Update on Early-Life T Cells: Impact on Oral Rotavirus Vaccines
Abstract
1. Introduction
2. Early-Life T Cells in Mice
2.1. Layered T-Cell Immunity in Early-Life Mice
2.2. Mouse Treg Cells in Early Life
2.3. Effector/Memory T Cells in Early Life
3. T Cells in Human Neonates and Infants
4. Conclusions and Future Directions: How May Early-Life T-Cell Immunity Impact RV Vaccines?
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, J.; Grow, S.; Iturriza-Gómara, M.; Hausdorff, W.P.; Fix, A.; Kirkwood, C.D. The Challenges and Opportunities of Next-Generation Rotavirus Vaccines: Summary of an Expert Meeting with Vaccine Developers. Viruses 2022, 14, 2565. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, B.D.; Chavers, T.; Parashar, U.; Tate, J.E. Global Estimates of Rotavirus Hospitalizations Among Children Below 5 Years in 2019 and Current and Projected Impacts of Rotavirus Vaccination. J. Pediatr. Infect. Dis. Soc. 2022, 11, 149–158. [Google Scholar] [CrossRef]
- Keita, A.M.; Doh, S.; Sow, S.O.; Powell, H.; Omore, R.; Jahangir Hossain, M.; Ogwel, B.; Ochieng, J.B.; Jones, J.C.M.; Zaman, S.M.A.; et al. Prevalence, Clinical Severity, and Seasonality of Adenovirus 40/41, Astrovirus, Sapovirus, and Rotavirus Among Young Children With Moderate-to-Severe Diarrhea: Results From the Vaccine Impact on Diarrhea in Africa (VIDA) Study. Clin. Infect. Dis. 2023, 76, S123–S131. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Iqbal, J.; Sadiq, K.; Umrani, F.; Rizvi, A.; Kabir, F.; Jamil, Z.; Syed, S.; Ehsan, L.; Zulqarnain, F.; et al. Association of Anti-Rotavirus IgA Seroconversion with Growth, Environmental Enteric Dysfunction and Enteropathogens in Rural Pakistani Infants. Vaccine 2022, 40, 3444–3451. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.H.; Armah, G.; Dennis, F.; Wang, L.; Rodgers, R.; Droit, L.; Baldridge, M.T.; Handley, S.A.; Harris, V.C. Enteric Virome Negatively Affects Seroconversion Following Oral Rotavirus Vaccination in a Longitudinally Sampled Cohort of Ghanaian Infants. Cell Host Microbe 2022, 30, 110–123.e5. [Google Scholar] [CrossRef] [PubMed]
- Parker, E.P.K.; Bronowski, C.; Sindhu, K.N.C.; Babji, S.; Benny, B.; Carmona-Vicente, N.; Chasweka, N.; Chinyama, E.; Cunliffe, N.A.; Dube, Q.; et al. Impact of Maternal Antibodies and Microbiota Development on the Immunogenicity of Oral Rotavirus Vaccine in African, Indian, and European Infants. Nat. Commun. 2021, 12, 7288. [Google Scholar] [CrossRef]
- Robertson, R.C.; Church, J.A.; Edens, T.J.; Mutasa, K.; Min Geum, H.; Baharmand, I.; Gill, S.K.; Ntozini, R.; Chasekwa, B.; Carr, L.; et al. The Fecal Microbiome and Rotavirus Vaccine Immunogenicity in Rural Zimbabwean Infants. Vaccine 2021, 39, 5391–5400. [Google Scholar] [CrossRef]
- Lauer, J.M.; Kirby, M.A.; Muhihi, A.; Ulenga, N.; Aboud, S.; Liu, E.; Choy, R.K.M.; Arndt, M.B.; Kou, J.; Fawzi, W.; et al. Assessing Environmental Enteric Dysfunction via Multiplex Assay and Its Relation to Growth and Development among HIV-Exposed Uninfected Tanzanian Infants. PLoS Negl. Trop. Dis. 2023, 17, e0011181. [Google Scholar] [CrossRef]
