Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age
Abstract
1. Introduction
1.1. Background
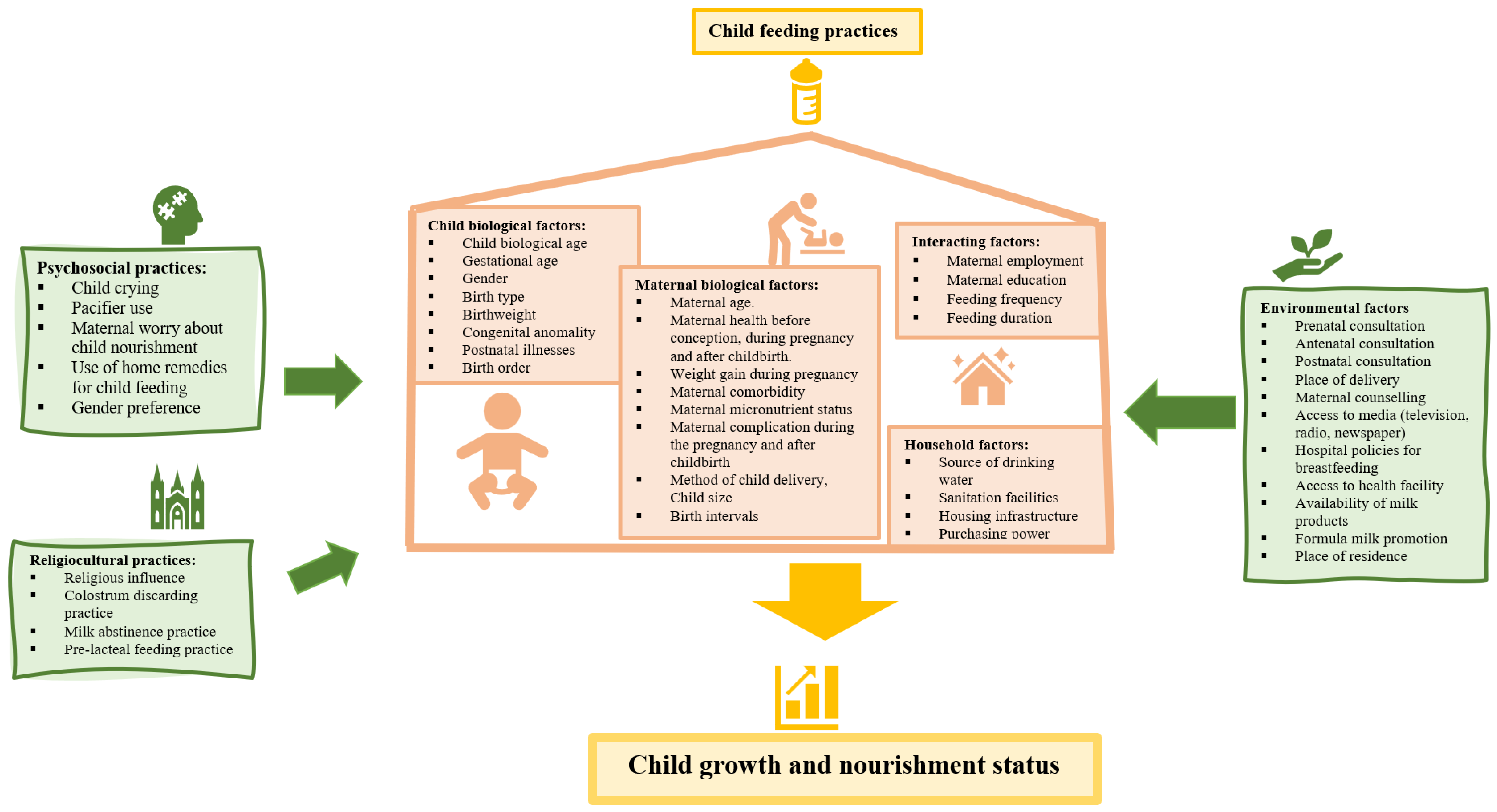
1.2. Conceptual Framework
2. Methodology
2.1. Datasets
2.2. Study Population, Sample Size, and Sampling Method
2.3. Measurement of Outcome Variables
2.4. Measurement of Independent Variables
2.5. Covariates
2.6. Data Management and Data Analysis
2.7. Ethical Clearance
3. Results
3.1. Health, Demographic, and Feeding Profile of the Study Sample
3.2. Associations between Feeding Indicators and CFM
3.2.1. Association of Continuation of Breastfeeding with CFM
3.2.2. Association of Predominant Feeding with CFM
3.2.3. Association of Solid, Semi-Solid, and Soft Foods with CFM
3.3. Associations between Feeding Practices and Coexisting Forms of Malnutrition
4. Discussion
5. Study Strength and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khaliq, A.; Qamar, M.; Hussaini, S.A.; Azam, K.; Zehra, N.; Hussain, M.; Jaliawala, H.A. Assessment of knowledge and practices about breastfeeding and weaning among working and non-working mothers. J. Pak. Med. Assoc. 2017, 67, 332–338. [Google Scholar]
- Di Benedetto, M.G.; Bottanelli, C.; Cattaneo, A.; Pariante, C.M.; Borsini, A. Nutritional and immunological factors in breast milk: A role in the intergenerational transmission from maternal psychopathology to child development. Brain Behav. Immun. 2020, 85, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Yi, D.Y.; Kim, S.Y. Human Breast Milk Composition and Function in Human Health: From Nutritional Components to Microbiome and MicroRNAs. Nutrients 2021, 13, 3094. [Google Scholar] [CrossRef] [PubMed]
- Sohail, J.; Khaliq, A. Knowledge, Attitude and Practice of Mothers Regarding Colostrum Feeding to Newborns in Rural Pakistan: A Cross-Sectional Study. Khyber Med. Univ. J. 2017, 9, 192–196. [Google Scholar]
- Chai, Y.; Nandi, A.; Heymann, J. Does extending the duration of legislated paid maternity leave improve breastfeeding practices? Evidence from 38 low-income and middle-income countries. BMJ Glob. Health 2018, 3, e001032. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1: Definitions: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington, DC, USA; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Eidelman, A.I.; Schanler, R.J. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- World Health Organization. Interventions by Global Target. Available online: https://www.who.int/elena/global-targets/en/ (accessed on 4 March 2022).
