Modeling Associations between Chemosensation, Liking for Fats and Sweets, Dietary Behaviors and Body Mass Index in Chronic Smokers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedures and Measures
2.2.1. Taste and Smell Function
2.2.2. Liking for Saturated Fats/Carbohydrates
2.2.3. Liking for E-juice Flavors
2.2.4. Smoking-Associated Dietary Behaviors
2.2.5. Body Mass Index
2.3. Statistical Analysis
3. Results
3.1. Body Mass Index (BMI)
3.2. Taste Function
3.3. Olfactory Function
3.4. Liking for Saturated Fats/Carbohydrates
3.5. Liking for E-juice Flavors
3.6. Smoking-Associated Dietary Behaviors
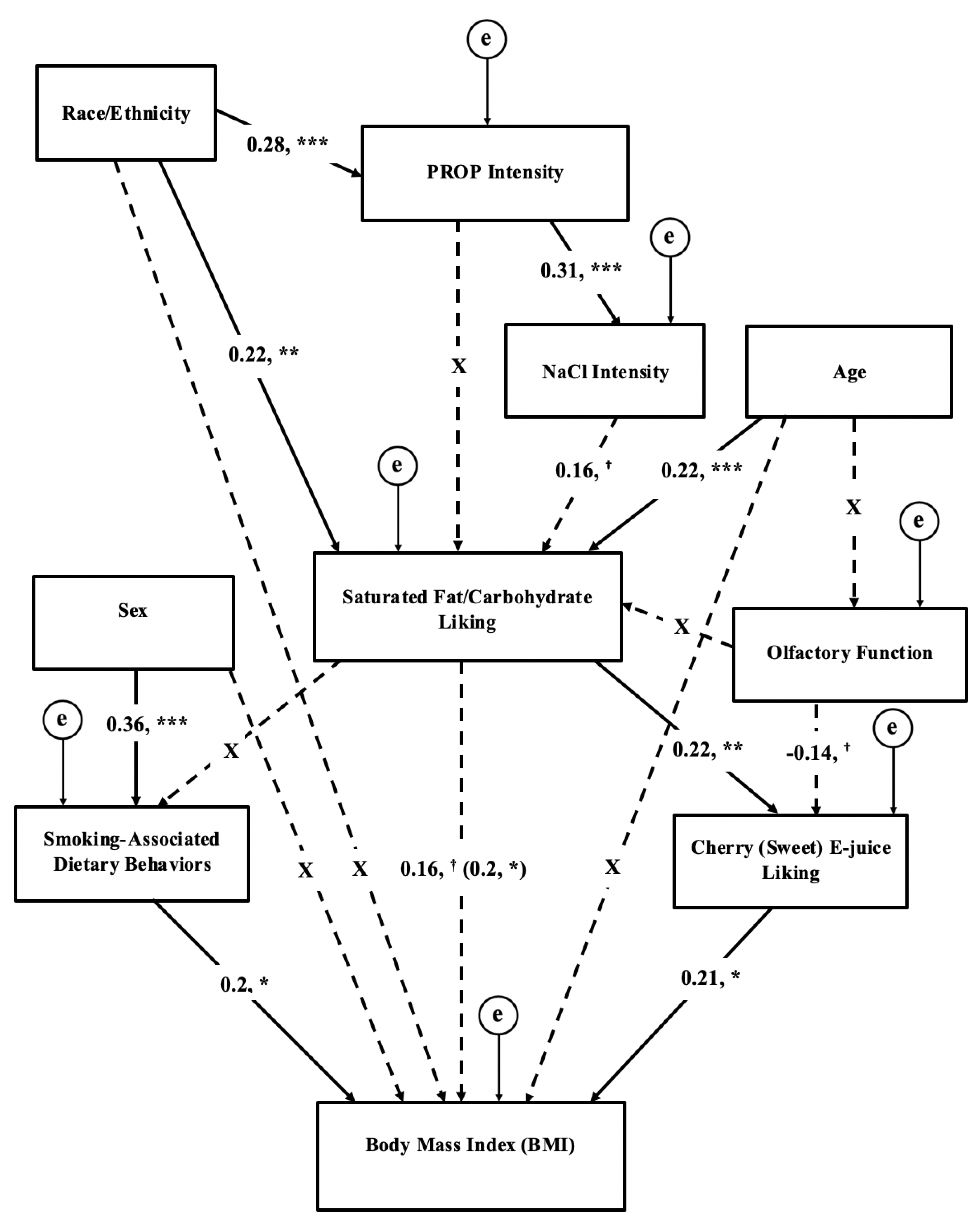
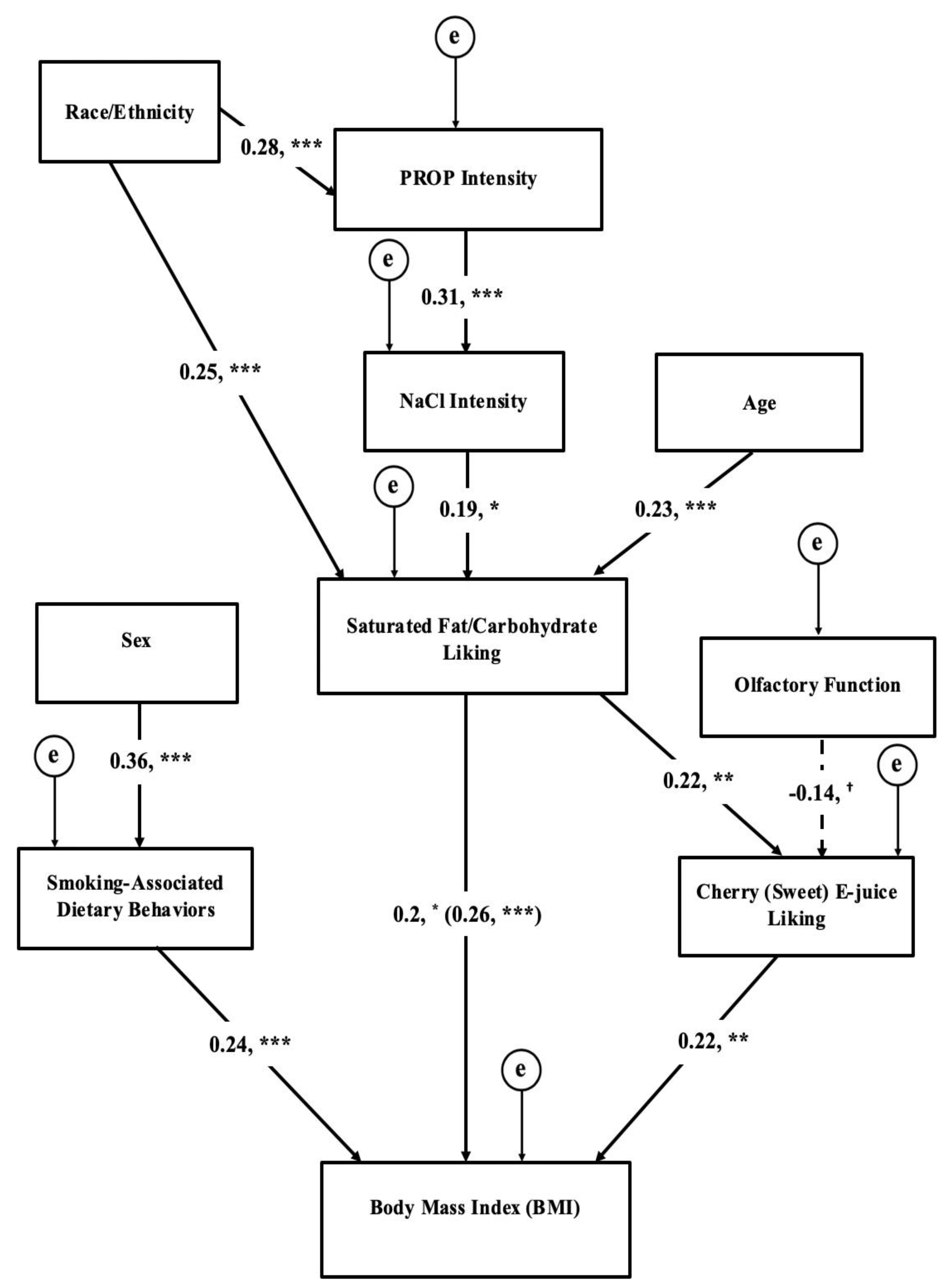
3.7. Structural Equation Modeling of Chemosensation, Liking, Behaviors, and BMI
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jamal, A.; Phillips, E.; Gentzke, A.S.; Homa, D.M.; Babb, S.D.; King, B.A.; Neff, L.J. Current Cigarette Smoking Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015-2016. NCHS Data Briefs. Available online: https://www.cdc.gov/nchs/data/databriefs/db219.pdf (accessed on 18 January 2019).