- Crawford, S.E.; Ramani, S.; Tate, J.E.; Parashar, U.D.; Svensson, L.; Hagbom, M.; Franco, M.A.; Greenberg, H.B.; O’Ryan, M.; Kang, G.; et al. Rotavirus Infection. Nat. Rev. Dis. Primers 2017, 3, 17083. [Google Scholar] [CrossRef]
- VanCott, J.L.; Prada, A.E.; McNeal, M.M.; Stone, S.C.; Basu, M.; Huffer, B., Jr.; Smiley, K.L.; Shao, M.; Bean, J.A.; Clements, J.D.; et al. Mice Develop Effective but Delayed Protective Immune Responses When Immunized as Neonates Either Intranasally with Nonliving VP6/LT(R192G) or Orally with Live Rhesus Rotavirus Vaccine Candidates. J. Virol. 2006, 80, 4949–4961. [Google Scholar] [CrossRef]
- Rey, L.M.; Gil, J.Á.; Mateus, J.; Rodríguez, L.-S.; Rondón, M.A.; Ángel, J.; Franco, M.A. LAP+ Cells Modulate Protection Induced by Oral Vaccination with Rhesus Rotavirus in a Neonatal Mouse Model. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Tabilas, C.; Smith, N.L.; Rudd, B.D. Shaping Immunity for Life: Layered Development of CD8+ T Cells. Immunol. Rev. 2023, 315, 108–125. [Google Scholar] [CrossRef]
- Torow, N.; Hand, T.W.; Hornef, M.W. Programmed and Environmental Determinants Driving Neonatal Mucosal Immune Development. Immunity 2023, 56, 485–499. [Google Scholar] [CrossRef] [PubMed]
- Laban, N.M.; Goodier, M.R.; Bosomprah, S.; Simuyandi, M.; Chisenga, C.; Chilyabanyama, O.N.; Chilengi, R. T-Cell Responses after Rotavirus Infection or Vaccination in Children: A Systematic Review. Viruses 2022, 14, 459. [Google Scholar] [CrossRef]
- Lockhart, A.; Mucida, D.; Parsa, R. Immunity to Enteric Viruses. Immunity 2022, 55, 800–818. [Google Scholar] [CrossRef] [PubMed]
- Rudd, B.D. Neonatal T Cells: A Reinterpretation. Annu. Rev. Immunol. 2020, 38, 229–247. [Google Scholar] [CrossRef]
- Davenport, M.P.; Smith, N.L.; Rudd, B.D. Building a T Cell Compartment: How Immune Cell Development Shapes Function. Nat. Rev. Immunol. 2020, 20, 499–506. [Google Scholar] [CrossRef]
- Ramanan, D.; Pratama, A.; Zhu, Y.; Venezia, O.; Sassone-Corsi, M.; Chowdhary, K.; Galván-Peña, S.; Sefik, E.; Brown, C.; Gélineau, A.; et al. Regulatory T Cells in the Face of the Intestinal Microbiota. Nat. Rev. Immunol. 2023, 23, 749–762. [Google Scholar] [CrossRef]
- Herzenberg, L.A.; Herzenberg, L.A. Toward a Layered Immune System. Cell 1989, 59, 953–954. [Google Scholar] [CrossRef]
- Knoop, K.A.; Gustafsson, J.K.; McDonald, K.G.; Kulkarni, D.H.; Coughlin, P.E.; McCrate, S.; Kim, D.; Hsieh, C.-S.; Hogan, S.P.; Elson, C.O.; et al. Microbial Antigen Encounter during a Preweaning Interval Is Critical for Tolerance to Gut Bacteria. Sci. Immunol. 2017, 2, eaao1314. [Google Scholar] [CrossRef]
- Lynn, D.J.; Benson, S.C.; Lynn, M.A.; Pulendran, B. Modulation of Immune Responses to Vaccination by the Microbiota: Implications and Potential Mechanisms. Nat. Rev. Immunol. 2022, 22, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.L.; Wissink, E.; Wang, J.; Pinello, J.F.; Davenport, M.P.; Grimson, A.; Rudd, B.D. Rapid Proliferation and Differentiation Impairs the Development of Memory CD8+ T Cells in Early Life. J. Immunol. 2014, 193, 177–184. [Google Scholar] [CrossRef]