- Olang, B.; Heidarzadeh, A.; Strandvik, B.; Yngve, A. Reasons given by mothers for discontinuing breastfeeding in Iran. Int. Breastfeed. J. 2012, 7, 7. [Google Scholar] [CrossRef]
- Lima, A.P.; Castral, T.C.; Leal, L.P.; Javorski, M.; Sette, G.C.; Scochi, C.G.; de Vasconcelos, M.G. Exclusive breastfeeding of premature infants and reasons for discontinuation in the first month after hospital discharge. Rev. Gauch. De Enferm. 2019, 40. [Google Scholar] [CrossRef]
- Hornsby, P.P.; Gurka, K.K.; Conaway, M.R.; Kellams, A.L. Reasons for early cessation of breastfeeding among women with low income. Breastfeed. Med. 2019, 143, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Brodribb, W.; Miller, Y. Introducing solids and water to Australian infants. J. Hum. Lact. 2013, 29, 214–221. [Google Scholar] [CrossRef]
- Garrison, M.P.; Maisano, P. Systematic Review of Factors Influencing Non–Medically Indicated Formula Supplementation of Newborns in the Hospital Setting. Nurs. Women’s Health 2019, 23, 340–350. [Google Scholar] [CrossRef]
- Zeleke, L.B.; Gebremichael, M.W.; Adinew, Y.M.; Gelaw, K.A. Appropriate Weaning Practice and Associated Factors among Infants and Young Children in Northwest Ethiopia. J. Nutr. Metab. 2017, 2017, 9608315. [Google Scholar]
- Falkner, F. Infant and Child Nutrition Worldwide: Issues and Perspectives; CRC Press: Boca Raton, FL, USA, 1991. [Google Scholar]
- Khaliq, A.; Wraith, D.; Nambiar, S.; Miller, Y. A review of the prevalence, trends, and determinants of coexisting forms of malnutrition in neonates, infants, and children. BMC Public Health 2022, 22, 879. [Google Scholar] [CrossRef]
- Khaliq, A.; Wraith, D.; Miller, Y.; Nambiar-Mann, S. Prevalence, trends, and socioeconomic determinants of coexisting forms of malnutrition amongst children under five years of age in Pakistan. Nutrients 2021, 13, 4566. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Funds. National Nutrition Survey 2018, Key Finding Report. 2019. Available online: https://www.unicef.org/pakistan/national-nutrition-survey-2018 (accessed on 21 October 2020).
