Lack of Association of Vascular Risk Factors with HIV-Associated Neurocognitive Disorders in cART-Treated Adults Aged ≥ 50 Years in Tanzania
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
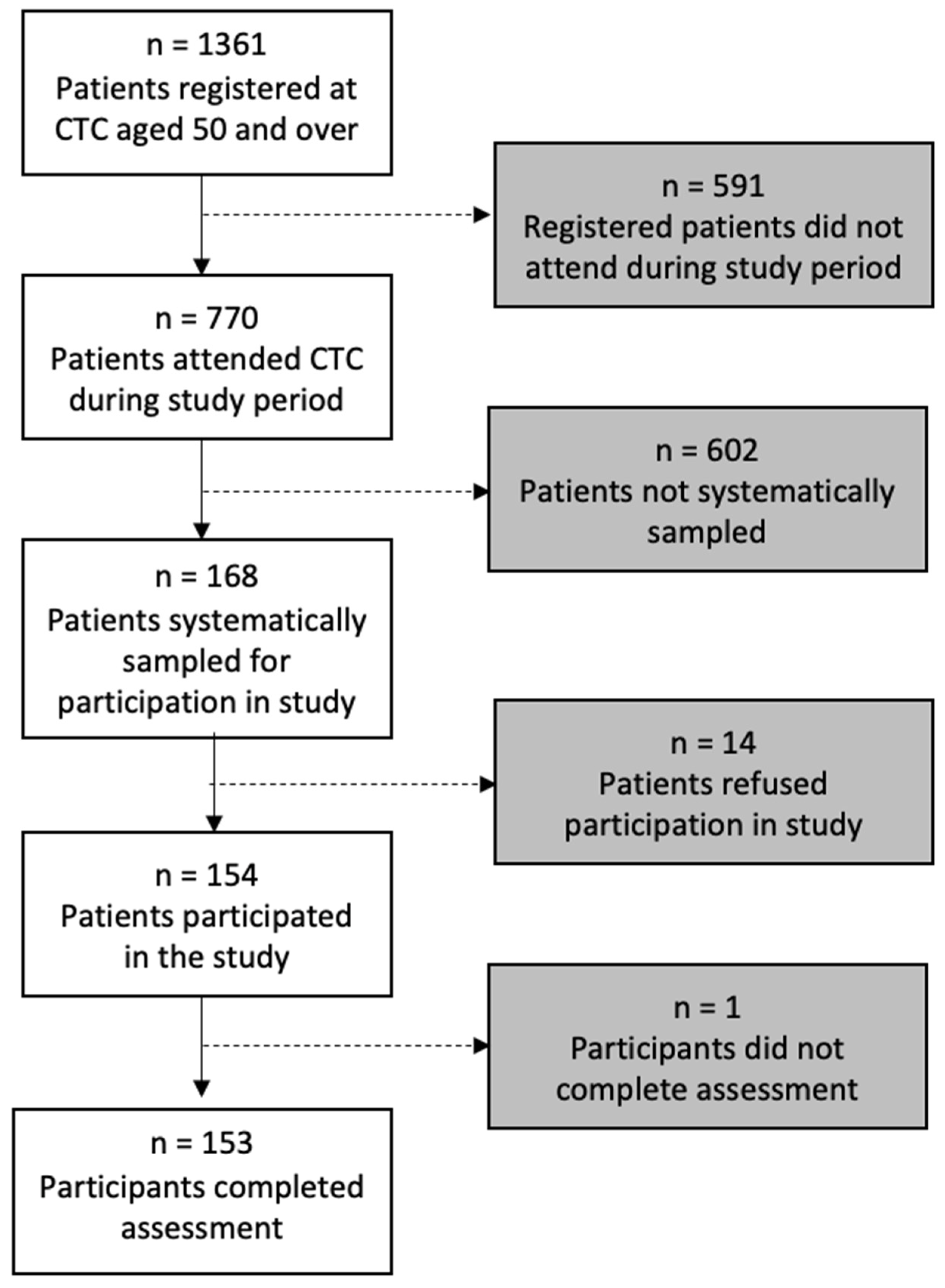
2.2. Sampling and Baseline Data Collection
2.3. Demographic and HIV-Disease Data
2.4. Assessment of Vascular Disease and Risk Factors
2.4.1. Vascular Risk Factors (VRFs)
2.4.2. Vascular End Organ Damage (EOD)
2.5. MRI Assessment
2.6. HAND Diagnosis and Classification
2.7. Statistical Methods
3. Results
3.1. Vascular Disease Burden
3.2. HAND Prevalence
3.3. Associations of HAND with HIV-Disease Factors
3.4. Associations of HAND with Vascular Risk Factors and Vascular EOD
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNAIDS. Global HIV & AIDS Statistics–2020 Fact Sheet. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 1 July 2021).
