Vegans, Vegetarians, and Omnivores: How Does Dietary Choice Influence Iodine Intake? A Systematic Review
Abstract
1. Introduction
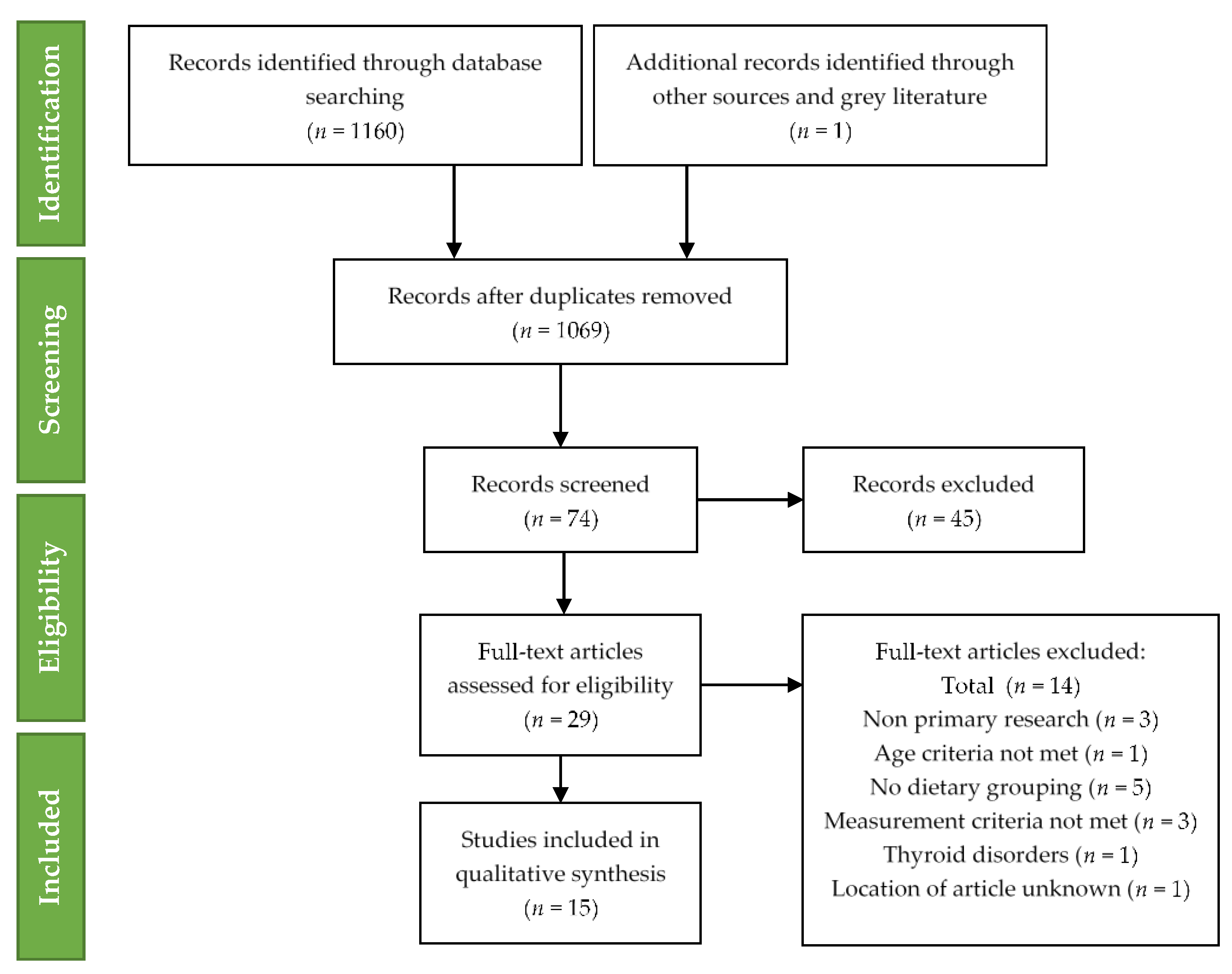
2. Materials and Methods
3. Results
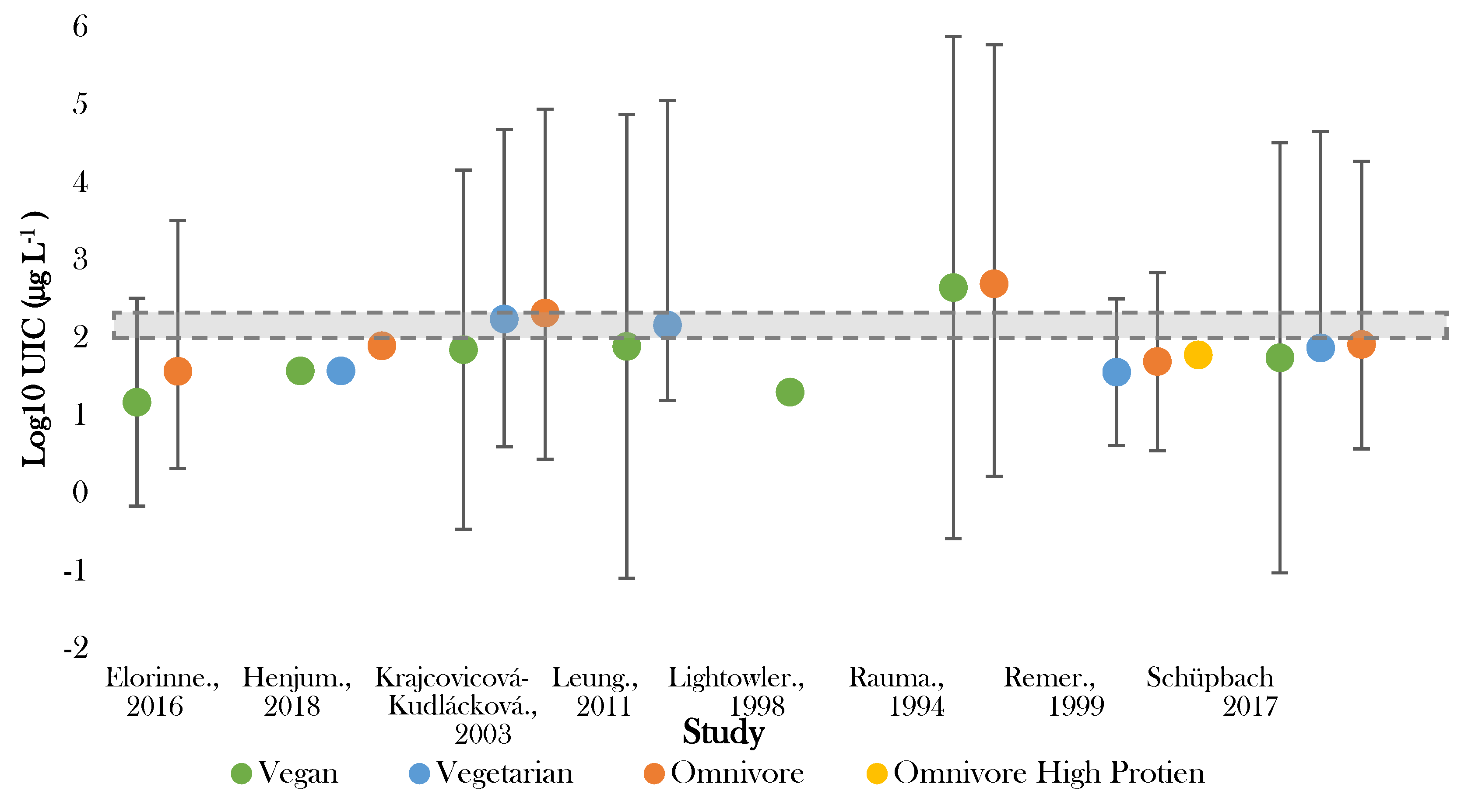
3.1. Urinary Iodine Status
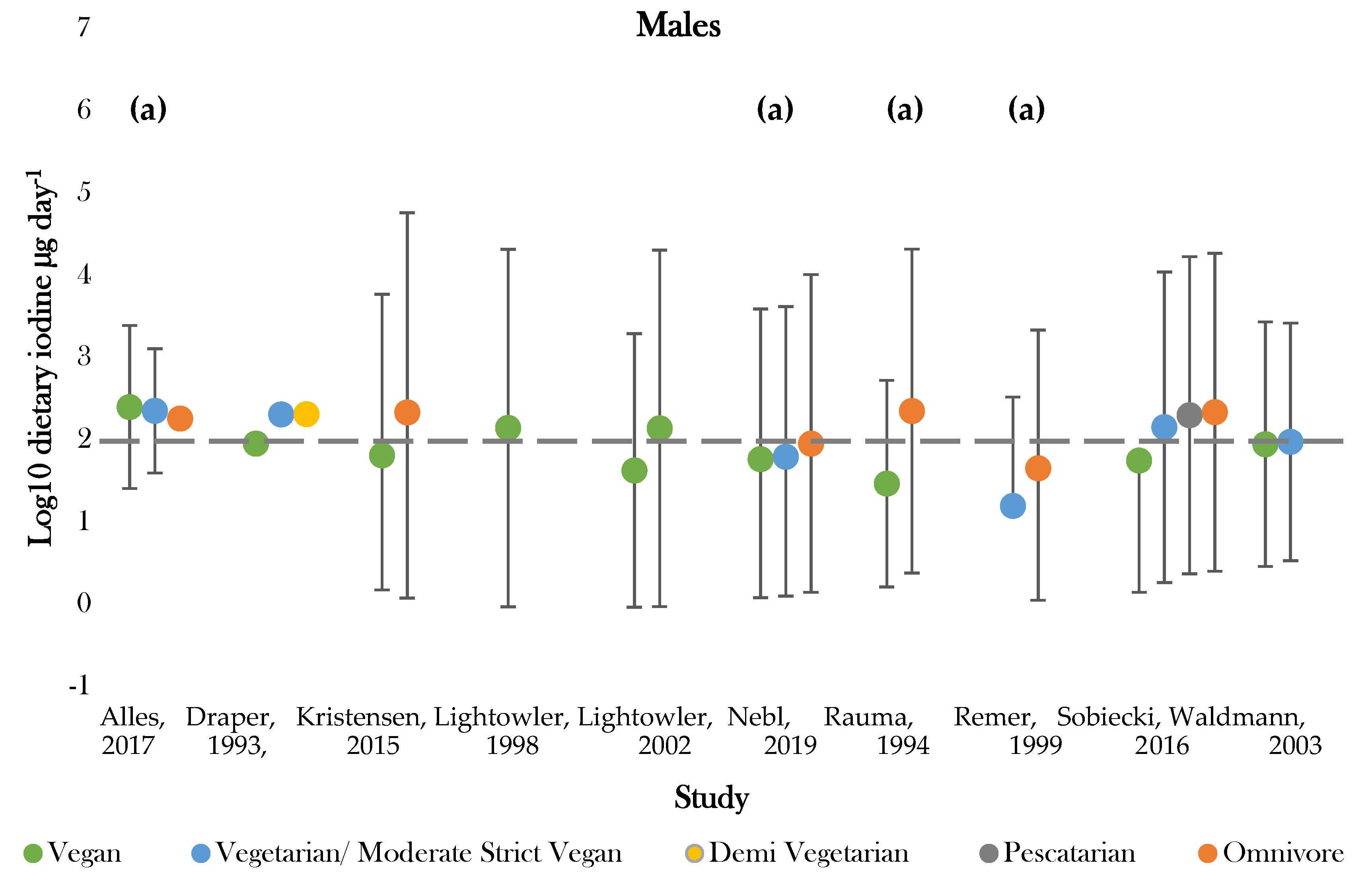
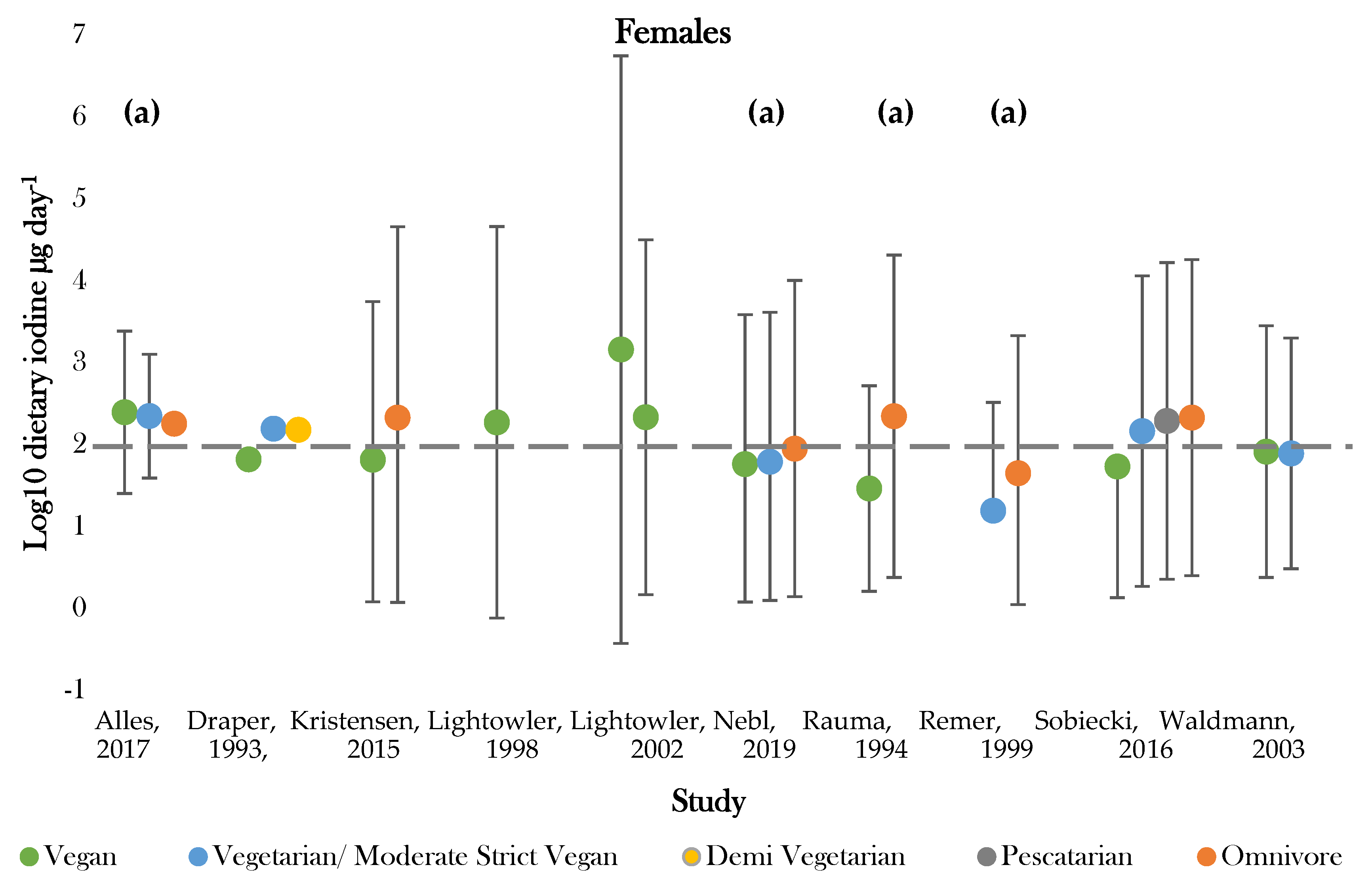
3.2. Dietary Iodine Intake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Phillips, F. Vegetarian nutrition. Nutr. Bull. 2005, 30, 132–167. [Google Scholar] [CrossRef]
- Sebastiani, G.; Herranz Barbero, A. The effects of vegetarian and vegan diet during pregnancy on the health of mothers and offspring. Nutrients 2019, 11, 557. [Google Scholar] [CrossRef] [PubMed]
- British Dietetic Association Confirms Well-Planned Vegan Diets Can Support Healthy Living in People of All Ages. Available online: https://www.bda.uk.com/resource/british-dietetic-association-confirms-well-planned-vegan-diets-can-support-healthy-living-in-people-of-all-ages.html (accessed on 24 February 2020).
- Vegan Diets: Everything You Need to Know—Dietitians Association of Australia. Available online: https://daa.asn.au/smart-eating-for-you/smart-eating-fast-facts/healthy-eating/vegan-diets-facts-tips-and-considerations/ (accessed on 7 October 2019).
- Craig, W.J.; Mangels, A.R. American Dietetic Association Position of the American Dietetic Association: Vegetarian diets. J. Am. Diet Assoc. 2009, 109, 1266–1282. [Google Scholar] [PubMed]
