Abstract
Dietary potassium intake is a dilemma in patients with chronic kidney disease (CKD). We investigated the association of urine potassium excretion, a surrogate for dietary potassium intake, with blood pressure variability (BPV) and cardiovascular (CV) outcomes in patients with pre-dialysis CKD. A total of 1860 participants from a cohort of pre-dialysis CKD (KNOW-CKD) patients were divided into the quartiles by spot urine potassium-to-creatinine ratio. The first quartile (26.423 ± 5.731 mmol/gCr) was defined as low urine potassium excretion. Multivariate linear regression analyses revealed an independent association of low urine potassium excretion with high BPV (adjusted β coefficient 1.163, 95% confidence interval 0.424 to 1.901). Cox regression analyses demonstrated that, compared to high urine potassium excretion, low urine potassium excretion is associated with increased risk of CV events (adjusted hazard ratio 2.502, 95% confidence interval 1.162 to 5.387) but not with all-cause mortality. In conclusion, low urine potassium excretion is associated with high BPV and increased risk of CV events in patients with pre-dialysis CKD. The restriction of dietary potassium intake should be individualized in patients with pre-dialysis CKD.
1. Introduction
Blood pressure (BP) variability (BPV) is an emerging mediator of clinical outcomes [1,2,3]. The association between long-term BPV and the risk of incident chronic kidney disease (CKD) has been repeatedly reported in the general population [4,5,6]. In patients with CKD, higher long-term BPV is associated with more rapid progression of CKD [7], poor cardiovascular (CV) outcomes and increased all-cause mortality [8]. A close relationship between BPV and the amount of dietary sodium has been reported both in normotensive [9] and hypertensive [10] subjects. Conversely, randomized trials proved that oral potassium supplements significantly reduce systolic BP (SBP), but not diastolic BP (DBP) [11], and improve arterial compliance [12] in the general population. Yet, the association between dietary potassium intake and BPV has not been elucidated specifically in CKD patients.
It is well known that high sodium intake not only increases blood pressure but also plays a role in endothelial dysfunction, CV structure and function, albuminuria and CKD progression, and CV mortality in the general population. Conversely, dietary potassium intake attenuates the effects mediated by dietary sodium intake [13,14]. However, dietary potassium intake is a dilemma in patients with CKD. Excess potassium intake imposes a potential risk of fatal arrhythmia due the limited capacity of potassium excretion in patients with advanced CKD [15], even though the restriction of dietary potassium intake in this population has been rarely advocated by supporting data. Rather, mounting evidence now suggests the benefits of high potassium diets in CKD patients. A cohort study composed of CKD stages 2–4 patients in the United States reported that high urine potassium excretion, a surrogate for dietary potassium intake, is associated with an increased risk of all-cause mortality [16]. Another cohort study of non-dialysis-dependent CKD patients revealed that high urine potassium excretion is associated with better composite renal outcomes [17]. It remains unclear, however, whether low dietary potassium negatively affects CV outcomes in CKD patients, while potassium-rich diets reduce CV events and all-cause mortality in the general population [18,19,20,21].
In the present study, using potassium-to-creatinine ratio (K+/Cr) in spot urine as a surrogate for dietary potassium intake, we investigated the association of low urine potassium with visit-to-visit long-term BPV in patients with CKD. We also examined whether other urinary electrolyte parameters, such as sodium-to-creatinine ratio (Na+/Cr) and sodium-to-potassium ratio (Na+/K+), are significantly related to BPV. Importantly, the impact of low urine potassium on the CV outcomes in CKD patients was analyzed.
2. Materials and Methods
2.1. Study Design and Participants
The Korean Cohort Study for Outcomes in Patients with Chronic Kidney Disease (KNOW-CKD) is a nationwide prospective cohort study involving 9 tertiary-care general hospitals in Korea [22]. Korean patients with CKD from stage 1 to pre-dialysis stage 5, who voluntarily provided informed consent, were enrolled between 2011 and 2015. The study was conducted in accordance with the principles of the Declaration of Helsinki, and the study protocol was approved by the institutional review boards of participating centers, including Seoul National University Hospital, Yonsei University Severance Hospital, Kangbuk Samsung Medical Center, Seoul St. Mary’s Hospital, Gil Hospital, Eulji General Hospital, Chonnam National University Hospital, and Pusan Paik Hospital. All participants had been under close observation, and participants who experienced study outcomes were reported by each participating center. The study observation period ended on 31 March 2019. A total of 2238 subjects were longitudinally followed (Figure 1). After further excluding those lacking the baseline spot urine potassium and creatinine measurement, lacking the baseline BP measurement, or with a total number of BP measurements during the follow-up period of less than 3, 1860 subjects were finally included for the analyses. The median follow-up duration was 5.623 years.
