Abstract
Adipokines and gastrointestinal tract hormones are important metabolic parameters, and both epigenetic factors and differential gene expression patterns may be associated with the alterations in their concentrations in children. The function of the FTO gene (FTO alpha-ketoglutarate dependent dioxygenase) in the regulation of the global metabolic rate is well described, whereas the influence of protooncogene PLAG1 (PLAG1 zinc finger) is still not fully understood. A cross-sectional study on a group of 26 children with various BMI values (15.3–41.7; median 28) was carried out. The aim was to evaluate the dependencies between the level of methylation and expression of aforementioned genes with the concentration of selected gastrointestinal tract hormones and adipokines in children. Expression and methylation were measured in peripheral blood mononuclear DNA by a microarray technique and a restriction enzyme method, respectively. All peptide concentrations were determined using the enzyme immunoassay method. The expression level of both FTO and PLAG1 genes was statistically significantly related to the concentration of adipokines: negatively for apelin and leptin receptor, and positively for leptin. Furthermore, both FTO methylation and expression negatively correlated with the concentration of resistin and visfatin. Cholecystokinin was negatively correlated, whereas fibroblast growth factor 21 positively correlated with methylation and expression of the FTO gene, while FTO and PLAG1 expression was negatively associated with the level of cholecystokinin and glucagon-like peptide-1. The PLAG1 gene expression predicts an increase in leptin and decrease in ghrelin levels. Our results indicate that the FTO gene correlates with the concentration of hormones produced by the adipose tissue and gastrointestinal tract, and PLAG1 gene may be involved in adiposity pathogenesis. However, the exact molecular mechanisms still need to be clarified.
Keywords:
epigenetics; expression; FTO; PLAG1; children; adipokines; gastrointestinal tract hormones 1. Introduction
Adipokines and gastrointestinal peptides, secreted by fat tissue and enteroendocrine cells, respectively, are crucial factors regulating food intake, as well as glucose and lipid homeostasis. Consequently, they are strongly associated with both the development and implications of obesity—a condition currently becoming one of the major concerns in pediatrics. According to the WHO (World Health Organization) data, in 2016, the prevalence of obesity in the 5–19 age group was equal to 6.8% globally, 21.4% in the USA, and 9.1% in Poland [1,2]. Both epigenetic factors and differential gene expression patterns have been previously reported to be associated with the alterations in the concentrations of adipokines and gastrointestinal hormones [3,4,5,6,7,8,9,10,11]. In turn, such alterations can be considered to contribute to the development of obesity, to result from it, or to be associated with changes in BMI (body mass index) without known causality. Out of the hormones studied in this paper, those which are typically upregulated in obesity include leptin [12,13], visfatin [14,15], apelin [16] and FGF21 (fibroblast growth factor 21) [17] (although, in case of the last two, there are conflicting data regarding childhood adiposity [16,18,19,20,21,22]), whereas adiponectin [23,24,25], ghrelin [13,26] and, probably, GLP-1 (glucagon-like peptide-1) [27] are usually downregulated. In contrast, levels of resistin [28,29,30] and cholecystokinin (CCK) [31] do not seem to differ between obese and lean individuals.
The FTO gene (FTO alpha-ketoglutarate dependent dioxygenase) [32,33] has been extensively described as linked to obesity, both in adults and in children, as indicated by SNP (single nucleotide polymorphism) research [34,35,36], as well as epigenome-wide association studies [37,38] (according to EWAS Atlas [39]). Furthermore, there is a growing body of evidence for the existing connection between FTO and concentrations of certain adipokines and gastrointestinal peptides. Namely, FTO polymorphisms have been shown to be related to altered levels of leptin, adiponectin, apelin, resistin, visfatin, ghrelin and GLP-1 [40,41,42,43,44,45,46,47,48].
The protooncogene PLAG1 (PLAG1 zinc finger) [33,49] is associated with neoplasms such as lipoblastoma or pleomorphic adenoma of the salivary gland [50,51]. In addition, it is currently being explored as a novel gene connected with anthropometric parameters [52,53,54]. So far, there have been no studies investigating its relationship with the concentrations of gastrointestinal hormones. However, PLAG1 cord blood methylation, possibly affecting its expression, has been recently linked to neonatal levels of leptin [3].
In our previous study, we showed that the expression of the FTO gene is elevated in childhood obesity and, along with the methylation of this gene, predicts changes in certain parameters of glucose-lipid metabolism, thus further emphasizing the role of this gene in adiposity [55]. We also identified an association between the PLAG1 expression and body fat content, showing an involvement of this gene in determining body composition. Here, we aimed to further explore the role of these genes in the pathogenesis of childhood obesity and its complications by analyzing the correlation between their expression and circulating levels of leptin, soluble leptin receptor, adiponectin, apelin, resistin, visfatin, ghrelin, cholecystokinin, FGF21 and GLP-1. To adjust for the possible influence of confounders on the observed associations, we constructed a multiple linear regression model. Furthermore, to investigate the epigenetic background for changes in the levels of studied hormones, we analyzed them in the context of FTO gene methylation.
2. Materials and Methods
In total, 26 children (16 boys, 10 girls) aged 6.6–17.7 (median: 14.65) years were included in the analysis of the cross-sectional study. The inclusion criteria for the study were children aged below 18 years, and the absence of acute and chronic diseases, except for primary obesity. The mean BMI percentile of the group was 82.47 ± 30.02.
2.1. Microarray Analysis
Blood samples (1.5 mL) were collected from each child. Total RNA extraction from blood mononuclears was performed using the RiboPure Blood Kit (Ambion, Life Technologies, Carlsbad, CA, USA). Whole-genome expression was assessed using the GeneChip Human Gene 1.0 ST Arrays (Affymetrix, Santa Clara, CA, USA). All procedures were done following the manufacturer’s instructions (GeneChip Whole Transcript sense Target Labeling Assay Manual, Version 4, Affymetrix, Santa Clara, CA, USA). Despite the fact that the goal of the study was to investigate only two genes, expression was analyzed on a genome-wide level for the purpose of other research.
2.2. Methylation Analysis
2.2.1. DNA and Selection of Fragments
Genomic DNA was isolated from the peripheral blood using MasterPure DNA Purification Kit for Blood (Epicentre). FTO (Chr16) methylation (upstream, 16:53703684-53703899) was tested with the method based on methylation-dependent (MDRE) and methylation-sensitive (MSRE) restriction enzymes. MDREs detect regions of DNA that are highly methylated, oppositely to MSREs, which can target the regions with low degrees of methylation [56,57]. The regions of interest in both genes were established according to the methyl-DIP data available in the Ensembl database [58] (Supplementary Materials). The palindrome fragments containing CCGG targets for the MDRE and MSRE enzymes were used. Table 1 contains the sequences of each primer that was used in the qPCR. The primers were designed using PrimerQuest (Integrated DNA Technologies) [59]. For this, we evaluated the methylation level of PLAG1 gene, region 1 ((PLAG1 exon1) 8:56211059-56211208). We used the PLAG1 methylation to control for FTO. The genome reference sequence used was GRCh38.p13.

Table 1.
Sequences of primers used for the qPCR reaction.
2.2.2. Restriction Enzyme Digestion
For MSRE reaction, we used the HpaII enzyme in combination with MspI (EpiJET, Thermo). These enzymes are isoschizomers that target CCGG sequences. Methylated CpG sites are resistant to HpaII digestion but still prone to MspI cleavage. Digestions with both enzymes were carried out overnight at 37 °C and terminated at 90 °C for 10 min. Both methylated and unmethylated pUC19/SmaI DNA were used to determine the digestion ratio. A total of 50 ng and 100 ng of genomic DNA was cleaved by FspE (MDRE) and HpaII (MSRE), respectively. FspEI modification-dependent endonuclease was used as the MDRE (New England BioLabs, Ipswich, MA, USA). The reaction was carried out in 30 µL in the presence of 2.5 U of enzyme and reaction buffer supplemented with Enzyme Activator Solution and BSA. After 4 h of incubation at 37 °C, the reaction was stopped at 80 °C for 20 min.