- Patel, P.; Rose, C.E.; Collins, P.Y.; Nuche-Berenguer, B.; Sahasrabuddhe, V.V.; Peprah, E.; Vorkoper, S.; Pastakia, S.D.; Rausch, D.; Levitt, N.S. Noncommunicable diseases among HIV-infected persons in low-income and middle-income countries: A systematic review and meta-analysis. AIDS Lond. Engl. 2018, 32 (Suppl. 1), S5. [Google Scholar] [CrossRef]
- Deeks, S.G.; Lewin, S.R.; Havlir, D.V. The end of AIDS: HIV infection as a chronic disease. Lancet 2013, 382, 1525–1533. [Google Scholar] [CrossRef]
- Guaraldi, G.; Orlando, G.; Zona, S.; Menozzi, M.; Carli, F.; Garlassi, E.; Berti, A.; Rossi, E.; Roverato, A.; Palella, F. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin. Infect. Dis. 2011, 53, 1120–1126. [Google Scholar] [CrossRef]
- Van Epps, P.; Kalayjian, R.C. Human immunodeficiency virus and aging in the era of effective antiretroviral therapy. Infect. Dis. Clin. 2017, 31, 791–810. [Google Scholar] [CrossRef]
- Antinori, A.; Arendt, G.; Becker, J.; Brew, B.; Byrd, D.; Cherner, M.; Clifford, D.; Cinque, P.; Epstein, L.; Goodkin, K. Updated research nosology for HIV-associated neurocognitive disorders. Neurology 2007, 69, 1789–1799. [Google Scholar] [CrossRef]
- Deeks, S.G. HIV infection, inflammation, immunosenescence, and aging. Annu. Rev. Med. 2011, 62, 141–155. [Google Scholar] [CrossRef]
- Heaton, R.; Clifford, D.; Franklin, D.; Woods, S.; Ake, C.; Vaida, F.; Ellis, R.; Letendre, S.; Marcotte, T.; Atkinson, J. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 2010, 75, 2087–2096. [Google Scholar] [CrossRef]
- Sacktor, N. Changing clinical phenotypes of HIV-associated neurocognitive disorders. J. Neurovirol. 2018, 24, 141–145. [Google Scholar] [CrossRef]
- Alford, K.; Vera, J. Cognitive impairment in people living with HIV in the ART era: A review. Br. Med. Bull. 2018, 127, 55–68. [Google Scholar] [CrossRef]
- Kinai, E.; Komatsu, K.; Sakamoto, M.; Taniguchi, T.; Nakao, A.; Igari, H.; Takada, K.; Watanabe, A.; Takahashi-Nakazato, A.; Takano, M. Association of age and time of disease with HIV-associated neurocognitive disorders: A Japanese nationwide multicenter study. J. Neurovirol. 2017, 23, 864–874. [Google Scholar] [CrossRef]
- Valcour, V.; Shikuma, C.; Shiramizu, B.; Watters, M.; Poff, P.; Selnes, O.; Holck, P.; Grove, J.; Sacktor, N. Higher frequency of dementia in older HIV-1 individuals: The Hawaii Aging with HIV-1 Cohort. Neurology 2004, 63, 822–827. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, M.; Lu, Q.; Farrell, M.; Lappin, J.M.; Shi, J.; Lu, L.; Bao, Y. Global prevalence and burden of HIV-associated neurocognitive disorder: A meta-analysis. Neurology 2020, 95, e2610–e2621. [Google Scholar] [CrossRef]
- Saylor, D.; Dickens, A.M.; Sacktor, N.; Haughey, N.; Slusher, B.; Pletnikov, M.; Mankowski, J.L.; Brown, A.; Volsky, D.J.; McArthur, J.C. HIV-associated neurocognitive disorder—Pathogenesis and prospects for treatment. Nat. Rev. Neurol. 2016, 12, 234–248. [Google Scholar] [CrossRef]
- Underwood, J.; Robertson, K.R.; Winston, A. Could antiretroviral neurotoxicity play a role in the pathogenesis of cognitive impairment in treated HIV disease? Aids 2015, 29, 253–261. [Google Scholar] [CrossRef]
- Bonnet, F.; Amieva, H.; Marquant, F.; Bernard, C.; Bruyand, M.; Dauchy, F.-A.; Mercié, P.; Greib, C.; Richert, L.; Neau, D. Cognitive disorders in HIV-infected patients: Are they HIV-related? Aids 2013, 27, 391–400. [Google Scholar] [CrossRef]
- Eaton, P.; Lewis, T.; Kellett-Wright, J.; Flatt, A.; Urasa, S.; Howlett, W.; Dekker, M.; Kisoli, A.; Rogathe, J.; Thornton, J. Risk factors for symptomatic HIV-associated neurocognitive disorder in adults aged 50 and over attending a HIV clinic in Tanzania. Int. J. Geriatr. Psychiatry 2020, 35, 1198–1208. [Google Scholar] [CrossRef]
- Namagga, J.K.; Rukundo, G.Z.; Voss, J.G. Prevalence and risk factors of HIV-associated neurocognitive disorders in rural Southwestern Uganda. J. Assoc. Nurses AIDS Care JANAC 2019, 30, 531. [Google Scholar] [CrossRef]
- Cysique, L.A.; Brew, B.J. Vascular cognitive impairment and HIV-associated neurocognitive disorder: A new paradigm. J. Neurovirol. 2019, 25, 710–721. [Google Scholar] [CrossRef]
- Moulignier, A.; Costagliola, D. Metabolic syndrome and cardiovascular disease impacts on the pathophysiology and phenotype of HIV-associated neurocognitive disorders. In Neurocognitive Complications of HIV-Infection: Neuropathogenesis to Implications for Clinical Practice; Springer: Cham, Switzerland, 2020; pp. 367–399. [Google Scholar]