- Torow, N.; Yu, K.; Hassani, K.; Freitag, J.; Schulz, O.; Basic, M.; Brennecke, A.; Sparwasser, T.; Wagner, N.; Bleich, A.; et al. Active Suppression of Intestinal CD4(+)TCRαβ(+) T-Lymphocyte Maturation during the Postnatal Period. Nat. Commun. 2015, 6, 7725. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.L.; Patel, R.K.; Reynaldi, A.; Grenier, J.K.; Wang, J.; Watson, N.B.; Nzingha, K.; Yee Mon, K.J.; Peng, S.A.; Grimson, A.; et al. Developmental Origin Governs CD8+ T Cell Fate Decisions during Infection. Cell 2018, 174, 117–130.e14. [Google Scholar] [CrossRef]
- Baumgarth, N. The Shaping of a B Cell Pool Maximally Responsive to Infections. Annu. Rev. Immunol. 2021, 39, 103–129. [Google Scholar] [CrossRef]
- Hu, Y.; Hu, Q.; Li, Y.; Lu, L.; Xiang, Z.; Yin, Z.; Kabelitz, D.; Wu, Y. Γδ T Cells: Origin and Fate, Subsets, Diseases and Immunotherapy. Signal Transduct. Target Ther. 2023, 8, 434. [Google Scholar] [PubMed]
- Yang, S.; Fujikado, N.; Kolodin, D.; Benoist, C.; Mathis, D. Immune Tolerance. Regulatory T Cells Generated Early in Life Play a Distinct Role in Maintaining Self-Tolerance. Science 2015, 348, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.B.; Patel, R.K.; Kean, C.; Veazey, J.; Oyesola, O.O.; Laniewski, N.; Grenier, J.K.; Wang, J.; Tabilas, C.; Yee Mon, K.J.; et al. The Gene Regulatory Basis of Bystander Activation in CD8+ T Cells. Sci. Immunol. 2024, 9, eadf8776. [Google Scholar] [CrossRef]
- Yuan, J.; Nguyen, C.K.; Liu, X.; Kanellopoulou, C.; Muljo, S.A. Lin28b Reprograms Adult Bone Marrow Hematopoietic Progenitors to Mediate Fetal-like Lymphopoiesis. Science 2012, 335, 1195–1200. [Google Scholar] [CrossRef]
- Wang, J.; Wissink, E.M.; Watson, N.B.; Smith, N.L.; Grimson, A.; Rudd, B.D. Fetal and Adult Progenitors Give Rise to Unique Populations of CD8+ T Cells. Blood 2016, 128, 3073–3082. [Google Scholar] [CrossRef]
- Bronevetsky, Y.; Burt, T.D.; McCune, J.M. Lin28b Regulates Fetal Regulatory T Cell Differentiation through Modulation of TGF-β Signaling. J. Immunol. 2016, 197, 4344–4350. [Google Scholar] [CrossRef]
- Fernandez, M.A.; Puttur, F.K.; Wang, Y.M.; Howden, W.; Alexander, S.I.; Jones, C.A. T Regulatory Cells Contribute to the Attenuated Primary CD8+ and CD4+ T Cell Responses to Herpes Simplex Virus Type 2 in Neonatal Mice. J. Immunol. 2008, 180, 1556–1564. [Google Scholar] [CrossRef]
- Knoop, K.A.; McDonald, K.G.; Coughlin, P.E.; Kulkarni, D.H.; Gustafsson, J.K.; Rusconi, B.; John, V.; Ndao, I.M.; Beigelman, A.; Good, M.; et al. Synchronization of Mothers and Offspring Promotes Tolerance and Limits Allergy. JCI Insight 2020, 5, 137943. [Google Scholar] [CrossRef] [PubMed]
- Torow, N.; Li, R.; Hitch, T.C.A.; Mingels, C.; Al Bounny, S.; van Best, N.; Stange, E.-L.; Simons, B.; Maié, T.; Rüttger, L.; et al. M Cell Maturation and CDC Activation Determine the Onset of Adaptive Immune Priming in the Neonatal Peyer’s Patch. Immunity 2023, 56, 1220–1238.e7. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, D.; Sefik, E.; Galván-Peña, S.; Wu, M.; Yang, L.; Yang, Z.; Kostic, A.; Golovkina, T.V.; Kasper, D.L.; Mathis, D.; et al. An Immunologic Mode of Multigenerational Transmission Governs a Gut Treg Setpoint. Cell 2020, 181, 1276–1290.e13. [Google Scholar] [CrossRef]