2.2.3. qPCR
Real-time experiments were performed according to the MIQE guidelines. For all reactions, we applied intercalating dye chemistry with SYBR Green, as well as hot start iTaq DNA polymerase (iTaq Universal SYBR Green Supermix, Bio-Rad). All reactions were run in triplicate on the CFX384 Touch Real-Time PCR Detection System (Bio-Rad). On each reaction plate, serial dilutions of the control DNA were run to establish the PCR efficiency and correct calculations.
2.2.4. Methylation Data Processing and Statistical Analysis
All downstream data processing and statistical analyses were performed with the statistical software R [60] together with the methylumi and limma [61] packages of the Bioconductor project [62].
Moderated t-statistics for each contrast and probe were created using an empirical Bayes model as implemented in limma (eBayes command). The p-values were adjusted for multiple comparisons as proposed by Benjamini and Hochberg [63], and an adjusted p-value > 0.05 was considered nonsignificant (ns).
2.3. Study Protocol
Blood concentrations of CCK, ghrelin, GLP-1, adiponectin, apelin, leptin, leptin receptor, resistin and visfatin were measured at fasting, as well as at 60 and 120 min of the standard oral glucose tolerance test (OGTT) conducted using 1.75 g of anhydrous glucose per kg of body mass (maximum of 75 g). Both tubes that contained EDTA or aprotinin (BectonDickinson, Plymouth, UK) and tubes without anticoagulant were used in the blood sample collection process. The blood samples were immediately transported to the diagnostic laboratory at a temperature of +4 °C and centrifuged for 15 min at a relative centrifugal force of 1590× g.
2.4. Laboratory Measurements
We assessed the concentrations of various hormones by the EIA method: CCK, ghrelin, GLP-1 (Phoenix Pharmaceuticals, Inc., Burlingame, CA, USA) and FGF-21 (Millipore Corporation, Burlington, MA, USA). Plasma samples for adipokine and soluble leptin receptor analyses were stored at −80 °C until the time of the measurement. Plasma concentrations of the peptides were measured using the following assays: enzyme immunoassay (EIA) (Phoenix Pharmaceuticals, Burlingame, CA, USA)—adiponectin, apelin and visfatin; enzyme-amplified sensitivity immunoassay (Biosource; Nivelles, Belgium)—leptin; (EIA) (BioVendor Research and Diagnostic Products, Brno, Czech Republic)—leptin receptor and resistin.
2.5. Anthropometric Measurements
Body weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively, using a balanced scale and a stadiometer. All measurements were conducted by an anthropometrist. Online World Health Organization (WHO) BMI calculators were used to determine the body mass index (BMI), BMI percentile (BMI_Perc) and BMI SD [64].
2.6. Statistical Analysis
The interval data are presented as mean ± SD, while the categorical data are presented as frequencies (N) and proportions (%). If any data were missing, the case was not included in the analysis for the given variable. All area-under-the-curve (AUC) values were calculated by applying the trapezoidal rule. The Spearman’s correlation coefficient (r) was used to estimate the relationship between the interval variables.
Multivariate linear regression models incorporating the expression and the methylation of genes were constructed in attempt to identify a link between the FTO gene methylation, FTO gene expression and PLAG1 gene expression with the serum level of adipokines and gastrointestinal tract hormones. A standard threshold of p-value = 0.05 was used to determine data significance. The Benjamini–Hochberg (BH) procedure was used to correct for multiple testing (assuming FDR = 0.05), and an adjusted pBH < 0.05 was considered as significant. All analyzes were performed with Statistica 13.3 software (Statsoft Inc., Tulsa, OK, USA).
The study protocol gained the approval of the Permanent Ethical Committee for Clinical Studies of the Medical College of the Jagiellonian University (KBET/249/B/2013 26 October 2013). All parents, children and adults signed a written informed consent before blood sample collection. That study respects the statements of The Code of Ethics of the World Medical Association (Declaration of Helsinki), printed in the British Medical Journal (18 July 1964).
3. Results
The characteristics of the study groups are presented in Table 2. Our study included 16 boys and 10 girls (61.54%/38.46%). The mean age was 13.98 ± 2.6 years. The mean values of the anthropometric parameters were height: 164.85 ± 13.9 cm, weight: 76.62 ± 24.98 kg, BMI: 27.87 ± 7.48 kg/m2, BMI percentiles: 82.47 ± 30.02 and BMI SD: 4.35 ± 3.9. The percentage of the methylation level of the FTO gene was 4.35 ± 3.9%, while the methylation level of the PLAG1 gene was 0.8 ± 0.8%. However, for this region of PLAG1 gene, there was a large loss of data due to the low digestion rate of the samples. As a result, we did not include the studied parameter in further analysis. Mean FTO expression was 266.72 ± 87.46, while PLAG1 expression was 82 ± 21.73. The exact concentrations of the adipokines and gastrointestinal hormones, as well as the values of the methylation and expression of genes, are given in Table 3 and Table S1.

Table 2.
Characteristics of the study group. Values are presented as mean ± standard deviation.

Table 3.
The metabolic parameters of the study group. Values are presented as mean ± standard deviation.
3.1. Spearman’s Correlation Results of Adipokines with FTO Gene Methylation, Expression and PLAG1 Gene Expression
In the case of the FTO gene methylation level, Spearman′s correlation coefficient r was insignificant.
By analyzing the FTO expression, a statistically significant correlation was obtained for apelin (AUC apelin r = −0.758, pBH < 0.001), leptin (AUC leptin r = 0.713, pBH < 0.001), leptin receptor (leptin receptor r = −0.622, pBH = 0.005) and resistin (resistin -OGTT 60 min r = −0.507, pBH = 0.020). Detailed information on the investigated parameters is presented in Table 4 and Table S2.

Table 4.
Correlation results of the adipokines serum levels with the FTO gene methylation, expression and PLAG1 gene expression.
According to our observations, the PLAG1 expression was associated with the serum concentration of apelin (AUC apelin r = −0.579, pBH = 0.014), leptin (AUC leptin r = 0.676, pBH = 0.002) and soluble leptin receptor (AUC leptin receptor r = −0.488, pPH = 0.04). Detailed data are presented in Table 4.
3.2. Spearman’s Correlation Results of Gastrointestinal Tract Hormones with FTO Gene Methylation, Expression and PLAG1 Gene Expression
The level of FTO gene methylation correlated with the plasma concentration of cholecystokinin (AUC CCK r = −0.508, pBH = 0.044) and FGF21 (AUC FGF r = 0.556, pBH = 0.04). In the case of the FTO gene expression level, a correlation was demonstrated for the plasma levels of cholecystokinin (AUC CCK r = −0.613, pBH = 0.044), FGF21 (AUC FGF21 r = 0.525, pBH = 0.016) and GLP-1 (AUC GLP-1 r = −0.638, pBH = 0.003). The level of PLAG1 expression did not correlate with gastrointestinal tract hormones serum levels. Detailed information on these dependencies is presented in Table 5 and Table S3.

Table 5.
Correlation results of the gastrointestinal tract hormones serum levels with the FTO gene methylation, expression and PLAG1 gene expression.
3.3. Multiple Linear Regression Model Explaining the Effect of FTO Gene Methylation, FTO Gene Expression and PLAG1 Gene Expression on the Plasma Concentrations of Adipokines and Gastrointestinal Tract Hormones
To assess the impact of the FTO gene methylation, FTO gene expression and PLAG1 gene expression on the plasma adipokines and gastrointestinal tract hormones, a linear regression model was created to investigate these relationships (additionally considering the sex of the subjects). In such a model, the FTO gene methylation level showed an effect on the AUC of CCK (B = −0.25 ± 0.12, p = 0.05), AUC of FGF21 (B = 20.51 ± 8.31, p = 0.023) and AUC of ghrelin (B = −39.47 ± 16.94, p = 0.032). FTO expression, on the other hand, affected the AUC of apelin (B = −1.09 ± 0.51, p = 0.045), AUC of adiponectin (B = 1.94 ± 0.80, p = 0.028), AUC of GLP-1 (B = −0.25 ± 0.1, p = 0.020) and AUC of leptin receptor (B = −4.00 ± 1.83, p = 0.041). The PLAG1 expression affected the AUC of ghrelin (B = −99.6 ± 33.3, p = 0.008) and AUC of leptin (B = 10.44 ± 4.12, p = 0.020). The exact results of the tested model are shown in Table 6.