- McIntosh, E.C.; Tureson, K.; Rotblatt, L.J.; Singer, E.J.; Thames, A.D. HIV, vascular risk factors, and cognition in the combination antiretroviral therapy era: A systematic review and meta-analysis. J. Int. Neuropsychol. Soc. 2021, 27, 365–381. [Google Scholar] [CrossRef]
- Adeloye, D. An estimate of the incidence and prevalence of stroke in Africa: A systematic review and meta-analysis. PLoS ONE 2014, 9, e100724. [Google Scholar] [CrossRef]
- Amegah, A.K. Tackling the growing burden of cardiovascular diseases in sub-Saharan Africa: Need for dietary guidelines. Circulation 2018, 138, 2449–2451. [Google Scholar] [CrossRef]
- Shah, A.S.; Stelzle, D.; Lee, K.K.; Beck, E.J.; Alam, S.; Clifford, S.; Longenecker, C.T.; Strachan, F.; Bagchi, S.; Whiteley, W. Global burden of atherosclerotic cardiovascular disease in people living with HIV: Systematic review and meta-analysis. Circulation 2018, 138, 1100–1112. [Google Scholar] [CrossRef]
- Hsue, P.Y.; Waters, D.D. Time to recognize HIV infection as a major cardiovascular risk factor. Am. Heart Assoc. 2018, 138, 1113–1115. [Google Scholar] [CrossRef]
- Walker, R.W.; Jusabani, A.; Aris, E.; Gray, W.K.; Unwin, N.; Swai, M.; Alberti, G.; Mugusi, F. Stroke risk factors in an incident population in urban and rural Tanzania: A prospective, community-based, case-control study. Lancet Glob. Health 2013, 1, e282–e288. [Google Scholar] [CrossRef]
- Kaddu-Mukasa, M.; Ssekasanvu, E.; Ddumba, E.; Thomas, D.; Katabira, E. Rheumatic manifestations among HIV positive adults attending the Infectious Disease Clinic at Mulago Hospital. Afr. Health Sci. 2011, 11. [Google Scholar]
- NACP National AIDS Control Programme. National Guidelines for the Management of HIV and AIDS; MoH Tanzania: Dar es Salaam, Tanzania, 2017. [Google Scholar]
- Weinberg, J.L.; Kovarik, C.L. The WHO clinical staging system for HIV/AIDS. AMA J. Ethics 2010, 12, 202–206. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO EXPERT Consultation; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Paccaud, F.; Schlüter-Fasmeyer, V.; Wietlisbach, V.; Bovet, P. Dyslipidemia and abdominal obesity: An assessment in three general populations. J. Clin. Epidemiol. 2000, 53, 393–400. [Google Scholar] [CrossRef]
- World Health Organization. The WHO STEPwise Approach to Noncommunicable Disease Risk Factor Surveillance (STEPS); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Chalmers, J.; MacMahon, S.; Mancia, G.; Whitworth, J.; Beilin, L.; Hansson, L.; Neal, B.; Rodgers, A.; Mhurchu, N.; Clark, T. 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines sub-committee of the World Health Organization. Clin. Exp. Hypertens. (N. Y. 1993) 1999, 21, 1009–1060. [Google Scholar]
- Noubiap, J.J.; Bigna, J.J.; Nansseu, J.R.; Nyaga, U.F.; Balti, E.V.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Prevalence of dyslipidaemia among adults in Africa: A systematic review and meta-analysis. Lancet Glob. Health 2018, 6, e998–e1007. [Google Scholar] [CrossRef]
- Sokolow, M.; Lyon, T.P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limbs leads. Am. Heart J. 1949, 37, 161–186. [Google Scholar] [CrossRef]
- Mendis, S.; Thygesen, K.; Kuulasmaa, K.; Giampaoli, S.; Mähönen, M.; Ngu Blackett, K.; Lisheng, L. World Health Organization definition of myocardial infarction: 2008–2009 revision. Int. J. Epidemiol. 2011, 40, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Desormais, I.; Aboyans, V.; Guerchet, M.; Ndamba-Bandzouzi, B.; Mbelesso, P.; Dantoine, T.; Mohty, D.; Marin, B.; Preux, P.M.; Lacroix, P. Prevalence of peripheral artery disease in the elderly population in urban and rural areas of Central Africa: The EPIDEMCA study. Eur. J. Prev. Cardiol. 2015, 22, 1462–1472. [Google Scholar] [CrossRef] [PubMed]
- Putnam, H.W.; Jones, R.; Rogathi, J.; Gray, W.K.; Swai, B.; Dewhurst, M.; Dewhurst, F.; Walker, R.W. Hypertension in a resource-limited setting: Is it associated with end organ damage in older adults in rural Tanzania? J. Clin. Hypertens. 2018, 20, 217–224. [Google Scholar] [CrossRef]