- Rupprecht, L.E.; Donny, E.C.; Sved, A.F. Obese Smokers as a Potential Subpopulation of Risk in Tobacco Reduction Policy. Yale J. Biol. Med. 2015, 88, 289–294. [Google Scholar] [PubMed]
- Mineur, Y.S.; Abizaid, A.; Rao, Y.; Salas, R.; DiLeone, R.J.; Gundisch, D.; Diano, S.; De Biasi, M.; Horvath, T.L.; Gao, X.B.; et al. Nicotine decreases food intake through activation of POMC neurons. Science 2011, 332, 1330–1332. [Google Scholar] [CrossRef] [PubMed]
- Audrain-McGovern, J.; Benowitz, N.L. Cigarette smoking, nicotine, and body weight. Clin. Pharmacol. Ther. 2011, 90, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Ginawi, I.; Bashir, A.; Alreshidi, Y.; Dirweesh, A.; Al-Hazimi, A.; Ahmed, H.; Kamal, E.; Ahmed, M. Association Between Obesity and Cigarette Smoking: A Community-Based Study. J. Endocrinol. Metab. 2016, 6, 149–153. [Google Scholar] [CrossRef]
- Jitnarin, N.; Kosulwat, V.; Rojroongwasinkul, N.; Boonpraderm, A.; Haddock, C.K.; Poston, W.S. The relationship between smoking, body weight, body mass index, and dietary intake among Thai adults: Results of the national Thai Food Consumption Survey. Asia Pac. J. Public Health 2014, 26, 481–493. [Google Scholar] [CrossRef] [PubMed]
- Mackay, D.F.; Gray, L.; Pell, J.P. Impact of smoking and smoking cessation on overweight and obesity: Scotland-wide, cross-sectional study on 40,036 participants. BMC Public Health 2013, 13, 348. [Google Scholar] [CrossRef] [PubMed]
- Dare, S.; Mackay, D.F.; Pell, J.P. Relationship between smoking and obesity: A cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE 2015, 10, e0123579. [Google Scholar] [CrossRef]
- Alkerwi, A.; Baydarlioglu, B.; Sauvageot, N.; Stranges, S.; Lemmens, P.; Shivappa, N.; Hebert, J.R. Smoking status is inversely associated with overall diet quality: Findings from the ORISCAV-LUX study. Clin. Nutr. 2017, 36, 1275–1282. [Google Scholar] [CrossRef]
- Chiolero, A.; Wietlisbach, V.; Ruffieux, C.; Paccaud, F.; Cornuz, J. Clustering of risk behaviors with cigarette consumption: A population-based survey. Prev. Med. 2006, 42, 348–353. [Google Scholar] [CrossRef]
- Lohse, T.; Rohrmann, S.; Bopp, M.; Faeh, D. Heavy Smoking Is More Strongly Associated with General Unhealthy Lifestyle than Obesity and Underweight. PLoS ONE 2016, 11, e0148563. [Google Scholar] [CrossRef] [PubMed]
- Ramallal, R.; Toledo, E.; Martinez, J.A.; Shivappa, N.; Hebert, J.R.; Martinez-Gonzalez, M.A.; Ruiz-Canela, M. Inflammatory potential of diet, weight gain, and incidence of overweight/obesity: The SUN cohort. Obesity (Silver Spring) 2017, 25, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Criscitelli, K.; Avena, N.M. The neurobiological and behavioral overlaps of nicotine and food addiction. Prev. Med. 2016, 92, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Pepino, M.Y.; Mennella, J.A. Cigarette smoking and obesity are associated with decreased fat perception in women. Obesity (Silver Spring) 2014, 22, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Duffy, V.B.; Glennon, S.G.; Larsen, B.A.; Rawal, S.; Oncken, C.; Litt, M.D. Heightened olfactory dysfunction and oral irritation among chronic smokers and heightened propylthiouracil (PROP) bitterness among menthol smokers. Physiol. Behav. 2018, 201, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Enoch, M.A.; Harris, C.R.; Goldman, D. Does a reduced sensitivity to bitter taste increase the risk of becoming nicotine addicted? Addict. Behav. 2001, 26, 399–404. [Google Scholar] [CrossRef]
- Ahijevych, K.; Tepper, B.J.; Graham, M.C.; Holloman, C.; Matcham, W.A. Relationships of PROP Taste Phenotype, Taste Receptor Genotype, and Oral Nicotine Replacement Use. Nicotine Tob. Res. 2015, 17, 1149–1155. [Google Scholar] [CrossRef]
