The Association between Malnutrition and Oral Health in Older People: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria for Studies
2.3. Selection Criteria Populaton
2.4. Methodological Quality Assessment
2.5. Data Extraction
2.6. Clinical and Methodological Heterogeneity
3. Results
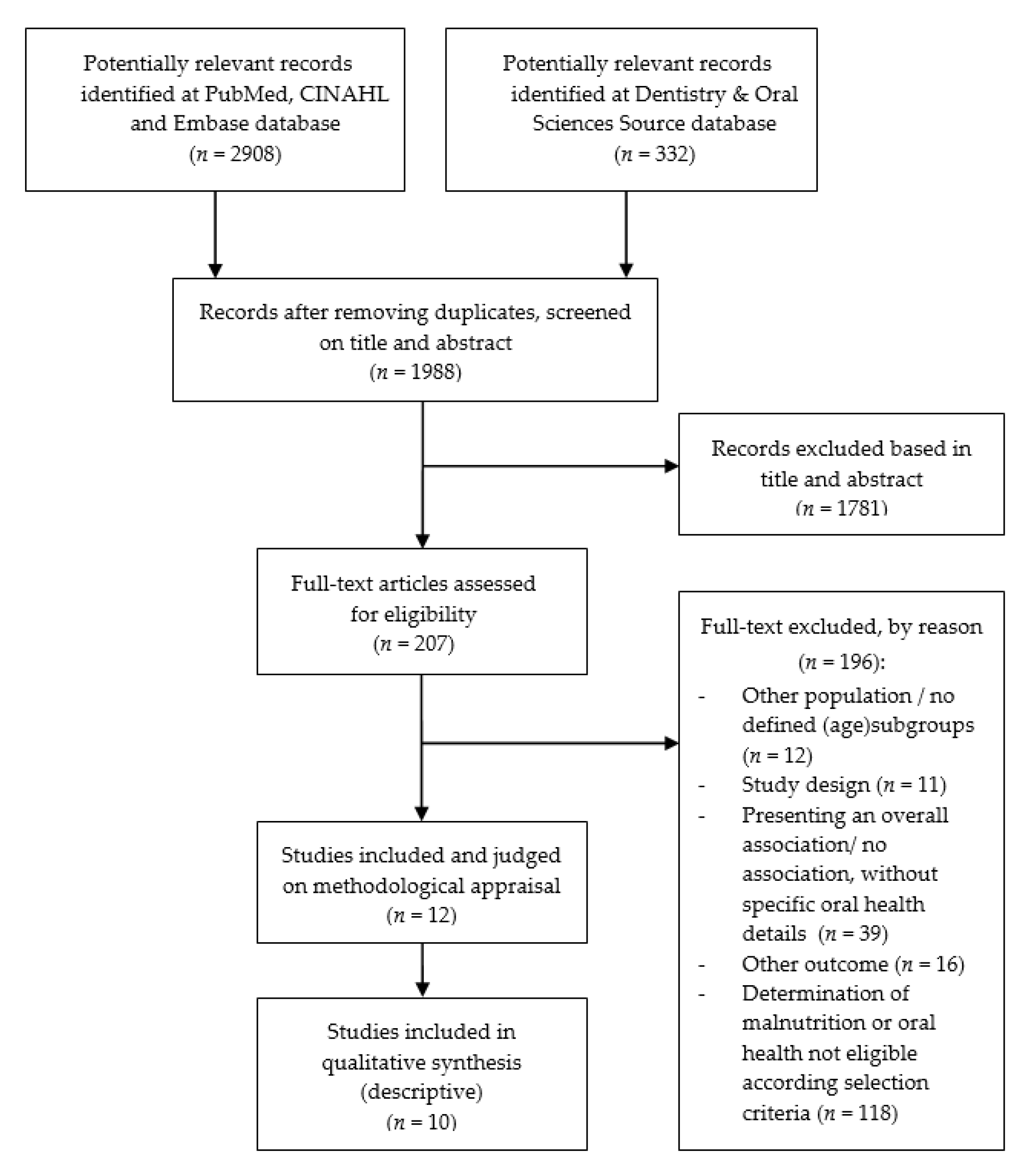
3.1. Study Selection
3.2. Methodological Quality of the Studies
3.3. Study Characteristics
3.4. Malnutrition and Hard Tissue Conditions of the Mouth
3.5. Malnutrition and Soft Tissue Conditions of the Mouth
3.6. Malnutrition and Hyposalivation or Xerostomia
3.7. Malnutrition and Subjective Oral Health
4. Discussion
4.1. Measurement and Definition of Malnutrition and Oral Health
4.2. Methodological Limitations of Included Studies
4.3. Strengths and Limitations
4.4. Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Suzman, R.; Beard, J. Global Health and Aging; WHO: Geneva, Switzerland, 2011; p. 26. Available online: https://www.who.int/ageing/publications/global_health.pdf (accessed on 3 February 2020).