- Akhtar, S. Malnutrition in South Asia—A critical reappraisal. Crit. Rev. Food Sci. Nutr. 2016, 56, 2320–2330. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, L.S.; Latham, M.C.; Ottesen, E.A. Global malnutrition. Parasitology 2000, 121, S5–S22. [Google Scholar] [CrossRef]
- Demilew, Y.M.; Tafere, T.E.; Abitew, D.B. Infant and young child feeding practice among mothers with 0–24 months old children in Slum areas of Bahir Dar City, Ethiopia. Int. Breastfeed. J. 2017, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Kolčić, I. Double burden of malnutrition: A silent driver of double burden of disease in low- and middle-income countries. J. Glob. Health 2012, 2, 020303. [Google Scholar] [CrossRef]
- Goates, S.; Du, K.; Braunschweig, C.A.; Arensberg, M.B. Economic burden of disease-associated malnutrition at the state level. PLoS ONE 2016, 11, e0161833. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Steketee, R.W.; Black, R.E.; Bhutta, Z.A.; Morris, S.S. How many child deaths can we prevent this year? Lancet 2003, 362, 65–71. [Google Scholar] [CrossRef]
- World Health Organisation. Children: Reducing Mortality. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality (accessed on 27 March 2020).
- Pakistan Demographic and Health Survey. Pakistan Demographic and Health Survey 2017–2018. Available online: https://dhsprogram.com/pubs/pdf/FR354/FR354.pdf (accessed on 19 October 2019).
- Pakistan Demographic and Health Survey. Pakistan Demographic and Health Survey 1990–1991. Available online: https://dhsprogram.com/pubs/pdf/FR29/FR29.pdf (accessed on 19 October 2019).
- United nations Children Funds. Surveys: Multiple Indicator Cluster Surveys 2020. Available online: http://mics.unicef.org/surveys (accessed on 17 April 2020).
- Mei, Z.; Grummer-Strawn, L.M. Standard deviation of anthropometric Z-scores as a data quality assessment tool using the 2006 WHO growth standards: A cross country analysis. J. Bull. World Health Organ. 2007, 85, 441–448. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Recommendations for Data Collection, Analysis and Reporting on Anthropometric Indicators in Children under 5 Years Old; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Vanderwall, C.; Clark, R.R.; Eickhoff, J.; Carrel, A.L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatrics 2017, 17, 135. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, X.; Yang, Y.; Liu, X.; Yang, C.; Wang, A.; Wang, Y.; Zhou, H. Double burden of malnutrition among children under 5 in poor areas of China. PLoS ONE 2018, 13, e0204142. [Google Scholar] [CrossRef]
- World Health Organization. Infant and Young Child Feeding 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (accessed on 17 May 2022).