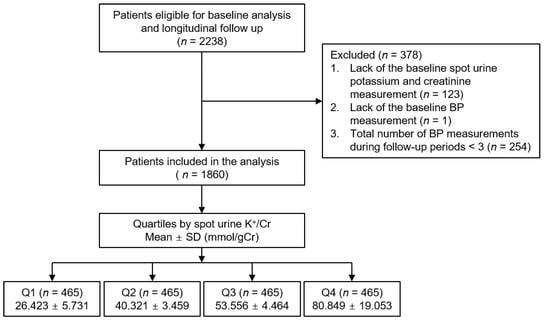
Figure 1.
Flow diagram of the study participants. Abbreviations: Cr, creatinine; K+/Cr, potassium/creatinine ratio; SD, standard deviation; Q1, 1st quartile; Q2, 2nd quartile; Q3, 3rd quartile; Q4, 4th quartile.
2.2. Data Collection
Demographic information was collected from all eligible participants, including age, gender, smoking history, medications (angiotensin-converting enzyme inhibitors and angiotensin receptor blockers (ACEi/ARBs), diuretics, and statins), and comorbid conditions, at the time of screening. Anthropometric indices (height, weight circumference (WC), and systolic and diastolic blood pressures (SBP and DBP)) were also measured. Body mass index (BMI) was calculated as weight/height2 (kg/m2). Laboratory data included hemoglobin, creatinine, albumin, glucose, triglyceride (TG), total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol (HDL-C), and high sensitive C-reactive protein (hs-CRP). Serum creatinine was measured by an isotope dilution mass spectrometry–traceable method, and estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [23]. CKD stages were determined by the Kidney Disease Improving Global Outcomes guidelines [24]. Urinary metrics, such as sodium, potassium, and creatinine (Cr), were measured in random, preferably second-voided, spot urine samples at the baseline. To measure the urinary potassium excretion, 24 h urine samples were collected in a total of 843 subjects. Subjects were divided into quartiles (Q1 to Q4) by spot urine K+/Cr (Figure 1 and Table 1), Na+/Cr (Supplemental Table S1), or Na+/K+ (Supplemental Table S2), where the 1st and 4th quartiles were defined as low and high, respectively.

Table 1.
Baseline characteristics of study participants in the quartiles by spot urine K+/Cr.
2.3. Determination of Visit-to-Visit BPV
BP was measured by an electronic sphygmomanometer after seated rest for 5 min, at 0, 6, and 12 months and then yearly thereafter up to 8 years. Long-term visit-to-visit BPV was determined by average real variability (ARV), standard deviation (SD), and coefficient of variation (CoV) of SBP across visits. The median number of BP measurements in the study participants was 6.
2.4. Study Outcomes
The outcomes of interest were extended major cardiovascular events (eMACEs) and all-cause mortality. eMACE was defined as the first occurrence of cardiac death and nonfatal CV events, including any nonfatal coronary artery event (unstable angina, myocardial infarction, or coronary intervention/surgery), hospitalization for heart failure, ischemic or hemorrhagic stroke, or symptomatic arrhythmia.
2.5. Statistical Analysis
Continuous variables were expressed as mean ± standard deviation or median (interquartile range). Categorical variables were expressed as number of participants and percentage. For descriptive analyses, Student’s T-test or one-way analysis of variance and χ2 test were used for continuous and categorical variates, respectively. The participants with any missing data were excluded for further analyses. The multivariate linear regression model was adjusted for covariates to address the association between low urine potassium excretion and visit-to-visit BPV. The models were adjusted for age, sex, Charlson comorbidity index, history of diabetes mellitus (DM), BMI, WC, SBP, DBP, medication (ACEi/ARBs, diuretics, number of antihypertensive drugs), hemoglobin, albumin, fasting glucose, HDL-C, TG, 25(OH) vitamin D, hs-CRP levels, eGFR, and spot urine albumin-to-creatinine ratio (ACR). The results of multivariate linear regression models were presented as β coefficient and 95% CIs. Survival time was defined as the interval between the enrollment and the first occurrence of the outcomes. Patients lost to follow-up were censored at the date of the last visit. To assess the association between low urine potassium excretion and the outcomes, Cox proportional hazard regression models were analyzed. The models were adjusted for age, sex, Charlson comorbidity index, history of DM, BMI, WC, SBP, DBP, medication (ACEi/ARBs, diuretics, number of antihypertensive drugs), hemoglobin, albumin, fasting glucose, HDL-C, TG, 25(OH) vitamin D, hs-CRP levels, eGFR, spot urine ACR, and ARV of SBP. The results of Cox proportional hazard models were presented as hazard ratios (HRs) and 95% confidence intervals (CIs). To confirm our findings, we conducted sensitivity analyses. To eliminate the possibility that urine potassium excretion may not reflect dietary potassium intake proportionally in patients with advanced CKD, those with CKD stage 5 at the baseline (n = 70) were excluded in multivariate linear regression and Cox regression analyses. In addition, as the subjects with eGFR ≥ 90 mL/min/1.73 m2 were considered close to normal kidney function, we excluded the subjects with eGFR ≥ 90 mL/min/1.73 m2 (n = 213) and conducted multivariate linear regression and Cox regression analyses. Two-sided p values < 0.05 were considered statistically significant. Statistical analysis was performed using SPSS for Windows version 22.0 (IBM Corp., Armonk, NY, USA) and R (version 4.1.1; R project for Statistical Computing, Vienna, Austria).