Table 6.
Multiple linear regression analysis of the FTO gene methylation, FTO gene expression and PLAG1 expression as predictors of changes in the plasma concentrations of adipokines and gastrointestinal tract hormones in children. Only the non-standardized regression coefficients 1 with p < 0.05 are shown.
4. Discussion
In our previous research, we demonstrated differences in the methylation and expression of the FTO gene between healthy and obese children [55]. In the current study, we showed that the expression and methylation level of the FTO gene and the expression of the PLAG1 gene are related to the concentrations of selected adipokines and gastrointestinal tract hormones. Finally, we conducted a multiple linear regression analysis to predict the changes in lipid metabolism parameters in children based on the FTO and PLAG1 genes. Our key findings, together with the hypothetical interactions explaining them, are illustrated in Figure 1.
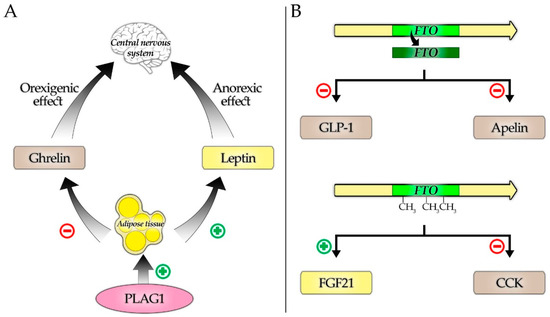
Figure 1.
Suggested mechanisms of interactions between the studied genes and hormones. (A) Regulation of ghrelin and leptin, key appetite and satiety controlling hormones by PLAG1, secondary to its fat tissue stimulating properties. (B) Selected hormones downregulated in response to the increased FTO expression (upper part) and influenced by the higher FTO methylation (down part).
4.1. FTO Gene
The FTO Alpha-Ketoglutarate Dependent Dioxygenase, based on the GeneCards—The Human Genes Database [65,66,67], belongs to a nuclear protein of the AlkB-related non-haem iron and 2-oxoglutarate-dependent oxygenase superfamily. Its exact physiological function is unknown. However, it has strong association with body mass index, obesity risk and type 2 diabetes (DM2) [67]. It regulates adipogenesis and body fat accumulation, thereby contributing to the regulation of body size and weight [68,69,70,71,72]. These findings suggest the existence of a relationship between the FTO gene and adipokines and gastrointestinal tract hormones. However, the expression and methylation of the FTO gene have not been described yet. In our previous study, we found that the obese children showed significantly higher expression of the FTO gene in comparison to the healthy controls, as well as significantly higher methylation values for the FTO gene [55], which confirmed a considerable role of the FTO gene in the development of obesity.
In our study, we showed that higher level of both FTO gene methylation and expression in children was associated with a decreased serum concentrations of adipokines and gastrointestinal tract hormones during fasting and after the oral glucose tolerance test, although the obtained data was not always statistically significant. Only two hormones—leptin and FGF-21—correlated positively with the expression and methylation of the FTO gene, and these results were statistically significant. Thus, it seems that the FTO gene may be an important factor regulating the mechanism of changes in the concentration of adipokines and gastrointestinal tract hormones in children. Namely, we hypothesize that higher expression of this gene causes an inhibition of the production or secretion of tissue hormones, and, as a consequence, a decrease in their circulating levels.
4.1.1. FTO and Adipokines
We showed a statistically significant relationship between the FTO gene expression and the concentrations of apelin, leptin, leptin receptor and resistin, while the relationship with the adiponectin and visfatin concentrations were not significant. In case of the FTO gene methylation, its correlation with the visfatin concentration was statistically significant, both during fasting and after OGTT, as was the association with the concentration of resistin, but only after the OGTT test. However, after the Benjamini-Hochberg adjustment, these results lost their statistical significance, similar to the remaining results.
Leptin, as one of the only adipokines analyzed in our study, correlated positively with the expression of the FTO gene. Leptin is a main protein regulating energy homeostasis in the body, inhibiting feeding and promoting energy expenditure. Moreover, mutation in its gene causes severe or morbid obesity with hypogonadism in humans [66,67]. The leptin receptor, in turn, is a receptor for leptin, and is involved in the regulation of fat metabolism [66,67]. In contrast to leptin, its concentration correlated negatively with the FTO gene expression. Leptin is among factors which are the most potently upregulated in response to fat tissue accumulation, and the FTO expression is higher in obese children. Combined, those two facts may explain the observed association, despite the supposed inhibitory action of FTO on the production or secretion of adipokines. The found opposite correlations of FTO gene expression with leptin and the leptin receptor could be explained by the downregulation mechanism caused by the higher leptin concentration, causing the saturation of its receptor and, consequently, a decrease in its availability. The relationship of the rs9939609 FTO gene variant with the highest leptin concentration has been well described independently of potential confounders, including in subjects with adiposity [40,41,42,73].
The relationship between the FTO gene and the concentration of apelin is very interesting. In our study, apelin correlated negatively with the FTO expression, both during fasting and after OGGT. Apelin is responsible for, i.a., cardiovascular function and insulin secretion, and its functional disorders are associated with DM2 and cardiovascular system diseases [66,67]. Most of the current data indicate that apelin levels increase with increasing BMI [22,74]. However, these data refer to prepubertal children or adults. In children in adolescence, the situation looks different, and in pubertal obese children, the apelin level may be lower compared to non-obese children [21]. Another factor that causes an increase in the apelin levels is physical activity. After an intense 12-week exercise period, people with DM2 experienced a significant increase in plasma apelin levels [75]. Son et al. showed that there is a positive correlation between plasma apelin concentration and lean body mass after intense physical activity [76]. The concentration of apelin is also significantly higher in people with an active lifestyle compared to a sedentary lifestyle [77]. Our observations showed that the increase in the FTO expression may be one of the predictors of the apelin serum level, which may have a beneficial effect on the lipid profile and carbohydrate metabolism of patients. It is worth noting that the concentration of apelin in adolescents may act differently than in people of a different age. Furthermore, additional factors, such as lifestyle or physical exercise, have an influence on the concentration of apelin.
The data concerning the FTO gene and both resistin and visfatin levels are inconsistent. Resistin is a hormone potentially linking obesity to DM2 [66,67]. We obtained statistically significant data for resistin correlated with the expression of the FTO gene, but only after the OGTT test. Thus, it is likely that the fasting resistin concentration is not related to the FTO gene, but that the resistin release as a result of loading with a carbohydrate meal is associated with the FTO gene. Visfatin is involved as a protein in many important biological processes, including metabolism. Serum visfatin was nearly significantly negatively correlated with the FTO expression at 60 min of OGTT and in the case of the AUC parameter. The lack of unambiguous data on changes in the concentrations of visfatin and resistin in adolescents with different body weight may indicate the existence of a more direct relationship and regulatory mechanism between the FTO gene and concentrations of both of the hormones.
Adiponectin is involved in the control of fat metabolism and insulin sensitivity, with direct anti-diabetic, anti-atherogenic and anti-inflammatory activities. It is also associated with disorders of the adipose tissue and insulin metabolism [66,67]. In our studies, adiponectin did not show a significant correlation with the FTO gene. However, all the correlations we obtained with the FTO gene were negative. The reason for poor correlation in our study may be attributed to the small patient group. In contrast, the study of the rs9939609 variant by Duicu et al. was performed on a group which consisted of about 400 children [42]. Further research into the FTO gene and adiponectin concentration is necessary.
4.1.2. FTO and Gastrointestinal Tract Hormones
The FTO gene is strongly associated with body mass index, obesity risk, the regulation of fat mass, body size, body fat accumulation and body weight [66,67]. Therefore, its interaction with gastrointestinal hormones, responsible for the feeling of hunger and satiety and food intake control, may play a key role in understanding the mechanisms leading to obesity. In our study, three of the four tested gastrointestinal tract hormones (CCK, GLP-1 and ghrelin) were negatively correlated with FTO gene. Only FGF21 correlated positively. The results were statistically significant during fasting and after the OGTT test for both the methylation and expression of FTO gene for CCK and FGF21, and in the case of GLP-1 for FTO expression only.