- Akagbosu, B.; Tayyebi, Z.; Shibu, G.; Paucar Iza, Y.A.; Deep, D.; Parisotto, Y.F.; Fisher, L.; Pasolli, H.A.; Thevin, V.; Elmentaite, R.; et al. Novel Antigen-Presenting Cell Imparts Treg-Dependent Tolerance to Gut Microbiota. Nature 2022, 610, 752–760. [Google Scholar] [CrossRef]
- Uchiyama, R.; Chassaing, B.; Zhang, B.; Gewirtz, A.T. Antibiotic Treatment Suppresses Rotavirus Infection and Enhances Specific Humoral Immunity. J. Infect. Dis. 2014, 210, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Lynn, M.A.; Tumes, D.J.; Choo, J.M.; Sribnaia, A.; Blake, S.J.; Leong, L.E.X.; Young, G.P.; Marshall, H.S.; Wesselingh, S.L.; Rogers, G.B.; et al. Early-Life Antibiotic-Driven Dysbiosis Leads to Dysregulated Vaccine Immune Responses in Mice. Cell Host Microbe 2018, 23, 653–660.e5. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, A.; Burr, A.H.P.; Overacre-Delgoffe, A.E.; Tometich, J.T.; Yang, D.; Huckestein, B.R.; Linehan, J.L.; Spencer, S.P.; Hall, J.A.; Harrison, O.J.; et al. Environmental Enteric Dysfunction Induces Regulatory T Cells That Inhibit Local CD4+ T Cell Responses and Impair Oral Vaccine Efficacy. Immunity 2021, 54, 1745–1757.e7. [Google Scholar] [CrossRef]
- Zens, K.D.; Chen, J.K.; Guyer, R.S.; Wu, F.L.; Cvetkovski, F.; Miron, M.; Farber, D.L. Reduced Generation of Lung Tissue-Resident Memory T Cells during Infancy. J. Exp. Med. 2017, 214, 2915–2932. [Google Scholar] [CrossRef]
- Thapa, P.; Guyer, R.S.; Yang, A.Y.; Parks, C.A.; Brusko, T.M.; Brusko, M.; Connors, T.J.; Farber, D.L. Infant T Cells Are Developmentally Adapted for Robust Lung Immune Responses through Enhanced T Cell Receptor Signaling. Sci. Immunol. 2021, 6, eabj0789. [Google Scholar] [CrossRef] [PubMed]
- Reina-Campos, M.; Scharping, N.E.; Goldrath, A.W. CD8+ T Cell Metabolism in Infection and Cancer. Nat. Rev. Immunol. 2021, 21, 718–738. [Google Scholar] [CrossRef] [PubMed]
- Tabilas, C.; Wang, J.; Liu, X.; Locasale, J.W.; Smith, N.L.; Rudd, B.D. Cutting Edge: Elevated Glycolytic Metabolism Limits the Formation of Memory CD8+ T Cells in Early Life. J. Immunol. 2019, 203, 2571–2576. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.R.; Jenkins, B.J.; Cronin, J.G.; Jones, N.; Thornton, C.A. A Role for Metabolism in Determining Neonatal Immune Function. Pediatr. Allergy Immunol. 2021, 32, 1616–1628. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.; El Guindy, A.; Panwala, C.M.; Hagan, P.M.; Camerini, V. Differential Appearance of T Cell Subsets in the Large and Small Intestine of Neonatal Mice. Pediatr. Res. 2001, 49, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Steege, J.C.; Buurman, W.A.; Forget, P.P. The Neonatal Development of Intraepithelial and Lamina Propria Lymphocytes in the Murine Small Intestine. Dev. Immunol. 1997, 5, 121–128. [Google Scholar] [CrossRef]
- Masopust, D.; Soerens, A.G. Tissue-Resident T Cells and Other Resident Leukocytes. Annu. Rev. Immunol. 2019, 37, 521–546. [Google Scholar] [CrossRef] [PubMed]