- LoketGezondleven.nl. Facts and Figures Elderly People in the Netherlands. National Institute for Public Health and the Environment Ministry of Health, Welfare and Sport. Available online: https://www.loketgezondleven.nl/gezonde-gemeente/themadossiers/gezond-en-vitaal-ouder-worden/feiten-en-waarden-ouderen (accessed on 23 November 2019).
- Guigoz, P.Y.; Vellas, M.B.; Garry, P.P.J. Assessing the Nutritional Status of the Elderly: The Mini Nutritional Assessment as Part of the Geriatric Evaluation. Nutr. Rev. 2009, 54, S59–S65. [Google Scholar] [CrossRef]
- Son, N.; Kavak, B.; Nazan, S.; Buket, K. Evaluation of nutritional status of elderly patients presenting to the Family Health Center. Pak. J. Med. Sci. 2018, 34, 446–451. [Google Scholar] [CrossRef]
- Leij-Halfwerk, S.; Verwijs, M.H.; van Houdt, S.; Borkent, J.W.; Guaitoli, P.R.; Pelgrim, T.; Heymans, M.W.; Power, L.; Visser, M.; Corish, C.A.; et al. Prevalence of protein-energy mal-nutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: A systematic review and meta-analysis. Maturitas 2019, 126, 80–89. [Google Scholar] [CrossRef]
- Voedingscentrum. Dutch Nutrition Center. Malnutrition. Available online: https://www.voedingscentrum.nl/encyclopedie/ondervoeding.aspx (accessed on 20 November 2019).
- Definition and Diagnosis Malnutrition. Available online: https://www.steeringgroepondervoeding.nl/toolkits/wat-is-ondervoeding (accessed on 15 November 2019).
- Kruizenga, H.; Beijer, S.; Huisman-de Waal, G.; Jonkers-Schuitema, C.; Klos, M.; Remijnse-Meester, W.; Thijs, A.; Witteman, B.; Tieland, M. Guideline for Malnutrition Recognition, Diagnosis and Treatment of Malnutrition in Adults; Steering Committee Malnutrition: The Netherlands, 2009; pp. 1–39. [Google Scholar]
- Sobotka, L.; Allison, S.P.; Forbes, A.; Meier, R.F.; Schneider, S.M.; Soeters, P.B.; Stanga, Z.; Van Gossum, A. Basics in Clinical Nutrition, 4th ed.; Galén: Praha, Czech Republic, 2019. [Google Scholar]
- Gil-Montoya, J.; Ponce, G.; Lara, I.S.; Barrios, R.; Llodra, J.; Bravo, M. Association of the oral health impact profile with malnutrition risk in Spanish elders. Arch. Gerontol. Geriatr. 2013, 57, 398–402. [Google Scholar] [CrossRef]
- Petersen, P.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people--call for public health action. Community Dent. Health 2010, 27, 21313969. [Google Scholar]
- Wang, T.-F.; Chen, Y.-Y.; Liou, Y.-M.; Chou, C. Investigating tooth loss and associated factors among older Taiwanese adults. Arch. Gerontol. Geriatr. 2014, 58, 446–453. [Google Scholar] [CrossRef]
- Kshetrimayum, N.; Reddy, C.V.K.; Siddhana, S.; Manjunath, M.; Rudraswamy, S.; Sulavai, S. Oral health-related quality of life and nutritional status of institutionalized elderly population aged 60 years and above in Mysore City, India. Gerodontology 2013, 30, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.-H.; Tang, S.T.; Wang, C.; Huang, G.-H. Trajectory and determinants of nutritional health in older patients during and six-month post-hospitalisation. J. Clin. Nurs. 2009, 18, 3299–3307. [Google Scholar] [CrossRef] [PubMed]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Factors associated with poor nutritional status among community dwelling Lebanese elderly subjects living in rural areas: Results of the AMEL study. J. Nutr. Health Aging 2014, 18, 487–494. [Google Scholar] [CrossRef] [PubMed]