- Mackenzie, I.; Wilkinson, I.; Cockcroft, J. Assessment of arterial stiffness in clinical practice. Qjm 2002, 95, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.; Stevens, P.E.; Bilous, R.W.; Coresh, J.; De Francisco, A.L.; De Jong, P.E.; Griffith, K.E.; Hemmelgarn, B.R.; Iseki, K.; Lamb, E.J. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Kawasaki, R.; Cheung, N.; Wang, J.J.; Klein, R.; Klein, B.E.; Cotch, M.F.; Sharrett, A.R.; Shea, S.; Islam, F.A.; Wong, T.Y. Retinal vessel diameters and risk of hypertension: The Multiethnic Study of Atherosclerosis. J. Hypertens. 2009, 27, 2386. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.; Gentry, T.; Kellett-Wright, J.; Eaton, P.; Joseph, M.; Urasa, S.; Howlett, W.; Dekker, M.; Kisoli, A.; Rogathe, J. Prevalence and 1-year incidence of HIV-associated neurocognitive disorder (HAND) in adults aged≥ 50 years attending standard HIV clinical care in Kilimanjaro, Tanzania. Int. Psychogeriatr. 2023, 35, 339–350. [Google Scholar] [CrossRef]
- Kellett-Wright, J.; Flatt, A.; Eaton, P.; Urasa, S.; Howlett, W.; Dekker, M.; Kisoli, A.; Duijinmaijer, A.; Thornton, J.; McCartney, J. Screening for HIV-associated neurocognitive disorder (hand) in adults aged 50 and over attending a government HIV clinic in Kilimanjaro, Tanzania. Comparison of the International HIV dementia scale (IHDS) and idea six item dementia screen. AIDS Behav. 2021, 25, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, N.; Mittmann, N.; Silver, I.L.; Shulman, K.I.; Busto, U.A.; Shear, N.H.; Naranjo, C.A. A validation study of the Geriatric Depression Scale short form. Int. J. Geriatr. Psychiatry 1996, 11, 457–460. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A systematic review of current usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Péus, D.; Newcomb, N.; Hofer, S. Appraisal of the Karnofsky Performance Status and proposal of a simple algorithmic system for its evaluation. BMC Med. Inform. Decis. Mak. 2013, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Collingwood, C.; Paddick, S.-M.; Kisoli, A.; Dotchin, C.L.; Gray, W.K.; Mbowe, G.; Mkenda, S.; Urasa, S.; Mushi, D.; Chaote, P. Development and community-based validation of the IDEA study Instrumental Activities of Daily Living (IDEA-IADL) questionnaire. Glob. Health Action 2014, 7, 25988. [Google Scholar] [CrossRef] [PubMed]
- Dewhurst, M.; Dewhurst, F.; Gray, W.; Chaote, P.; Orega, G.; Walker, R. The high prevalence of hypertension in rural-dwelling Tanzanian older adults and the disparity between detection, treatment and control: A rule of sixths? J. Hum. Hypertens. 2013, 27, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, M.E.; Wit, F.W.; Roos, M.T.; Brewster, L.M.; Akande, T.M.; De Beer, I.H.; Mfinanga, S.G.; Kahwa, A.M.; Gatongi, P.; Van Rooy, G. Hypertension in sub-Saharan Africa: Cross-sectional surveys in four rural and urban communities. PLoS ONE 2012, 7, e32638. [Google Scholar] [CrossRef]
- Hertz, J.T.; Sakita, F.M.; Manavalan, P.; Madut, D.B.; Thielman, N.M.; Mmbaga, B.T.; Staton, C.A.; Galson, S.W. The Burden of Hypertension and Diabetes in an Emergency Department in Northern Tanzania. Ethn. Dis. 2019, 29, 559. [Google Scholar] [CrossRef] [PubMed]
- Ataklte, F.; Erqou, S.; Kaptoge, S.; Taye, B.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Burden of undiagnosed hypertension in sub-saharan Africa: A systematic review and meta-analysis. Hypertension 2015, 65, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Brennan, A.T.; Jamieson, L.; Crowther, N.J.; Fox, M.P.; George, J.A.; Berry, K.M.; Stokes, A.; Maskew, M.; Sanne, I.; Long, L. Prevalence, incidence, predictors, treatment, and control of hypertension among HIV-positive adults on antiretroviral treatment in public sector treatment programs in South Africa. PLoS ONE 2018, 13, e0204020. [Google Scholar] [CrossRef] [PubMed]
- Bigna, J.J.; Ndoadoumgue, A.L.; Nansseu, J.R.; Tochie, J.N.; Nyaga, U.F.; Nkeck, J.R.; Foka, A.J.; Kaze, A.D.; Noubiap, J.J. Global burden of hypertension among people living with HIV in the era of increased life expectancy: A systematic review and meta-analysis. J. Hypertens. 2020, 38, 1659–1668. [Google Scholar] [CrossRef]
- Hertz, J.T.; Prattipati, S.; Kweka, G.L.; Mlangi, J.J.; Tarimo, T.G.; Mmbaga, B.T.; Thielman, N.M.; Sakita, F.M.; Rubach, M.P.; Bloomfield, G.S. Prevalence and predictors of uncontrolled hypertension, diabetes, and obesity among adults with HIV in northern Tanzania. Glob. Public Health 2022, 17, 3747–3759. [Google Scholar] [CrossRef]