- Scientific Advisory Committe on Nutrition Statement on Iodine and Health. 2014. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/339439/SACN_Iodine_and_Health_2014.pdf (accessed on 7 October 2019).
- Eastman, C.J.; Zimmermann, M.B. The Iodine Deficiency Disorders, 1st ed.; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A., Hershman, J.M., Kaltsas, G., Koch, C., Kopp, P., et al., Eds.; Endotext [Internet]: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Ahad, F.; Ganie, S.A. Iodine, Iodine metabolism and Iodine deficiency disorders revisited. Indian J. Endocrinol. Metab. 2010, 14, 13–17. [Google Scholar] [PubMed]
- Zimmermann, M.B. Iodine deficiency. Endocr. Rev. 2009, 30, 376–408. [Google Scholar] [CrossRef]
- Zimmermann, M.B. Thyroid gland: Iodine deficiency and thyroid nodules. Nat. Rev. Endocrinol. 2014, 10, 707–708. [Google Scholar] [CrossRef]
- Popoveniuc, G.; Jonklaas, J. Thyroid Nodules. Med. Clin. N. Am. 2012, 96, 329–349. [Google Scholar] [CrossRef]
- Leung, A.M.; Braverman, L.E. Consequences of excess iodine. Nat. Rev. Endocrinol. 2014, 10, 136–142. [Google Scholar] [CrossRef]
- Li, M.; Eastman, C.J. The changing epidemiology of iodine deficiency. Nat. Rev. Endocrinol. 2012, 8, 434–440. [Google Scholar] [CrossRef]
- Iodine Global Network (IGN)—Home. Available online: http://www.ign.org/ (accessed on 13 September 2019).