- Paik, D.H.; Farber, D.L. Anti-Viral Protective Capacity of Tissue Resident Memory T Cells. Curr. Opin. Virol. 2021, 46, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Parsa, R.; London, M.; Rezende de Castro, T.B.; Reis, B.; Buissant des Amorie, J.; Smith, J.G.; Mucida, D. Newly Recruited Intraepithelial Ly6A+CCR9+CD4+ T Cells Protect against Enteric Viral Infection. Immunity 2022, 55, 1234–1249.e6. [Google Scholar] [CrossRef]
- von Hoesslin, M.; Kuhlmann, M.; de Almeida, G.P.; Kanev, K.; Wurmser, C.; Gerullis, A.-K.; Roelli, P.; Berner, J.; Zehn, D. Secondary Infections Rejuvenate the Intestinal CD103 + Tissue-Resident Memory T Cell Pool. Sci. Immunol. 2022, 7, eabp9553. [Google Scholar] [CrossRef]
- Fung, H.Y.; Teryek, M.; Lemenze, A.D.; Bergsbaken, T. CD103 Fate Mapping Reveals That Intestinal CD103- Tissue-Resident Memory T Cells Are the Primary Responders to Secondary Infection. Sci. Immunol. 2022, 7, eabl9925. [Google Scholar] [CrossRef] [PubMed]
- Tomov, V.T.; Palko, O.; Lau, C.W.; Pattekar, A.; Sun, Y.; Tacheva, R.; Bengsch, B.; Manne, S.; Cosma, G.L.; Eisenlohr, L.C.; et al. Differentiation and Protective Capacity of Virus-Specific CD8+ T Cells Suggest Murine Norovirus Persistence in an Immune-Privileged Enteric Niche. Immunity 2017, 47, 723–738.e5. [Google Scholar] [CrossRef] [PubMed]
- Jaimes, M.C.; Feng, N.; Greenberg, H.B. Characterization of Homologous and Heterologous Rotavirus-Specific T-Cell Responses in Infant and Adult Mice. J. Virol. 2005, 79, 4568–4579. [Google Scholar] [CrossRef] [PubMed]
- Malloy, A.M.W.; Lu, Z.; Kehl, M.; Pena DaMata, J.; Lau-Kilby, A.W.; Turfkruyer, M. Increased Innate Immune Activation Induces Protective RSV-Specific Lung-Resident Memory T Cells in Neonatal Mice. Mucosal Immunol. 2023, 16, 593–605. [Google Scholar] [CrossRef] [PubMed]
- Mold, J.E.; Michaëlsson, J.; Burt, T.D.; Muench, M.O.; Beckerman, K.P.; Busch, M.P.; Lee, T.-H.; Nixon, D.F.; McCune, J.M. Maternal Alloantigens Promote the Development of Tolerogenic Fetal Regulatory T Cells in Utero. Science 2008, 322, 1562–1565. [Google Scholar] [CrossRef] [PubMed]
- Mold, J.E.; Venkatasubrahmanyam, S.; Burt, T.D.; Michaëlsson, J.; Rivera, J.M.; Galkina, S.A.; Weinberg, K.; Stoddart, C.A.; McCune, J.M. Fetal and Adult Hematopoietic Stem Cells Give Rise to Distinct T Cell Lineages in Humans. Science 2010, 330, 1695–1699. [Google Scholar] [CrossRef]
- Li, N.; van Unen, V.; Abdelaal, T.; Guo, N.; Kasatskaya, S.A.; Ladell, K.; McLaren, J.E.; Egorov, E.S.; Izraelson, M.; Chuva de Sousa Lopes, S.M.; et al. Memory CD4+ T Cells Are Generated in the Human Fetal Intestine. Nat. Immunol. 2019, 20, 301–312. [Google Scholar] [CrossRef]
- Hiwarkar, P.; Hubank, M.; Qasim, W.; Chiesa, R.; Gilmour, K.C.; Saudemont, A.; Amrolia, P.J.; Veys, P. Cord Blood Transplantation Recapitulates Fetal Ontogeny with a Distinct Molecular Signature That Supports CD4+ T-Cell Reconstitution. Blood Adv. 2017, 1, 2206–2216. [Google Scholar] [CrossRef]
- Bunis, D.G.; Bronevetsky, Y.; Krow-Lucal, E.; Bhakta, N.R.; Kim, C.C.; Nerella, S.; Jones, N.; Mendoza, V.F.; Bryson, Y.J.; Gern, J.E.; et al. Single-Cell Mapping of Progressive Fetal-to-Adult Transition in Human Naive T Cells. Cell Rep. 2021, 34, 108573. [Google Scholar] [CrossRef]
- Michaëlsson, J.; Mold, J.E.; McCune, J.M.; Nixon, D.F. Regulation of T Cell Responses in the Developing Human Fetus. J. Immunol. 2006, 176, 5741–5748. [Google Scholar] [CrossRef]
