Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal
Abstract
1. Introduction
2. Food-Based Dietary Guidelines
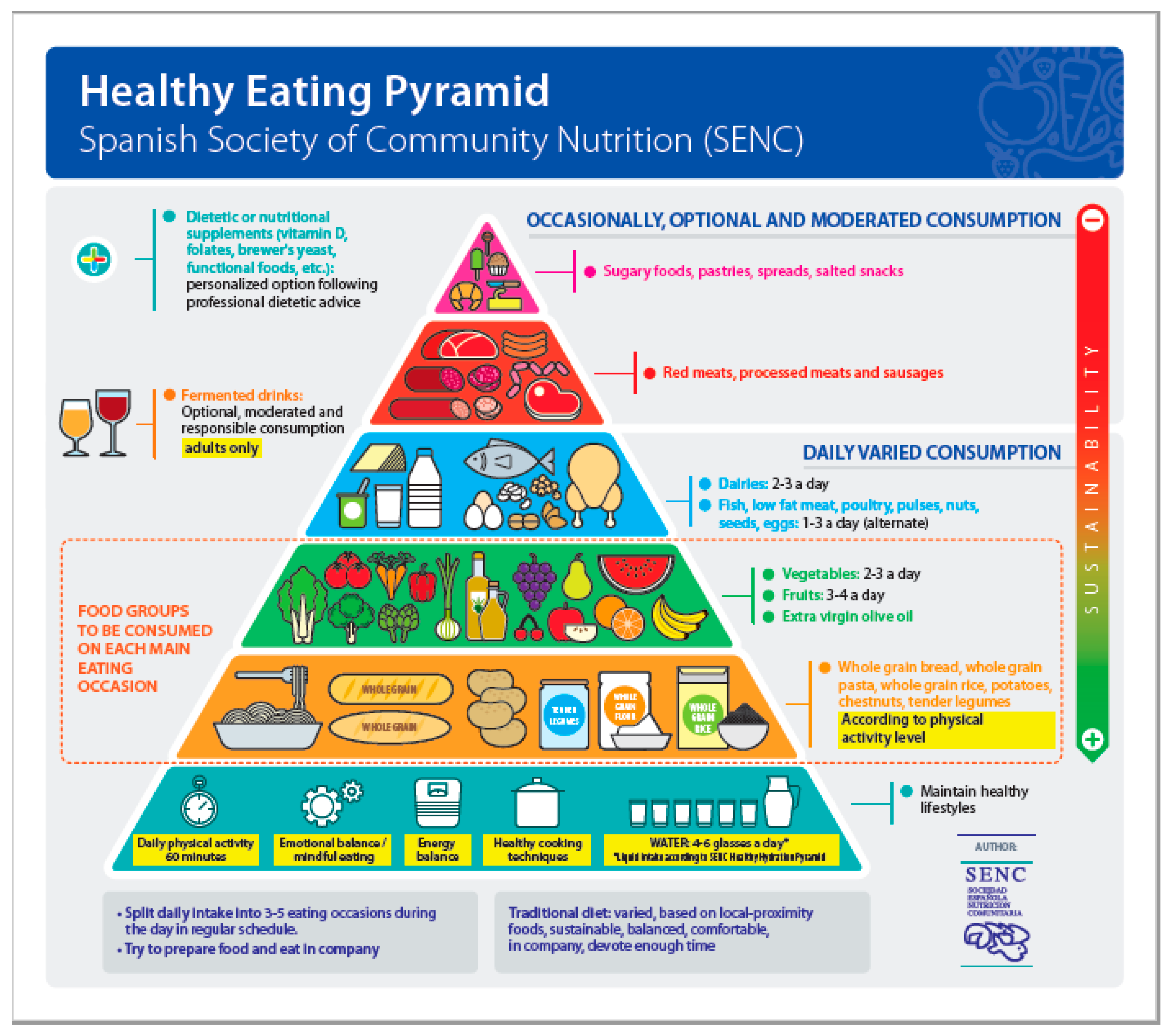
3. The Contribution of the Spanish Society of Community Nutrition to FBDGs in Spain
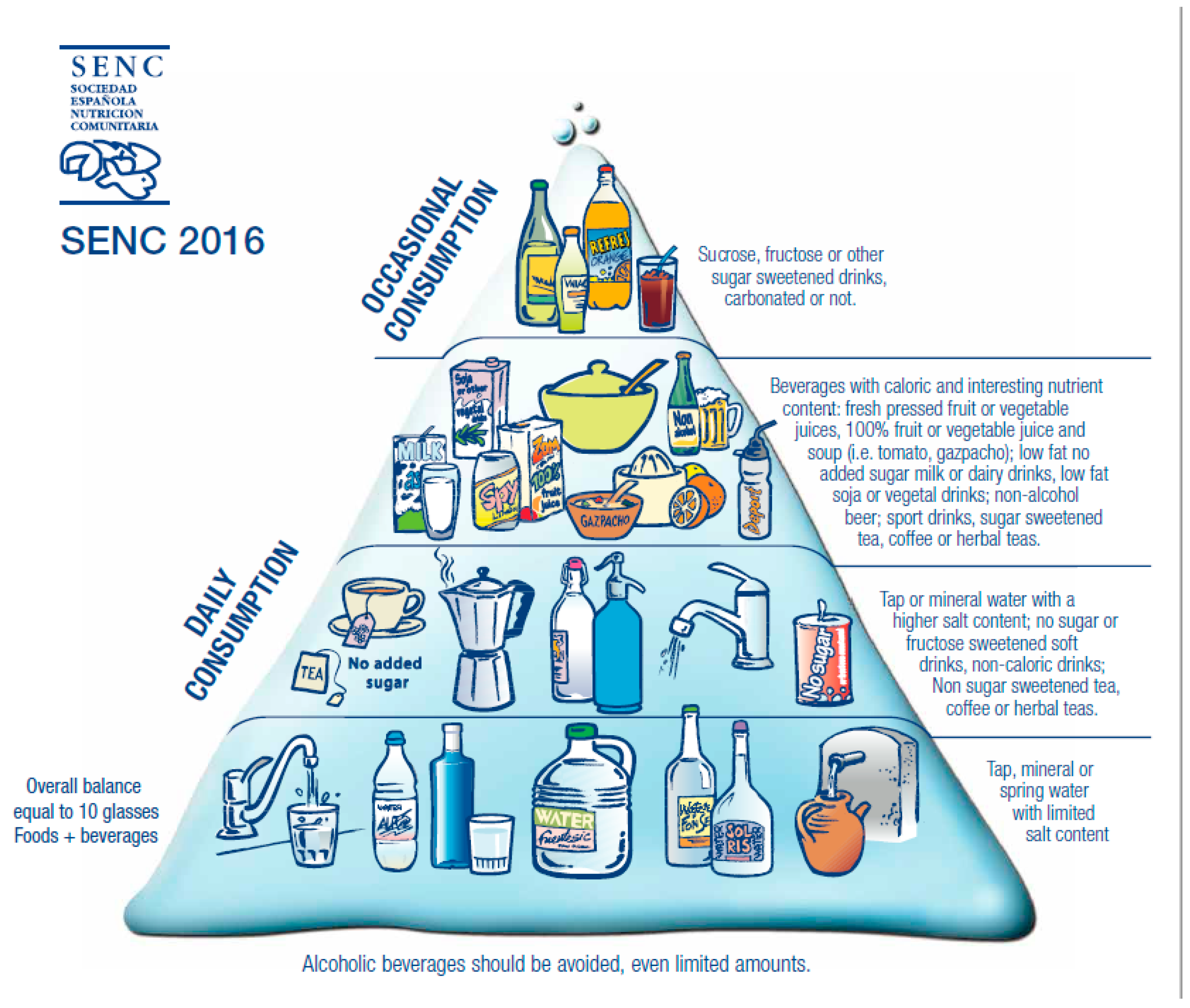
4. New Food-Based Dietary Guidelines for the Spanish Population
- People who do not use alcoholic beverages should not start drinking because of the potential beneficial effects attributed to low-grade fermented alcoholic beverages. An optimal diet can achieve equivalent results without the potential risks of drinking alcoholic beverages, even if they have low alcohol content.