- Dehkordi, O.; Rose, J.E.; Balan, K.V.; Millis, R.M.; Bhatti, B.; Jayam-Trouth, A. Co-expression of nAChRs and molecules of the bitter taste transduction pathway by epithelial cells of intrapulmonary airways. Life Sci. 2010, 86, 281–288. [Google Scholar] [CrossRef]
- Snedecor, S.M.; Pomerleau, C.S.; Mehringer, A.M.; Ninowski, R.; Pomerleau, O.F. Differences in smoking-related variables based on phenylthiocarbamide “taster” status. Addict. Behav. 2006, 31, 2309–2312. [Google Scholar] [CrossRef]
- Cannon, D.S.; Baker, T.B.; Piper, M.E.; Scholand, M.B.; Lawrence, D.L.; Drayna, D.T.; McMahon, W.M.; Villegas, G.M.; Caton, T.C.; Coon, H.; et al. Associations between phenylthiocarbamide gene polymorphisms and cigarette smoking. Nicotine Tob. Res. 2005, 7, 853–858. [Google Scholar] [CrossRef]
- Baker, A.N.; Miranda, A.M.; Garneau, N.L.; Hayes, J.E. Self-reported smoking status, TAS2R38 variants, and propylthiouracil phenotype: An exploratory crowdsourced cohort study. Chem. Senses 2018, 43, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Wooding, S.; Kim, U.K.; Bamshad, M.J.; Larsen, J.; Jorde, L.B.; Drayna, D. Natural selection and molecular evolution in PTC, a bitter-taste receptor gene. Am. J. Hum. Genet. 2004, 74, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Ajmani, G.S.; Suh, H.H.; Wroblewski, K.E.; Pinto, J.M. Smoking and olfactory dysfunction: A systematic literature review and meta-analysis. Laryngoscope 2017, 127, 1753–1761. [Google Scholar] [CrossRef] [PubMed]
- Boesveldt, S.; de Graaf, K. The Differential Role of Smell and Taste for Eating Behavior. Perception 2017, 46, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Tepper, B.J.; Melis, M.; Koelliker, Y.; Gasparini, P.; Ahijevych, K.L.; Tomassini Barbarossa, I. Factors Influencing the Phenotypic Characterization of the Oral Marker, PROP. Nutrients 2017, 9, 1275. [Google Scholar] [CrossRef] [PubMed]
- Tepper, B.J. Nutritional implications of genetic taste variation: The role of PROP sensitivity and other taste phenotypes. Annu. Rev. Nutr. 2008, 28, 367–388. [Google Scholar] [CrossRef] [PubMed]
- Tepper, B.J.; Banni, S.; Melis, M.; Crnjar, R.; Tomassini Barbarossa, I. Genetic sensitivity to the bitter taste of 6-n-propylthiouracil (PROP) and its association with physiological mechanisms controlling body mass index (BMI). Nutrients 2014, 6, 3363–3381. [Google Scholar] [CrossRef]
- Hayes, J.E.; Sullivan, B.S.; Duffy, V.B. Explaining variability in sodium intake through oral sensory phenotype, salt sensation and liking. Physiol. Behav. 2010, 100, 369–380. [Google Scholar] [CrossRef]
- Proserpio, C.; de Graaf, C.; Laureati, M.; Pagliarini, E.; Boesveldt, S. Impact of ambient odors on food intake, saliva production and appetite ratings. Physiol. Behav. 2017, 174, 35–41. [Google Scholar] [CrossRef]
- Boesveldt, S.; Postma, E.M.; Boak, D.; Welge-Luessen, A.; Schopf, V.; Mainland, J.D.; Martens, J.; Ngai, J.; Duffy, V.B. Anosmia-A Clinical Review. Chem. Senses 2017, 42, 513–523. [Google Scholar] [CrossRef]
- Aschenbrenner, K.; Hummel, C.; Teszmer, K.; Krone, F.; Ishimaru, T.; Seo, H.S.; Hummel, T. The influence of olfactory loss on dietary behaviors. Laryngoscope 2008, 118, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Manesse, C.; Ferdenzi, C.; Sabri, M.; Bessy, M.; Rouby, C.; Faure, F.; Bellil, D.; Jomain, S.N.; Landis, B.; Hugentobler, M.; et al. Dysosmia-Associated Changes in Eating Behavior. Chem. Percept. 2017, 10, 104–113. [Google Scholar] [CrossRef]