- De Marchi, R.J.; Hugo, F.; Hilgert, J.; Padilha, D.M.P. Association between oral health status and nutritional status in south Brazilian independent-living older people. Nutrients 2008, 24, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Gil-Montoya, J.; de Mello, A.L.F.; Barrios, R.; Gonzalez-Moles, M.A.; Bravo, M. Oral health in the elderly patient and its impact on general well-being: A nonsystematic review. Clin. Interv. Aging 2015, 10, 461–467. [Google Scholar] [CrossRef] [Green Version]
- Sheetal, A.; Hiremath, V.K.; Patil, A.G.; Sajjansetty, S.; Kumar, S.R. Malnutrition and its Oral Outcome—A Review. J. Clin. Diagn. Res. 2013, 7, 178–180. [Google Scholar] [CrossRef]
- Morris, A.M.; Engelberg, J.K.; Orozco, M.; Schmitthenner, B. The Link between Malnutrition and Poor Oral Health in Older Adults. 4 June 2019. Available online: https://www.westhealth.org/the-link-between-malnutrition-and-poor-oral-health-in-older-adults/ (accessed on 16 October 2019).
- Toniazzo, M.P.; Amorim, P.D.S.; Muniz, F.W.M.G.; Weidlich, P. Relationship of nutritional status and oral health in elderly: Systematic review with meta-analysis. Clin. Nutr. 2018, 37, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, S.; Savabi, G.; Khazaei, S.; Savabi, O.; Esmaillzadeh, A.; Keshteli, A.H.; Adibi, P. Association between food intake and oral health in elderly: SEPAHAN systematic review no. 8. Dent. Res. J. 2011, 8, S15–S20. [Google Scholar]
- Van Lancker, A.; Verhaeghe, S.; Van Hecke, A.; Vanderwee, K.; Goossens, J.; Beeckman, D. The association between malnutrition and oral health status in elderly in long-term care facilities: A systematic review. Int. J. Nurs. Stud. 2012, 49, 1568–1581. [Google Scholar] [CrossRef] [PubMed]
- Van Steenberghe, D.; Beertsen, W.; van der Velden, U.; Quirynen, M. Periodontology, 1st ed.; Bohn Stafleu van Loghum: Houten, The Netherlands, 2015; p. 533. [Google Scholar]
- Gonsalves, W.C.; Wrightson, A.S.; Henry, R.G. Common oral conditions in older persons. Am. Fam. Phys. 2008, 78, 18841733. [Google Scholar]
- Professional Association of Nursing Home Doctors and Social Geriatricians. Oral Care Guideline for Care Dependent Clients in Nursing Homes. Available online: http://www.platformouderenzorg.nl/dossiers/richtenmondzorgnvva_web.pdf (accessed on 10 March 2020).
- Wiener, R.C.; Wu, B.; Crout, R.; Wiener, M.; Plassman, B.; Kao, E.; McNeil, D. Hyposalivation and Xerostomia in Dentate Older Adults. J. Am. Dent. Assoc. 2010, 141, 279–284. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2014. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 4 July 2020).