3. Results
3.1. Baseline Characteristics
To clarify the baseline characteristics of study participants, the subjects were divided into quartiles by spot urine K+/Cr (Table 1). The follow-up durations were not different among the quartile groups. As urine potassium excretion increased from the 1st quartile (Q1) to the 4th quartile (Q4), the mean age significantly increased, while the frequency of male participants decreased. The Charlson comorbidity index, which quantifies the burden of comorbid conditions, was marginally lower in Q4 than in Q1. The frequency of diuretic use and medication of antihypertensive drugs no less than three was significantly higher in Q1. The other demographic and anthropometric findings were not significantly different among the groups. Serum potassium levels were not different across the quartile groups, while 24 h urine potassium proportionally increased from Q1 to Q4. Total cholesterol, HDL-C, and low-density lipoprotein cholesterol were lowest and highest in Q1 and Q4, respectively. Serum 25(OH) vitamin D level increased as the urine potassium excretion increased. Serum hsCRP level significantly differed among the groups, with the highest in Q2 and the lowest in Q4. Whereas no significant difference in spot urine ACR was observed across the groups, eGFR tended to be preserved as urine potassium excretion increased. Accordingly, those with early stages of CKD were relatively abundant in Q4, while those with advanced stages of CKD were more frequently observed in Q1.
3.2. Association between Spot Urine K+/Cr and BPV in Patients with Pre-Dialysis CKD
To determine the association between urine potassium excretion and BPV, BPV was compared in the quartiles by urine K+/Cr (Figure 2). The ARV of Q1 (i.e., low urine potassium excretion, spot urine K+/Cr ≤ 34.209 mmol/g) was greater than that of the rest, although statistical significance was not observed between Q1 and Q4. ARV was also compared in the quartiles by spot urine Na+/Cr and Na+/K+, which failed to reveal any significant differences across the groups.
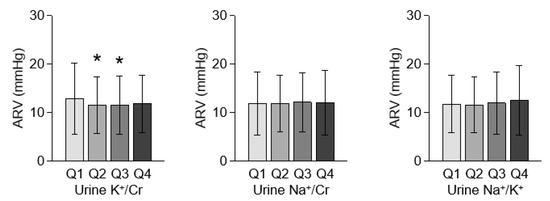
Figure 2.
Comparison of BP variability in the quartiles by urine K+/Cr. Error bars indicate standard deviation. *, p < 0.05 versus Q1 by one-way ANOVA with Scheffe’s post hoc analyses. Abbreviations: ARV, average real variability; BP, blood pressure; BPV, blood pressure variability; K+/Cr, potassium-to-creatinine ratio; Na+/Cr, sodium-to-creatinine ratio; Na+/K+, sodium-to-potassium ratio; Q1, 1st quartile; Q2, 2nd quartile; Q3, 3rd quartile; Q4, 4th quartile.
To examine whether low urine potassium excretion is independently associated with greater BPV, a multivariate linear regression model was analyzed with covariate adjustment (Table 2). In the analysis including all subjects, low urine K+/Cr was independently associated with ARV (adjusted β coefficient 1.163, 95% CI 0.424 to 1.901), but not with SD (adjusted β coefficient 0.431, 95% CI −0.176 to 1.037) or CoV (adjusted β coefficient 0.004, 95% CI −0.001 to 0.009). None of high urine K+/Cr, low urine Na+/Cr, high Na+/Cr, low urine Na+/K+, or high urine Na+/K+ was significantly associated with any BPV indices.

Table 2.
Multivariate linear regression analysis for BPV with various electrolyte profiles in spot urine samples.
3.3. Association of Low Urine Potassium Excretion with Adverse CV Outcomes in Patients with Pre-Dialysis CKD
To investigate the association between low urine potassium excretion and clinical outcomes, a Cox regression model was analyzed with covariate adjustment (Table 3). Compared to high urine potassium excretion, low potassium excretion was associated with increased risk of eMACE (adjusted HR 2.502, 95% CI 1.162 to 5.387). Low urine potassium excretion was not associated with all-cause mortality (adjusted HR 0.604, 95% CI 0.204 to 1.519). Urine sodium excretion (Supplemental Table S3) and urine Na+/K+ (Supplemental Table S4) were not significantly associated with eMACE or all-cause mortality, suggesting that potassium excretion level might better predict the CV outcomes in patients with CKD using spot urine samples.