- Drinks that can be considered are limited exclusively to low-grade fermented alcoholic beverages (wine, beer, cider, cava, or champagne (sparkling wines with double fermentation)).
- People with chronic diseases or taking medications or supplements should consult with a doctor and follow recommendations at all times, even if advised to avoid alcohol altogether.
- Spirits and liquor should be avoided in the context of a healthy diet and lifestyle.
- In Spain, there are good-tasting, socially acceptable alternatives for private or social consumption of alcoholic beverages, such as non-alcoholic beer, de-alcoholized wines, and similar products available in virtually all establishments in the country.
- Regarding the location of fermented beverages external to the main content of the Healthy Eating Pyramid and the specific section in the FBDGs, the decisive factor was that, in Spain, wine is legally considered “food” (Ministry of Agriculture, Fisheries and Food), aside from its important cultural, gastronomic, economic, and social value. Excluding this reference and similar beverages from the graphical representation or from the contents of the FBDGs would not per se prevent excessive or inappropriate consumption and, most importantly, it would mean that the Guide could not clearly provide criteria and limits for consumption or its reasoned exclusion.
4.1. Collaboration with the Scientific Societies of Family and Community Medicine
- Its use in primary healthcare centers and clinics in public and private healthcare systems, both in healthcare practice and in health promotion programs;
- Stimulation of brief dietary advice in healthcare practice, whenever deemed suitable;
- Bolsters healthcare practitioners to address the demands of information by patients with greater confidence in the proposed recommendations;
- Helps healthcare professionals to feel confident because they have updated, agreed upon, approved, and homogeneous criteria in hand for application and points of reference (health center, pharmacy, nursing or diet and nutrition consultation);
- Enables its use as a resource in educational settings and other community groups in information and health education actions.
4.2. New Sections: Diet in the 21st Century
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
- 9
- Faculty of Medicine and Health Sciences, Universitat Rovira i Virgili, 43201 Reus, Tarragona, Spain; victoria.arija@urv.cat
- 10
- Grupo de Nutrición SEMG, 28005 Madrid, Spain; lupe@semg.es
- 11
- Servicio de Salud de Aragón, 50013 Zaragoza, Spain
- 12
- COMPASS Group Spain, 28054 Madrid, Spain; beatriz.dediego@compass-group.es
- 13
- Coordinador del Grupo de Nutrición de SEMERGEN, 28009 Madrid, Spain; Jose.Manuel.Fernandez.Garcia@sergas.es
- 14
- Servicio Gallego de Salud, 15970 Santiago de Compostela, Spain
- 15
- Department of Physiology, University of Murcia, Murcia Spain; garaulet@um.es
- 16
- Hospital Universitario Ramón y Cajal, 28034 Madrid, Spain; maria.garriga@salud.madrid.org
- 17
- Biobanco Vasco para la Investigación-Fundación Vasca de Innovación e Investigación Sanitarias (BIOEF), 48902 Barakaldo, Spain; Martagnz_2@hotmail.com
- 18
- Institute of Nutrition and Food Sciences, University of Granada, 18010 Granada, Spain; agil@ugr.es; emiliom@ugr.es
- 19
- Fundación Iberoamericana de Nutrición, FINUT, 18016 Armilla Granada, Spain
- 20
- SEPEAP, 08006 Barcelona, Spain; venancioms@telecable.es
- 21
- Centro de Salud El Llano, Servicio Asturiano de Salud, 33209 Gijón, Spain
- 22
- Conselleria de Sanidad Universal y Salud Pública. Generalitat Valenciana, Valencia, Spain; quiles_joa@gva.es
- 23
- Universidad de Cádiz, 11009 Cádiz, Spain; amelia.rodriguez@uca.es
- 24
- National Center for Epidemiology, Carlos III Institute of Health, Avda. Monforte de Lemos, 5, 28029 Madrid, Spain; e.ruiz@externos.isciii.es
- 25
- CIBERESP (Consortium for Biomedical Research in Epidemiology and Public Health), Madrid, Spain
- 26
- Departament de Salut, Generalitat de Catalunya, 08005 Barcelona, Spain; gemma.salvador@gencat.cat
- 27
- Research Group on Community Nutrition & Oxidative Stress, University of the Balearic Islands, 07122 Palma de Mallorca, Spain; pep.tur@uib.es
- 28
- Nutrición Sin Fronteras, 08029 Barcelona, Spain; merce@nutricionsinfronteras.org
References
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi-Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 diseases, 1990–2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef]
- European Commission. Cost of Non-Communicable Diseases in the EU. Available online: https://ec.europa.eu/jrc/en/health-knowledge-gateway/societal-impacts/costs (accessed on 1 October 2019).
- FAO. Sustainable diets and biodiversity FAO. In Proceedings of the FAO International Scientific Symposium, Biodiversity and Sustainable Diets, Rome, Italy, 3–5 November 2012. [Google Scholar]
- Meybeck, A.; Gitz, V. Sustainable diets within sustainable food systems. Proc. Nutr. Soc. 2017, 76, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dernini, S.; Larion, D.; Berry, E.M.; Brunori, G.; Capone, R.; Donini, L.M.; Iannetta, M.; Mattioni, D.; Piscopo, S.; Serra-Majem, L.; et al. The Med Diet 4.0 framework: A multidimensional driver for revitalizing the Mediterranean Diet as a sustainable diet model. In Sustainable Diets: Linking Nutrition and Food Systems; Burlingame, B., Dernini, S., Eds.; CABI: Boston, MA, USA, 2019; pp. 187–198. [Google Scholar]
- World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. Sustainable Development Goals (SDGs); WHO: Geneva, Switzerland; Available online: https://www.who.int/sdg/en/ (accessed on 1 October 2019).