- Schubert, C.R.; Cruickshanks, K.J.; Fischer, M.E.; Huang, G.H.; Klein, B.E.; Klein, R.; Pankow, J.S.; Nondahl, D.M. Olfactory impairment in an adult population: The Beaver Dam Offspring Study. Chem. Senses 2012, 37, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, M.A.; Palmer, A.M.; Correa, J.B.; Brandon, T.H. Smoking by young women with restrained eating following a food prime in the context of an alternative distractor. Exp. Clin. Psychopharmacol. 2018, 26, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Kennedy, R.D.; Lagasse, L.P.; Czaplicki, L.M.; Cohen, J.E. E-cigarettes and Weight Loss-Product Design Innovation Insights from Industry Patents. Nicotine Tob. Res. 2018, 20, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Morean, M.E.; Wedel, A.V. Vaping to lose weight: Predictors of adult e-cigarette use for weight loss or control. Addict. Behav. 2017, 66, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Soule, E.K.; Lopez, A.A.; Guy, M.C.; Cobb, C.O. Reasons for using flavored liquids among electronic cigarette users: A concept mapping study. Drug Alcohol Depend. 2016, 166, 168–176. [Google Scholar] [CrossRef]
- Feirman, S.P.; Lock, D.; Cohen, J.E.; Holtgrave, D.R.; Li, T. Flavored Tobacco Products in the United States: A Systematic Review Assessing Use and Attitudes. Nicotine Tob. Res. 2016, 18, 739–749. [Google Scholar] [CrossRef]
- Kim, H.; Lim, J.; Buehler, S.S.; Brinkman, M.C.; Johnson, N.M.; Wilson, L.; Cross, K.S.; Clark, P.I. Role of sweet and other flavours in liking and disliking of electronic cigarettes. Tob. Control 2016, 25, ii55–ii61. [Google Scholar] [CrossRef]
- Audrain-McGovern, J.; Strasser, A.A.; Wileyto, E.P. The impact of flavoring on the rewarding and reinforcing value of e-cigarettes with nicotine among young adult smokers. Drug Alcohol Depend. 2016, 166, 263–267. [Google Scholar] [CrossRef]
- Kennedy, R.D.; Awopegba, A.; De Leon, E.; Cohen, J.E. Global approaches to regulating electronic cigarettes. Tob. Control 2017, 26, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Wood, L. Research and Markets: E-Cigarette & Vaporizer Market to Reach USD 50 Billion by 2025—Global Analysis & Forecast Report 2015–2025; Business Wire, Inc.: San Francisco, CA, USA, 2015. [Google Scholar]
- Sandberg, A.; Skold, C.M.; Grunewald, J.; Eklund, A.; Wheelock, A.M. Assessing recent smoking status by measuring exhaled carbon monoxide levels. PLoS ONE 2011, 6, e28864. [Google Scholar] [CrossRef] [PubMed]
- Sobell, L.C.; Sobell, M.B. Alcohol Timeline Followback Users’ Manual; Addiction Research Foundation: Toronto, ON, Canada, 1995. [Google Scholar]
- Green, B.G.; Dalton, P.; Cowart, B.; Shaffer, G.; Rankin, K.; Higgins, J. Evaluating the ‘Labeled Magnitude Scale’ for measuring sensations of taste and smell. Chem. Senses 1996, 21, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Bartoshuk, L.M.; Duffy, V.B.; Green, B.G.; Hoffman, H.J.; Ko, C.W.; Lucchina, L.A.; Marks, L.E.; Snyder, D.J.; Weiffenbach, J.M. Valid across-group comparisons with labeled scales: The gLMS versus magnitude matching. Physiol. Behav. 2004, 82, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Taste and Smell Examination Component Manual: National Health and Examination Survey (NHANES). Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/Taste_Smell.pdf (accessed on 18 January 2019).
- Zoghbi, M.; Stone, A.; Papsavas, P.; Swede, H.; Hubert, P.; Tisher, D.; Duffy, V.B. Evaluating Taste Preferences and Dietary Quality with a Simple Liking Survey: Application in Bariatric Treatment Settings. Bariatr. Surg. Pract. Patient Care 2017. [Google Scholar] [CrossRef]
- Pallister, T.; Sharafi, M.; Lachance, G.; Pirastu, N.; Mohney, R.P.; MacGregor, A.; Feskens, E.J.; Duffy, V.; Spector, T.D.; Menni, C. Food Preference Patterns in a UK Twin Cohort. Twin Res. Hum. Genet. 2015, 18, 793–805. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services, U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 2015. Available online: https://health.gov/dietaryguidelines/2015/ (accessed on 18 January 2019).