We obtained the negative correlation between the concentration of cholecystokinin and FTO gene methylation, as well as the FTO expression, at every timepoint we studied. These results may be explained by the fact that cholecystokinin induces satiety by interacting with the CCK-1 receptors located in specialized regions of the hindbrain [78]. We showed that higher expression of the FTO gene occurs usually in people with higher BMI, in whom the process of activating the satiety center may be disturbed. Therefore, this association may result from the pre-existing eating disorders. It is also supported by the fact that CCK is the main protein in the regulation of energy intake in the organism [79]. However, it is worth mentioning that, in our study, in the multiple linear regression analysis for the FTO gene, the methylation of the FTO gene was the best predictor of CCK plasma concentrations among all studied gastrointestinal tract hormones in children.
Glucagon-like peptide 1 is a peptide hormone formed in the intestinal epithelial endocrine L-cells in the differential processing of proglucagon. Its main action is to stimulate insulin secretion and to inhibit glucagon secretion, thereby limiting postprandial glucose excursions [80]. We found a strong negative correlation between the FTO gene expression and GLP-1 concentration both during fasting and after the OGTT test. It is possible that, in addition to genetic factors, including the FTO gene, environmental factors and physical activity have a significant impact on GLP-1 concentration. However, this be studied as the subject of further research.
In the case of ghrelin, the negative correlation we found was not statistically significant. Ghrelin is a powerful appetite stimulant, which plays an important role in energy homeostasis. It is secreted when the stomach is empty, and then binds to the growth hormone secretagogue receptor in the hypothalamus, causing causes the secretion of the growth hormone [66,67]. These facts may suggest that ghrelin could be related to the FTO gene, but the available data are contradictory. Magno et al., studying the FTO rs9939609 polymorphism, showed that the subject with AA genotype indeed had decreased postprandial ghrelin concentration [46]. In contrast, Danaher et al. did not confirm the relationship between the rs9939609 polymorphism of the FTO gene and the preprandial or postprandial ghrelin level [81]. These various reports may highlight the complexity of the interaction mechanisms between FTO and ghrelin, but more research is needed to fully understand them.
FGF21 is a protein that stimulates the uptake of glucose in adipose tissue. An FGF21 disturbance may cause, i.a., acquired lipodystrophy [66,67]. It was the only gastrointestinal tract hormone for which we showed the positive correlation with both FTO gene expression and FTO methylation. The association was observed during fasting and after the OGTT test, as well as for the AUC parameter. The genome-wide meta-analysis by Tanaka et al. showed that both the FTO and FGF21 genes are very strongly connected to food intake regulation [82]. Therefore, it appears that both genes may well reflect the degree of eating disorder in children, and perhaps even predict this condition, acting synergistically.
4.2. PLAG1 Gene
The PLAG1 (PLAG1 zinc finger) is a protooncogene encoding a protein with two putative nuclear localization signals, which functions as a transcription factor. It is responsible for the upregulation of genes such as IGF2, CRABP2, CRLF1, PIGF and CRIP2. The PLAG1 function triggers cellular proliferation and is associated with the development of lipoblastomas and pleomorphic adenomas of the salivary gland [50,51,66,83]. It is also commonly overexpressed in AML (acute myeloid leukemia) and hepatoblastoma [84,85]. In addition, studies have indicated that PLAG1 could contribute to the determination of body composition. According to the GWAS Catalog [86,87], PLAG1 polymorphisms are associated with traits such as birth weight [52], lean body mass [53] and BMI-adjusted hip circumference [54]. In our previous research, we showed that PLAG1 expression correlated positively with body fat percent in children [55]. The possible involvement of PLAG1 in fat tissue growth suggests that it could also influence the amount of synthesized adipokines. Similarly, the concentrations of gastrointestinal tract hormones, which regulate food intake, thereby also affecting body composition, could be associated with PLAG1 function.
4.2.1. PLAG1 and Adipokines
In our study, we showed that the PLAG1 expression correlated with levels of certain adipokines measured during OGTT—positively in the case of leptin, and negatively in the case of the leptin receptor and apelin. However, the multiple linear regression analysis revealed that an association independent of confounders occurred only in case of leptin concentration. There were no statistically significant outcomes regarding the concentrations of adiponectin, resistin and visfatin.
Kadakia et al. found that higher cord blood methylation of the PLAG1 gene, probably resulting in the inhibition of its expression, is associated with lower leptin levels [3]. Our results further confirm the likely existence of a link between these two factors. Concentrations of IGF-2, the key PLAG1 target gene, were shown to be higher in children with obesity compared to the control group [88], and were found to be associated with increased leptin levels in adult, normal-weight patients [89]. However, Kleiman et al. showed that leptin expression is inhibited, rather than promoted, by IGF-2 [90]. These conflicting results suggest that a pathway linking PLAG1 to leptin could be independent of IGF-2. However, it remains unclear whether there is a direct mechanism connecting PLAG1 to leptin synthesis on a molecular level. Therefore, the most likely reason for the found association is the aforementioned increase in the fat tissue content related to PLAG1 expression, which ultimately results in augmented leptin production (Figure 1). The aforementioned mechanism of leptin receptor being downregulated by the increased concentration of its ligand could also explain the found negative correlation between the PLAG1 expression and leptin receptor levels.
An observed negative correlation between the PLAG1 expression and apelin concentration was not confirmed by multiple linear regression analysis. We suppose that this correlation is unlikely to arise from a simple interaction between the PLAG1 and apelin systems, but rather results from one of the possible confounders which could alter apelin levels, such as low physical activity [77]. Furthermore, Reinehr et al. showed that apelin concentrations in children did not vary depending on BMI or body fat percent [20], which could explain why PLAG1 expression does not cause an increase in apelin production despite being associated with higher fat tissue content.
4.2.2. PLAG1 and Gastrointestinal Tract Hormones
The construction of multiple linear regression model revealed a negative association between the PLAG1 expression and concentrations of ghrelin. The levels of CCK, GLP-1 and FGF21 did not correlate significantly with the expression of PLAG1.
Ghrelin concentrations are typically decreased in obesity, except for Prader–Willi syndrome, where elevated ghrelin secretion is considered one of the factors leading to overeating [13,26]. The obesity-associated reduction in levels of ghrelin, which is an orexigenic factor, could be considered a compensatory mechanism aimed to prevent further weight gain [91]. A negative correlation between the body fat percent and ghrelin levels, which was reported in a study by Tschöp et al. [26], provides a very clear explanation of our obtained results given the known association of PLAG1 and fat tissue content (Figure 1). Reduced ghrelin concentration in adiposity most likely results from the decreased sensitivity of ghrelin-producing cells in the stomach to noradrenalin, which normally stimulates ghrelin secretion, or from the increased abundance of duodenal somatostatin cells, resulting in an augmented somatostatin-mediated suppression of ghrelin cells [13,91]. The exact mechanism linking increased fat content and, therefore, PLAG1, to the described processes leading to decreased ghrelin levels is yet to be elucidated.
4.3. Limitations
The study population of 26 participants yields a relatively small cohort, which could possibly undermine the validity of the outcomes. Future studies using larger samples are required for definite confirmation of the obtained results.
Out of the two studied genes, the analysis included the methylation data only for the FTO gene. The PLAG1 methylation was not included in the calculations due to the fact that the CpG sites within this gene, which we initially intended to investigate, proved to be of no influence on the expression of the gene [55].
Although analyzing gene expression in peripheral blood mononuclear cells in nutrigenomic research is supported by studies [92,93,94], there is a risk that the outcomes could be affected by variations in the proportions of cell types comprising the mononuclear cells. Similarly, the methylation results could be influenced by differences in the proportions of the cell types in the whole blood.
5. Conclusions
Higher expression and, in selected cases, methylation of the FTO gene, lowers the levels of adipokines and gastrointestinal tract hormones in children. This effect is especially clear for apelin, resistin, leptin receptor, cholecystokinin and GLP-1. In contrast, the serum levels of leptin and FGF21 increase in the context of increasing the FTO expression. All these factors are crucial in weight gain and obesity development.
We also showed that the PLAG1 gene expression predicts an increase in leptin and decrease in ghrelin levels, with both hormones being key regulators of appetite and satiety. PLAG1 may be involved in certain aspects of obesity pathogenesis. However, its role in the development of childhood adiposity may be more complex.