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013, 380, 2224–2260. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Missbach, B.; König, J.; Hoffmann, G. Adherence to a Mediterranean diet and risk of diabetes: A systematic review and meta-analysis. Public Health Nutr. 2015, 1, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific Opinion on establishing Food-Based Dietary Guidelines. EFSA J. 2010, 8, 1460.
- FAO/WHO. Preparation and Use of Food-Based Dietary Guidelines; Nutrition Programme-WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Aranceta Bartrina, J.; Serra Majem, L.L. (Eds.) Objetivos nutricionales y guias dieteticas. In Nutricion y Salud Pública. Métodos, Bases Científicas y Aplicaciones, 2nd ed.; Elsevier: Barcelona, Spain, 2006; pp. 684–697. [Google Scholar]
- Bechthold, A.; Boeing, H.; Tetens, I.; Schwingshackl, L.; Nothlings, U. Perspective: Food-based dietary guidelines in Europe—Scientific concepts, current status, and perspectives. Adv. Nutr. 2018, 9, 544–560. [Google Scholar] [CrossRef]
- Varela Moreiras, G.; Serra Majem, L.; Aranceta-Bartrina, J. Conclusions. Nutrition and gastronomy in the different autonomous communities. Gastronomy from Segovia in national context. Nutr. Hosp. 2019, 36, 139–141. (In Spanish) [Google Scholar] [CrossRef]
- Pérez-Rodrigo, C.; Aranceta-Bartrina, J. National Diet Recommendations. In Encyclopedia of Food Security and Sustainability; Ferranti, P., Berry, E.M., Anderson, J.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; Volume 2, pp. 275–282. [Google Scholar]
- Erve, I.; Tulen, C.B.M.; Jansen, J.; Minnema, R.; Schenk, P.R.; Wolvers, D.; van Rossum, C.T.M.; Verhagen, H. Overview of Elements within National Food-Based Dietary Guidelines. Eur. J. Nutr. Food Saf. 2017, 7, 1–56. [Google Scholar]
- Herforth, A.; Arimond, M.; Álvarez-Sánchez, C.; Coates, J.; Christianson, K.; Muehlhoff, E. A Global Review of Food-Based Dietary Guidelines. Adv. Nutr. 2019, 10, 590–605. [Google Scholar] [CrossRef]
- Ferguson, J.F.; Allayee, H.; Gerszten, R.E.; Ideraabdullah, F.; Kris-Etherton, P.M.; Ordovás, J.M.; Rimm, E.B.; Wang, T.J.; Bennett, B.J. American Heart Association Council on Functional Genomics and Translational Biology, Council on Epidemiology and Prevention, and Stroke Council. Nutrigenomics, the Microbiome, and Gene-Environment Interactions: New Directions in Cardiovascular Disease Research, Prevention, and Treatment: A Scientific Statement from the American Heart Association. Circ. Cardiovasc. Genet. 2016, 9, 291–313. [Google Scholar]
- Magni, P.; Bier, D.M.; Pecorelli, S.; Agostoni, C.; Astrup, A.; Brighenti, F.; Cook, R.; Folco, E.; Fontana, L.; Gibson, R.A.; et al. Perspective: Improving nutritional guidelines for sustainable health policies: Current status and perspectives. Adv. Nutr. 2017, 8, 532–545. [Google Scholar] [PubMed]
- Jager, M.J.; van der Sande, R.; Essink-Bot, M.L.; van den Muijsenbergh, M.E.T.C. Views and experiences of ethnic minority diabetes patients on dietetic care in the Netherlands—A qualitative study. Eur. J. Public Health 2019, 29, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Bero, L. Developing reliable dietary guidelines. BMJ 2017, 359, j4845. [Google Scholar] [CrossRef] [PubMed]
- Blake, P.; Durão, S.; Naude, C.E.; Bero, L. An analysis of methods used to synthesize evidence and grade recommendations in food-based dietary guidelines. Nutr. Rev. 2018, 76, 290–300. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019. [Google Scholar] [CrossRef]
- Nordic Council of Ministers. Nordic Nutrition Recommendations 2012. Integrating Nutrition and Physical Activity, 5th ed.; Nordic Council of Ministers, Nordic Council of Ministers Secretariat: Copenhagen, Denmark, 2014.
- Pan American Health Organization (PAHO); Institute of Nutrition of Central America and Panama (INCAP). Food-Based Dietary Guidelines and Health Promotion in Latin America; PAHO: Washington, DC, USA; INCAP: Washington, DC, USA, 1999. [Google Scholar]
- WHO. Regional Office for the Western Pacific. Development of Food based Dietary Guidelines for the Western Pacific Region; WHO: Manila, Philippines, 1999. [Google Scholar]
- Aranceta, J.; Pérez-Rodrigo, C.; Serra Majem, L.L. Nutrición comunitaria. Rev. Med. Univ. Navar. 2006, 50, 39–45. [Google Scholar]
- Gil, A.; Mañas, M.; Martínez de Victoria, E. Guías alimentarias y estilos de vida saludable. In Tratado de Nutrición, 3rd ed.; Tomo, I.V., Gil, A., Eds.; Panamericana: Madrid, Spain, 2017; pp. 49–66. [Google Scholar]
- Bengoa, J.M. About the 2nd World Basque Conference. The Nutrition Symposium. Donosti, 1987. Gac. Médica De Bilbao 2003, 100, 28–29. [Google Scholar]
- Tormo Santamaría, M.; Trescastro López, E.; Pereyra Zamora, P.; Galiana Sánchez, M.; Bernabeu-Mestre, J. The health educator network as a nutrition education strategy: The example of the EDALNU programme (1963–1994). Nutr. Hosp. 2017, 34, 738–744. [Google Scholar] [CrossRef]
- Serra Majem, L.; Aranceta, J.; Mataix, J. Documento de Consenso: Guías Alimentarias para la Población Española; SG-Editores: Barcelona, Spain, 1995; pp. 1–318. [Google Scholar]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61 (Suppl. 6), 1402S–1406S. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Lloveras, G.; Salleras, L. Changing patterns of fat consumption in Spain. Eur. J. Clin. Nutr. 1993, 47 (Suppl. 1), S13–S20. [Google Scholar]
- SENC. Guías Alimentarias para la Población Española: Recomendaciones para una Dieta Saludable; IM&C, S.A: Madrid, Spain, 2001; pp. 1–502. [Google Scholar]
- SENC. Guía Práctica Sobre Hábitos de Alimentación y Salud; SENC-Instituto Omega 3: Madrid, Spain, 2002. [Google Scholar]
- Aranceta, J.; Pérez Rodrigo, C.; Serra Alías, M.; Iraeta Aranbarri, I.; Bellido López-Para, A.; Barinagarrementeria Balentziaga, A.; Fernández Escobedo, A. Alimentación Saludable. Guía para el Profesorado. Programa Perseo; AESAN: Madrid, Spain, 2007; pp. 1–120. [Google Scholar]
- Dapcich, V.; Salvador Castell, G.; Ribas Barba, L.; Pérez Rodrigo, C.; Aranceta Bartrina, J.; Serra Majem, L.L. Guía de la Alimentación Saludable; Everest-SENC: Madrid, Spain, 2005. [Google Scholar]
- AESAN. Pirámide NAOS. Available online: http://www.aecosan.msssi.gob.es/AECOSAN/web/nutricion/subseccion/piramide_NAOS.htm (accessed on 1 October 2019).