- Thome, J.J.; Bickham, K.L.; Ohmura, Y.; Kubota, M.; Matsuoka, N.; Gordon, C.; Granot, T.; Griesemer, A.; Lerner, H.; Kato, T.; et al. Early-Life Compartmentalization of Human T Cell Differentiation and Regulatory Function in Mucosal and Lymphoid Tissues. Nat. Med. 2016, 22, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Mandl, J.N.; Monteiro, J.P.; Vrisekoop, N.; Germain, R.N. T Cell-Positive Selection Uses Self-Ligand Binding Strength to Optimize Repertoire Recognition of Foreign Antigens. Immunity 2013, 38, 263–274. [Google Scholar] [CrossRef]
- St John, L.S.; Wan, L.; He, H.; Garber, H.R.; Clise-Dwyer, K.; Alatrash, G.; Rezvani, K.; Shpall, E.J.; Bollard, C.M.; Ma, Q.; et al. PR1-Specific Cytotoxic T Lymphocytes Are Relatively Frequent in Umbilical Cord Blood and Can Be Effectively Expanded to Target Myeloid Leukemia. Cytotherapy 2016, 18, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- McCarron, M.; Reen, D.J. Activated Human Neonatal CD8+ T Cells Are Subject to Immunomodulation by Direct TLR2 or TLR5 Stimulation. J. Immunol. 2009, 182, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Pekalski, M.L.; García, A.R.; Ferreira, R.C.; Rainbow, D.B.; Smyth, D.J.; Mashar, M.; Brady, J.; Savinykh, N.; Dopico, X.C.; Mahmood, S.; et al. Neonatal and Adult Recent Thymic Emigrants Produce IL-8 and Express Complement Receptors CR1 and CR2. JCI Insight 2017, 2, 93739. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Albarrán, A.O.; López-Portales, O.H.; Gutiérrez-Reyna, D.Y.; Rodríguez-Jorge, O.; Sánchez-Villanueva, J.A.; Ramírez-Pliego, O.; Bergon, A.; Loriod, B.; Holota, H.; Imbert, J.; et al. CD8+ T Cells from Human Neonates Are Biased toward an Innate Immune Response. Cell Rep. 2016, 17, 2151–2160. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, D.; Fleming, P.; Virasami, A.; Michel, M.L.; Sebire, N.J.; Costeloe, K.; Carr, R.; Klein, N.; Hayday, A. Interleukin-8 (CXCL8) Production Is a Signatory T Cell Effector Function of Human Newborn Infants. Nat. Med. 2014, 20, 1206–1210. [Google Scholar] [CrossRef] [PubMed]
- Schönland, S.O.; Zimmer, J.K.; Lopez-Benitez, C.M.; Widmann, T.; Ramin, K.D.; Goronzy, J.J.; Weyand, C.M. Homeostatic Control of T-Cell Generation in Neonates. Blood 2003, 102, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Rouault-Pierre, K.; Kamdar, S.; Gomez-Tourino, I.; Wood, K.; Donaldson, I.; Mein, C.A.; Bonnet, D.; Hayday, A.C.; Gibbons, D.L. Adaptive from Innate: Human IFN-Γ+CD4+ T Cells Can Arise Directly from CXCL8-Producing Recent Thymic Emigrants in Babies and Adults. J. Immunol. 2017, 199, 1696–1705. [Google Scholar] [CrossRef]
- Montecino-Rodriguez, E.; Casero, D.; Fice, M.; Le, J.; Dorshkind, K. Differential Expression of PU.1 and Key T Lineage Transcription Factors Distinguishes Fetal and Adult T Cell Development. J. Immunol. 2018, 200, 2046–2056. [Google Scholar] [CrossRef]
- He, X.-S.; Holmes, T.H.; Mahmood, K.; Kemble, G.W.; Dekker, C.L.; Arvin, A.M.; Greenberg, H.B. Phenotypic Changes in Influenza-Specific CD8+ T Cells after Immunization of Children and Adults with Influenza Vaccines. J. Infect. Dis. 2008, 197, 803–811. [Google Scholar] [CrossRef]