- World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring their Elimination A Guide for Programme Managers, 3rd ed.; World Health Organization: Geneva, Switzerland, 2007; pp. 1–60. [Google Scholar]
- Pearce, E.N.; Caldwell, K.L. Urinary iodine, thyroid function, and thyroglobulin as biomarkers of iodine status. Am. J. Clin Nutr. 2016, 104, 898–901. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Pfrimer, K.; Doreste-Alonso, J.; Ribas-Barba, L.; Sánchez-Villegas, A.; Ortiz-Andrellucchi, A.; Henríquez-Sánchez, P. Dietary assessment methods for intakes of iron, calcium, selenium, zinc and iodine. Br. J. Nutr. 2009, 102. [Google Scholar] [CrossRef] [PubMed]
- Gunnarsdottir, I.; Dahl, L. Iodine intake in human nutrition: A systematic literature review. Food Nutr. Res. 2012, 56, 19731. [Google Scholar] [CrossRef] [PubMed]
- Fuge, R. Soils and iodine deficiency. In Essentials of Medical Geology; Selinus, O., Ed.; Springer: Dordrecht, The Netherlands, 2013; pp. 417–432. [Google Scholar]
- Humphrey, O.S.; Young, S.D. Iodine uptake, storage and translocation mechanisms in spinach (Spinacia oleracea L.). Environ. Geochem. Health 2019, 41, 2145–2156. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. Iodine deficiency in industrialized countries. Clin. Endocrinol. 2011, 75, 287–288. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.; Rayman, M. British Dietetic Association: Iodine Food Fact Sheet. 2016. Available online: https://www.bda.uk.com/resource/iodine.html (accessed on 20 May 2020).