- Divala, O.H.; Amberbir, A.; Ismail, Z.; Beyene, T.; Garone, D.; Pfaff, C.; Singano, V.; Akello, H.; Joshua, M.; Nyirenda, M.J. The burden of hypertension, diabetes mellitus, and cardiovascular risk factors among adult Malawians in HIV care: Consequences for integrated services. BMC Public Health 2016, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mhode, M.; Nyamhanga, T. Experiences and impact of stigma and discrimination among people on antiretroviral therapy in Dar es Salaam: A qualitative perspective. AIDS Res. Treat. 2016, 2016, 7925052. [Google Scholar] [CrossRef] [PubMed]
- Johnston, L.E.; Stewart, B.T.; Yangni-Angate, H.; Veller, M.; Upchurch, G.R.; Gyedu, A.; Kushner, A.L. Peripheral arterial disease in sub-Saharan Africa: A review. JAMA Surg. 2016, 151, 564–572. [Google Scholar] [CrossRef]
- Jingi, A.M.; Noubiap, J.J.N.; Kamdem, P.; Kingue, S. Determinants and improvement of electrocardiographic diagnosis of left ventricular hypertrophy in a black African population. PLoS ONE 2014, 9, e96783. [Google Scholar] [CrossRef]
- Nkum, B.C.; Micah, F.B.; Ankrah, T.C.; Nyan, O. Left ventricular hypertrophy and insulin resistance in adults from an urban community in The Gambia: Cross-sectional study. PLoS ONE 2014, 9, e93606. [Google Scholar] [CrossRef] [PubMed]
- Abd ElHafeez, S.; Bolignano, D.; D’Arrigo, G.; Dounousi, E.; Tripepi, G.; Zoccali, C. Prevalence and burden of chronic kidney disease among the general population and high-risk groups in Africa: A systematic review. BMJ Open 2018, 8, e015069. [Google Scholar] [CrossRef] [PubMed]
- Kaboré, N.F.; Poda, A.; Zoungrana, J.; Da, O.; Ciaffi, L.; Semdé, A.; Yaméogo, I.; Sawadogo, A.B.; Delaporte, E.; Meda, N. Chronic kidney disease and HIV in the era of antiretroviral treatment: Findings from a 10-year cohort study in a west African setting. BMC Nephrol. 2019, 20, 1–10. [Google Scholar] [CrossRef]
- Freiberg, M.S.; Chang, C.-C.H.; Skanderson, M.; Patterson, O.V.; DuVall, S.L.; Brandt, C.A.; So-Armah, K.A.; Vasan, R.S.; Oursler, K.A.; Gottdiener, J. Association between HIV infection and the risk of heart failure with reduced ejection fraction and preserved ejection fraction in the antiretroviral therapy era: Results from the Veterans Aging Cohort Study. JAMA Cardiol. 2017, 2, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Beckman, J.A.; Duncan, M.S.; Alcorn, C.W.; So-Armah, K.; Butt, A.A.; Goetz, M.B.; Tindle, H.A.; Sico, J.J.; Tracy, R.P.; Justice, A.C. Association of human immunodeficiency virus infection and risk of peripheral artery disease. Circulation 2018, 138, 255–265. [Google Scholar] [CrossRef]
- Agu, C.E.; Uchendu, I.K.; Nsonwu, A.C.; Okwuosa, C.N.; Achukwu, P.U. Prevalence and associated risk factors of peripheral artery disease in virologically suppressed HIV-infected individuals on antiretroviral therapy in Kwara state, Nigeria: A cross sectional study. BMC Public Health 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Asch, F.M.; Shah, S.; Rattin, C.; Swaminathan, S.; Fuisz, A.; Lindsay, J. Lack of sensitivity of the electrocardiogram for detection of old myocardial infarction: A cardiac magnetic resonance imaging study. Am. Heart J. 2006, 152, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Hertz, J.T.; Sakita, F.M.; Kweka, G.L.; Limkakeng, A.T.; Galson, S.W.; Jinny, J.Y.; Tarimo, T.G.; Temu, G.; Thielman, N.M.; Bettger, J.P. Acute myocardial infarction under-diagnosis and mortality in a Tanzanian emergency department: A prospective observational study. Am. Heart J. 2020, 226, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Sardana, M.; Hsue, P.Y.; Tseng, Z.H.; Vittinghoff, E.; Nah, G.; Dewland, T.A.; Marcus, G.M. Human immunodeficiency virus infection and incident atrial fibrillation. J. Am. Coll. Cardiol. 2019, 74, 1512–1514. [Google Scholar] [CrossRef] [PubMed]
- Hamadou, B.; Ngweth, M.N.; Fotso, M.M.; Mfeukeu-Kuate, L.; Jingi, A.M.; Noubiap, J.J.; Nganou, C.N.; Boombhi, J.; Amougou, S.N.; Menanga, A. Echocardiographic and electrocardiographic abnormalities in adults living with human immunodeficiency virus: A cross-sectional study in the Yaoundé Central Hospital, Cameroon. Cardiovasc. Diagn. Ther. 2017, 7, 607. [Google Scholar] [CrossRef]