- Thomson, Z.; He, Z.; Swanson, E.; Henderson, K.; Phalen, C.; Zaim, S.R.; Pebworth, M.-P.; Okada, L.Y.; Heubeck, A.T.; Roll, C.R.; et al. Trimodal Single-Cell Profiling Reveals a Novel Pediatric CD8αα+ T Cell Subset and Broad Age-Related Molecular Reprogramming across the T Cell Compartment. Nat. Immunol. 2023, 24, 1947–1959. [Google Scholar] [CrossRef]
- Connors, T.J.; Baird, J.S.; Yopes, M.C.; Zens, K.D.; Pethe, K.; Ravindranath, T.M.; Ho, S.-H.; Farber, D.L. Developmental Regulation of Effector and Resident Memory T Cell Generation during Pediatric Viral Respiratory Tract Infection. J. Immunol. 2018, 201, 432–439. [Google Scholar] [CrossRef]
- Senda, T.; Dogra, P.; Granot, T.; Furuhashi, K.; Snyder, M.E.; Carpenter, D.J.; Szabo, P.A.; Thapa, P.; Miron, M.; Farber, D.L. Microanatomical Dissection of Human Intestinal T-Cell Immunity Reveals Site-Specific Changes in Gut-Associated Lymphoid Tissues over Life. Mucosal Immunol. 2019, 12, 378–389. [Google Scholar] [CrossRef]
- Connors, T.J.; Matsumoto, R.; Verma, S.; Szabo, P.A.; Guyer, R.; Gray, J.; Wang, Z.; Thapa, P.; Dogra, P.; Poon, M.M.L.; et al. Site-Specific Development and Progressive Maturation of Human Tissue-Resident Memory T Cells over Infancy and Childhood. Immunity 2023, 56, 1894–1909.e5. [Google Scholar] [CrossRef]
- Poon, M.M.L.; Caron, D.P.; Wang, Z.; Wells, S.B.; Chen, D.; Meng, W.; Szabo, P.A.; Lam, N.; Kubota, M.; Matsumoto, R.; et al. Tissue Adaptation and Clonal Segregation of Human Memory T Cells in Barrier Sites. Nat. Immunol. 2023, 24, 309–319. [Google Scholar] [CrossRef]
- Connors, T.J.; Ravindranath, T.M.; Bickham, K.L.; Gordon, C.L.; Zhang, F.; Levin, B.; Baird, J.S.; Farber, D.L. Airway CD8+ T Cells Are Associated with Lung Injury during Infant Viral Respiratory Tract Infection. Am. J. Respir. Cell Mol. Biol. 2016, 54, 822–830. [Google Scholar] [CrossRef]
- Matsumoto, R.; Gray, J.; Rybkina, K.; Oppenheimer, H.; Levy, L.; Friedman, L.M.; Khamaisi, M.; Meng, W.; Rosenfeld, A.M.; Guyer, R.S.; et al. Induction of Bronchus-Associated Lymphoid Tissue Is an Early Life Adaptation for Promoting Human B Cell Immunity. Nat. Immunol. 2023, 24, 1370–1381. [Google Scholar] [CrossRef]
- Renz, H.; Adkins, B.D.; Bartfeld, S.; Blumberg, R.S.; Farber, D.L.; Garssen, J.; Ghazal, P.; Hackam, D.J.; Marsland, B.J.; McCoy, K.D.; et al. The Neonatal Window of Opportunity-Early Priming for Life. J. Allergy Clin. Immunol. 2018, 141, 1212–1214. [Google Scholar] [CrossRef]
- Tabilas, C.; Iu, D.S.; Daly, C.W.P.; Mon, K.J.Y.; Reynaldi, A.; Wesnak, S.P.; Grenier, J.K.; Davenport, M.P.; Smith, N.L.; Grimson, A.; et al. Early Microbial Exposure Shapes Adult Immunity by Altering CD8+ T Cell Development. Proc. Natl. Acad. Sci. USA 2022, 119, e2212548119. [Google Scholar] [CrossRef]
- Parra, M.; Herrera, D.; Jácome, M.F.; Mesa, M.C.; Rodríguez, L.-S.; Guzmán, C.; Angel, J.; Franco, M.A. Circulating Rotavirus-Specific T Cells Have a Poor Functional Profile. Virology 2014, 468–470, 340–350. [Google Scholar] [CrossRef]