- SENC. Objetivos nutricionales para la población española. Consenso de la Sociedad Española de Nutrición Comunitaria 2011. Rev. Esp. Nutr. Comunitaria 2011, 17, 178–199. [Google Scholar]
- Grupo colaborativo de la Sociedad Española de Nutrición Comunitaria (SENC). Guías alimentarias para la población española (SENC, 2016): La nueva pirámide de la alimentación saludable. Nutr. Hosp. 2016, 33 (Suppl. 8), 1–48. [Google Scholar]
- Grupo de Expertos SENC-Observatorio de la Nutrición y Actividad Física. Guía para una hidratación saludable. La Declaración de Zaragoza. SENC, 2008. Rev Esp. Nutr. Comunitaria 2009, 15, 225–230. [Google Scholar]
- Aranceta, J. (Ed.) Guía de la Alimentación Saludable para Atención Primaria y Colectivos Ciudadanos; SENC-Planeta: Madrid, Spain, 2018. [Google Scholar]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- Gil, A.; Ruiz-Lopez, M.D.; Fernandez-Gonzalez, M.; Martinez de Victoria, E. The FINUT Healthy Lifestyles Guide: Beyond the Food Pyramid. Adv. Nutr. 2014, 5, 358S–367S. [Google Scholar] [CrossRef] [PubMed]
- Sáez-Almendros, S.; Obrador, B.; Bach-Faig, A.; Serra-Majem, L. Environmental footprints of Mediterranean versus Western dietary patterns: Beyond the health benefits of the Mediterranean diet. Environ. Health 2013, 12, 118. [Google Scholar] [CrossRef]
- WWF. LiveWell in Spain. Available online: http://livewellforlife.eu/livewell-plate/livewell-in-spain (accessed on 1 October 2019).
- Baute, V.; Sampath-Kumar, R.; Nelson, S.; Basil, B. Nutrition Education for the Health-care Provider Improves Patient Outcomes. Glob. Adv. Health. Med. 2018, 7, 2164956118795995. [Google Scholar] [CrossRef]
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition in medical education: A systematic review. Lancet Planet Health 2019, 3, e379–e389. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- Nicklas, T.A.; Jahns, L.; Bogle, M.L.; Chester, D.N.; Giovanni, M.; Klurfeld, D.M.; Laugero, K.; Liu, Y.; Lopez, S.; Tucker, K.L. Barriers and facilitators for consumer adherence to the dietary guidelines for Americans: The HEALTH study. J. Acad. Nutr. Diet 2013, 113, 1317–1331. [Google Scholar] [CrossRef]
- Bisogni, C.A.; Jastran, M.; Seligson, M.; Thompson, A. How people interpret healthy eating: Contributions of qualitative research. J. Nutr. Educ. Behav. 2012, 44, 282–301. [Google Scholar] [CrossRef] [PubMed]
- Mertens, E.; van’t Veer, P.; Hiddink, G.J.; Steijns, J.M.; Kuijsten, A. Operationalising the health aspects of sustainable diets: A review. Public Health Nutr. 2016, 20, 739–757. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Bes-Rastrollo, M.; de Gaetano, G.; Iacoviello, L. Challenges to the Mediterranean diet at a time of economic crisis. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Serra-Majem, L.; Subirana, I.; Izquierdo-Pulido, M.; Fitó, M.; Elosua, R. Association of increased monetary cost of dietary intake, diet quality and weight management in Spanish adults. Br. J. Nutr. 2016, 115, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Mendez, C.; Garcia-Espejo, I. Social inequalities in following official guidelines on healthy diet during the period of economic crisis in Spain. Int. J. Health Serv. 2019, 49, 582–605. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Román-Viñas, B.; Sanchez-Villegas, A.; Guasch-Ferré, M.; Corella, D.; La Vecchia, C. Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol. Asp. Med. 2019, 67, 1–55. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Martínez-González, M.Á.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; Lorgeril, M.D. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef]
- Lorgeril, M.E.; Salen, P.; Martin, J.; Monjaud, I.; Delaye, J.; Mamelle, N. Mediterranean Diet, Traditional Risk Factors, and the Rate of Cardiovascular Complications After Myocardial Infarction Final Report of the Lyon Diet Heart Study. Circulation 1999, 99, 779–785. [Google Scholar] [CrossRef]
- Lorgeril, M.E. Mediterranean Diet and Cardiovascular Disease: Historical Perspective and Latest Evidence. Curr. Atheroscler. Rep. 2013, 15, 1–5. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Bamia, C.; Trichopoulos, D. Mediterranean diet and survival among patients with coronary heart disease in Greece. Arch. Intern Med. 2005, 165, 929–935. [Google Scholar] [CrossRef]
- Lai, J.S.; Hiles, S.; Bisquera, A.; Hure, A.J.; McEvoy, M.; Attia, J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am. J. Clin. Nutr. 2014, 99, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Parsaik, A.K.; Mielke, M.M.; Erwin, P.J.; Knopman, D.S.; Petersen, R.C.; Roberts, R.O. Association of Mediterranean diet with mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. J. Alzheimers Dis. 2014, 39, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Giugliano, D. Mediterranean diet and type 2 diabetes. Diabetes Metab. Res. Rev. 2014, 30 (Suppl. 1), 34–40. [Google Scholar] [CrossRef] [PubMed]
- Buckland, G.; Travier, N.; Cottet, V.; González, C.A.; Lujan-Barroso, L.; Agudo, A.; Trichopoulou, A.; Lagiou, P.; Trichopoulos, D.; Peeters, P.H.; et al. Adherence to the Mediterranean diet and risk of breast cancer in the European prospective investigation into cancer and nutrition cohort study. Int. J. Cancer 2013, 132, 2918–2927. [Google Scholar] [CrossRef] [PubMed]
- Lourida, I.; Soni, M.; Thompson-Coon, J.; Purandare, N.B.; Lang, I.A.; Ukoumunne, O.C.; Llewellyn, D.J. Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology 2013, 24, 479–489. [Google Scholar] [CrossRef]
- Psaltopoulou, T.; Sergentanis, T.N.; Panagiotakos, D.B.; Sergentanis, I.N.; Kosti, R.; Scarmeas, N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 2013, 74, 580–591. [Google Scholar] [CrossRef]
- Rossi, M.; Turati, F.; Lagiou, P.; Trichopoulos, D.; Augustin, L.S.; Vecchia, C.L.; Trichopoulou, A. Mediterranean diet and glycaemic load in relation to incidence of type 2 diabetes: Results from the Greek cohort of the population-based European Prospective Investigation into Cancer and Nutrition (EPIC). Diabetologia 2013, 56, 2405–2413. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ortiz-Andrellucchi, A. The Mediterranean diet as an example of food and nutrition sustainability: A multidisciplinary approach. Nutr. Hosp. 2018, 35, 96–101. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, I.; Corella, D.; Aros, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E.; Predimed investigators. Benefits of the Mediterranean diet: Insights from the PREDIMED study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Fresán, U.; Martínez-González, M.A.; Sabaté, J.; Bes-Rastrollo, M. Global sustainability (health, environment and monetary costs) of three dietary patterns: Results from a Spanish cohort (the SUN project). BMJ Open 2019, 9, e021541. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Alvarez, A.; Egan, B.; de Klein, S.; Dima, L.; Maggi, F.M.; Isoniemi, M.; Ribas-Barba, L.; Raats, M.M.; Meissner, E.M.; Badea, M.; et al. Usage of plant food supplements across six European countries: Findings from the PlantLIBRA consumer survey. PLoS ONE 2014, 9, e92265. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Aranceta, J. Réplica: La recomendación del consumo de alcohol en las ‘Guías alimentarias para la población española’. Un mensaje demasiado ambiguo. Nutr. Hosp. 2017, 34, 1006–1008. [Google Scholar] [PubMed]
- Ruiz, E.; Ávila, J.M.; Valero, T.; del Pozo, S.; Rodriguez, P.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; et al. Energy Intake, Profile, and Dietary Sources in the Spanish Population: Findings of the ANIBES Study. Nutrients 2015, 7, 4739–4762. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Agricultura, Pesca y Alimentación. Informe del Consumo Alimentario en España. Available online: https://www.mapa.gob.es/es/alimentacion/temas/consumo-y-comercializacion-y-distribucion-alimentaria/panel-de-consumo-alimentario/ultimos-datos/default.aspx (accessed on 1 October 2019).