Table 3.
Cox regression analysis of urine potassium excretion for clinical outcomes.
3.4. Sensitivity Analyses
To eliminate the possibility that urine potassium excretion may not reflect dietary potassium intake proportionally in patients with advanced CKD, those with CKD stage 5 at the baseline (n = 70) were excluded in multivariate linear regression (Supplemental Table S5) and Cox regression analyses (Supplemental Table S6). Low urine K+/Cr was robustly associated with an increase in ARV (Adjusted β coefficient 1.092, 95% CI 0.353 to 1.832) and was also associated with increased risk of eMACE (adjusted HR 2.475, 95% CI 1.128 to 5.428). After excluding the subjects with eGFR ≥ 90 mL/min/1.73 m2, who were considered close to normal kidney function, multivariate linear regression analysis (Supplemental Table S7) revealed that low urine K+/Cr is still associated with an increase in ARV (Adjusted β coefficient 1.225, 95% CI 0.433 to 2.018). Low urine K+/Cr was also robustly associated with increased risk of eMACE (adjusted HR 2.857, 95% CI 1.247 to 6.546), even after excluding 70 participants who were CKD stage 1 patients at the baseline (Supplemental Table S8).
3.5. Subgroup Analyses
To evaluate whether the association of low urine potassium excretion with BPV and the risk of CV events is modified by subgroups, we conducted subgroup analyses. The subgroups were stratified by age (<60 or ≥60 years), diuretic use (without or with), eGFR (≥45 or <45 mL/min/1.73 m2), and spot urine ACR (<300 or ≥300 mg/g). Multivariate linear regression analysis demonstrated that the association of low urine potassium excretion with an increase in BPV is significantly more prominent in the subjects with <45 mL/min/1.73 m2 than in the subjects with ≥45 mL/min/1.73 m2 (p for interaction = 0.026) (Supplemental Table S9). Cox regression analysis regarding the association of low urine potassium excretion with the risk of eMACE (Table 4) and all-cause mortality (Supplemental Table S10) revealed that P for interactions was >0.05 for all subgroups, suggesting that the association of low urine potassium excretion with increased risk of eMACE or all-cause mortality is not modified by these factors.

Table 4.
Cox regression analysis of urine potassium excretion for eMACE in various subgroups.
4. Discussion
In the present study, we demonstrated that low urine potassium excretion is independently associated with high BPV in patients with pre-dialysis CKD. We also proved that low urine potassium excretion is significantly associated with increased risk of eMACE. Subgroup analyses demonstrated that, while the association between low urine potassium excretion and the risk of eMACE was not modified by age, diuretic use, eGFR, and spot urine ACR, the association of low urine potassium excretion with high ARV is more prominent in subjects with eGFR < 45 mL/min/1.73 m2.
Despite the concern that excess potassium intake may impose a potential risk of fatal arrhythmia due to hyperkalemia in patients with advanced CKD [15], recent studies have provided evidence that the restriction of dietary potassium intake may attenuate the beneficial action of potassium with respect to CKD progression [17] and all-cause mortality [16]. Our data further expanded the advantage conferred by dietary potassium intake to the CV outcomes in CKD patients, which is largely in line with the findings observed in the general population [18,19,20,21]. The precise mechanism for how dietary potassium intake improves CV outcomes in CKD patients as well as in the general population is still unclear. Although potassium, as a potent vasodilator, reduces vascular resistance [25,26], and thereby its supplementation leads to a decrease in BP [21], the measured SBP of the subjects in the current study was not concordant with urine potassium excretion, as SBP was higher in the 3rd and 4th quartiles. We therefore hypothesize that stabilization of BPV, instead of mean BP control, may mediate the impact of dietary potassium intake on the improvement of clinical outcomes, such as eMACE.
The independent role of BPV has been illustrated by several reports [4,5,6,7,16,27]. Although the underlying mechanism of increased BPV has not yet been elucidated, evidence so far suggests certain biological processes may drive the worsening of BPV. For instance, decreased arterial elasticity and increased arterial stiffness have been observed in those with greater BPV [28,29]. Impairment of nitric oxide-drive vascular relaxation [30] may also partly contribute to the increase of BPV. A previous study reported that markers of vascular inflammation are associated with high BPV, independent of SBP [31]. Considering the theoretical action of potassium ion in vascular beds [32], it is reasonable to expect the role of dietary potassium intake in the stabilization of BPV. In this context, our data present a clinical relevance that, in addition to dietary sodium restriction [9,10], dietary potassium intake may modulate BPV in patients with CKD.