- Andersson, M.; de Benoist, B.; Delange, F. Iodine Deficiency in Europe: A Continuing Public Health Problem, 1st ed.; World Health Organization: Geneva, Switzerland, 2007; pp. 154–196. [Google Scholar]
- Gärtner, R. Recent data on iodine intake in Germany and Europe. J. Trace Elem. Med. Biol. 2016, 37, 85–89. [Google Scholar] [CrossRef]
- Bath, S.C.; Button, S.; Rayman, M.P. Availability of iodised table salt in the UK—Is it likely to influence population iodine intake? Public Health Nutr. 2014, 17, 450–454. [Google Scholar] [CrossRef]
- Appleby, P.N.; Thorogood, M. The Oxford Vegetarian Study: An overview. Am. J. Clin. Nutr. 1999, 70, 525–531. [Google Scholar] [CrossRef]
- Elsabie, W.; Aboel Einen, K. Comparative Evaluation of Some Physicochemical Properties for Different Types of Vegan Milk with Cow Milk. Dairy Sci. Technol. 2016, 7, 457–461. [Google Scholar] [CrossRef]
- Bath, S.C.; Hill, S.; Infante, H.G. Iodine concentration of milk-alternative drinks available in the UK in comparison with cows’ milk. Br. J. Nutr. 2017, 118, 525–532. [Google Scholar] [CrossRef]
- 52% of UK Meat-Free New Product Launches Are Vegan-Mintel. Available online: https://www.mintel.com/press-centre/food-and-drink/more-than-half-of-all-meat-free-new-product-launches-in-the-uk-carry-a-vegan-claim-1 (accessed on 24 February 2020).
- Fields, C.; Borak, J. Iodine Deficiency in Vegetarian and Vegan Diets: Evidence-Based Review of the World’s Literature on Iodine Content in Vegetarian Diets. In Comprehensive Handbook of Iodine, 1st ed.; Elsevier Science Publishing Co.: Amsterdam, The Netherlands, 2009; pp. 521–531. [Google Scholar]
- Fields, C.; Dourson, M.; Borak, J. Iodine-deficient vegetarians: A hypothetical perchlorate-susceptible population? RTP 2005, 42, 37–46. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement—Flow of information through the different phases of a systematic review. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Howard, C. Subject & Course Guides: Evidence Based Medicine: PICO. Available online: https://researchguides.uic.edu/c.php?g=252338&p=3954402 (accessed on 13 September 2019).
- Data extraction forms|Cochrane Developmental, Psychosocial and Learning Problems. Available online: https://dplp.cochrane.org/data-extraction-forms (accessed on 13 September 2019).
- Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI). Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 13 September 2019).
- Allès, B.; Baudry, J. Comparison of Sociodemographic and Nutritional Characteristics between Self-Reported Vegetarians, Vegans, and Meat-Eaters from the NutriNet-Santé Study. Nutrients 2017, 9, 1023. [Google Scholar] [CrossRef] [PubMed]
- Draper, A.; Lewis, J. The energy and nutrient intakes of different types of vegetarian: A case for supplements? Br. J. Nutr. 1993, 69, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Henjum, S.; Brantsæter, A.L.; Kurniasari, A.; Dahl, L.; Aadland, E.K.; Gjengedal, E.L.F.; Birkeland, S.; Aakre, I. Suboptimal iodine status and low iodine knowledge in young Norwegian women. Nutrients 2018, 10, 941. [Google Scholar] [CrossRef]
- Krajcovicová-Kudlácková, M.; Bucková, K.; Klimes, I.; Seboková, E. Iodine deficiency in vegetarians and vegans. Ann. Nutr. Metab. 2003, 47, 183–185. [Google Scholar] [CrossRef]
- Leung, A.M.; LaMar, A.; He, X.; Braverman, L.E.; Pearce, E.N. Iodine status and thyroid function of Boston-area vegetarians and vegans. J. Clin. Endocrinol. 2011, 96, 1303–1307. [Google Scholar] [CrossRef]
- Lightowler, H.J.; Davies, G.J. Iodine intake and iodine deficiency in vegans as assessed by the duplicate-portion technique and urinary iodine excretion. Br. J. Nutr. 1998, 80, 529–535. [Google Scholar] [CrossRef]
- Lightowler, H.J.; Davies, G.J. Assessment of iodine intake in vegans: Weighed dietary record vs duplicate portion technique. Eur. J. Clin. Nutr. 2002, 56, 765–770. [Google Scholar] [CrossRef]
- Nebl, J.; Schuchardt, J.P.; Wasserfurth, P.; Haufe, S.; Eigendorf, J.; Tegtbur, U.; Hahn, A. Characterization, dietary habits and nutritional intake of omnivorous, lacto-ovo vegetarian and vegan runners—A pilot study. BMC Nutr. 2019, 5, 51. [Google Scholar] [CrossRef]
- Schüpbach, R.; Wegmüller, R.; Berguerand, C.; Bui, M.; Herter-Aeberli, I. Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur. J. Clin. Nutr. 2017, 56, 283–293. [Google Scholar] [CrossRef]
- Sobiecki, J.G.; Appleby, P.N.; Bradbury, K.E.; Key, T.J. High Compliance with Dietary Recommendations in a Cohort of Meat Eaters, Fish Eaters, Vegetarians, and Vegans. Nutr. Res. 2016, 36, 464–477. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, A.; Koschizke, J.W.; Leitzmann, C.; Hahn, A. Dietary intakes and lifestyle factors of a vegan population in Germany: Results from the German Vegan Study. Eur. J. Clin. Nutr. 2003, 57, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Remer, T.; Neubert, A.; Manz, F. Increased risk of iodine deficiency with vegetarian nutrition. Br. J. Nutr. 1999, 81, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Elorinne, A.-L.; Alfthan, G.; Erlund, I.; Kivimäki, H.; Paju, A.; Salminen, I.; Turpeinen, U.; Voutilainen, S.; Laakso, J. Food and Nutrient Intake and Nutritional Status of Finnish Vegans and Non-Vegetarians. PLoS ONE 2016, 11, e0148235. [Google Scholar] [CrossRef]
- Kristensen, N.B.; Madsen, M.L.; Hansen, T.H.; Allin, K.H.; Hoppe, C.; Fagt, S.; Lausten, M.S.; Gøbel, R.J.; Vestergaard, H.; Hansen, T.; et al. Intake of macro- and micronutrients in Danish vegans. Nutr. J. 2015, 14, 115. [Google Scholar] [CrossRef] [PubMed]
- Rauma, A.L.; Törmälä, M.L.; Nenonen, M.; Hänninen, O. Iodine status in vegans consuming a living food diet. Nutr. Res. 1994, 14, 1789–1795. [Google Scholar] [CrossRef]
- VMNIS|Vitamin and Mineral Nutrition Information System Urinary Iodine Concentrations for Determining Iodine Status in Populations. Available online: https://www.who.int/vmnis/indicators/urinaryiodine/en/ (accessed on 12 September 2019).