- Instituto Nacional de Estadística (INE). Encuesta de Presupuestos Familiares. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176806&menu=ultiDatos&idp=1254735976608 (accessed on 1 October 2019).
- Canadian Society for Exercise Physiology. 2011 Canadian Physical Activity Guidelines; Canadian Society for Exercise Physiology: Ottawa, ON, Canada, 2011; Available online: http://www.csep.ca/cmfiles/guidelines/csep_guidelines_handbook.pdf (accessed on 1 October 2019).
- US Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report. 2008. Available online: https://health.gov/paguidelines/report/pdf/CommitteeReport.pdf (accessed on 1 October 2019).
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010; Available online: http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf (accessed on 1 October 2019).
- Warren, J.M.; Smith, N.; Ashwell, M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: Effectiveness and associated potential mechanisms. Nutr. Res. Rev. 2017, 30, 272–283. [Google Scholar] [CrossRef]
- Dalen, J.; Smith, B.W.; Shelley, B.M.; Sloan, A.L.; Leahigh, L.; Begay, D. Pilot study: Mindful Eating and Living (MEAL): Weight, eating behavior, and psychological outcomes associated with a mindfulness based intervention for people with obesity. Complement. Med. 2010, 18, 260–264. [Google Scholar] [CrossRef]
- Miller, C.K.; Kristeller, J.L.; Headings, A.; Nagaraja, H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Educ. Behav. 2014, 41, 145–154. [Google Scholar] [CrossRef]
- Fuentes Artiles, R.; Staub, K.; Aldakak, L.; Eppenberger, P.; Rühli, F.; Bender, N. Mindful eating and common diet programs lower body weight similarly: Systematic review and meta-analysis. Obes. Rev. 2019. [Google Scholar] [CrossRef]
- Weltens, N.; Zhao, D.; Oudenhove, L. Where is the comfort in comfort foods? Mechanisms linking fat signaling, reward, and emotion. Neurogastroenterol. Motil. 2014, 26, 303–315. [Google Scholar] [CrossRef]
- Berthoud, H.R. Metabolic and hedonic drives in the neural control of appetite: Who is the boss? Curr. Opin. Neurobiol. 2011, 21, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Donoso, C.; Sánchez-Villegas, A.; Martínez-González, M.A.; Gea, A.; Mendonça, R.D.; Lahortiga-Ramos, F.; Bes-Rastrollo, M. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: The SUN Project. Eur. J. Nutr. 2019. [Google Scholar] [CrossRef] [PubMed]
- Sarmugam, R.; Worsley, A. Dietary Behaviours, Impulsivity and Food Involvement: Identification of Three Consumer Segments. Nutrients 2015, 7, 8036–8057. [Google Scholar] [CrossRef] [PubMed]
- Welch, N.; McNaughton, S.A.; Hunter, W.; Hume, C.; Crawford, D. Is the perception of time pressure a barrier to healthy eating and physical activity among women? Public Health. Nutr. 2009, 12, 888–895. [Google Scholar] [CrossRef]
- Verplanken, B.; Sato, A. The psychology of impulse buying: An integrative self-regulation approach. J. Consum. Pol. 2011, 34, 197–210. [Google Scholar] [CrossRef]
- Kalla, S.M.; Arora, A.P. Impulse buying: A literature review. Glob. Bus. Rev. 2011, 12, 145–157. [Google Scholar] [CrossRef]
- Nederkoorn, C. Effects of sales promotions, weight status, and impulsivity on purchases in a supermarket. Obesity 2014, 22, E2–E5. [Google Scholar] [CrossRef]
- Manore, M.M.; Larson-Meyer, D.E.; Lindsay, A.R.; Hongu, N.; Houtkooper, L. Dynamic energy balance: An integrated framework for discussing diet and physical activity in obesity prevention-is it more than eating less and exercising more? Nutrients 2017, 9, 905. [Google Scholar] [CrossRef]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef]
- Tetens, I. European Food Safety Authority: EFSA: Panel on Dietetic Products, Nutrition, and Allergies (NDA); Scientific Opinion on Dietary reference values for water. EFSA J. 2010, 8, 1459. [Google Scholar] [CrossRef]
- Samaniego-Vaesken, M.L.; Ruiz, E.; Partearroyo, T.; Aranceta-Bartrina, J.; Gil, A.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. Added Sugars and Low- and No-Calorie Sweeteners in a Representative Sample of Food Products Consumed by the Spanish ANIBES Study Population. Nutrients 2018, 10, 1265. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Sánchez-Villegas, A.; Ortega, R.M.; Aranceta-Bartrina, J.; Gil, A.; González-Gross, M.; Varela-Moreiras, G.; Serra-Majem, L. Beverage Consumption Habits and Association with Total Water and Energy Intakes in the Spanish Population: Findings of the ANIBES Study. Nutrients 2016, 8, 232. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Watson, P.; Cordery, P.A.; Walsh, N.P.; Oliver, S.J.; Dolci, A.; Rodriguez-Sanchez, N.; Galloway, S.D. A randomized trial to assess the potential of different beverages to affect hydration status: Development of a beverage hydration index. Am. J. Clin. Nutr. 2016, 103, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Zong, G.; Gao, A.; Hu, F.B.; Sun, Q. Whole Grain Intake and Mortality from All Causes, Cardiovascular Disease, and Cancer: A Meta-Analysis of Prospective Cohort Studies. Circulation 2016, 133, 2370–2380. [Google Scholar] [CrossRef]
- Chen, G.C.; Tong, X.; Xu, J.Y.; Han, S.F.; Wan, Z.X.; Qin, J.B.; Qin, L.Q. Whole-grain intake and total, cardiovascular, and cancer mortality: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2016, 104, 164–172. [Google Scholar] [CrossRef]
- Pol, K.; Christensen, R.; Bartels, E.M.; Raben, A.; Tetens, I.; Kristensen, M. Whole grain and body weight changes in apparently healthy adults: A systematic review and meta-analysis of randomized controlled studies. Am. J. Clin. Nutr. 2013. [Google Scholar] [CrossRef]
- Fardet, A.; Boirie, Y. Associations between food and beverage groups and major diet-related chronic diseases: An exhaustive review of pooled/meta-analyses and systematic reviews. Nutr. Rev. 2014, 72, 741–762. [Google Scholar] [CrossRef]