Nevertheless, it is still unknown whether a potassium-rich diet or a specified dietary potassium intake should be encouraged in patients with CKD, considering that the association of low urine potassium excretion with high ARV was more prominent in subjects with eGFR < 45 mL/min/1.73 m2 (Supplementary Table S7). Taken together, the studies thus far lack evidence that dietary potassium restriction reduces the risk of CKD progression, CV events, or all-cause mortality. It seems prudent that the restriction of dietary potassium intake should be individualized for CKD patients, even when their CKD stages are advanced, provided that serum potassium level and electrocardiogram are closely monitored [33].
The definition of BPV is variable [34]. Very short-term BPV is calculated from the measurement of beat-to-beat BPs over variable time periods. Short-term to mid-term BPV is defined from the BP measurement by ambulatory or home BP monitoring, whereas visit-to-visit BPV is obtained from a long-term measurement of BP via office or ambulatory BP monitoring. Even a visit-to-visit BPV via office BP monitoring has been variously defined. The SD of SBP and/or DBP measurements across visits was adopted in some studies [3,7], CoV (calculated as SD divided by the mean BP) in other studies [5,29,35], and both in other studies [4,6,36]. SD is relatively easier and probably more practical, but tends to correlate with the average of blood pressure measurements. Therefore, CoV, which is calculated by dividing the mean value by the SD, has been also used to determine visit-to-visit BPV [37]. ARV, which is defined as the average of the absolute differences of consecutive measurements, is a more reliable and sensitive representation of time series variability, despite relatively low sampling frequency compared to SD [38]; this is the reason why ARV was used for the primary analysis in the current study. The other index of BPV is the variation independent of the mean (VIM), which is calculated based on non-linear regression [39]. However, VIM is considered to be a better index of BP variability than the other indices, because VIM is not associated with mean blood pressure. However, VIM was not evaluated in this study, as there is a significant difference between VIM and the other indices of BPV (SD, CoV, and ARV) and as it is less practical in clinical perspectives [37].
There are a number of limitations in this study. First, we are not able to clarify the casual relation between low urine potassium excretion and the risk of eMACE, primarily due to the observational nature of the current study. Second, despite the robust relation between low urine potassium excretion and poor CV outcomes, all-cause mortality was not significantly associated with low urine potassium excretion. This could be primarily attributed to the relatively rare frequency of death events, since the events occurred only in 71 out of 1860 subjects (3.8%). We should mention that this may be changeable, as the death events accumulate during the follow up. Third, although we adopted K+/Cr in spot urine samples as a surrogate for dietary potassium intake, 24 h urinary potassium excretion is still a gold standard for estimating daily potassium intake. Yet, the urine collection for 24 h imposed a substantial burden to the subjects, and 24 h urine potassium could be measured only for a portion of the participants (843 out of 1860). Thus, the estimation of dietary potassium intake from spot urine K+/Cr seems a realistic and practical alternative. Fourth, urinary potassium excretion may not reflect dietary potassium intake accurately in the subjects with advanced CKD, due to the fact that the contribution of the gut in potassium elimination steadily increases with the decreasing GFR. However, we conducted a sensitivity analysis that excluded the subjects with CKD stage 5 at the baseline, to minimize the possibility that urine potassium excretion may not reflect dietary potassium intake proportionally in patients with advanced CKD. Fifth, it is possible that the risk of sever hyperkalemia could be underestimated, as the events due to severe hyperkalemia were not clearly defined; however, we included symptomatic arrhythmia as a component of eMACE. Sixth, as the overall nutritional status at the baseline seems better in the subjects with higher urinary potassium excretion, it is still possible that the regression analyses may not provide sufficient adjustment to compensate for the differences shown in the baseline characteristics. Seventh, despite the association between urine potassium excretion and BPV in this study, we were not able to determine the precise mechanism for how urine potassium, but not sodium, excretion is specifically associated with BPV in subjects with pre-dialysis CKD. Lastly, as this cohort study enrolled only Koreans, caution is required to extrapolate the data in the present study to other populations.
In conclusion, we report that low urine potassium excretion is independently associated with high BPV and is also significantly associated with increased risk of eMACE in patients with pre-dialysis CKD. Considering the potential CV benefit conferred by a high potassium diet, the restriction of dietary potassium intake should be individualized in patients with pre-dialysis CKD.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13124443/s1, Table S1: Baseline characteristics of study participants in the quartiles by spot urine Na+/Cr. Table S2: Baseline characteristics of study participants in the quartiles by spot urine Na+/K+. Table S3: Cox regression analysis of urine sodium excretion for clinical outcomes. Table S4: Cox regression analysis of urine Na+/K+ for clinical outcomes. Table S5: Multivariate linear regression analysis for BPV with low urine potassium excretion excluding the subjects with CKD stage 5. Table S6: Cox regression analysis of urine potassium excretion for clinical outcomes excluding the subjects with CKD stage 5. Table S7: Multivariate linear regression analysis for BPV with low urine potassium excretion excluding the subjects with CKD stage 1. Table S8: Cox regression analysis of urine potassium excretion for clinical outcomes excluding the subjects with CKD stage 1. Table S9: Multivariate linear regression analysis for ARV with low urine potassium excretion in various subgroups. Table S10: Cox regression analysis of urine potassium excretion for all-cause mortality in various subgroups.