- Martin, A. The “apports nutritionnels conseillés (ANC)” for the French population. Reprod. Nutr. Dev. 2001, 41, 119–128. [Google Scholar] [CrossRef]
- The Department of Health Dietary Reference Values A Guide. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/743790/Dietary_Reference_Values_-_A_Guide__1991_.pdf (accessed on 12 September 2019).
- Nordic Council of Ministers Nordic Nutrition Recommendations 2012 Integrating Nutrition and Physical Activity. Available online: https://norden.diva-portal.org/smash/get/diva2:704251/FULLTEXT01.pdf (accessed on 12 September 2019).
- Jod. Available online: https://www.dge.de/wissenschaft/referenzwerte/jod/ (accessed on 24 April 2020).
- National Research Council. Food and Nutrition Board Recommended Dietary Allowances; National Academies Press: Washington, DC, USA, 1989; pp. 1–277. [Google Scholar]
- German Nutrition Society. The Nutrition Report 2000, 2000th ed.; German Nutrition Society: Bonn, Germany, 2000; pp. 1–37. [Google Scholar]
- Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; National Academies Press: Washington, DC, USA, 2001; pp. 1–500. [Google Scholar]
- Iodine Global Network (IGN)—Global Iodine Scorecard and Map. Available online: https://www.ign.org/scorecard.htm (accessed on 20 March 2020).
- Black, M.M. Micronutrient Deficiencies and Cognitive Functioning. Nutr. J. 2003, 133, 3927s–3931s. [Google Scholar] [CrossRef]
- Zimmermann, M.B. Iodine deficiency and excess in children: Worldwide status in 2013. Endocr. Pract. 2013, 19, 839–846. [Google Scholar] [CrossRef]
- Martinelli, D.; Berkmanienė, A. The Politics and the Demographics of Veganism: Notes for a Critical Analysis. Int. J. Semiot. Law 2018, 31, 501–530. [Google Scholar] [CrossRef]
- Andersson, M.; Aeberli, I.; Wüst, N.; Piacenza, A.M.; Bucher, T.; Henschen, I.; Haldimann, M.; Zimmermann, M.B. The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J. Clin. Endocrinol. Metab. 2010, 95, 5217–5224. [Google Scholar] [CrossRef] [PubMed]
- Nyström, H.F.; Brantsæter, A.L.; Erlund, I.; Gunnarsdottir, I.; Hulthén, L.; Laurberg, P.; Mattisson, I.; Rasmussen, L.B.; Virtanen, S.; Meltzer, H.M. Iodine status in the Nordic countries past and present. Nutr. Res. 2016, 60, 31969. [Google Scholar] [CrossRef] [PubMed]
- International Vegetarian Union—History of IVU. Available online: https://ivu.org/history/ (accessed on 26 September 2019).
- Leitzmann, C. Vegetarian nutrition: Past, present, future. Am. J. Clin. Nutr. 2014, 100, 496s–502s. [Google Scholar] [CrossRef]
- Juan, W.; Yamini, S.; Britten, P. Food Intake Patterns of Self-identified Vegetarians Among the U.S. Population, 2007–2010. Procedia Food Sci. 2015, 4, 86–93. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in populations: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef]
- Bingham, S.A.; Cassidy, A.; Cole, T.J.; Welch, A.; Runswick, S.A.; Black, A.E.; Thurnham, D.; Bates, C.; Khaw, K.T.; Key, T.J.A.; et al. Validation of weighed records and other methods of dietary assessment using the 24 h urine nitrogen technique and other biological markers. Br. J. Nutr. 1995, 73, 531–550. [Google Scholar] [CrossRef]
- DAPA Measurement Toolkit. Available online: https://dapa-toolkit.mrc.ac.uk/diet/objective-methods/duplicate-diets (accessed on 26 September 2019).
