago/Turabian StyleDib, Sarah, Jonathan C. K. Wells, Simon Eaton, and Mary Fewtrell. 2022. "A Breastfeeding Relaxation Intervention Promotes Growth in Late Preterm and Early Term Infants: Results from a Randomized Controlled Trial" Nutrients 14, no. 23: 5041. https://doi.org/10.3390/nu14235041
APA StyleDib, S., Wells, J. C. K., Eaton, S., & Fewtrell, M. (2022). A Breastfeeding Relaxation Intervention Promotes Growth in Late Preterm and Early Term Infants: Results from a Randomized Controlled Trial. Nutrients, 14(23), 5041. https://doi.org/10.3390/nu14235041