- Mead, E.L.; Duffy, V.; Oncken, C.; Litt, M.D. E-cigarette palatability in smokers as a function of flavorings, nicotine content and propylthiouracil (PROP) taster phenotype. Addict. Behav. 2018. [Google Scholar] [CrossRef]
- Smith, S.S.; Piper, M.E.; Bolt, D.M.; Fiore, M.C.; Wetter, D.W.; Cinciripini, P.M.; Baker, T.B. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 2010, 12, 489–499. [Google Scholar] [CrossRef]
- Drewnowski, A.; Hann, C. Food preferences and reported frequencies of food consumption as predictors of current diet in young women. Am. J. Clin. Nutr. 1999, 70, 28–36. [Google Scholar] [CrossRef]
- Kendzor, D.E.; Businelle, M.S.; Cofta-Woerpel, L.M.; Reitzel, L.R.; Castro, Y.; Vidrine, J.I.; Mazas, C.A.; Cinciripini, P.M.; Wetter, D.W. Mechanisms linking socioeconomic disadvantage and BMI in smokers. Am. J. Health Behav. 2013, 37, 587–598. [Google Scholar] [CrossRef]
- Fan, M.; Su, M.; Tan, Y.; Liu, Q.; Ren, Y.; Li, L.; Lv, J. Gender, Age, and Education Level Modify the Association between Body Mass Index and Physical Activity: A Cross-Sectional Study in Hangzhou, China. PLoS ONE 2015, 10, e0125534. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.A.; Bartoshuk, L.M.; Fillingim, R.B.; Dotson, C.D. Exploring Ethnic Differences in Taste Perception. Chem. Senses 2016, 41, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Dinehart, M.E.; Hayes, J.E.; Bartoshuk, L.M.; Lanier, S.L.; Duffy, V.B. Bitter taste markers explain variability in vegetable sweetness, bitterness, and intake. Physiol. Behav. 2006, 87, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Buuren, S.V.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Allyn and Bacon: Boston, MA, USA, 2001; Volume xxvi. [Google Scholar]
- Lee, S.Y.; Wang, S.J. Sensitivity analysis of structural equation models. Psychometrika 1996, 61, 93–108. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Press: New York, NY, USA, 1998; Volume xiv. [Google Scholar]
- Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion. Behavioral Risk Factor Surveillance System Prevalence & Trends Data. Available online: https://www.cdc.gov/brfss/brfssprevalence/ (accessed on 18 January 2019).
- Tanaka, A.; Cui, R.; Kitamura, A.; Liu, K.; Imano, H.; Yamagishi, K.; Kiyama, M.; Okada, T.; Iso, H.; Investigators, C. Heavy Alcohol Consumption is Associated with Impaired Endothelial Function. J. Atheroscler. Thromb. 2016, 23, 1047–1054. [Google Scholar] [CrossRef] [PubMed]
- Tepper, B.J.; Ullrich, N.V. Influence of genetic taste sensitivity to 6-n-propylthiouracil (PROP), dietary restraint and disinhibition on body mass index in middle-aged women. Physiol. Behav. 2002, 75, 305–312. [Google Scholar] [CrossRef]
- Hoffman, H.J.; Rawal, S.; Li, C.M.; Duffy, V.B. New chemosensory component in the U.S. National Health and Nutrition Examination Survey (NHANES): First-year results for measured olfactory dysfunction. Rev. Endocr. Metab. Disord. 2016, 17, 221–240. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among US adults? J. Am. Diet Assoc. 2011, 111, 1904–1911. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X. Between-group differences in nutrition- and health-related psychosocial factors among US adults and their associations with diet, exercise, and weight status. J. Acad. Nutr. Diet. 2012, 112, 486–498. [Google Scholar] [CrossRef]
- Sharafi, M.; Rawal, S.; Fernandez, M.L.; Huedo-Medina, T.B.; Duffy, V.B. Taste phenotype associates with cardiovascular disease risk factors via diet quality in multivariate modeling. Physiol. Behav. 2018, 194, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.E.; Cruickshanks, K.J.; Pankow, J.S.; Pankratz, N.; Schubert, C.R.; Huang, G.H.; Klein, B.E.; Klein, R.; Pinto, A. The associations between 6-n-propylthiouracil (PROP) intensity and taste intensities differ by TAS2R38 haplotype. J. Nutrigenet. Nutrigenom. 2014, 7, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Bartoshuk, L.M.; Duffy, V.B.; Hayes, J.E.; Moskowitz, H.R.; Snyder, D.J. Psychophysics of sweet and fat perception in obesity: Problems, solutions and new perspectives. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 1137–1148. [Google Scholar] [CrossRef] [PubMed]