- World Health Organization (WHO). Indicators for Assessing Infant and Young Child Feeding Practices: Part 2: Measurement; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Shamim, S.; Naz, F.; Jamalvi, S.W.; Ali, S.S. Effect of weaning period on nutritional status of children. J. Coll. Physicians Surg. Pak. 2006, 16, 529–531. [Google Scholar]
- Hirano, A.R.; Baggio, M.A.; Ferrari, R.A.P. Breastfeeding, Supplementary Feeding and Food and Nutrition Security in A Border. Cogitare Enferm. 2021, 26. [Google Scholar] [CrossRef]
- Foote, K.D.; Marriott, L.D. Weaning of infants. Arch. Dis. Child. 2003, 88, 488–492. [Google Scholar] [CrossRef]
- Putri, E.S.; Siregar, S.M.F.; Husna, A.; Marniati, M.; Darmawan, D. Relation of Dietary Habits and Weaning with Nutritional Status of Children. Indones. J. Public Health 2020, 7, 28–33. [Google Scholar] [CrossRef]
- Ishmah, A. Hubungan Berat Bayi Lahir, Usia Penyapihan, Tingkat Kecukupan Energi Dengan Kejadian Stunting Pada Balita di Desa Jatisono, Kecamatan Gajah, Kabupaten Demak. Ph.D. Thesis, University of Muhammadiyah Semarang, Semarang, Indonesia, 2017. [Google Scholar]
- Oddo, V.M.; Rah, J.H.; Semba, R.D.; Sun, K.; Akhter, N.; Sari, M.; De Pee, S.; Moench-Pfanner, R.; Bloem, M.; Kraemer, K. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. Am. J. Clin. Nutr. 2012, 95, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.S.; Kakuma, R. Optimal duration of exclusive breastfeeding. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2012; Volume 8. [Google Scholar]
- Grummer-Strawn, L.M.; Mei, Z. Does Breastfeeding Protect Against Pediatric Overweight? Analysis of Longitudinal Data From the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics 2004, 113, e81–e86. [Google Scholar] [CrossRef]
- Vyas, S.; Kandpal, S.D.; Semwal, J.; Chauhan, S.; Nautiyal, V. Trends in weaning practices among infants and toddlers in a hilly terrain of a newly formed state of India. Int. J. Prev. Med. 2014, 5, 741. [Google Scholar] [PubMed]
- Wijlaars, L.P.M.M.; Johnson, L.; Van Jaarsveld, C.H.; Wardle, J. Socioeconomic status and weight gain in early infancy. Int. J. Obes. 2011, 35, 963–970. [Google Scholar] [CrossRef]
- Ahmad, D.; Afzal, M.; Imtiaz, A. Effect of socioeconomic factors on malnutrition among children in Pakistan. Future Bus. J. 2020, 6, 30. [Google Scholar] [CrossRef]
- Qureshi, R. Socio-Demographic Factors Associated with Malnutrition Among Children Less Than Five Years. J. Ann. of Punjab Med. Coll. 2019, 13, 181–184. [Google Scholar]
- Ali, A.; Hussain, S.A. The Impact of Household Socio-Economic Status on Child Stunting in Pakistan. In Proceedings of the International Conference on Statistical Sciences, Lahore, Pakistan, 18–20 February 2021; pp. 93–102. [Google Scholar]
| Variable | Category | Frequency (%) (n= 17,782) |
|---|---|---|
| Demographic profile | ||
| Child age in months | 2.59 ± 1.65 months | |
| Sex | Male | 8981 (50.5%) |
| Female | 8801 (49.5%) | |
| History of illness in past 14 days | No | 11,810 (66.4%) |
| Yes | 5972 (33.6%) | |
| Maternal education | No education | 9069 (51.1%) |
| Primary | 3155 (17.8%) | |
| Secondary or higher | 5225 (31.1%) | |
| Wealth index | Poorest | 4066 (22.9%) |
| Poorer | 3823 (21.5%) | |
| Middle | 3717 (20.9%) | |
| Richer | 3337 (18.8%) | |
| Richest | 2839 (16.0%) | |
| Type of place of residence | Rural | 12,088 (67.9%) |
| Urban | 5694 (32.1%) | |