- Wang, X.; Ouyang, Y.; Liu, J.; Zhu, M.; Zhao, G.; Bao, W.; Hu, B.F. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014, 349, g4490. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G.; Kalle-Uhlmann, T.; Arregui, M.; Buijsse, B.; Boeing, H. Fruit and vegetable consumption and changes in anthropometric variables in adult populations: A systematic review and meta-analysis of prospective cohort studies. PLoS ONE 2015, 10, e0140846. [Google Scholar] [CrossRef]
- FAO/WHO. Fats and Fatty Acids in Human Nutrition: Report of an Expert Consultation; FAO Food and Nutrition Paper No. 91; FAO: Rome, Italy, 2010. [Google Scholar]
- Ros, E.; Miranda, J.L.; Picó, C.; Rubio, M.A.; Babio, N.; Sala-Vila, A.; Pérez-Jiménez, F.; Escrich, E.; Bulló, M.; Solanas, M. Consenso sobre las grasas y aceites en la alimentación de la población española adulta; postura de la Federación Española de Sociedades de Alimentación, Nutrición y Dietética (FESNAD). Nutr. Hosp. 2015, 32, 435–477. [Google Scholar]
- Lawrence, G.D. Dietary fats and health: Dietary recommendations in the context of scientific evidence. Adv. Nutr. 2013, 4, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Astrup, A. A changing view on saturated fatty acids and dairy: From enemy to friend. Am. J. Clin. Nutr. 2014, 100, 1407–1408. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.Q.; Xu, J.Y.; Han, S.F.; Zhang, Z.L.; Zhao, Y.Y.; Szeto, I.M. Dairy consumption and risk of cardiovascular disease: An updated meta-analysis of prospective cohort studies. Asia Pac. J. Clin. Nutr. 2015, 24, 90–100. [Google Scholar] [PubMed]
- Food and Agriculture Organization of the United Nations and the World Health Organization. Joint FAO/WHO Expert Consultation on the Risks and Benefits of Fish Consumption; Food and Agriculture Organization of the United Nations and the World Health Organization: Rome, Italy, 2010; Available online: http://www.fao.org/docrep/014/ba0136e/ba0136e00.pdf (accessed on 1 October 2019).
- Food and Drug Administration, Environmental Protection Agency. What You Need to Know about Mercury in Fish and Shellfish; EPA-823-R-04-005; Food and Drug Administration, Environmental Protection Agency: Washington, DC, USA, 2004.
- AESAN. Recomendaciones de Consumo de Pescado (pez Espada, Tiburón, Atún Rojo y Lucio) Debido a la Presencia de Mercurio. Available online: http://www.aesan.msssi.gob.es/AECOSAN/web/para_el_consumidor/ampliacion/mercurio_pescado.shtml (accessed on 1 October 2019).
- García López, M.L.; Martín Esteban, M.; Rodríguez Artalejo, F.; Rodríguez Ferri, E. La alergia por anisakis y medidas de prevención. Opinión del Comité Científico de la AESA sobre una cuestión presentada por la Presidencia, en relación con los factores favorecedores de la aparición de alergia a Anisakis, así como de las medidas de prevención aplicable. Available online: http://www.aecosan.msssi.gob.es/AECOSAN/docs/documentos/seguridad_alimentaria/evaluacion_riesgos/informes_comite/ANISAKIS_ALERGIA.pdf (accessed on 1 October 2019).
- Afshin, A.; Micha, R.; Khatibzadeh, S.; Mozaffarian, D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2014, 100, 278–288. [Google Scholar] [CrossRef]
- Średnicka-Tober, D.; Barański, M.; Seal, C.J.; Sanderson, R.; Benbrook, C.; Steinshamn, H.; Gromadzka-Ostrowska, J.; Rembiałkowska, E.; Skwarło-Sońta, K.; Eyre, M.; et al. Higher PUFA and n-3 PUFA, conjugated linoleic acid, α-tocopherol and iron, but lower iodine and selenium concentrations in organic milk: A systematic literature review and meta- and redundancy analyses. Br. J. Nutr. 2016, 115, 1043–1060. [Google Scholar] [CrossRef]
- Farmery, A.K.; O’Kane, G.; McManus, A.; Green, B.S. Consuming sustainable seafood: Guidelines, recommendations and realities. Public Health Nutr. 2018, 1503–1514. [Google Scholar] [CrossRef] [PubMed]
- Batlle-Bayer, L.; Bala, A.; García-Herrero, I.; Lemaire, E.; Song, G.; Aldaco, R.; Fullana-i-Palmer, P. The Spanish Dietary Guidelines: A potential tool to reduce greenhouse gas emissions of current dietary patterns. J. Clean. Prod. 2019. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N. Red meat and processed meat consumption and all-cause mortality: A meta-analysis. Am. J. Epidemiol. 2014, 79, 282–289. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Kelly, S.A. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 9, 8–18. [Google Scholar] [CrossRef]
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary sugars and body weight: Systematic review and meta-analyses of randomized controlled trials and cohort studies. BMJ 2012, 346, e7492. [Google Scholar] [CrossRef]
- Biesalski, H.K.; Tinz, J. Multivitamin/mineral supplements: Rationale and safety—A systematic review. Nutrition 2017, 33, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Shenkin, A. Micronutrient supplements: Who needs them? A personal view. Nutr. Bull. 2013, 38, 191–200. [Google Scholar] [CrossRef]
- Costanzo, S.; Di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: A meta-analysis. Eur. J. Epidemiol. 2011, 26, 833–850. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, L.; Carson, J.A.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef] [PubMed]
- Gea, A.; Bes-Rastrollo, M.; Toledo, E.; Garcia-Lopez, M.; Beunza, J.J.; Estruch, R.; Martinez-Gonzalez, M.A. Mediterranean alcohol-drinking pattern and mortality in the SUN (Seguimiento Universidad de Navarra) Project: A prospective cohort study. Br. J. Nutr. 2014, 111, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Bazal, P.; Gea, A.; Martínez-González, M.A.; Salas-Salvadó, J.; Asensio, E.M.; Muñoz-Bravo, C.; Fiol, M.; Muñoz, M.A.; Lapetra, J.; Serra-Majem, L.L.; et al. Mediterranean alcohol-drinking pattern, low to moderate alcohol intake and risk of atrial fibrillation in the PREDIMED study. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 676–683. [Google Scholar] [CrossRef]