- Dewhurst, M.J.; Adams, P.C.; Gray, W.K.; Dewhurst, F.; Orega, G.P.; Chaote, P.; Walker, R.W. Strikingly low prevalence of atrial fibrillation in elderly Tanzanians. J. Am. Geriatr. Soc. 2012, 60, 1135–1140. [Google Scholar] [CrossRef] [PubMed]
- Soliman, E.Z.; Prineas, R.J.; Case, L.D.; Zhang, Z.-m.; Goff Jr, D.C. Ethnic distribution of ECG predictors of atrial fibrillation and its impact on understanding the ethnic distribution of ischemic stroke in the Atherosclerosis Risk in Communities (ARIC) study. Stroke 2009, 40, 1204–1211. [Google Scholar] [CrossRef]
- Hooi, J.D.; Kester, A.D.; Stoffers, H.E.; Rinkens, P.; Knottnerus, J.; Van Ree, J. Asymptomatic peripheral arterial occlusive disease predicted cardiovascular morbidity and mortality in a 7-year follow-up study. J. Clin. Epidemiol. 2004, 57, 294–300. [Google Scholar] [CrossRef]
- Walker, R.; Whiting, D.; Unwin, N.; Mugusi, F.; Swai, M.; Aris, E.; Jusabani, A.; Kabadi, G.; Gray, W.K.; Lewanga, M. Stroke incidence in rural and urban Tanzania: A prospective, community-based study. Lancet Neurol. 2010, 9, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.W.; McLarty, D.G.; Masuki, G.; Kitange, H.M.; Whiting, D.; Moshi, A.F.; Massawe, J.G.; Amaro, R.; Mhina, A.; Alberti, K. Age specific prevalence of impairment and disability relating to hemiplegic stroke in the Hai District of northern Tanzania. J. Neurol. Neurosurg. Psychiatry 2000, 68, 744–749. [Google Scholar] [CrossRef]
- Walker, R.; Jusabani, A.; Aris, E.; Gray, W.; Mugusi, F.; Swai, M.; Alberti, K.; Unwin, N. Correlates of short-and long-term case fatality within an incident stroke population in Tanzania. S. Afr. Med. J. 2013, 103, 107–112. [Google Scholar] [CrossRef]
- Grueter, B.E.; Schulz, U.G. Age-related cerebral white matter disease (leukoaraiosis): A review. Postgrad. Med. J. 2012, 88, 79–87. [Google Scholar] [CrossRef]
- Haddow, L.J.; Floyd, S.; Copas, A.; Gilson, R.J.C. A systematic review of the screening accuracy of the HIV Dementia Scale and International HIV Dementia Scale. PLoS ONE 2013, 8, e61826. [Google Scholar] [CrossRef] [PubMed]
- Howlett, W.P.; Urasa, S.J.; Maro, V.P.; Walker, R.W.; Kilonzo, K.G.; Howlett, P.J.; Dekker, M.C. Neurological disorders in Northern Tanzania: A 6-year prospective hospital-based case series. Afr. Health Sci. 2022, 22, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, R.; Schmidt, H.; Haybaeck, J.; Loitfelder, M.; Weis, S.; Cavalieri, M.; Seiler, S.; Enzinger, C.; Ropele, S.; Erkinjuntti, T. Heterogeneity in age-related white matter changes. Acta Neuropathol. 2011, 122, 171–185. [Google Scholar] [CrossRef]
- Graff-Radford, J.; Aakre, J.A.; Knopman, D.S.; Schwarz, C.G.; Flemming, K.D.; Rabinstein, A.A.; Gunter, J.L.; Ward, C.P.; Zuk, S.M.; Spychalla, A. Prevalence and heterogeneity of cerebrovascular disease imaging lesions. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1195–1205. [Google Scholar]
- Akinyemi, R.O.; Ovbiagele, B.; Adeniji, O.A.; Sarfo, F.S.; Abd-Allah, F.; Adoukonou, T.; Ogah, O.S.; Naidoo, P.; Damasceno, A.; Walker, R.W. Stroke in Africa: Profile, progress, prospects and priorities. Nat. Rev. Neurol. 2021, 17, 634–656. [Google Scholar] [CrossRef]
- Chow, F.C.; Price, R.W.; Hsue, P.Y.; Kim, A.S. Greater risk of stroke of undetermined etiology in a contemporary HIV-infected cohort compared with uninfected individuals. J. Stroke Cerebrovasc. Dis. 2017, 26, 1154–1160. [Google Scholar] [CrossRef] [PubMed]
- Chow, F.C.; Regan, S.; Feske, S.; Meigs, J.B.; Grinspoon, S.K.; Triant, V.A. Comparison of ischemic stroke incidence in HIV-infected and non-HIV-infected patients in a US health care system. J. Acquir. Immune Defic. Syndr. 2012, 60, 351. [Google Scholar] [CrossRef]
- Lin, H.-L.; Muo, C.-H.; Lin, C.-Y.; Chen, H.-J.; Chen, P.-C. Incidence of stroke in patients with HIV infection: A population-based study in Taiwan. PLoS ONE 2019, 14, e0217147. [Google Scholar] [CrossRef]
- Ryom, L.; Lundgren, J.D.; El-Sadr, W.; Reiss, P.; Kirk, O.; Law, M.; Phillips, A.; Weber, R.; Fontas, E.; Monforte, A.d.A. Cardiovascular disease and use of contemporary protease inhibitors: The D: A: D international prospective multicohort study. Lancet HIV 2018, 5, e291–e300. [Google Scholar] [CrossRef]
- Gutierrez, J.; Hatleberg, C.I.; Evans, H.; Yin, M.T. Role of pre-stroke immunity in ischemic stroke mechanism among patients with HIV. AIDS Care 2019, 31, 270–274. [Google Scholar] [CrossRef]