| Nutritional profile | ||
| Total population | Healthy children | 11,651 (65.5%) |
| Malnourished children | 6131 (34.5%) | |
| Standalone forms of malnutrition | 3389 (19.1%) | |
| Coexisting forms of malnutrition | 2742 (15.4%) | |
| Standalone forms of malnutrition (55.3%, n = 3389) * | Wasting ∞ | 1594 (47%) |
| Stunting ∞ | 1083 (32%) | |
| Underweight ∞ | 374 (11%) | |
| Overweight/obesity ∞ | 338 (10%) | |
| Coexisting forms of malnutrition (44.7%, n = 2742) * | Coexistence of underweight with wasting ¥ | 846 (30.9%) |
| Coexistence of underweight with stunting ¥ | 1125 (41.1%) | |
| Coexistence of underweight with wasting and stunting ¥ | 368 (13.4%) | |
| Coexistence of stunting with overweight/obesity ¥ | 403 (14.6%) | |
| Feeding profile | ||
| Feeding indicators | ||
| Continuation of breastfeeding practices | No | 2440 (13.7%) |
| Yes | 15,342 (86.3%) | |
| Predominant feeding (PF) practices | No | 9693 (54.5%) |
| Yes | 8089 (45.5%) | |
| Solid and semisolid food (SSF) practices | No | 6716 (37.8%) |
| Yes | 11,066 (62.2%) | |
| Feeding practices | ||
| Derived feeding practices | Exclusive breastfeeding (EBF) | 3708 (20.8%) |
| Supplementary breastfeeding (SBF) | 11,637 (65.4%) | |
| Weaning | 2441 (13.7%) | |
| Variable | Categories | Coexistence of Underweight with Wasting 1 | Coexistence of Underweight with Stunting 2 | Coexistence of Underweight with Wasting and Stunting 3 | Coexistence of Stunting with Overweight/Obesity 4 |
|---|---|---|---|---|---|
| Continuation of breastfeeding (CBF) practices | No | Ref | Ref | Ref | Ref |
| Yes | 0.52 (0.31 to 0.87) * | 0.50 (0.31 to 0.83) * | 0.47 (0.26 to 0.85) * | 0.97 (0.75 to 1.24) | |
| Age | 0.97 (0.75 to 1.24) | ||||
| Sex | Male | Ref | Ref | - | |
| Female | 0.67 (0.53 to 0.85) * | 0.72 (0.53 to 0.96) * | |||
| Health status | No | - | - | Ref | |
| Yes | 0.71 (0.55 to 0.91) * | ||||
| Maternal education | No education | Ref | - | ||
| Primary | 0.67 (0.45 to 1.01) | ||||
| Secondary or Higher | 0.60 (0.40 to 0.89) * | ||||
| Socioeconomic status | Poorest | Ref | - | Ref | |
| Poorer | 0.95 (0.68 to 1.32) | 1.04 (0.74 to 1.45) | |||
| Middle | 1.12 (0.78 to 1.57) | 1.15 (0.81 to 1.66) | |||
| Richer | 1.72 (1.48 to 2.60) * | 1.44 (0.99 to 2.10) | |||
| Richest | 1.70 (1.06 to 2.71) * | 1.82 (1.25 to 2.64) * | |||
| Type of place of residence | Rural | - | Ref | - | |
| Urban | 1.58 (1.12 to 2.23) * |
| Variable | Categories | Coexistence of Underweight with Wasting 1 | Coexistence of Underweight with Stunting 2 | Coexistence of Underweight with Wasting and Stunting 3 | Coexistence of Stunting with Overweight/Obesity 4 |
|---|---|---|---|---|---|
| Predominant feeding (PF) practices | No | Ref | Ref | Ref | Ref |
| Yes | 1.09 (0.85 to 1.40) | 0.87 (0.69 to 1.11) | 1.12 (0.83 to 1.51) | 0.81 (0.62 to 1.03) | |
| Age | 0.89 (0.82 to 0.97) * | ||||
| Sex | Male | Ref | Ref | - | |
| Female | 0.68 (0.54 to 0.86) * | 0.73 (0.54 to 0.98) * | |||
| Health status | No | - | - | Ref | |
| Yes | 0.70 (0.55 to 0.90) * | ||||
| Maternal education | No education | Ref | - | ||
| Primary | 0.66 (0.44 to 0.99) * | ||||
| Secondary or Higher | 0.62 (0.41 to 0.92) * | ||||
| Socioeconomic status | Poorest | Ref | - | Ref | |
| Poorer | 0.96 (0.69 to 1.34) | 1.05 (0.75 to 1.46) | |||
| Middle | 1.15 (0.81 to 1.63) | 1.17 (0.81 to 1.67) | |||
| Richer | 1.79 (1.19 to 2.71) * | 1.46 (1.01 to 2.12) * | |||