Author Contributions
Conceptualization, S.H.S. (Sang Heon Suh); methodology, S.H.S. (Sang Heon Suh), S.H.S. (Su Hyun Song), T.R.O., H.S.C., and C.S.K.; formal analysis, S.H.S. (Sang Heon Suh); resources, E.H.B., J.L., S.H.H., Y.H.K., D.-W.C., and K.-H.O.; data curation, S.H.S. (Sang Heon Suh); writing—original draft preparation, S.H.S. (Sang Heon Suh); writing—review and editing, S.H.S. (Sang Heon Suh), S.K.M., and S.W.K.; supervision, S.K.M. and S.W.K.; funding acquisition, C.S.K., K.-H.O., and S.W.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention (2011E3300300, 2012E3301100, 2013E3301600, 2013E3301601, 2013E3301602, 2016E3300200, 2016E3300201, 2016E3300202, and 2019E320100), by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (HR20C0021), and a grant (BCRI20062) of Chonnam National University Hospital Biomedical Research Institute.
Institutional Review Board Statement
The study protocol was approved by the Institutional Review Board at each participating clinical center (Seoul National University Hospital (1104–089-359), Seoul National University Bundang Hospital (B-1106/129–008), Yonsei University Severance Hospital (4–2011-0163), Kangbuk Samsung Medical Center (2011–01-076), Seoul St. Mary’s Hospital (KC11OIMI0441), Gil Hospital (GIRBA2553), Eulji General Hospital (201105–01), Chonnam National University Hospital (CNUH-2011-092), and Busan Paik Hospital (11–091)).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
KNOW-CKD: Study Group Clinical Centers. Seoul National University, Curie Ahn, Kook-Hwan Oh, Dong Wan Chae, Ho Jun Chin, Hayne Cho Park, Seungmi Lee, Hyun Hwa Jang, and Hyun Jin Cho. Yonsei University, Severance Hospital, Kyu Hun Choi, Seung Hyeok Han, Tae Hyun Yoo, and Mi Hyun Yu. Kangbuk Samsung Medical Center, Kyubeck Lee, and Sooyeon Jin. The Catholic University of Korea, Seoul St. Mary’s Hospital, Yong-Soo Kim, and Sol Ji Kim. Gachon University, Gil Hospital, Wookyung Chung, Youkyoung Jang, and Ji Hye Park. Eulji University, Eulji General Hospital, Young-Hwan Hwang, Su-Ah Sung, and Jeong Ok So. Chonnam University, Soo Wan Kim and Ji Seon Lee. Inje University, Pusan Paik Hospital, Yeong Hoon Kim, Sun Woo Kang, and Yun Jin Kim. Epidemiology and Biostatistics. Department of Preventive Medicine, Seoul National University College of Medicine, Byung-Joo Park, Sue Kyung Park and Juyeon Lee. Coordinating Center. Medical Research Collaborating Center, Seoul National University Hospital and Seoul National University College of Medicine, Joongyub Lee, Dayeon Nam, Soohee Kang, MSc and Heejung Ahn. Central Laboratory, Donghee Seo, Lab Genomics, Korea and Dae Yeon Cho, Lab Genomics, Korea. Biobank. Korea Biobank, Korea Centers for Disease Control and Prevention, Osong, Korea. Korea Center for Disease Control and Prevention, Dukhyoung Lee, Hyekyung Park (Project Officer), Eunkyeong Jung (Project Officer), Suyeon Jeong, Eunmi Ahn and Sil-Hea Sung.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mezue, K.; Goyal, A.; Pressman, G.S.; Matthew, R.; Horrow, J.C.; Rangaswami, J. Blood pressure variability predicts adverse events and cardiovascular outcomes in SPRINT. J. Clin. Hypertens. 2018, 20, 1247–1252. [Google Scholar] [CrossRef] [Green Version]
- Myasoedova, E.; Crowson, C.S.; Green, A.B.; Matteson, E.L.; Gabriel, S.E. Longterm blood pressure variability in patients with rheumatoid arthritis and its effect on cardiovascular events and all-cause mortality in RA: A population-based comparative cohort study. J. Rheumatol. 2014, 41, 1638–1644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, S.; Shin, J.; Choi, S.Y.; Sung, K.C.; Ihm, S.H.; Kim, K.I.; Kim, Y.M. Impact of Visit-to-Visit Variability in Systolic Blood Pressure on Cardiovascular Outcomes in Korean National Health Insurance Service-National Sample Cohort. Am. J. Hypertens. 2017, 30, 577–586. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Li, D.; Song, Y.; Gao, L.; Fan, F.; Wang, B.; Liang, M.; Wang, G.; Li, J.; Zhang, Y.; et al. Visit-to-visit variability in blood pressure and the development of chronic kidney disease in treated general hypertensive patients. Nephrol. Dial. Transplant. 2020, 35, 1739–1746. [Google Scholar] [CrossRef]