- Jusabani, A.; Gray, W.K.; Swai, M.; Walker, R. Post-stroke carotid ultrasound findings from an incident Tanzanian population. Neuroepidemiology 2011, 37, 245–248. [Google Scholar] [CrossRef]
- Estrada, V.; Portilla, J. Dyslipidemia related to antiretroviral therapy. AIDS Rev. 2011, 13, 49–56. [Google Scholar]
- Muya, E.; Kamuhabwa, A. Comparative assessment of the magnitude of hyperlipidemia in HIV-infected patients receiving lopinavir/r-and atazanavir/r-based antiretroviral drugs. J. Int. Assoc. Provid. AIDS Care (JIAPAC) 2019, 18, 2325958219841908. [Google Scholar] [CrossRef]
- Semu, H.; Zack, R.M.; Liu, E.; Hertzmark, E.; Spiegelman, D.; Sztam, K.; Hawkins, C.; Chalamila, G.; Muya, A.; Siril, H. Prevalence and risk factors for overweight and obesity among HIV-infected adults in Dar es Salaam, Tanzania. J. Int. Assoc. Provid. AIDS Care (JIAPAC) 2016, 15, 512–521. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Coetzee, L.; Bogler, L.; De Neve, J.W.; Bärnighausen, T.; Geldsetzer, P.; Vollmer, S. HIV, antiretroviral therapy and non-communicable diseases in sub-Saharan Africa: Empirical evidence from 44 countries over the period 2000 to 2016. J. Int. AIDS Soc. 2019, 22, e25364. [Google Scholar] [CrossRef]
- Gelpi, M.; Afzal, S.; Lundgren, J.; Ronit, A.; Roen, A.; Mocroft, A.; Gerstoft, J.; Lebech, A.-M.; Lindegaard, B.; Kofoed, K.F. Higher risk of abdominal obesity, elevated low-density lipoprotein cholesterol, and hypertriglyceridemia, but not of hypertension, in people living with human immunodeficiency virus (HIV): Results from the Copenhagen comorbidity in HIV infection study. Clin. Infect. Dis. 2018, 67, 579–586. [Google Scholar] [CrossRef]
- Matoti-Mvalo, T.; Puoane, T. Perceptions of body size and its association with HIV/AIDS. S. Afr. J. Clin. Nutr. 2011, 24, 40–45. [Google Scholar] [CrossRef]
- Sacktor, N.; Skolasky, R.L.; Seaberg, E.; Munro, C.; Becker, J.T.; Martin, E.; Ragin, A.; Levine, A.; Miller, E. Prevalence of HIV-associated neurocognitive disorders in the Multicenter AIDS Cohort Study. Neurology 2016, 86, 334–340. [Google Scholar] [CrossRef]
- Mwangala, P.N.; Mabrouk, A.; Wagner, R.; Newton, C.R.; Abubakar, A.A. Mental health and well-being of older adults living with HIV in sub-Saharan Africa: A systematic review. BMJ Open 2021, 11, e052810. [Google Scholar] [CrossRef]
- Marincowitz, C.; Genis, A.; Goswami, N.; De Boever, P.; Nawrot, T.S.; Strijdom, H. Vascular endothelial dysfunction in the wake of HIV and ART. FEBS J. 2019, 286, 1256–1270. [Google Scholar] [CrossRef]
- McCutchan, J.; Marquie-Beck, J.; Fitzsimons, C.; Letendre, S.; Ellis, R.; Heaton, R.; Wolfson, T.; Rosario, D.; Alexander, T.; Marra, C. Role of obesity, metabolic variables, and diabetes in HIV-associated neurocognitive disorder. Neurology 2012, 78, 485–492. [Google Scholar] [CrossRef]
- Wright, E.J.; Grund, B.; Cysique, L.A.; Robertson, K.; Brew, B.J.; Collins, G.; Shlay, J.; Winston, A.; Read, T.; Price, R.W. Factors associated with neurocognitive test performance at baseline: A substudy of the INSIGHT Strategic Timing of AntiRetroviral Treatment (START) trial. HIV Med. 2015, 16, 97–108. [Google Scholar] [CrossRef]
- Zhou, B.; Lu, Y.; Hajifathalian, K.; Bentham, J.; Di Cesare, M.; Danaei, G.; Bixby, H.; Cowan, M.J.; Ali, M.K.; Taddei, C. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4· 4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Paddick, S.-M.; Longdon, A.; Kisoli, A.; Gray, W.K.; Dotchin, C.L.; Jusabani, A.; Iqbal, A.; Hughes, J.; Teodorczuk, A.; Chaote, P. The prevalence of dementia subtypes in rural Tanzania. Am. J. Geriatr. Psychiatry 2014, 22, 1613–1622. [Google Scholar] [CrossRef]
- Gutierrez, J.; Albuquerque, A.L.; Falzon, L. HIV infection as vascular risk: A systematic review of the literature and meta-analysis. PLoS ONE 2017, 12, e0176686. [Google Scholar] [CrossRef]
- Saloner, R.; Sun-Suslow, N.; Morgan, E.E.; Lobo, J.; Cherner, M.; Ellis, R.J.; Heaton, R.K.; Grant, I.; Letendre, S.L.; Iudicello, J.E.; et al. Plasma biomarkers of vascular dysfunction uniquely relate to a vascular-risk profile of neurocognitive deficits in virally-suppressed adults with HIV. Brain Behav. Immun. -Health 2022, 26, 100560. [Google Scholar] [CrossRef]