- WHO Expert Committee on Problems Related to Alcohol Consumption. Second report. WHO Tech. Rep. Ser. 2007, 944, 1–57. [Google Scholar]
- Garaulet, M.; Gómez-Abellán, P. Timing of food intake and obesity: A novel association. Physiol. Behav. 2014, 134, 44–50. [Google Scholar] [CrossRef]
- Burgess-Champoux, T.; Larson, N.; Neumark-Sztainer, D.; Hannan, P.J.; Story, M. Are family meal patterns associated with overall diet quality during the transition from early to middle adolescence? J. Nutr. Educ. Behav. 2009, 41, 79–86. [Google Scholar] [CrossRef]
- Monsivais, P.; Aggarwal, A.; Drewnowski, A. Time spent on home food preparation and indicators of healthy eating. Am. J. Prev. Med. 2014, 47, 796–802. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Aranceta-Bartrina, J.; Ortiz-Andrelluchi, A.; Ruano-Rodriguez, C.; Gonzalez-Padilla, E.; Dernini, S. Decalogue of Gran Canaria for sustainable food and nutrition in the community. In Sustainable Diets: Linking Nutrition and Food Systems; Burlingame, B., Dernini, S., Eds.; CABI: Boston, MA, USA, 2019; pp. 255–260. [Google Scholar]
- Corella, D.; Coltell, O.; Portolés, O.; Sotos-Prieto, M.; Fernández-Carrión, R.; Ramirez-Sabio, J.B.; Zanón-Moreno, V.; Mattei, J.; Sorlí, J.V.; Ordovas, J.M. A Guide to Applying the Sex-Gender Perspective to Nutritional Genomics. Nutrients 2018, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Zinöcker, M.K.; Lindseth, I.A. The western diet-microbiome-host interaction and its role in metabolic disease. Nutrients 2018, 10, 365. [Google Scholar] [CrossRef] [PubMed]
- Ordovas, J.M.; Ferguson, L.R.; Tai, E.S.; Mathers, J.C. Personalised nutrition and health. BMJ 2018, 361. [Google Scholar] [CrossRef] [PubMed]
- Storr, T.; Maher, J.; Swanepoel, E. Online nutrition information for pregnant women: A content analysis. Matern. Child. Nutr. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Wickham, C.A.; Carbone, E.T. What’s technology cooking up? A systematic review of the use of technology in adolescent food literacy programs. Appetite 2018, 125, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Boyer, C.; Gaudinat, A.; Hanbury, A.; Appel, R.D.; Ball, M.J.; Carpentier, M.; van Bemmel, J.H.; Bergmans, J.P.; Hochstrasser, D.; Lindberg, D.; et al. Accessing Reliable Health Information on the Web: A Review of the HON Approach. Stud. Health Technol. Inform. 2017, 245, 1004–1008. [Google Scholar]
- Mohn, E.S.; Kern, H.J.; Saltzman, E.; Mitmesser, S.H.; McKay, D.L. Evidence of Drug-Nutrient Interactions with Chronic Use of Commonly Prescribed Medications: An Update. Pharmaceutics 2018, 10, 36. [Google Scholar] [CrossRef]
- Engle-Stone, R.; Vosti, S.A.; Luo, H.; Kagin, J.; Tarini, A.; Adams, K.P.; French, C.; Brown, K.H. Weighing the risks of high intakes of selected micronutrients compared with the risks of deficiencies. Ann. N. Y. Acad. Sci. 2019, 1446, 81–101. [Google Scholar] [CrossRef]
- McHill, A.W.; Phillips, A.J.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.; Klerman, E.B. Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef]
- Aranceta Bartrina, J. Nutrición Comunitaria, 3rd ed.; Elsevier-Masson: Barcelona, Spain, 2013. [Google Scholar]
- Serra Majem, L.L.; Aranceta Bartrina, J. Guias alimentarias y Educacion Nutricional. In Tratado de Medicina Preventiva (PIEDROLA), 11th ed.; Elsevier-Masson: Barcelona, Spain, 2008; pp. 1056–1068. [Google Scholar]
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013.
- Mithril, C.; Dragsted, L.O.; Meyer, C.; Blauert, E.; Krog Holt, M.; Astrup, A. Guidelines for the New Nordic Diet. Public Health Nutr. 2012, 15, 1941–1947. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. Dietary Guidelines for Americans 2015–2020. Available online: health.gov/dietary guidelines/2015/guidelines/ (accessed on 10 July 2019).
- Ambrosini, G. Childhood dietary patterns and later obesity: A review of the evidence. Proc. Nutr. Soc. 2014, 73, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Perez-Rodrigo, C.; Gil, A.; Gonzalez-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G.; Aranceta-Bartrina, J. Clustering of Dietary Patterns, Lifestyles, and Overweight among Spanish Children and Adolescents in the ANIBES Study. Nutrients 2015, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: A review. Int. J. Behav. Nutr. Phys. Act 2014, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Henríquez-Sánchez, P.; Ruiz-Canela, M.; Lahortiga, F.; Molero, P.; Toledo, E.; Martínez-González, M.A. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project. BMC Med. 2015, 13, 197. [Google Scholar] [CrossRef]
- Martínez-Lapiscina, E.H.; Clavero, P.; Toledo, E.; Estruch, R.; Salas-Salvadó, J.; San Julián, B.; Sanchez-Tainta, A.; Ros, E.; Valls-Pedret, C.; Martinez-Gonzalez, M.Á. Mediterranean diet improves cognition: The PREDIMED-NAVARRA randomised trial. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1318–1325. [Google Scholar] [CrossRef]
- Kahleova, H.; Salas-Salvadó, J.; Rahelić, D.; Kendall, C.W.; Rembert, E.; Sievenpiper, J.L. Dietary Patterns and Cardiometabolic Outcomes in Diabetes: A Summary of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 2209. [Google Scholar] [CrossRef]
- Hansen, C.P.; Overvad, K.; Kyrø, C.; Olsen, A.; Tjønneland, A.; Johnsen, S.P.; Jakobsen, M.U.; Dahm, C.C. Adherence to a Healthy Nordic Diet and Risk of Stroke: A Danish Cohort Study. Stroke 2017, 48, 259–264. [Google Scholar] [CrossRef]
- UNESCO. Intangible cultural Heritage. Mediterranean diet Cyprus, Croatia, Spain, Greece, Italy, Morocco and Portugal Inscribed in 2013 (8.COM) on the Representative List of the Intangible Cultural Heritage of Humanity. Available online: https://ich.unesco.org/en/RL/mediterranean-diet-00884 (accessed on 1 October 2019).