- Andersson, P.; Hallberg, I.; Lorefält, B.; Unosson, M.; Renvert, S. Oral health problems in elderly rehabilitation patients. Int. J. Dent. Hyg. 2004, 2, 70–77. [Google Scholar] [CrossRef] [PubMed]
- El Osta, N.; Hennequin, M.; Tubert-Jeannin, S.; Naaman, N.B.A.; El Osta, L.; Geahchan, N. The pertinence of oral health indicators in nutritional studies in the elderly. Clin. Nutr. 2014, 33, 316–321. [Google Scholar] [CrossRef]
- Huppertz, V.A.; van der Putten, G.-J.; Halfens, R.J.; Schols, J.M.; de Groot, L. Association between Malnutrition and Oral Health in Dutch Nursing Home Residents: Results of the LPZ Study. J. Am. Med. Dir. Assoc. 2017, 18, 948–954. [Google Scholar] [CrossRef]
- Kiesswetter, E.; Hengeveld, L.M.; Keijser, B.J.; Volkert, D.; Visser, M. Oral health determinants of incident malnutrition in community-dwelling older adults. J. Dent. 2019, 85, 73–80. [Google Scholar] [CrossRef]
- Lindmark, U.; Jansson, H.; Lannering, C.; Johansson, L. Oral health matters for the nutritional status of older persons-A population-based study. J. Clin. Nurs. 2017, 27, 1143–1152. [Google Scholar] [CrossRef]
- Mesas, A.E.; De Andrade, S.; Cabrera, M.A.S.; Bueno, V.L.R.D.C. Salud oral y déficit nutricional en adultos mayores no institucionalizados en Londrina, Paraná, Brasil. Rev. Bras. Epidemiol. 2010, 13, 434–445. [Google Scholar] [CrossRef] [Green Version]
- Poisson, P.; Laffond, T.; Campos, S.; Dupuis, V.; Bourdel-Marchasson, I. Relationships between oral health, dysphagia and undernutrition in hospitalised elderly patients. Gerodontology 2016, 33, 161–168. [Google Scholar] [CrossRef]
- Samnieng, P.; Ueno, M.; Shinada, K.; Zaitsu, T.; Wright, F.A.C.; Kawaguchi, Y. Oral Health Status and Chewing Ability is Related to Mini-Nutritional Assessment Results in an Older Adult Population in Thailand. J. Nutr. Gerontol. Geriatr. 2011, 30, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Soini, H.; Muurinen, S.; Routasalo, P.; Sandelin, E.; Savikko, N.; Suominen, M.; Ainamo, A.; Pitkala, K.H. Oral and nutritional status--Is the MNA a useful tool for dental clinics. J. Nutr. Health Aging 2006, 10, 500–501. [Google Scholar]
- Takahashi, M.; Maeda, K.; Wakabayashi, H. Prevalence of sarcopenia and association with oral health-related quality of life and oral health status in older dental clinic outpatients. Geriatr. Gerontol. Int. 2018, 18, 915–921. [Google Scholar] [CrossRef]
- Jung, S.H.; Ryu, J.I.; Jung, D.B. Association of total tooth loss with socio-behavioural health indicators in Korean elderly. J. Oral Rehabilitation 2010, 38, 517–524. [Google Scholar] [CrossRef]
- Ikebe, K.; Nokubi, T.; Sajima, H.; Kobayashi, S.; Hata, K.; Ono, T.; Ettinger, R.L. Perception of dry mouth in a sample of community-dwelling older adults in Japan. Speéc. Care Dent. 2001, 21, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Makhija, S.K.; Gilbert, G.H.; Litaker, M.S.; Allman, R.M.; Sawyer, P.; Locher, J.L.; Ritchie, C.S. Association Between Aspects of Oral Health–Related Quality of Life and Body Mass Index in Community-Dwelling Older Adults. J. Am. Geriatr. Soc. 2007, 55, 1808–1816. [Google Scholar] [CrossRef]
- Alam, I.; Bangash, F. Oral health and nutritional status of the free-living elderly in Peshawar, Pakistan. Saudi Med. J. 2010, 31, 713–715. [Google Scholar] [PubMed]