This is the first study linking the adipokines and gastrointestinal hormones concentrations with the expression of PLAG1 and FTO genes. To confirm the results and to discover the exact molecular mechanisms of the found associations, further research including larger populations is necessary.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13103585/s1, Methylation regions, Table S1: The metabolic parameters of the study group (including values at OGTT time points), Table S2: Correlation results of adipokines serum levels with FTO gene methylation, expression and PLAG1 gene expression (including values at OGTT time points), Table S3: Correlation results of gastrointestinal tract hormones serum levels with FTO gene methylation, expression and PLAG1 gene expression (including values at OGTT time points).
Author Contributions
Conceptualization, S.S. and W.C.; methodology, S.S., W.C., A.G., W.S. and M.S.; validation, A.G. and P.T.; formal analysis, W.C., S.S., K.M., W.K., A.Ł. and A.G.; investigation, W.C., M.S., W.S., S.S. and P.T.; data curation, S.S. and W.C., writing—original draft preparation, W.C., S.S., K.M., W.K. and A.Ł.; writing—review and editing, W.C., S.S., M.S., W.S. and A.G.; visualization, K.M., W.K. and A.Ł.; supervision, W.C. and S.S.; project administration, W.C. and S.S.; funding acquisition, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Science Centre under grant number NN 407 198737 and University Grant K/ZDS/003825.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the The Permanent Ethical Committee for Clinical Studies of the Jagiellonian University Medical College (KBET/249/B/2013 26 October 2013).
Informed Consent Statement
All parents, children, and adults signed a written informed consent before blood sample collection.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Acknowledgments
All authors are grateful to the study participants and their parents.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Overweight/Obesity. Available online: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/overweight-obesity (accessed on 9 May 2021).
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; Lu, Y.; et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Kadakia, R.; Zheng, Y.; Zhang, Z.; Zhang, W.; Josefson, J.L.; Hou, L. Association of Cord Blood Methylation with Neonatal Leptin: An Epigenome Wide Association Study. PLoS ONE 2019, 14, e0226555. [Google Scholar] [CrossRef] [Green Version]
- Aslibekyan, S.; Do, A.N.; Xu, H.; Li, S.; Irvin, M.R.; Zhi, D.; Tiwari, H.K.; Absher, D.M.; Shuldiner, A.R.; Zhang, T.; et al. CPT1A Methylation Is Associated with Plasma Adiponectin. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 225–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakatochi, M.; Ichihara, S.; Yamamoto, K.; Ohnaka, K.; Kato, Y.; Yokota, S.; Hirashiki, A.; Naruse, K.; Asano, H.; Izawa, H.; et al. Epigenome-Wide Association Study Suggests That SNPs in the Promoter Region of RETN Influence Plasma Resistin Level via Effects on DNA Methylation at Neighbouring Sites. Diabetologia 2015, 58, 2781–2790. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Kohli, S.; Dua, S.; Thinlas, T.; Mohammad, G.; Pasha, M.A.Q. Genetic Differences and Aberrant Methylation in the Apelin System Predict the Risk of High-Altitude Pulmonary Edema. Proc. Natl. Acad. Sci. USA 2015, 112, 6134–6139. [Google Scholar] [CrossRef] [Green Version]
- Wiemerslage, L.; Islam, R.; Van Der Kamp, C.; Cao, H.; Olivo, G.; Ence-Eriksson, F.; Castillo, S.; Larsen, A.L.; Bandstein, M.; Dahlberg, L.S.; et al. A DNA Methylation Site within the KLF13 Gene Is Associated with Orexigenic Processes Based on Neural Responses and Ghrelin Levels. Int. J. Obes. 2017, 41, 990–994. [Google Scholar] [CrossRef]
- Li, P.; Gao, X.; Sun, X.; Li, W.; Yi, B.; Zhu, L. A Novel Epigenetic Mechanism of FXR Inhibiting GLP-1 Secretion via MiR-33 and Its Downstream Targets. Biochem. Biophys. Res. Commun. 2019, 517, 629–635. [Google Scholar] [CrossRef]
- Płatek, T.; Polus, A.; Góralska, J.; Raźny, U.; Dziewońska, A.; Micek, A.; Dembińska-Kieć, A.; Solnica, B.; Malczewska-Malec, M. Epigenetic Regulation of Processes Related to High Level of Fibroblast Growth Factor 21 in Obese Subjects. Genes 2021, 12, 307. [Google Scholar] [CrossRef]
- Chandra, R.; Wang, Y.; Shahid, R.A.; Vigna, S.R.; Freedman, N.J.; Liddle, R.A. Immunoglobulin-like Domain Containing Receptor 1 Mediates Fat-Stimulated Cholecystokinin Secretion. J. Clin. Investig. 2013, 123, 3343–3352. [Google Scholar] [CrossRef] [Green Version]
- Osinski, C.; Le Gléau, L.; Poitou, C.; de Toro-Martin, J.; Genser, L.; Fradet, M.; Soula, H.A.; Leturque, A.; Blugeon, C.; Jourdren, L.; et al. Type 2 Diabetes Is Associated with Impaired Jejunal Enteroendocrine GLP-1 Cell Lineage in Human Obesity. Int. J. Obes. 2021, 45, 170–183. [Google Scholar] [CrossRef]
- Reinehr, T.; Kratzsch, J.; Kiess, W.; Andler, W. Circulating Soluble Leptin Receptor, Leptin, and Insulin Resistance before and after Weight Loss in Obese Children. Int. J. Obes. 2005, 29, 1230–1235. [Google Scholar] [CrossRef] [Green Version]
- Cui, H.; López, M.; Rahmouni, K. The Cellular and Molecular Bases of Leptin and Ghrelin Resistance in Obesity. Nat. Rev. Endocrinol. 2017, 13, 338–351. [Google Scholar] [CrossRef]
- Kamińska, A.; Kopczyńska, E.; Bronisz, A.; Żmudzińska, M.; Bieliński, M.; Borkowska, A.; Tyrakowski, T.; Junik, R. An Evaluation of Visfatin Levels in Obese Subjects. Endokrynol. Pol. 2010, 61, 169–173. [Google Scholar]
- Taşkesen, D.; Kirel, B.; Us, T. Serum Visfatin Levels, Adiposity and Glucose Metabolism in Obese Adolescents. J. Clin. Res. Pediatr. Endocrinol. 2012, 4, 76–81. [Google Scholar] [CrossRef]
- Castan-Laurell, I.; Dray, C.; Attané, C.; Duparc, T.; Knauf, C.; Valet, P. Apelin, Diabetes, and Obesity. Endocrine 2011, 40, 1–9. [Google Scholar] [CrossRef]
- Zhang, X.; Yeung, D.C.Y.; Karpisek, M.; Stejskal, D.; Zhou, Z.G.; Liu, F.; Wong, R.L.C.; Chow, W.S.; Tso, A.W.K.; Lam, K.S.L.; et al. Serum FGF21 Levels Are Increased in Obesity and Are Independently Associated with the Metabolic Syndrome in Humans. Diabetes 2008, 57, 1246–1253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baek, J.; Nam, H.-K.; Rhie, Y.-J.; Lee, K.-H. Serum FGF21 Levels in Obese Korean Children and Adolescents. J. Obes. Metab. Syndr. 2017, 26, 204–209. [Google Scholar] [CrossRef] [Green Version]
- Li, G.; Yin, J.; Fu, J.; Li, L.; Grant, S.F.A.; Li, C.; Li, M.; Mi, J.; Li, M.; Gao, S. FGF21 Deficiency Is Associated with Childhood Obesity, Insulin Resistance and Hypoadiponectinaemia: The BCAMS Study. Diabetes Metab. 2017, 43, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Woelfle, J.; Roth, C.L. Lack of Association between Apelin, Insulin Resistance, Cardiovascular Risk Factors, and Obesity in Children: A Longitudinal Analysis. Metabolism 2011, 60, 1349–1354. [Google Scholar] [CrossRef]
- Tapan, S.; Tascilar, E.; Abaci, A.; Sonmez, A.; Kilic, S.; Erbil, M.K.; Ozcan, O. Decreased Plasma Apelin Levels in Pubertal Obese Children. J. Pediatr. Endocrinol. Metab. 2010, 23, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Vehapoglu, A.; Ustabas, F.; Ozgen, T.I.; Terzioglu, S.; Cermik, B.B.; Ozen, O.F. Role of Circulating Adipocytokines Vaspin, Apelin, and Visfatin in the Loss of Appetite in Underweight Children: A Pilot Trial. J. Pediatr. Endocrinol. Metab. 2015, 28, 1065–1071. [Google Scholar] [CrossRef]
- Weiss, R.; Dufour, S.; Groszmann, A.; Petersen, K.; Dziura, J.; Taksali, S.E.; Shulman, G.; Caprio, S. Low Adiponectin Levels in Adolescent Obesity: A Marker of Increased Intramyocellular Lipid Accumulation. J. Clin. Endocrinol. Metab. 2003, 88, 2014–2018. [Google Scholar] [CrossRef] [Green Version]