- Medina, F.X. Food consumption and civil society: Mediterranean diet as a sustainable resource for the Mediterranean area. Public Health Nutr. 2011, 14, 2346–2349. [Google Scholar] [CrossRef]
- Pereira-da-Silva, L.; Rêgo, C.; Pietrobelli, A. The Diet of Preschool Children in the Mediterranean Countries of the European Union: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 572. [Google Scholar] [CrossRef]
- Tognon, G.; Moreno, L.A.; Mouratidou, T.; Veidebaum, T.; Molnár, D.; Russo, P.; Siani, A.; Akhandaf, Y.; Krogh, V.; Tornaritis, M.; et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int. J. Obes. 2014, 38 (Suppl. 2), S108–S114. [Google Scholar] [CrossRef]
- Partearroyo, T.; Laja García, A.I.; Varela-Moreiras, G. Strengths and weaknesses of food and diet in the Spanish population of the 21st century. Nutr. Hosp. 2019, 36, 3–6. [Google Scholar] [CrossRef] [PubMed]
- FAO. Food Based Dietary Guidelines. Available online: http://www.fao.org/nutrition/nutrition-education/food-dietary-guidelines/en/ (accessed on 5 July 2019).
- Leow, S.; Jackson, B.; Alderson, J.A.; Guelfi, K.J.; Dimmock, J.A. A Role for Exercise in Attenuating Unhealthy Food Consumption in Response to Stress. Nutrients 2018, 10, 176. [Google Scholar] [CrossRef] [PubMed]
- Leng, G.; Adan, R.A.H.; Belot, M.; Brunstrom, J.M.; de Graaf, K.; Dickson, S.L.; Hare, T.; Maier, S.; Menzies, J.; Preissl, H.; et al. The determinants of food choice. Nutr. Soc. 2017, 76, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Brazil. Secretariat of Health Care Primary Health Care Department. Dietary Guidelines for the Brazilian Population, 2nd ed.; Ministry of Health of Brazil, Secretariat of Health Care Primary Health Care Department: Brasilia-DF, Brazil, 2014.
- Thompson, S.; Gower, R.; Darmon, N.; Vieux, F.; Murphy-Bokern, D.; Maillot, M. A Balance of Healthy and Sustainable Food Choices for France, Spain and Sweden. LifeWell for Life. Healthy People, Healthy Planet. Available online: http://livewellforlife.eu/livewell-plate/livewell-in-spain (accessed on 20 August 2019).
- Gonzalez Fischer, C.; Garnett, T. Plates, Pyramids, Planet. Developments in National Healthy and Sustainable Dietary Guidelines: A State of Play Assessment. FAO-The University of Oxford. 2016. Available online: http://www.fao.org/3/a-i5640e.pdf (accessed on 21 July 2019).
- Tur Marí, M.A.; Serra Alías, M.; Ngo de la Cruz, J.; Vidal Ibáñez, M. Una Alimentación Sana para Todos (Reedición); AESAN: Madrid, Spain, 2008. [Google Scholar]
- Johnston, B.C.; Alonso-Coello, P.; Bala, M.M.; Zeraatkar, D.; Rabassa, M.; Valli, C.; Marshall, C.; El Dib, R.; Vernooij, R.W.M.; Vandvik, P.O.; et al. Methods for trustworthy nutritional recommendations NutriRECS (Nutritional Recommendations and accessible Evidence summaries Composed of Systematic reviews): A protocol. BMC Med. Res. Methodol. 2018, 18, 162. [Google Scholar] [CrossRef] [PubMed]
- Gaglani, J.; Oakeshott, P. Conducting a survey of patient reported advice on diet and exercise in primary care. Educ. Prim. Care 2018, 29, 178–179. [Google Scholar] [CrossRef] [PubMed]

| 1. Dietary recommendations: How to plan a healthy diet |
| 2. Designing a daily and weekly menu that is balanced, appealing, and healthy |
| 3. Guidance for intelligent, healthy, and sustainable food purchases |
| 4. How to read nutrition labels |
| 5. Cooking and food preparation processes: safe and healthy cooking techniques |
| 6. Preservation and reconstitution of foods at home |
| 7. 10 tips for safety in the kitchen |
| 8. How to better manage food waste (food Rs): reduce waste, reuse, recycle, repair, reject, and responsibility when buying |
| 9. Precision feeding: a new perspective |
| 10. Diet, pregnancy, and breast-feeding: preconception dietary advice |
| 11. Diet in childhood and youth |
| 12. Diet in the older adult and aging processes |
| 13. Nutrition education at home, in schools, in primary healthcare, and at work. |
| 14. Diet 3.0 |
| 15. Dietary advice in primary healthcare: drug—nutrient interactions |
| 16. Chronobiology of nutrition: principles and applications |
| 1. Select and consume locally sourced foods and products grown in your region and buy them in local markets nearby. |
| 2. Whenever possible, consume foods that are in season. They are healthier, cheaper, and sustainable. |
| 3. Value traditional local food and recipes; they are part of our culture and make up our identity. |
| 4. Learn to buy and cook in the company of others, it is more fun and enriching and we learn from each other. |
| 5. Plan your menu and shopping lists. Try to reduce food waste and recycle adequately at home and in the community. |
| 6. Prioritize plant-based foods. Limit the consumption of meat, processed meats, and dairy products. Your health and the planet will appreciate it. |
| 7. Terrestrial and aquatic biodiversity is critical. We should promote it to ensure its continuity. It is everyone’s responsibility. |
| 8. Take an interest in whether the agricultural, livestock, and fishing procedures which provide the foods you eat are SUSTAINABLE. |
| 9. Enjoy the company and the pleasure of food at mealtimes but always within the context of balance and moderation. Reduce portion sizes. |
| 10. Enjoy the Mediterranean diet. It is one of the best examples of a healthy and sustainable diet. UNESCO declared it as an Intangible Cultural Heritage of Humanity. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C.; The Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients 2019, 11, 2675. https://doi.org/10.3390/nu11112675
Aranceta-Bartrina J, Partearroyo T, López-Sobaler AM, Ortega RM, Varela-Moreiras G, Serra-Majem L, Pérez-Rodrigo C, The Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients. 2019; 11(11):2675. https://doi.org/10.3390/nu11112675
Chicago/Turabian StyleAranceta-Bartrina, Javier, Teresa Partearroyo, Ana M. López-Sobaler, Rosa M. Ortega, Gregorio Varela-Moreiras, Lluis Serra-Majem, Carmen Pérez-Rodrigo, and The Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). 2019. "Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal" Nutrients 11, no. 11: 2675. https://doi.org/10.3390/nu11112675
APA StyleAranceta-Bartrina, J., Partearroyo, T., López-Sobaler, A. M., Ortega, R. M., Varela-Moreiras, G., Serra-Majem, L., Pérez-Rodrigo, C., & The Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). (2019). Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients, 11(11), 2675. https://doi.org/10.3390/nu11112675