- Rasmussen, L.B.; Ovesen, L.; Bülow, I.; Jørgensen, T.; Knudsen, N.; Laurberg, P.; Perrild, H. Evaluation of a semi-quantitative food frequency questionnaire to estimate iodine intake. Eur. J. Clin. Nutr. 2001, 55, 287–292. [Google Scholar] [CrossRef]
- O’Kane, S.M.; Pourshahidi, L.K.; Mulhern, M.S.; Weir, R.R.; Hill, S.; O’Reilly, J.; Kmiotek, D.; Deitrich, C.; Mackle, E.M.; Fitzgerald, E.; et al. The effect of processing and seasonality on the iodine and selenium concentration of cow’s milk produced in Northern Ireland (NI): Implications for population dietary intake. Nutrients 2018, 10, 287. [Google Scholar] [CrossRef]
- Yeh, T.S.; Hung, N.H.; Lin, T.C. Analysis of iodine content in seaweed by GC-ECD and estimation of iodine intake. J. Food Drug Anal. 2014, 22, 189–196. [Google Scholar] [CrossRef]
- Bouga, M.; Combet, E. Emergence of Seaweed and Seaweed-Containing Foods in the UK: Focus on Labeling, Iodine Content, Toxicity and Nutrition. Foods 2015, 4, 240–253. [Google Scholar] [CrossRef]
- Lightowler, H.J. Assessment of Iodine Intake and Iodine Status in Vegans. In Comprehensive Handbook of Iodine; Elsevier Inc.: Amsterdam, The Netherlands, 2009; pp. 429–436. [Google Scholar]
- Dasgupta, P.K.; Liu, Y.; Dyke, J.V. Iodine nutrition: Iodine content of iodized salt in the United States. Environ. Sci. Technol. 2008, 42, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Rana, R.; Raghuvanshi, R.S. Effect of different cooking methods on iodine losses. J. Food Sci. Technol. 2013, 50, 1212–1216. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rayman, M.P.; Bath, S.C. The new emergence of iodine deficiency in the UK: Consequences for child neurodevelopment. Ann. Clin. Biochem. 2015, 52, 705–708. [Google Scholar] [CrossRef] [PubMed]
| Criteria Category | Inclusion | Exclusion |
|---|---|---|
| Population | Adults (aged ≥ 18 y) residing in industrialised nations. | Individuals (aged < 18 y), unless results display separate data; adults residing in developing countries; populations with a high prevalence of thyroid disorders. |
| Intervention/exposure | Participants with any type of dietary preference or restriction. Voluntary or otherwise. | Use of a dietary grouping without defining diet characteristics. |
| Comparators | Differing dietary preference or restriction. | None. |
| Outcome measure | Iodine intake or status measured by UIC or analysis of dietary records. | No analysis of iodine intake or status; use of thyroid measures alone for iodine intake and status. |
| Study design | Any study design with relevant outcomes. | None. |
| Question | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study, Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Rating |
| Observational Cohort Cross-Sectional Studies | |||||||||||||||
| Alles, 2017 [36] |  + + |  + + |  + + |  + + |  − − |  − − |  − − |  − − |  + + |  + + |  + + |  − − |  a a |  + + | Fair |
| Draper, 1993 [37] |  + + |  − − |  r r |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  − − | Fair |
| Henjum, 2018 [38] |  + + |  + + |  r r |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Krajcovicová-Kudlácková, 2003 [39] |  + + |  − − |  r r |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  − − | Fair |
| Leung, 2011 [40] |  + + |  − − |  r r |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Lightowler, 1998 [41] |  + + |  + + |  + + |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Fair |
| Lightowler, 2002 [42] |  + + |  + + |  + + |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Nebl, 2019 [43] |  + + |  + + |  + + |  + + |  − − |  − − |  − − |  − − |  + + |  + + |  + + |  r r |  a a |  − − | Good |
| Schűpbach, 2017 [44] |  + + |  − − |  + + |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Sobiecki, 2016 [45] |  + + |  + + |  + + |  + + |  + + |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Waldmann, 2003 [46] |  + + |  − − |  + + |  + + |  − − |  − − |  − − |  + + |  + + |  + + |  + + |  − − |  a a |  + + | Good |
| Controlled Intervention Studies | |||||||||||||||
| Remer, 1999 [47] |  − − |  ? ? |  − − |  - - |  − − |  + + |  + + |  + + |  + + |  + + |  + + |  + + |  + + |  + + | Good |
| Case-Control Studies | |||||||||||||||
| Elorinne, 2016 [48] |  + + |  − − |  + + |  + + |  r r |  + + |  ? ? |  ? ? |  − − |  + + |  − − |  + + |  a a |  a a | Fair |
| Kristensen, 2015 [49] |  + + |  + + |  − − |  − − |  + + |  + + |  ? ? |  ? ? |  − − |  + + |  − − |  + + |  a a |  a a | Fair |
| Rauma, 1994 [50] |  + + |  − − |  − − |  + + |  − − |  + + |  ? ? |  ? ? |  − − |  + + |  − − |  − − |  a a |  a a | Poor |
 +, yes;
+, yes;  −, no;
−, no;  ?, cannot determine;
?, cannot determine;  a, not applicable;
a, not applicable;  r, not reported;
r, not reported;  (outlined), fixed answers according to NHLBI recommendations.
(outlined), fixed answers according to NHLBI recommendations.| Study, Year | Assessment Method | Dietary Group (n) (Male, Female) | Iodine Status by UIC (µg day−1) | Criteria for Iodine Deficiency Disorders |
|---|---|---|---|---|
| Elorinne, 2016 [48] | Spot UIC Sandell–Kolthoff method. | Vegan (21) | 15.0 (4.6, 21.8) 1,** | Severe |
| Omnivore (18) | 37.4 (17.7, 86.5) 1 | Moderate | ||
| Henjum, 2018 [38] | Spot UIC. | Vegan (9) | 38.0 1,** | Moderate |
| Vegetarian (27) | ||||
| Omnivore (367) | 80.0 1 | Mild | ||
| Krajcovicová-Kudlácková, 2003 [39] | 24 h UIC Sandell–Kolthoff method. | Vegan (15) (6,9) | 71.0 (9.0–204.0) 2,** | Mild |