- Okada, H.; Fukui, M.; Tanaka, M.; Matsumoto, S.; Mineoka, Y.; Nakanishi, N.; Asano, M.; Yamazaki, M.; Hasegawa, G.; Nakamura, N. Visit-to-visit blood pressure variability is a novel risk factor for the development and progression of diabetic nephropathy in patients with type 2 diabetes. Diabetes Care 2013, 36, 1908–1912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noshad, S.; Mousavizadeh, M.; Mozafari, M.; Nakhjavani, M.; Esteghamati, A. Visit-to-visit blood pressure variability is related to albuminuria variability and progression in patients with type 2 diabetes. J. Hum. Hypertens. 2014, 28, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Whittle, J.; Lynch, A.I.; Tanner, R.M.; Simpson, L.M.; Davis, B.R.; Rahman, M.; Whelton, P.K.; Oparil, S.; Muntner, P. Visit-to-Visit Variability of BP and CKD Outcomes: Results from the ALLHAT. Clin. J. Am. Soc. Nephrol. 2016, 11, 471–480. [Google Scholar] [CrossRef] [Green Version]
- Mallamaci, F.; Tripepi, G.; D’Arrigo, G.; Borrelli, S.; Garofalo, C.; Stanzione, G.; Provenzano, M.; De Nicola, L.; Conte, G.; Minutolo, R.; et al. Blood Pressure Variability, Mortality, and Cardiovascular Outcomes in CKD Patients. Clin. J. Am. Soc. Nephrol. 2019, 14, 233–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruddy, M.C.; Arora, A.; Malka, E.S.; Bialy, G.B. Blood pressure variability and urinary electrolyte excretion in normotensive adults. Am. J. Hypertens. 1993, 6, 480–486. [Google Scholar] [CrossRef]
- Ozkayar, N.; Dede, F.; Ates, I.; Akyel, F.; Yildirim, T.; Altun, B. The relationship between dietary salt intake and ambulatory blood pressure variability in non-diabetic hypertensive patients. Nefrologia 2016, 36, 694–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, D.; He, J.; Wu, X.; Duan, X.; Whelton, P.K. Effect of potassium supplementation on blood pressure in Chinese: A randomized, placebo-controlled trial. J. Hypertens. 2001, 19, 1325–1331. [Google Scholar] [CrossRef]
- He, F.J.; Marciniak, M.; Carney, C.; Markandu, N.D.; Anand, V.; Fraser, W.D.; Dalton, R.N.; Kaski, J.C.; MacGregor, G.A. Effects of potassium chloride and potassium bicarbonate on endothelial function, cardiovascular risk factors, and bone turnover in mild hypertensives. Hypertension 2010, 55, 681–688. [Google Scholar] [CrossRef]
- Cupisti, A.; Kovesdy, C.P.; D’Alessandro, C.; Kalantar-Zadeh, K. Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function. Nutrients 2018, 10, 261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aaron, K.J.; Sanders, P.W. Role of dietary salt and potassium intake in cardiovascular health and disease: A review of the evidence. Mayo Clin. Proc. 2013, 88, 987–995. [Google Scholar] [CrossRef] [Green Version]
- Kovesdy, C.P.; Matsushita, K.; Sang, Y.; Brunskill, N.J.; Carrero, J.J.; Chodick, G.; Hasegawa, T.; Heerspink, H.L.; Hirayama, A.; Landman, G.W.D.; et al. Serum potassium and adverse outcomes across the range of kidney function: A CKD Prognosis Consortium meta-analysis. Eur. Heart J. 2018, 39, 1535–1542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonberg-Yoo, A.K.; Tighiouart, H.; Levey, A.S.; Beck, G.J.; Sarnak, M.J. Urine Potassium Excretion, Kidney Failure, and Mortality in CKD. Am. J. Kidney Dis. 2017, 69, 341–349. [Google Scholar] [CrossRef]
- Kim, H.W.; Park, J.T.; Yoo, T.H.; Lee, J.; Chung, W.; Lee, K.B.; Chae, D.W.; Ahn, C.; Kang, S.W.; Choi, K.H.; et al. Urinary Potassium Excretion and Progression of CKD. Clin. J. Am. Soc. Nephrol. 2019, 14, 330–340. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef] [Green Version]
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef] [Green Version]