- Everaars, B.; Weening, L.; Jerković-Ćosić, K.; Schoonmade, L.; Bleijenberg, N.; De Wit, N.J.; Van Der Heijden, G.J.M.G. Measurement properties of oral health assessments for non-dental healthcare professionals in older people: A systematic review. BMC Geriatr. 2020, 20, 4–18. [Google Scholar] [CrossRef] [PubMed]
| First Author | Publication Year, Country | Number of Participants | Mean Age | Setting | Measurement of Malnutrition | Measurement of Oral Health | Methodological Quality Score |
|---|---|---|---|---|---|---|---|
| Andersson [28] | 2004, Sweden | n = 161 M: 43 F: 118 | 81.7 (range 65–89) | Three rehabilitation wards at a university hospital | SGA | ROAG | 9 |
| El Osta [29] | 2013, Lebanon | n = 201 F: 121 M: 80 | F: 71.6 ± 6 M: 72.7 ± 7 | Older people attending two acute care units | MNA | GOHAI, DMTF/DTF, prosthetic status, posterior dental FUs | 9 |
| Huppertz [30] | 2017, The Netherlands | n = 3320 M: 1059 F: 2261 | 84.3 ± 7.4 | Nursing homes | BMI in combination with unintentional weight loss | Standardized questionnaire on potential indicators of poor oral health | 9 |
| Kiesswetter [31] | 2019, The Netherlands | n = 893 M: 418 F: 475 | 67.6 ± 6.1 | Community-dwelling older people | BMI, time-specific weight loss | Self-administered questionnaire (22 items) on four oral health domains | 8 |
| Lindmark [32] | 2017, Sweden | n = 1156 M: 443 F: 713 | 82.8 ± 7.9 | Nursing homes and hospitals | MNA-SF | ROAG-J | 8 |
| Mesas [33] | 2010, Sweden | n = 267 M: 107 F: 160 | 66.5 ± 4.1 | Community-dwelling older people | MNA | GOHAI, number of teeth, prosthesis, posterior occlusion, stimulated salivary flow, CPITN | 10 |
| Poisson [34] | 2014, France | n = 159 M: 51 F: 108 | 85.3 ± 5.7 | Patients hospitalized in acute care units: 78% (n = 124) from home, 22% (n = 35) from nursing homes | Weight loss, BMI, MNA | Oral examination by dentist, DMTF index, gingival inflammation, oral candidiasis, salivary test (insufficiency if salivary flow < 0.1 g/min/weight compress < 0.35 g) | 9 |
| Samnieng [35] | 2011, Thailand | n = 612 M: 158 F: 454 | 68.8 ± 5.9 | Community-dwelling older people | MNA | Dental status assessed by dentist; DMFT, prostheses, FTUs | 9 |
| Soini [36] | 2006, Finland | n = 3088 M: 649 F: 2439 | NH: 81 LT: 83 | Institutionalized older people from NH (n = 2036) and LT (n = 1052) | MNA | Oral status evaluated by trained ward nurses | 9 |
| Takahashi [37] | 2018, Japan | n = 279 M: 106 F: 173 | 76 ± 7.5 | Older people at a dental clinic | Sarcopenia (GS, HS, MNA-SF, BMI, EAT-10, CC). | Number of teeth, FTUs. Primary outcome: OHIP to evaluate OHRQoL. Secondary outcome: OHAT | 9 |
| Item | [Ref] | Prevalence (N(%)), or No. of Teeth/FU | ||
|---|---|---|---|---|
| MN |
At Risk of MN | Well-Nourished | ||
| No. of FUs: <4 FUs 5 or 6 FUs 7 or 8 FUs | [29] | n total = 85 n = 52 (61%) ** n = 6 (7.1%) n = 27 (31.8%) | - - - | n total = 116 n = 38 (32.8%) ** n = 24 (20.7%) 54 (46.6%) |
| No. of decayed teeth | [35] | 1.6 ± 0.3 * | 1.3 ± 0.1 * | 1.1 ± 0.2 * |
| No. of teeth | [35] [37] | 8.7 ± 1.4 * 13.4 ± 9.3 | 10.1 ± 0.4 * - | 13.2 ± 0.7 * 18.9 ± 7.8 |
| No. of FTUs | [35] [37] | 8.3 ± 1.1 * 10.0 ± 3.5 | 8.4 ± 0.3 * | 10.3 ± 0.5 * 10.5 ± 2.5 |