| Vegetarian (31) (12,19) | 177.0 (44.0–273.0) 2,** | Optimal | ||
| Omnivore (Mixed Diet) (35) (15,20) | 210.0 (76.0–423.0) 2 | Optimal with risk of health consequences | ||
| Leung, 2011 [40] | Spot UIC spectrophotometry. | Vegan (62) (19,43) | 78.5 (6.8–964.7) 2,* | Mild |
| Vegetarian (78) (26,52) | 147.0 (9.3–778.6) 2 | Optimal | ||
| Lightowler, 1998 [41] | Four 24 h UIC Sandell–Kolthoff method reaction. | Vegan (30) (11,19) | Total, 20.2 1, M, 16.8 1, F, 20.5 1 | Severe-Moderate |
| Rauma, 1994 [50] | 24 h UIC. | Vegan (Living Food Diet) (10) | <450.0 (<200.0–1700.0) 2 | Optimal with risk of health consequences |
| Omnivore (12) | <500.0 (300.0−1200.0) 2 | |||
| Remer, 1999 [47] | Two 24 h UIC. | Vegetarian (6) (3,3) | 36.6 ± 8.8 3,* | Moderate |
| Omnivore (6) (3,3) | 50.2 ± 14.0 3 | Mild | ||
| Omnivore (High Protein) (6) (3,3) | 61.0 ± 8 3 | Mild | ||
| Schüpbach, 2017 [44] | Four fasted spot UIC. | Vegan (53) (20,33) | 56.0 (27.0–586.0) 2,* | Mild |
| Vegetarian (53) (17,36) | 75.0 (1.0–610.0) 2 | Mild | ||
| Omnivore (100) (37,63) | 83.0 (22.0–228.0) 2 | Mild |
| Study, Year | Study Design | Location | Dietary Groups | Sample (n) (Male, Female) | Method of Dietary Classification | Average Diet Adherence (Years) |
|---|---|---|---|---|---|---|
| Alles, 2017 [36] | Cross-Sectional | France | Vegan | 789 | Assessed by investigators pre-study | NA |
| Vegetarian | 2370 | |||||
| Omnivore | 90,664 | |||||
| Draper, 1993 [37] | Cross-sectional | London, UK | Vegan | 38 (18,20) | Self-reported | 1.0 |
| Lacto-Vegetarian | 52 (16,36) | 2.0 | ||||
| Demi-vegetarian | 37 (13,24) | 5.0–9.0 | ||||
| Elorinne, 2016 [48] | Matched pairs by age and sex | Kuopio, Finland | Vegan | 22 (16,6) | Self-reported | 8.6 |
| Omnivore | 19 (11,8) | NA | ||||
| Henjum, 2018 [38] | Cross-Sectional | Norway, eastern and western geographical regions | Vegan | 27 | Self-reported | NA |
| Vegetarian | 9 | |||||
| Omnivore | 367 | |||||
| Kristensen, 2015 [49] | Matched pairs by age | Denmark | Vegan | 75 (36,39) | Self-reported | ≤1.0 |
| Omnivore | 1627 (716, 911) | NA | ||||
| Krajcovicová-Kudlácková, 2003 [39] | Cross-sectional | Slovakia | Vegan | 15 (6,9) | Self-reported | 9.7 |
| Vegetarian | 31 (12,19) | 9.0 | ||||
| Omnivore (Mixed Diet) | 35 (15,20) | NA | ||||
| Leung, 2011 [40] | Cross-sectional | Boston, Massachusetts | Vegan | 63 | Self-reported | 11.3 ± 11.7 1 |
| Vegetarian | 78 | 5.6 ± 5.7 1 | ||||
| Lightowler, 1998 [41] | Cross-sectional | London and surrounding counties, UK | Vegan | 30 (11,19) | Self-reported | M, 10.0, F, 9.2 |
| Lightowler, 2002 [42] | Cross-sectional | London and the south-east of England, UK | Vegan | 26 (11, 15) | Self-reported | M, 9.9, F, 11.7 |
| Nebl, 2019 [43] | Cross-sectional | Hanover, Germany | Vegan | 27 (11,16) | Assessed by investigators pre-study | >2.0 |
| Vegetarian | 25 (10, 15) | >2.0 | ||||
| Omnivore | 27 (10,17) | >3.0 | ||||
| Rauma, 1994 [50] | Matched pairs | Kuopio, Finland. | Vegan (Living Food Diet) | 12 | Self-reported | 6.7 ± 3.8 1 |
| Omnivore | 12 | NA | ||||
| Remer, 1999 [47] | Repeated-measures | Germany | Vegetarian (Lacto) | 6 (3,3) | Allocated by investigators | 0.0 |
| Omnivore | 6 (3,3) | |||||
| Omnivore (High protein) | 6 (3,3) | |||||
| Schüpbach, 2017 [44] | Cross-sectional | Lausanne and Zurich, Switzerland | Vegan | 53 (20,33) | Self-reported | ≤1.0 |
| Vegetarian | 53 (17,36) | ≤1.0 | ||||
| Omnivore | 100 (37,63) | ≤1.0 | ||||
| Sobiecki, 2016 [45] | Cross-sectional | Oxford, UK | Vegan | 803 | Assessed by investigators pre-study | ≤1.0 |
| Vegetarian | 6673 | ≤1.0 | ||||
| Pescatarian | 4531 | ≤1.0 | ||||
| Omnivore (Meat-eaters) | 18,244 | ≤1.0 | ||||
| Waldmann, 2003 [46] | Cross-sectional | Hanover, Germany | Vegan (Strict) | 98 | Assessed by investigators pre-study | 4.3 |
| Vegan (Moderate) | 56 | 3.4 |
| Study, Year | Assessment of Dietary Iodine | Criteria for Iodine Intake Used in Study | Dietary Group (N) (Male, Female) | Dietary Iodine Intake (µG Day−1) | Contribution of Iodised Salt, Seaweed, and Iodine-Containing Supplements | Meeting Criteria (Y/N) |
|---|---|---|---|---|---|---|
| Allès, 2017 [36] | Three repeated 24 h dietary records. | 150 µg day−1 RDI for the French population (2001) [52]. | Vegan (789) Vegetarian (2370) Omnivore (90,664) | 248.3 ± 9.8 (a) 1 222.6 ± 5.7 (a) 1 180.1 ± 1.1 (a) 1,** | Seaweed, salt, or supplements not measured. | Y Y Y |
| Draper, 1993 [37] | Three-day weighted food diaries. Analysed using UK Ministry of Agriculture, Fisheries and Food data. | DRV of 140 µg day−1 Department of Health (1991) [53]. | Vegan (38) (18,20) | M, 98.0 ± 42.0 2,** F, 66.0 ± 22.0 2,** | 95% used sea salt or seaweed. 30%–40% consumed food supplements containing seaweed 1–2 days a month. 15.6 µg day−1 provided by dietary supplements. | N |
| Lacto-Vegetarian (52) (16,36) | M, 216.0 ± 73.0 2,** F, 167.0 ± 59.0 2,** | No iodine provided by salt, seaweed or supplements. | Y | |||
| Demi-Vegetarian (35) (13,24) | M, 253.0 ± 164.0 2,** F, 172.0 ± 91.0 2,** | No iodine provided by salt, seaweed or supplements. | Y | |||
| Kristensen, 2015 [49] | Four-day weighed food diary. | 150 µg day−1 NNR (2012) [54]. | Vegan (70) (33,37) | M, 64.0 (43.0–91.0) 3,** F, 65.0 (54.0–86.0) 3,** | Salt not measured. Three vegans consumed seaweed. 9.0 µg day−1 (M) and 6.0 µg day−1 (F) was provided by dietary supplements. | N |