- Duffy, V.B. Associations between oral sensation, dietary behaviors and risk of cardiovascular disease (CVD). Appetite 2004, 43, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Hayes, J.E.; Duffy, V.B. Oral sensory phenotype identifies level of sugar and fat required for maximal liking. Physiol. Behav. 2008, 95, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Tepper, B.J.; Nurse, R.J. PROP taster status is related to fat perception and preference. Ann. N. Y. Acad. Sci. 1998, 855, 802–804. [Google Scholar] [CrossRef]
- Stevenson, R.J.; Boakes, R.A.; Oaten, M.J.; Yeomans, M.R.; Mahmut, M.; Francis, H.M. Chemosensory Abilities in Consumers of a Western-Style Diet. Chem. Senses 2016, 41, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Risso, D.S.; Mezzavilla, M.; Pagani, L.; Robino, A.; Morini, G.; Tofanelli, S.; Carrai, M.; Campa, D.; Barale, R.; Caradonna, F.; et al. Global diversity in the TAS2R38 bitter taste receptor: Revisiting a classic evolutionary PROPosal. Sci. Rep. 2016, 6, 25506. [Google Scholar] [CrossRef]
- Choi, S.E. Racial differences between African Americans and Asian Americans in the effect of 6-n-propylthiouracil taste intensity and food liking on body mass index. J. Acad. Nutr. Diet. 2014, 114, 938–944. [Google Scholar] [CrossRef]
- Sharafi, M.; Duffy, V.B.; Miller, R.J.; Winchester, S.B.; Huedo-Medina, T.B.; Sullivan, M.C. Dietary behaviors of adults born prematurely may explain future risk for cardiovascular disease. Appetite 2016, 99, 157–167. [Google Scholar] [CrossRef]
- Duffy, V.B.; Lanier, S.A.; Hutchins, H.L.; Pescatello, L.S.; Johnson, M.K.; Bartoshuk, L.M. Food preference questionnaire as a screening tool for assessing dietary risk of cardiovascular disease within health risk appraisals. J. Am. Diet. Assoc. 2007, 107, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Duffy, V.B.; Hayes, J.E.; Sullivan, B.S.; Faghri, P. Surveying food and beverage liking: A tool for epidemiological studies to connect chemosensation with health outcomes. Ann. N. Y. Acad. Sci. 2009, 1170, 558–568. [Google Scholar] [CrossRef] [PubMed]
- Deglaire, A.; Mejean, C.; Castetbon, K.; Kesse-Guyot, E.; Hercberg, S.; Schlich, P. Associations between weight status and liking scores for sweet, salt and fat according to the gender in adults (The Nutrinet-Sante study). Eur. J. Clin. Nutr. 2015, 69, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Lampure, A.; Castetbon, K.; Deglaire, A.; Schlich, P.; Peneau, S.; Hercberg, S.; Mejean, C. Associations between liking for fat, sweet or salt and obesity risk in French adults: A prospective cohort study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 74. [Google Scholar] [CrossRef] [PubMed]
- De Biasi, M.; Dani, J.A. Reward, addiction, withdrawal to nicotine. Annu. Rev. Neurosci. 2011, 34, 105–130. [Google Scholar] [CrossRef]
- Perkins, K.A.; Epstein, L.H.; Stiller, R.L.; Fernstrom, M.H.; Sexton, J.E.; Jacob, R.G. Perception and hedonics of sweet and fat taste in smokers and nonsmokers following nicotine intake. Pharmacol. Biochem. Behav. 1990, 35, 671–676. [Google Scholar] [CrossRef]
- Farsalinos, K.E.; Polosa, R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: A systematic review. Ther. Adv. Drug Saf. 2014, 5, 67–86. [Google Scholar] [CrossRef]
- Litt, M.D.; Duffy, V.; Oncken, C. Cigarette smoking and electronic cigarette vaping patterns as a function of e-cigarette flavourings. Tob. Control 2016, 25, ii67–ii72. [Google Scholar] [CrossRef]
- Rosbrook, K.; Erythropel, H.C.; DeWinter, T.M.; Falinski, M.; O’Malley, S.; Krishnan-Sarin, S.; Anastas, P.T.; Zimmerman, J.B.; Green, B.G. The effect of sucralose on flavor sweetness in electronic cigarettes varies between delivery devices. PLoS ONE 2017, 12, e0185334. [Google Scholar] [CrossRef]
- Kroemer, N.B.; Veldhuizen, M.G.; Delvy, R.; Patel, B.P.; O’Malley, S.S.; Small, D.M. Sweet taste potentiates the reinforcing effects of e-cigarettes. Eur. Neuropsychopharmacol. 2018, 28, 1089–1102. [Google Scholar] [CrossRef]