| Richest | 1.82 (1.14 to 2.90) * | 1.81 (1.25 to 2.62) * | |||
| Type of place of residence | Rural | - | Ref | - | |
| Urban | 1.51 (1.07 to 2.13) * |
| Variable | Categories | Coexistence of Underweight with Wasting 1 | Coexistence of Underweight with Stunting 2 | Coexistence of Underweight with Wasting and Stunting 3 | Coexistence of Stunting with Overweight/Obesity 4 |
|---|---|---|---|---|---|
| Solid and semisolid food (SSF) practices | No | Ref | Ref | Ref | Ref |
| Yes | 1.05 (0.80 to 1.40) | 0.66 (0.51 to 0.86) * | 1.03 (0.74 to 1.44) | 1.04 (0.81 to 1.32) | |
| Age | 0.87 (0.81 to 0.94) * | ||||
| Sex | Male | Ref | Ref | - | |
| Female | 0.67 (0.53 to 0.85) * | 0.73 (0.54 to 0.98) * | |||
| Health status | No | - | Ref | ||
| Yes | 0.71 (0.55 to 0.91) * | ||||
| Maternal education | No education | Ref | - | ||
| Primary | 0.65 (0.44 to 0.97) * | ||||
| Secondary or Higher | 0.61 (0.41 to 0.91) * | ||||
| Socioeconomic status | Poorest | Ref | - | Ref | |
| Poorer | 0.97 (0.69 to 1.35) | 1.04 (0.74 to 1.45) | |||
| Middle | 1.15 (0.81 to 1.62) | 1.15 (0.80 to 1.65) | |||
| Richer | 1.78 (1.18 to 2.68) * | 1.44 (0.99 to 2.09) | |||
| Richest | 1.80 (1.13 to 2.87) * | 1.82 (1.25 to 2.64) * | |||
| Type of place of residence | Rural | - | Ref | - | |
| Urban | 1.52 (1.08 to 2.15) * |
| Variable | Categories | Coexistence of Underweight with Wasting 1 | Coexistence of Underweight with Stunting 2 | Coexistence of Underweight with Wasting and Stunting 3 | Coexistence of Stunting with Overweight/Obesity 4 |
|---|---|---|---|---|---|
| Feeding practices | Exclusive breastfeeding (EBF) | Ref | Ref | Ref | Ref |
| Supplementary breastfeeding (SBF) | 1.10 (0.81 to 1.51) | 0.84 (0.63 to 1.14) | 1.16 (0.78 to 1.71) | 0.71 (0.51 to 0.97) * | |
| Early initiation of weaning | 1.96 (1.12 to 3.47) * | 1.65 (0.95 to 2.85) | 2.25 (1.16 to 4.36) * | 0.81 (0.58 to 1.12) | |
| Age | - | 0.89 (0.82 to 0.96) * | |||
| Sex | Male | Ref | Ref | - | |
| Female | 0.67 (0.53 to 0.85) * | 0.72 (0.53 to 0.97) * | |||
| Health status | No | - | - | Ref | |
| Yes | 0.71 (0.55 to 0.90) * | ||||
| Maternal education | No education | Ref | - | ||
| Primary | 0.68 (0.46 to 1.02) | ||||
| Secondary or Higher | 0.61 (0.41 to 0.91) * | ||||
| Socioeconomic status | Poorest | Ref | - | Ref | |
| Poorer | 0.95 (0.68 to 1.33) | 1.03 (0.74 to 1.45) | |||
| Middle | 1.11 (0.78 to 1.57) | 1.18 (0.82 to 1.70) | |||
| Richer | 1.73 (1.15 to 2.61) * | 1.48 (1.01 to 2.15) * | |||
| Richest | 1.70 (1.06 to 2.72) * | 1.88 (1.29 to 2.74) * | |||
| Type of place of residence | Rural | - | Ref | - | |
| Urban | 1.58 (1.12 to 2.24) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khaliq, A.; Wraith, D.; Miller, Y.; Nambiar, S. Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age. Nutrients 2022, 14, 4242. https://doi.org/10.3390/nu14204242
Khaliq A, Wraith D, Miller Y, Nambiar S. Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age. Nutrients. 2022; 14(20):4242. https://doi.org/10.3390/nu14204242
Chicago/Turabian StyleKhaliq, Asif, Darren Wraith, Yvette Miller, and Smita Nambiar. 2022. "Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age" Nutrients 14, no. 20: 4242. https://doi.org/10.3390/nu14204242
APA StyleKhaliq, A., Wraith, D., Miller, Y., & Nambiar, S. (2022). Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age. Nutrients, 14(20), 4242. https://doi.org/10.3390/nu14204242