- Jaimes, M.C.; Rojas, O.L.; González, A.M.; Cajiao, I.; Charpilienne, A.; Pothier, P.; Kohli, E.; Greenberg, H.B.; Franco, M.A.; Angel, J. Frequencies of Virus-Specific CD4(+) and CD8(+) T Lymphocytes Secreting Gamma Interferon after Acute Natural Rotavirus Infection in Children and Adults. J. Virol. 2002, 76, 4741–4749. [Google Scholar] [CrossRef]
- Angel, J.; Steele, A.D.; Franco, M.A. Correlates of Protection for Rotavirus Vaccines: Possible Alternative Trial Endpoints, Opportunities, and Challenges. Hum. Vaccin. Immunother. 2014, 10, 3659–3671. [Google Scholar] [CrossRef]
- Lavelle, E.C.; Ward, R.W. Mucosal Vaccines—Fortifying the Frontiers. Nat. Rev. Immunol. 2022, 22, 236–250. [Google Scholar] [CrossRef]
- Araki, K.; Turner, A.P.; Shaffer, V.O.; Gangappa, S.; Keller, S.A.; Bachmann, M.F.; Larsen, C.P.; Ahmed, R. MTOR Regulates Memory CD8 T-Cell Differentiation. Nature 2009, 460, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Mannick, J.B.; Del Giudice, G.; Lattanzi, M.; Valiante, N.M.; Praestgaard, J.; Huang, B.; Lonetto, M.A.; Maecker, H.T.; Kovarik, J.; Carson, S.; et al. MTOR Inhibition Improves Immune Function in the Elderly. Sci. Transl. Med. 2014, 6, 268ra179. [Google Scholar] [CrossRef] [PubMed]
- DuPont, H.L.; Jiang, Z.-D.; Alexander, A.S.; DuPont, A.W.; Brown, E.L. Intestinal IgA-Coated Bacteria in Healthy- and Altered-Microbiomes (Dysbiosis) and Predictive Value in Successful Fecal Microbiota Transplantation. Microorganisms 2022, 11, 93. [Google Scholar] [CrossRef]
- Hsu, P.S.; Nanan, R. Does Breast Milk Nurture T Lymphocytes in Their Cradle? Front. Pediatr. 2018, 6, 268. [Google Scholar] [CrossRef]
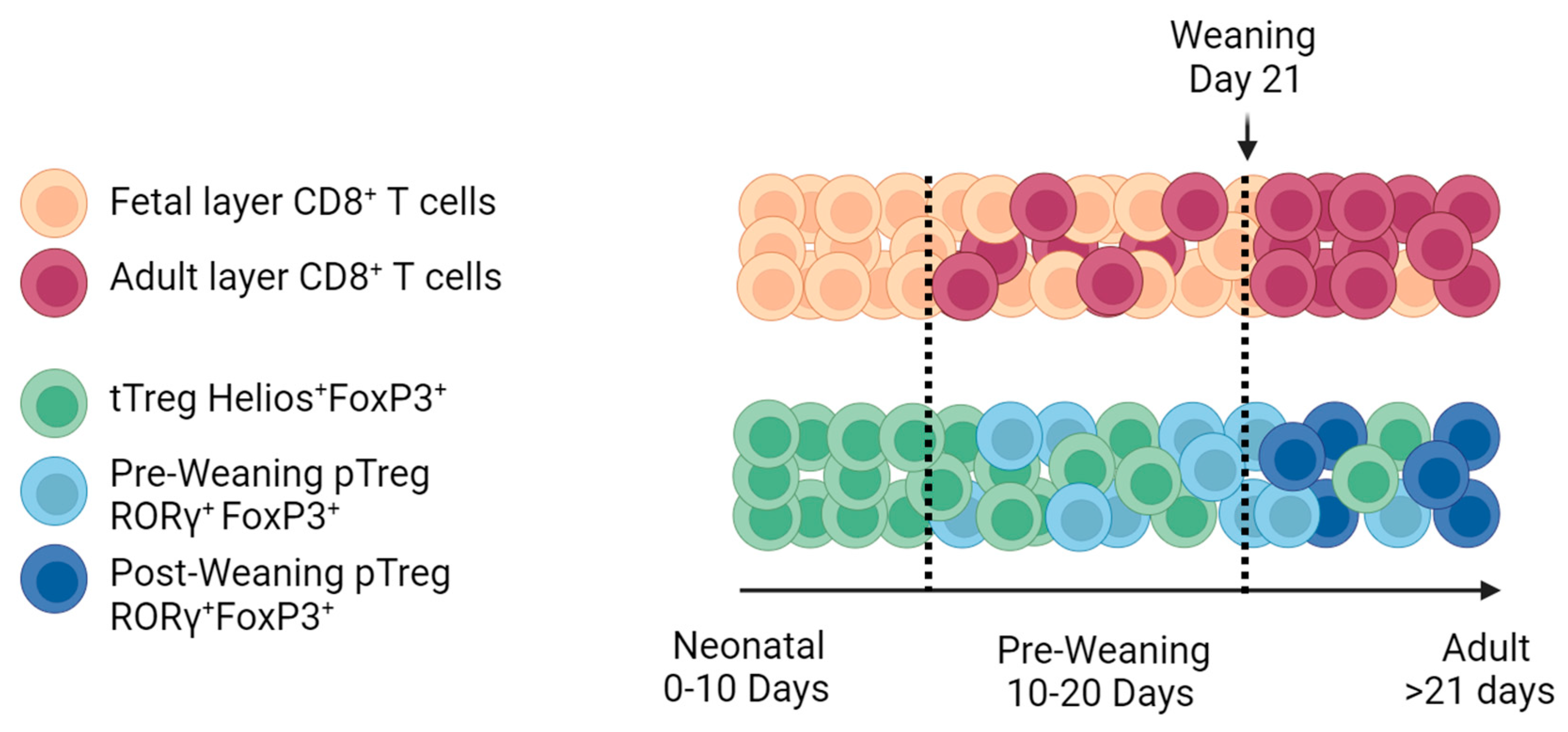
| T cells are functionally and transcriptionally different from adult T cells, supporting the hypothesis of the layered immunity theory. |
| T cells exhibit increased expression levels of innate-like receptors and respond in a bystander fashion. |
| TCRs are cross-reactive/autoreactive with limited diversity due to a lack of expression of TdT. |
| CD8+ T cells are prone to rapidly proliferating and differentiating in short-lived cells depending on the expression of T-bet. |
| Long-lived memory T-cell responses are diminished. |
| CD4+ T cells are prone to become Treg cells, and both humans and mice have comparable Helios+ and RORγ+ Treg subsets. |
| Both seem to have reduced capacity for the generation of mucosal TRM. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montenegro, C.; Perdomo-Celis, F.; Franco, M.A. Update on Early-Life T Cells: Impact on Oral Rotavirus Vaccines. Viruses 2024, 16, 818. https://doi.org/10.3390/v16060818
Montenegro C, Perdomo-Celis F, Franco MA. Update on Early-Life T Cells: Impact on Oral Rotavirus Vaccines. Viruses. 2024; 16(6):818. https://doi.org/10.3390/v16060818
Chicago/Turabian StyleMontenegro, Catherine, Federico Perdomo-Celis, and Manuel A. Franco. 2024. "Update on Early-Life T Cells: Impact on Oral Rotavirus Vaccines" Viruses 16, no. 6: 818. https://doi.org/10.3390/v16060818
APA StyleMontenegro, C., Perdomo-Celis, F., & Franco, M. A. (2024). Update on Early-Life T Cells: Impact on Oral Rotavirus Vaccines. Viruses, 16(6), 818. https://doi.org/10.3390/v16060818