- Cook, N.R.; Obarzanek, E.; Cutler, J.A.; Buring, J.E.; Rexrode, K.M.; Kumanyika, S.K.; Appel, L.J.; Whelton, P.K.; Trials of Hypertension Prevention Collaborative Research Group. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: The Trials of Hypertension Prevention follow-up study. Arch. Intern. Med. 2009, 169, 32–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whelton, P.K.; He, J.; Cutler, J.A.; Brancati, F.L.; Appel, L.J.; Follmann, D.; Klag, M.J. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA 1997, 277, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.-H.; Park, S.K.; Park, H.C.; Chin, H.J.; Chae, D.W.; Choi, K.H.; Han, S.H.; Yoo, T.H.; Lee, K.; Kim, Y.-S.; et al. KNOW-CKD (KoreaN cohort study for Outcome in patients With Chronic Kidney Disease): Design and methods. BMC Nephrol. 2014, 15, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Chapter 1: Definition and classification of CKD. Kidney Int. Suppl. (2011) 2013, 3, 19–62. [CrossRef] [PubMed] [Green Version]
- Fujita, T.; Ito, Y. Salt loads attenuate potassium-induced vasodilation of forearm vasculature in humans. Hypertension 1993, 21, 772–778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips, R.J.; Robinson, B.F. The dilator response to K+ is reduced in the forearm resistance vessels of men with primary hypertension. Clin. Sci. 1984, 66, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Jhee, J.H.; Seo, J.; Lee, C.J.; Park, J.T.; Han, S.H.; Kang, S.W.; Park, S.; Yoo, T.H. Ambulatory blood pressure variability and risk of cardiovascular events, all-cause mortality, and progression of kidney disease. J. Hypertens. 2020, 38, 1712–1721. [Google Scholar] [CrossRef]
- Shimbo, D.; Shea, S.; McClelland, R.L.; Viera, A.J.; Mann, D.; Newman, J.; Lima, J.; Polak, J.F.; Psaty, B.M.; Muntner, P. Associations of aortic distensibility and arterial elasticity with long-term visit-to-visit blood pressure variability: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Hypertens. 2013, 26, 896–902. [Google Scholar] [CrossRef] [Green Version]
- Nagai, M.; Hoshide, S.; Nishikawa, M.; Masahisa, S.; Kario, K. Visit-to-visit blood pressure variability in the elderly: Associations with cognitive impairment and carotid artery remodeling. Atherosclerosis 2014, 233, 19–26. [Google Scholar] [CrossRef]
- Diaz, K.M.; Veerabhadrappa, P.; Kashem, M.A.; Feairheller, D.L.; Sturgeon, K.M.; Williamson, S.T.; Crabbe, D.L.; Brown, M.D. Relationship of visit-to-visit and ambulatory blood pressure variability to vascular function in African Americans. Hypertens. Res. 2012, 35, 55–61. [Google Scholar] [CrossRef] [Green Version]
- Tatasciore, A.; Zimarino, M.; Renda, G.; Zurro, M.; Soccio, M.; Prontera, C.; Emdin, M.; Flacco, M.; Schillaci, G.; De Caterina, R. Awake blood pressure variability, inflammatory markers and target organ damage in newly diagnosed hypertension. Hypertens. Res. 2008, 31, 2137–2146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahranavard, T.; Carbone, F.; Montecucco, F.; Xu, S.; Al-Rasadi, K.; Jamialahmadi, T.; Sahebkar, A. The role of potassium in atherosclerosis. Eur. J. Clin. Investig. 2021, 51, e13454. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef] [PubMed]
- Parati, G.; Ochoa, J.E.; Lombardi, C.; Bilo, G. Assessment and management of blood-pressure variability. Nat. Rev. Cardiol. 2013, 10, 143–155. [Google Scholar] [CrossRef]
- Wong, Y.K.; Chan, Y.H.; Hai, J.S.H.; Lau, K.K.; Tse, H.F. Predictive value of visit-to-visit blood pressure variability for cardiovascular events in patients with coronary artery disease with and without diabetes mellitus. Cardiovasc. Diabetol. 2021, 20, 88. [Google Scholar] [CrossRef]
- Eguchi, K.; Hoshide, S.; Schwartz, J.E.; Shimada, K.; Kario, K. Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am. J. Hypertens. 2012, 25, 962–968. [Google Scholar] [CrossRef] [Green Version]
- Hoshide, S. Clinical implication of visit-to-visit blood pressure variability. Hypertens. Res. 2018, 41, 993–999. [Google Scholar] [CrossRef]
- Mena, L.; Pintos, S.; Queipo, N.V.; Aizpúrua, J.A.; Maestre, G.; Sulbarán, T. A reliable index for the prognostic significance of blood pressure variability. J. Hypertens. 2005, 23, 505–511. [Google Scholar] [CrossRef] [Green Version]
- Rothwell, P.M.; Howard, S.C.; Dolan, E.; O’Brien, E.; Dobson, J.E.; Dahlöf, B.; Sever, P.S.; Poulter, N.R. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010, 375, 895–905. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).