| Omnivore (1257) (566,691) | M, 213.0 (180.0–269.0) 3 F, 178.0 (146.0–215.0) 3 | Salt not measured. No iodine provided by seaweed. 107 µg day−1 (M) and 78.9 µg day−1 (F) was provided by dietary supplements. | Y | |||
| Lightowler, 1998 [41] | Four-day weighed food diary with duplicate portion technique. | 140 mg day−1 RNI Department of Health (1991) [53]. | Vegan (30) (11,19) | M, 138.0 ± 149.0 2 F, 187.0 ± 246.0 2 | Salt not measured. Three vegans consumed seaweed, resulting in significantly higher iodine intake (p < 0.001) Seaweed consumers were over six times the RNI. Iodine-containing supplements were consumed by five (45%) males and seven females (37%). Providing 54.0 mg day−1 on average to the diet. | M, N F, Y |
| Lightowler, 2002 [42] | Four -day food diaries with duplicate portion technique. Analysed using CompEat 4 software. | 140 mg day−1 RNI Department of Health (1991) [53]. | Vegan (26) (11,15) | Diet Diary M, 42.0 ± 46.0 2 F, 1448.0 ± 3879.0 2 Duplicate Diary M, 137.0 ± 147.0 2 F, 216.0 ± 386.0 2 | Salt not measured. Two vegans consumed seaweed, resulting in iodine intake to exceed the RNI. Dietary supplement intake was recorded but not included to dietary intake. | Diet Diary M, N F, Y Duplicate DiaryM, N F, Y |
| Nebl, 2019 [43] | Three-day food diaries analysed by PROD16.4®. | 200 µg day−1 RV German, Austrian and Swiss Nutrition Societies (2019) [55] | Vegan (27) (10,17) | 57.7 (48.4, 67.0) 4,* | Salt or seaweed not measured. No iodine provided by supplements. | N |
| Vegetarian (25) (10,15) | 61.6 (49.4, 73.7) 4,* | N | ||||
| Omnivore (27) (11,16) | 88.8 (64.1, 114.0) 4,** | N | ||||
| Rauma, 1994 [50] | Seven-day food diaries analysed by NUTRICA Finland. | 0.1–0.2 mg day−1 RDA (120–200 µg day−1) Committee on Dietary Allowances, Food and Nutrition Board, National Research Council (1989) [56]. | Vegan (Living Food Diet) (9) | 29.0 ± 18.0 2 | One participant did not use iodised salt. 25% of daily iodine in vegans was provided by seaweed (estimated >8.0 µg day−1). Four vegans consumed seaweed, resulting in higher intake. | N |
| Omnivore (8) | 222.0 ± 93.0 2 | Y | ||||
| Remer, 1999 [47] | Five-day dietary intervention of pre-selected food items representing each diet. Calculated using food tables. | NA | Vegetarian (Ovo-Vegetarian)(6) Omnivore (6) | 15.6 ± 21.0 2 35.2 ± 15.0 2 | No iodized salt, seaweed or supplements were permitted during the study. All drinks including water were low in iodine and other minerals. | N N |
| Omnivore (High Protein) (6) | 44.5 ± 16.5 2 | N | ||||
| Waldmann, 2003 [46] | Pre-study questionnaire identifying regularly consumed foods. Two estimated nine-day FFQs using 7 days of records. | 200 mg day−1 RI, German Society of Nutrition (2000) [57] | Vegan (Strict) (98) (48,50) Vegan (Moderate) (56) (19,37) | M, 87.7 ± 30.6 2 F, 82.1 ± 34.4 2 M, 93.7 ± 27.8 2 F, 78.1 ± 25.6 2 | Salt not measured. Seaweed intake not measured. 46% of participants used some form of nutritional supplement. Iodine-specific supplements were not recorded. | N N |
| Sobiecki, 2016 [45] | 112-item semi-quantitative FFQ. Analysed based on UK Ministry of Agriculture, Fisheries and Food data. | 150 µg day−1 RDA, dietary reference intakes for iodine (2001) [58] | Vegan (803) (269,534) | M, 55.5 ± 40.0 2 F, 54.1 ± 40.0 2 Total, 58.5 (a) 2 | Salt not measured. Two participants who consumed seaweed had values close to the maximum tolerable daily intake for iodine. Supplement intakes recorded did not specify iodine content. | M, N F, Y (a), N |
| Vegetarian (6673) (1516,5157) | M, 141.0 ± 77.4 2 F, 146.1 ± 78.8 2Total, 148.1 (a) 2 | M, N F, N (a), N | ||||
| Pescatarian (4431) (782,3749) | M, 197.4 ± 84.7 2 F, 194.8 ± 85.9 2 Total, 196.8 (a) 2 | Y (a), Y | ||||
| Omnivore (Meat-Eaters) (18,244) (3798,14446) | M, 214.3 ± 85.6 2 F, 213.8 ± 85.2 2 Total, 212.2 (a) 2 | Y (a), Y |
| Country | Year | Iodate and/or Iodide | Iodine Amount (ppm) | State of Legislation |
|---|---|---|---|---|
| Boston (U.S.) | 1920 | Iodide | 43 | Mandatory |
| Denmark | 1999 | Iodide | 13 | Mandatory |
| France | 1997 | Iodide | 10–15 | Voluntary |
| Finland | 1963 | Iodide | 25 | Voluntary |
| Germany | 1981 | Iodate | 15–20 | Voluntary |
| Norway | NA | Iodide | 5 | Voluntary |
| Slovakia | 1966 | Iodide | 25 ± 10 | Mandatory |
| Switzerland | 1922 | Both | 20–30 | Voluntary |
| UK | NA | Iodide | 10–22 | Voluntary |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eveleigh, E.R.; Coneyworth, L.J.; Avery, A.; Welham, S.J.M. Vegans, Vegetarians, and Omnivores: How Does Dietary Choice Influence Iodine Intake? A Systematic Review. Nutrients 2020, 12, 1606. https://doi.org/10.3390/nu12061606
Eveleigh ER, Coneyworth LJ, Avery A, Welham SJM. Vegans, Vegetarians, and Omnivores: How Does Dietary Choice Influence Iodine Intake? A Systematic Review. Nutrients. 2020; 12(6):1606. https://doi.org/10.3390/nu12061606
Chicago/Turabian StyleEveleigh, Elizabeth R., Lisa J. Coneyworth, Amanda Avery, and Simon J. M. Welham. 2020. "Vegans, Vegetarians, and Omnivores: How Does Dietary Choice Influence Iodine Intake? A Systematic Review" Nutrients 12, no. 6: 1606. https://doi.org/10.3390/nu12061606
APA StyleEveleigh, E. R., Coneyworth, L. J., Avery, A., & Welham, S. J. M. (2020). Vegans, Vegetarians, and Omnivores: How Does Dietary Choice Influence Iodine Intake? A Systematic Review. Nutrients, 12(6), 1606. https://doi.org/10.3390/nu12061606