- Soberg, S.; Sandholt, C.H.; Jespersen, N.Z.; Toft, U.; Madsen, A.L.; von Holstein-Rathlou, S.; Grevengoed, T.J.; Christensen, K.B.; Bredie, W.L.P.; Potthoff, M.J.; et al. FGF21 Is a Sugar-Induced Hormone Associated with Sweet Intake and Preference in Humans. Cell Metab. 2017, 25, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Sylvetsky, A.C.; Welsh, J.A.; Brown, R.J.; Vos, M.B. Low-calorie sweetener consumption is increasing in the United States. Am. J. Clin. Nutr. 2012, 96, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Mosdol, A.; Vist, G.E.; Svendsen, C.; Dirven, H.; Lillegaard, I.T.L.; Mathisen, G.H.; Husoy, T. Hypotheses and evidence related to intense sweeteners and effects on appetite and body weight changes: A scoping review of reviews. PLoS ONE 2018, 13, e0199558. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.E.; Perez, V. Low-calorie sweeteners and body weight and composition: A meta-analysis of randomized controlled trials and prospective cohort studies. Am. J. Clin. Nutr. 2014, 100, 765–777. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Abou-Setta, A.M.; Chauhan, B.F.; Rabbani, R.; Lys, J.; Copstein, L.; Mann, A.; Jeyaraman, M.M.; Reid, A.E.; Fiander, M.; et al. Nonnutritive sweeteners and cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 2017, 189, E929–E939. [Google Scholar] [CrossRef] [PubMed]
- Berridge, K.C. Wanting and Liking: Observations from the Neuroscience and Psychology Laboratory. Inquiry (Oslo) 2009, 52, 378. [Google Scholar] [CrossRef] [PubMed]
- Piasecki, T.M.; Piper, M.E.; Baker, T.B.; Hunt-Carter, E.E. WISDM primary and secondary dependence motives: Associations with self-monitored motives for smoking in two college samples. Drug Alcohol Depend. 2011, 114, 207–216. [Google Scholar] [CrossRef]
- Bel-Serrat, S.; Julian-Almarcegui, C.; Gonzalez-Gross, M.; Mouratidou, T.; Bornhorst, C.; Grammatikaki, E.; Kersting, M.; Cuenca-Garcia, M.; Gottrand, F.; Molnar, D.; et al. Correlates of dietary energy misreporting among European adolescents: The Healthy Lifestyle in Europe by Nutrition in Adolescence (HELENA) study. Br. J. Nutr. 2016, 115, 1439–1452. [Google Scholar] [CrossRef]
- Tuorila, H.; Huotilainen, A.; Lähteenmäki, L.; Ollila, S.; Tuomi-Nurmi, S.; Urala, N. Comparison of affective rating scales and their relationship to variables reflecting food consumption. Food Qual. Pref. 2008, 19, 51–61. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef]
- Murphy, C.M.; Rohsenow, D.J.; Johnson, K.C.; Wing, R.R. Smoking and weight loss among smokers with overweight and obesity in Look AHEAD. Health Psychol. 2018, 37, 399–406. [Google Scholar] [CrossRef] [PubMed]
| Variable Number | Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | 1 | |||||||
| 2 | PROP intensity | 0.05 | 1 | ||||||
| 3 | 0.32 NaCl intensity | 0.09 | 0.32 c | 1 | |||||
| 4 | Fat/carb liking | 0.29 c | 0.18 a | 0.22 a | 1 | ||||
| 5 | SDBI | 0.11 | 0.08 | 0.01 | −0.11 | 1 | |||
| 6 | Olfaction | −0.12 | 0.06 | −0.06 | −0.18 a | 0.03 | 1 | ||
| 7 | Sweet E-J liking | 0.12 | −0.01 | 0.03 | 0.26 c | −0.02 | −0.19 a | 1 | |
| 8 | BMI | 0.17 | 0.07 | −0.07 | 0.24 b | 0.22 a | −0.02 | 0.27 c | 1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larsen, B.A.; Litt, M.D.; Huedo-Medina, T.B.; Duffy, V.B. Modeling Associations between Chemosensation, Liking for Fats and Sweets, Dietary Behaviors and Body Mass Index in Chronic Smokers. Nutrients 2019, 11, 271. https://doi.org/10.3390/nu11020271
Larsen BA, Litt MD, Huedo-Medina TB, Duffy VB. Modeling Associations between Chemosensation, Liking for Fats and Sweets, Dietary Behaviors and Body Mass Index in Chronic Smokers. Nutrients. 2019; 11(2):271. https://doi.org/10.3390/nu11020271
Chicago/Turabian StyleLarsen, Brittany A., Mark D. Litt, Tania B. Huedo-Medina, and Valerie B. Duffy. 2019. "Modeling Associations between Chemosensation, Liking for Fats and Sweets, Dietary Behaviors and Body Mass Index in Chronic Smokers" Nutrients 11, no. 2: 271. https://doi.org/10.3390/nu11020271
APA StyleLarsen, B. A., Litt, M. D., Huedo-Medina, T. B., & Duffy, V. B. (2019). Modeling Associations between Chemosensation, Liking for Fats and Sweets, Dietary Behaviors and Body Mass Index in Chronic Smokers. Nutrients, 11(2), 271. https://doi.org/10.3390/nu11020271