- Araki, S.; Dobashi, K.; Kubo, K.; Asayama, K.; Shirahata, A. High Molecular Weight, Rather than Total, Adiponectin Levels Better Reflect Metabolic Abnormalities Associated with Childhood Obesity. J. Clin. Endocrinol. Metab. 2006, 91, 5113–5116. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.S.; Lee, W.J.; Funahashi, T.; Tanaka, S.; Matsuzawa, Y.; Chao, C.L.; Chen, C.L.; Tai, T.Y.; Chuang, L.M. Plasma Adiponectin Levels in Overweight and Obese Asians. Obes. Res. 2002, 10, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Tschöp, M.; Weyer, C.; Tataranni, P.A.; Devanarayan, V.; Ravussin, E.; Heiman, M.L. Circulating Ghrelin Levels Are Decreased in Human Obesity. Diabetes 2001, 50, 707–709. [Google Scholar] [CrossRef] [Green Version]
- Hira, T.; Pinyo, J.; Hara, H. What Is GLP-1 Really Doing in Obesity? Trends Endocrinol. Metab. 2020, 31, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Boettner, A.; Seidel, B.; Lammert, A.; Bär, J.; Schuster, E.; Thiery, J.; Kiess, W.; Kratzsch, J. Serum Resistin Levels of Obese and Lean Children and Adolescents: Biochemical Analysis and Clinical Relevance. J. Clin. Endocrinol. Metab. 2005, 90, 4503–4509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.H.; Chan, J.L.; Yiannakouris, N.; Kontogianni, M.; Estrada, E.; Seip, R.; Orlova, C.; Mantzoros, C.S. Circulating Resistin Levels Are Not Associated with Obesity or Insulin Resistance in Humans and Are Not Regulated by Fasting or Leptin Administration: Cross-Sectional and Interventional Studies in Normal, Insulin-Resistant, and Diabetic Subjects. J. Clin. Endocrinol. Metab. 2003, 88, 4848–4856. [Google Scholar] [CrossRef] [Green Version]
- Zou, C.C.; Liang, L.; Hong, F.; Fu, J.F.; Zhao, Z.Y. Serum Adiponectin, Resistin Levels and Non-Alcoholic Fatty Liver Disease in Obese Children. Endocr. J. 2005, 52, 519–524. [Google Scholar] [CrossRef] [Green Version]
- Rehfeld, J.F. Measurement of Cholecystokinin in Plasma with Reference to Nutrition Related Obesity Studies. Nutr. Res. 2020, 76, 1–8. [Google Scholar] [CrossRef]
- FTO Gene Symbol Report | HUGO Gene Nomenclature Committee. Available online: https://www.genenames.org/data/gene-symbol-report/#!/hgnc_id/HGNC:24678 (accessed on 14 May 2021).
- Tweedie, S.; Braschi, B.; Gray, K.; Jones, T.E.M.; Seal, R.L.; Yates, B.; Bruford, E.A. Genenames.Org: The HGNC and VGNC Resources in 2021. Nucleic Acids Res. 2021, 49, D939–D946. [Google Scholar] [CrossRef]
- Frayling, T.M.; Timpson, N.J.; Weedon, M.N.; Zeggini, E.; Freathy, R.M.; Lindgren, C.M.; Perry, J.R.B.; Elliott, K.S.; Lango, H.; Rayner, N.W.; et al. A Common Variant in the FTO Gene Is Associated with Body Mass Index and Predisposes to Childhood and Adult Obesity. Science 2007, 316, 889–894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Justice, A.E.; Chittoor, G.; Blanco, E.; Graff, M.; Wang, Y.; Albala, C.; Santos, J.L.; Angel, B.; Lozoff, B.; Voruganti, V.S.; et al. Genetic Determinants of BMI from Early Childhood to Adolescence: The Santiago Longitudinal Study. Pediatr. Obes. 2019, 14. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.E.R.; Andrade, N.L.; de Oliveira Cunha, D.; Leão-Cordeiro, J.A.B.; Vilanova-Costa, C.A.S.T.; Silva, A.M.T.C. The FTO Rs9939609 Polymorphism and Obesity Risk in Teens: Evidence-Based Meta-Analysis. Obes. Res. Clin. Pract. 2018, 12, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Monteiro, C.; Matos, A.; You, J.; Fraga, A.; Pereira, C.; Catalán, V.; Rodríguez, A.; Gómez-Ambrosi, J.; Frühbeck, G.; et al. Epigenome-Wide DNA Methylation Profiling of Periprostatic Adipose Tissue in Prostate Cancer Patients with Excess Adiposity-a Pilot Study. Clin. Epigenetics 2018, 10, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirchner, H.; Sinha, I.; Gao, H.; Ruby, M.A.; Schönke, M.; Lindvall, J.M.; Barrès, R.; Krook, A.; Näslund, E.; Dahlman-Wright, K.; et al. Altered DNA Methylation of Glycolytic and Lipogenic Genes in Liver from Obese and Type 2 Diabetic Patients. Mol. Metab. 2016, 5, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zou, D.; Li, Z.; Gao, R.; Sang, J.; Zhang, Y.; Li, R.; Xia, L.; Zhang, T.; Niu, G.; et al. EWAS Atlas: A Curated Knowledgebase of Epigenome-Wide Association Studies. Nucleic Acids Res. 2019, 47, D983–D988. [Google Scholar] [CrossRef] [PubMed]
- Mehrdad, M.; Doaei, S.; Gholamalizadeh, M.; Fardaei, M.; Fararouei, M.; Eftekhari, M.H. Association of FTO Rs9939609 Polymorphism with Serum Leptin, Insulin, Adiponectin, and Lipid Profile in Overweight Adults. Adipocyte 2020, 9, 51–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genis-Mendoza, A.D.; Martínez-Magaña, J.J.; Ruiz-Ramos, D.; Gonzalez-Covarrubias, V.; Tovilla-Zarate, C.A.; Narvaez, M.L.L.; Castro, T.B.G.; Juárez-Rojop, I.E.; Nicolini, H. Interaction of FTO Rs9939609 and the Native American-Origin ABCA1 p.Arg230Cys with Circulating Leptin Levels in Mexican Adolescents Diagnosed with Eating Disorders: Preliminary Results. Psychiatry Res. 2020, 291, 113270. [Google Scholar] [CrossRef]
- Duicu, C.; MǍrginean, C.O.; VoidǍzan, S.; Tripon, F.; BǍnescu, C. FTO Rs 9939609 SNP Is Associated with Adiponectin and Leptin Levels and the Risk of Obesity in a Cohort of Romanian Children Population. Medicine (Baltimore) 2016, 95, e3709. [Google Scholar] [CrossRef]
- Ghafarian-Alipour, F.; Ziaee, S.; Ashoori, M.R.; Zakeri, M.S.; Boroumand, M.A.; Aghamohammadzadeh, N.; Abbasi-Majdi, M.; Shool, F.; Asbaghi, N.S.; Mohammadi, A.; et al. Association between FTO Gene Polymorphisms and Type 2 Diabetes Mellitus, Serum Levels of Apelin and Androgen Hormones among Iranian Obese Women. Gene 2018, 641, 361–366. [Google Scholar] [CrossRef]
- Majdi, M.A.; Mohammadzadeh, N.A.; Lotfi, H.; Mahmoudi, R.; Alipour, F.G.; Shool, F.; Moghanloo, M.N.; Porfaraj, S.; Zarghami, N. Correlation of Resistin Serum Level with Fat Mass and Obesity-Associated Gene (FTO) Rs9939609 Polymorphism in Obese Women with Type 2 Diabetes. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, S715–S720. [Google Scholar] [CrossRef]
- López-Bermejo, A.; Petry, C.J.; Díaz, M.; Sebastiani, G.; De Zegher, F.; Dunger, D.B.; Ibáñez, L. The Association between the FTO Gene and Fat Mass in Humans Develops by the Postnatal Age of Two Weeks. J. Clin. Endocrinol. Metab. 2008, 93, 1501–1505. [Google Scholar] [CrossRef] [Green Version]
- Magno, F.C.C.M.; Guaraná, H.C.; Fonseca, A.C.P.; Cabello, G.M.K.; Carneiro, J.R.I.; Pedrosa, A.P.; Ximenes, A.C.; Rosado, E.L. Influence of FTO Rs9939609 Polymorphism on Appetite, Ghrelin, Leptin, IL6, TNFα Levels, and Food Intake of Women with Morbid Obesity. Diabetes, Metab. Syndr. Obes. Targets Ther. 2018, 11, 199–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karra, E.; O’Daly, O.G.; Choudhury, A.I.; Yousseif, A.; Millership, S.; Neary, M.T.; Scott, W.R.; Chandarana, K.; Manning, S.; Hess, M.E.; et al. A Link between FTO, Ghrelin, and Impaired Brain Food-Cue Responsivity. J. Clin. Investig. 2013, 123, 3539–3551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorling, J.L.; Clayton, D.J.; Jones, J.; Carter, W.G.; Thackray, A.E.; King, J.A.; Pucci, A.; Batterham, R.L.; Stensel, D.J. A Randomized Crossover Trial Assessing the Effects of Acute Exercise on Appetite, Circulating Ghrelin Concentrations, and Butyrylcholinesterase Activity in Normal-Weight Males with Variants of the Obesity-Linked FTO Rs9939609 Polymorphism. Am. J. Clin. Nutr. 2019, 110, 1055–1066. [Google Scholar] [CrossRef] [PubMed]
- PLAG1 Gene Symbol Report | HUGO Gene Nomenclature Committee. Available online: https://www.genenames.org/data/gene-symbol-report/#!/hgnc_id/HGNC:9045 (accessed on 14 May 2021).