| Association ND and edentulism | [33] | Crude OR: 1.44 a (95% CI 0.61–3.33) Adjusted OR b: 0.65 (95% CI 0.23–1.83) | ||
| Item | [Ref] | Prevalence’s | ||
|---|---|---|---|---|
| MN |
At Risk of MN | Well-Nourished | ||
| Tongue | [32] [28] |
40 (20.3%) 43 (49%) |
38 (7.4%) - |
21 (4.7%) - |
| Mucous membranes | [32] [28] |
41 (21.3%) 26 (30%) |
37 (7.2%) - |
14 (3.2%) - |
| Lips | [32] [28] |
35 (17.8%) 48 (55%) |
26 (5.0%) - |
17 (3.8%) - |
| Gums | [32] [28] |
26 (14.4%) 14 (16%) |
42 (8.7%) - |
20 (5.0%) - |
| Candidiasis | [34] |
12 (15.6%) p < 0.001 | - | - |
| Association MN and tongue problems | [28] | OR 4.4 (95 % CI 2.0–9.6; p < 0.0005) | ||
| Outcomes | First Author [Ref] |
|---|---|
| Hyposalivation | |
| Association nutritional deficit and stimulated salivary flow < 0.7 mL/min: Crude OR 1.96 (95% CI 1.06–3.83) Adjusted OR 2.18 (95% CI 1.06–4.50). | Mesas [33] |
| Association salivary flow rate < 0.7 (mL/min) and nutritional deficit: Adjusted OR 2.18 (95% CI 1.06–4.50). | Poisson [34] |
| Xerostomia | |
| Perception of xerostomia as parameter of explaining MNA variation: OR 3.49 (95% CI 1.657–7.337; p = 0.001). | El Osta [29] |
| Association between xerostomia and incident malnutrition HR 2.63 (95% CI 1.18–6.26). | Kiesswetter [31] |
| Outcomes and Prevalence: Subjective Oral Health | First Author [Ref] |
|---|---|
| Negative self-perception of oral health: Crude OR: 3.95 (95% CI 2.04–7.67) Adjusted OR: 3.41 (95% CI 1.59–7.33) | Mesas [33] |
| OHRQoL/oral status: Poorer OHRQoL and oral health status (all p < 0.001). GOHAI score explains MNA variation: OR: 2.905 (95% CI 1.40–6.00; p = 0.004). | Takahashi [37] El Osta [29] |
| OHRQoL/oral status: Negative correlation between the ROAG-J total score and MNA total score (r = −0.241; p < 0.001). | Lindmark [32] |
| Association between toothache while chewing (adjusted) HR 2.14 (95% CI 1.10–4.19; p = 0.026). | Huppertz [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Algra, Y.; Haverkort, E.; Kok, W.; Etten-Jamaludin, F.v.; Schoot, L.v.; Hollaar, V.; Naumann, E.; Schueren, M.d.v.d.; Jerković-Ćosić, K. The Association between Malnutrition and Oral Health in Older People: A Systematic Review. Nutrients 2021, 13, 3584. https://doi.org/10.3390/nu13103584
Algra Y, Haverkort E, Kok W, Etten-Jamaludin Fv, Schoot Lv, Hollaar V, Naumann E, Schueren Mdvd, Jerković-Ćosić K. The Association between Malnutrition and Oral Health in Older People: A Systematic Review. Nutrients. 2021; 13(10):3584. https://doi.org/10.3390/nu13103584
Chicago/Turabian StyleAlgra, Yne, Elizabeth Haverkort, Wilhelmina Kok, Faridi van Etten-Jamaludin, Liedeke van Schoot, Vanessa Hollaar, Elke Naumann, Marian de van der Schueren, and Katarina Jerković-Ćosić. 2021. "The Association between Malnutrition and Oral Health in Older People: A Systematic Review" Nutrients 13, no. 10: 3584. https://doi.org/10.3390/nu13103584
APA StyleAlgra, Y., Haverkort, E., Kok, W., Etten-Jamaludin, F. v., Schoot, L. v., Hollaar, V., Naumann, E., Schueren, M. d. v. d., & Jerković-Ćosić, K. (2021). The Association between Malnutrition and Oral Health in Older People: A Systematic Review. Nutrients, 13(10), 3584. https://doi.org/10.3390/nu13103584