- PLAG1—Zinc Finger Protein PLAG1—Homo Sapiens (Human)—PLAG1 Gene & Protein. Available online: https://www.uniprot.org/uniprot/Q6DJT9 (accessed on 23 April 2021).
- Bateman, A.; Martin, M.-J.; Orchard, S.; Magrane, M.; Agivetova, R.; Ahmad, S.; Alpi, E.; Bowler-Barnett, E.H.; Britto, R.; Bursteinas, B.; et al. UniProt: The Universal Protein Knowledgebase in 2021. Nucleic Acids Res. 2021, 49, D480–D489. [Google Scholar] [CrossRef]
- Warrington, N.M.; Beaumont, R.N.; Horikoshi, M.; Day, F.R.; Helgeland, Ø.; Laurin, C.; Bacelis, J.; Peng, S.; Hao, K.; Feenstra, B.; et al. Maternal and Fetal Genetic Effects on Birth Weight and Their Relevance to Cardio-Metabolic Risk Factors. Nat. Genet. 2019, 51, 804–814. [Google Scholar] [CrossRef]
- Hübel, C.; Gaspar, H.A.; Coleman, J.R.I.; Finucane, H.; Purves, K.L.; Hanscombe, K.B.; Prokopenko, I.; Graff, M.; Ngwa, J.S.; Workalemahu, T.; et al. Genomics of Body Fat Percentage May Contribute to Sex Bias in Anorexia Nervosa. Am. J. Med. Genet. Part. B Neuropsychiatr. Genet. 2019, 180, 428–438. [Google Scholar] [CrossRef] [Green Version]
- Shungin, D.; Winkler, T.; Croteau-Chonka, D.C.; Ferreira, T.; Locke, A.E.; Mägi, R.; Strawbridge, R.J.; Pers, T.H.; Fischer, K.; Justice, A.E.; et al. New Genetic Loci Link Adipose and Insulin Biology to Body Fat Distribution. Nature 2015, 518, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Czogała, W.; Czogała, M.; Strojny, W.; Wątor, G.; Wołkow, P.; Wójcik, M.; Multanowski, M.B.; Tomasik, P.; Wędrychowicz, A.; Kowalczyk, W.; et al. Methylation and Expression of FTO and PLAG1 Genes in Childhood Obesity: Insight into Anthropometric Parameters and Glucose-Lipid Metabolism. Nutrients 2021, 13, 1683. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Kokubun, S.; Itoi, E.; Roach, H.I. Improved Quantification of DNA Methylation Using Methylation-Sensitive Restriction Enzymes and Real-Time PCR. Epigenetics 2007, 2, 86–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redshaw, N.; Huggett, J.F.; Taylor, M.S.; Foy, C.A.; Devonshire, A.S. Quantification of Epigenetic Biomarkers: An Evaluation of Established and Emerging Methods for DNA Methylation Analysis. BMC Genom. 2014, 15, 1174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howe, K.L.; Achuthan, P.; Allen, J.; Allen, J.; Alvarez-Jarreta, J.; Ridwan Amode, M.; Armean, I.M.; Azov, A.G.; Bennett, R.; Bhai, J.; et al. Ensembl 2021. Nucleic Acids Res. 2021, 49, D884–D891. [Google Scholar] [CrossRef] [PubMed]
- Untergasser, A.; Cutcutache, I.; Koressaar, T.; Ye, J.; Faircloth, B.C.; Remm, M.; Rozen, S.G. Primer3—New Capabilities and Interfaces. Nucleic Acids Res. 2012, 40, e115. [Google Scholar] [CrossRef] [Green Version]
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 13 May 2021).
- Smyth, G.K. Linear Models and Empirical Bayes Methods for Assessing Differential Expression in Microarray Experiments. Stat. Appl. Genet. Mol. Biol. 2004, 3, 3. [Google Scholar] [CrossRef]
- Gentleman, R.C.; Carey, V.J.; Bates, D.M.; Bolstad, B.; Dettling, M.; Dudoit, S.; Ellis, B.; Gautier, L.; Ge, Y.; Gentry, J.; et al. Bioconductor: Open Software Development for Computational Biology and Bioinformatics. Genome Biol. 2004, 5, R80. [Google Scholar] [CrossRef] [Green Version]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- WHO Anthro Survey Analyser and Other Tools. Available online: https://www.who.int/toolkits/child-growth-standards/software (accessed on 4 March 2021).
- FTO Gene—GeneCards | FTO Protein | FTO. Antibody. Available online: https://www.genecards.org/cgi-bin/carddisp.pl?gene=FTO&keywords=FTO (accessed on 16 April 2021).
- Stelzer, G.; Rosen, N.; Plaschkes, I.; Zimmerman, S.; Twik, M.; Fishilevich, S.; Stein, T.I.; Nudel, R.; Lieder, I.; Mazor, Y.; et al. The GeneCards Suite: From Gene Data Mining to Disease Genome Sequence Analyses. Curr. Protoc. Bioinform. 2016, 54, 1.30.1–1.30.33. [Google Scholar] [CrossRef]
- O’Leary, N.A.; Wright, M.W.; Brister, J.R.; Ciufo, S.; Haddad, D.; McVeigh, R.; Rajput, B.; Robbertse, B.; Smith-White, B.; Ako-Adjei, D.; et al. Reference Sequence (RefSeq) Database at NCBI: Current Status, Taxonomic Expansion, and Functional Annotation. Nucleic Acids Res. 2016, 44, D733–D745. [Google Scholar] [CrossRef] [Green Version]
- Jia, G.; Yang, C.G.; Yang, S.; Jian, X.; Yi, C.; Zhou, Z.; He, C. Oxidative Demethylation of 3-Methylthymine and 3-Methyluracil in Single-Stranded DNA and RNA by Mouse and Human FTO. FEBS Lett. 2008, 582, 3313–3319. [Google Scholar] [CrossRef] [Green Version]
- Han, Z.; Niu, T.; Chang, J.; Lei, X.; Zhao, M.; Wang, Q.; Cheng, W.; Wang, J.; Feng, Y.; Chai, J. Crystal Structure of the FTO Protein Reveals Basis for Its Substrate Specificity. Nature 2010, 464, 1205–1209. [Google Scholar] [CrossRef]
- Speakman, J.R. The ‘Fat Mass and Obesity Related’ (FTO) Gene: Mechanisms of Impact on Obesity and Energy Balance. Curr. Obes. Rep. 2015, 4, 73–91. [Google Scholar] [CrossRef]
- Di Renzo, L.; Cioccoloni, G.; Falco, S.; Abenavoli, L.; Moia, A.; Sinibaldi Salimei, P.; De Lorenzo, A. Influence of FTO Rs9939609 and Mediterranean Diet on Body Composition and Weight Loss: A Randomized Clinical Trial NCT01890070 NCT. J. Transl. Med. 2018, 16, 308. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Park, J.H.; Park, S.E.; Shon, J.; Park, Y.J. The Fat Mass- and Obesity-Associated (FTO) Gene to Obesity: Lessons from Mouse Models. Obesity 2018, 26, 1674–1686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labayen, I.; Ruiz, J.R.; Ortega, F.B.; Dalongeville, J.; Jiménez-Pavón, D.; Castillo, M.J.; De Henauw, S.; González-Gross, M.; Bueno, G.; Molnar, D.; et al. Association between the FTO Rs9939609 Polymorphism and Leptin in European Adolescents: A Possible Link with Energy Balance Control. The HELENA Study. Int. J. Obes. 2011, 35, 66–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Z.; Luo, X.; Liu, M.; Chen, L. Function and Regulation of Apelin/APJ System in Digestive Physiology and Pathology. J. Cell Physiol. 2019, 234, 7796–7810. [Google Scholar] [CrossRef] [PubMed]
- Kadoglou, N.P.E.; Vrabas, I.S.; Kapelouzou, A.; Lampropoulos, S.; Sailer, N.; Kostakis, A.; Liapis, C.D.; Angelopoulou, N. The Impact of Aerobic Exercise Training on Novel Adipokines, Apelin and Ghrelin, in Patients with Type 2 Diabetes. Med. Sci. Monit. 2012, 18, CR290-5. [Google Scholar] [CrossRef] [Green Version]
- Son, J.S.; Chae, S.A.; Park, B.I.; Du, M.; Song, W. Plasma Apelin Levels in Overweight/Obese Adults Following a Single Bout of Exhaustive Exercise: A Preliminary Cross-Sectional Study. Endocrinol. Diabetes Nutr. 2019, 66, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Kadoglou, N.P.E.; Vrabas, I.S.; Kapelouzou, A.; Angelopoulou, N. The Association of Physical Activity with Novel Adipokines in Patients with Type 2 Diabetes. Eur. J. Intern. Med. 2012, 23, 137–142. [Google Scholar] [CrossRef]
- Chandra, R.; Liddle, R.A. Cholecystokinin. Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Crovesy, L.; Rosado, E.L. Interaction between Genes Involved in Energy Intake Regulation and Diet in Obesity. Nutrition 2019, 67–68, 110547. [Google Scholar] [CrossRef] [PubMed]
- Holst, J.J. The Physiology of Glucagon-like Peptide 1. Physiol. Rev. 2007, 87, 1409–1439. [Google Scholar] [CrossRef]
- Danaher, J.; Stathis, C.G.; Cooke, M.B. Similarities in Metabolic Flexibility and Hunger Hormone Ghrelin Exist between FTO Gene Variants in Response to an Acute Dietary Challenge. Nutrients 2019, 11, 2518. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, T.; Ngwa, J.S.; Van Rooij, F.J.A.; Zillikens, M.C.; Wojczynski, M.K.; Frazier-Wood, A.C.; Houston, D.K.; Kanoni, S.; Lemaitre, R.N.; Luan, J.N.A.; et al. Genome-Wide Meta-Analysis of Observational Studies Shows Common Genetic Variants Associated with Macronutrient Intake. Am. J. Clin. Nutr. 2013, 97, 1395–1402. [Google Scholar] [CrossRef] [Green Version]
- PLAG1 Gene—GeneCards | PLAG1 Protein | PLAG1 Antibody. Available online: https://www.genecards.org/cgi-bin/carddisp.pl?gene=PLAG1&keywords=PLAG1 (accessed on 16 April 2021).
- Van Dyck, F.; Declercq, J.; Braem, C.; Van de Ven, W. PLAG1, the Prototype of the PLAG Gene Family: Versatility in Tumour Development (Review). Int. J. Oncol. 2007, 30, 765–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zatkova, A.; Rouillard, J.M.; Hartmann, W.; Lamb, B.J.; Kuick, R.; Eckart, M.; Von Schweinitz, D.; Koch, A.; Fonatsch, C.; Pietsch, T.; et al. Amplification and Overexpression of the IGF2 Regulator PLAG1 in Hepatoblastoma. Genes Chromosom. Cancer 2004, 39, 126–137. [Google Scholar] [CrossRef]
- GWAS Catalog. Available online: https://www.ebi.ac.uk/gwas/home (accessed on 6 March 2021).
- Buniello, A.; Macarthur, J.A.L.; Cerezo, M.; Harris, L.W.; Hayhurst, J.; Malangone, C.; McMahon, A.; Morales, J.; Mountjoy, E.; Sollis, E.; et al. The NHGRI-EBI GWAS Catalog of Published Genome-Wide Association Studies, Targeted Arrays and Summary Statistics 2019. Nucleic Acids Res. 2019, 47, D1005–D1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Street, M.E.; Smerieri, A.; Montanini, L.; Predieri, B.; Iughetti, L.; Valenzise, M.; De Luca, F.; Vigone, M.; Weber, G.; Maghnie, M.; et al. Interactions among Pro-Inflammatory Cytokines, IGF System and Thyroid Function in Pre-Pubertal Obese Subjects. J. Biol. Regul. Homeost. Agents 2013, 27, 259–266. [Google Scholar]
- Seck, T.; Englaro, P.; Blum, W.F.; Scheidt-Nave, C.; Rascher, W.; Ziegler, R.; Pfeilschifter, J. Leptin Concentrations in Serum from a Randomly Recruited Sample of 50- to 80-Year-Old Men and Women: Positive Association with Plasma Insulin-like Growth Factors (IGFs) and IGF-Binding Protein-3 in Lean, but Not in Obese, Individuals. Eur. J. Endocrinol. 1998, 138, 70–75. [Google Scholar] [CrossRef] [Green Version]
- Kleiman, A.; Keats, E.C.; Chan, N.G.; Khan, Z.A. Elevated IGF2 Prevents Leptin Induction and Terminal Adipocyte Differentiation in Hemangioma Stem Cells. Exp. Mol. Pathol. 2013, 94, 126–136. [Google Scholar] [CrossRef]
- Uchida, A.; Zechner, J.F.; Mani, B.K.; Park, W.M.; Aguirre, V.; Zigman, J.M. Altered Ghrelin Secretion in Mice in Response to Diet-Induced Obesity and Roux-En-Y Gastric Bypass. Mol. Metab. 2014, 3, 717–730. [Google Scholar] [CrossRef]
- de Mello, V.D.F.; Kolehmanien, M.; Schwab, U.; Pulkkinen, L.; Uusitupa, M. Gene Expression of Peripheral Blood Mononuclear Cells as a Tool in Dietary Intervention Studies: What Do We Know so Far? Mol. Nutr. Food Res. 2012, 56, 1160–1172. [Google Scholar] [CrossRef] [PubMed]
- Reynés, B.; Priego, T.; Cifre, M.; Oliver, P.; Palou, A. Peripheral Blood Cells, a Transcriptomic Tool in Nutrigenomic and Obesity Studies: Current State of the Art. Compr. Rev. Food Sci. Food Saf. 2018, 17, 1006–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohane, I.S.; Valtchinov, V.I. Quantifying the white blood cell transcriptome as an accessible window to the multiorgan transcriptome. Bioinformatics 2012, 28, 538–545. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).