- Vos, A.G.; Idris, N.S.; Barth, R.E.; Klipstein-Grobusch, K.; Grobbee, D.E. Pro-inflammatory markers in relation to cardiovascular disease in HIV infection. A systematic review. PLoS ONE 2016, 11, e0147484. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | |
| Females [n (%)] | 103 (67.3) |
| Median age [years (IQR)] | 56 (53–61.5) |
| Stratified Age Ranges [n (%)] | |
| 50–54 years | 55 (35.9) |
| 55–59 years | 42 (27.5) |
| 60–64 years | 32 (20.9) |
| 65–70 | 15 (9.8) |
| 70+ years | 9 (5.9) |
| Highest education level [n (%)] (m = 1) | |
| 0 years | 8 (5.3) |
| 1–4 years | 18 (11.8) |
| 5–7 years | 104 (68.4) |
| More than 7 years | 18 (11.8) |
| Higher education | 4 (2.6) |
| Occupation [n (%)] (m = 4) | |
| Sedentary | 44 (29.5) |
| Farmer | 89 (59.7) |
| Other manual job | 5 (3.4) |
| Not classified | 3 (2.0) |
| Never worked | 8 (5.4) |
| Currently in employment [n (%)] (m = 4) | 140 (94.0) |
| Marital status [n (%)] (m = 3) | |
| Married | 42 (28.0) |
| Widow(er) | 61 (40.7) |
| Divorced | 2 (1.3) |
| Separated | 37 (24.7) |
| Never married | 8 (5.3) |
| Household status [n (%)] (m = 3) | |
| Living alone | 34 (22.7) |
| Living with spouse | 27 (18.0) |
| Living with spouse and others | 24 (16.0) |
| Living with family | 60 (40.0) |
| Other | 5 (3.3) |
| HIV disease characteristics | |
| Median time since HIV diagnosis [years (IQR)] (m = 1) | 11.0 (6.0–13.0) |
| Mean current CD4 count ± SD [cells/mm3] (m = 23) | 499.8 ± 269.6 |
| Viral load (copies/mL) [n (%)] (m = 4) | |
| <20 20–10,000 >10,000 | 105 (70.5) 24 (16.1) 20 (13.4) |
| On cART treatment [n (%)] | 152 (99.3) |
| cART regimen * [n (%)] | |
| First line Second line Not yet initiated | 117 (76.5) 35 (22.9) 1 (0.7) |
| Forgets medication (self-report) [n (%)] (m = 1) | |
| Never Rarely Often Not applicable | 136 (89.5) 13 (8.6) 2 (1.3) 1 (0.7) |
| Time off medication in the last 12 months (self-report) [n (%)] (m = 1) | |
| No Yes Not applicable | 142 (93.4) 9 (5.9) 1 (0.7) |
| WHO clinical stage [n (%)] (m = 2) | |
| I II III IV | 3 (2.0) 25 (16.6) 122 (80.8) 1 (0.7) |
| Previous CNS infection [n (%)] (m = 3) | 4 (2.7) |
| TB infection status [n (%)] (m = 4) | |
| No infection Previous infection Current infection | 125 (83.9) 23 (15.4) 1 (0.7) |
| Positive syphilis VDRL [n (%)] (m = 12) | 23 (16.3) |
| Positive Hepatitis B [n (%)] (m = 11) | 6 (4.2) |
| Positive Hepatitis C [n (%)] (m = 11) | 1 (0.7) |
| Vascular Risk Factors (VRFs) | |
| Median BMI [kg/m2 (IQR)] | 22.9 (20.0–26.6) |
| BMI categories (kg/m2) [n (%)] | |
| Underweight (<18.5) | 14 (9.2) |
| Normal (18.5–24.9) | 82 (53.6) |
| Overweight (25.0–29.9) | 41 (26.8) |
| Obese (≥30) | 16 (10.5) |
| Mean WHR ± SD (m = 5) | 0.873 ± 0.08 |
| Abdominal obesity [n (%)] (m = 5) | 81 (54.7) |
| Mean systolic BP ± SD (mmHg) (m = 1) | 133.9 ± 27.3 |
| Mean diastolic BP ± SD (mmHg) (m = 1) | 80.72 ± 12.3 |
| Hypertension [n (%)] | 52 (34.0) |
| Diabetes Mellitus (self-report) [n (%)] (m = 3) | 8 (5.3) |
| If DM, on treatment [n (%)] | |
| Yes | 6 (75.0) |
| No | 1 (12.5) |
| Defaulted from treatment | 1 (12.5) |
| Smoking status [n (%)] | |
| Never smoked | 113 (73.9) |
| Previously smoker | 33 (21.6) |
| Current smoker | 7 (4.6) |
| Alcohol consumption [n (%)] (48 values missing) | |
| Never | 17 (16.2) |
| Previous | 31 (29.5) |
| Occasional | 31 (29.5) |
| Regular | 26 (24.8) |
| Mean serum cholesterol ± SD [mmol/L] (m = 12) | 4.7 ± 1.2 |
| Hypercholesterolaemia [n (%)] (m = 12) | 47 (33.3) |
| End Organ Damage (EOD) | |
| Atrial fibrillation [n (%)] (m = 1) | 0 (0.0) |
| Previous stroke [n (%)] | 8 (5.2) |
| Prior MI [n (%)] (m = 3) | 2 (1.3) |
| LVH [n (%)] (m = 1) | 19 (12.5) |
| Proteinuria [n (%)] (m = 1) | 5 (3.3) |
| Median serum creatinine [μol/L (IQR)] | 66.0 (56.0–77.5) |
| CKD [n (%)] (m = 12) | 8 (5.7) |
| Mean ABPI ± SD | 1.1 ± 0.2 |
| PAD [n (%)] (m = 3) | 5 (3.3) |
| Arterial stiffening [n (%)] (m = 3) | 6 (4.0) |
| Median pulse pressure [mmHg (IQR)] | 49.0 (39.0–62.0) |
| Risk Factor | 50–59 Years (n = 97) | ≥60 Years (n = 56) | Chi-Squared Test | ||
|---|---|---|---|---|---|
| Prevalence (%) | 95% CI | Prevalence (%) | 95% CI | ||
| Obesity | 11.3 | 5.0–17.7 | 8.9 | 1.5–16.4 | X2= 0.221, p = 0.639 |
| Abdominal obesity | 54.7 (m = 2) | 44.7–64.7 | 54.7 (m = 3) | 41.3–68.1 | X2 = <0.0001, p = 0.998 |
| Hypertension | 26.8 | 18.0–35.6 | 46.4 | 33.4–59.5 | X2 = 6.094, p = 0.014 ** |
| Diabetes mellitus | 4.2 (m = 2) | 0.2–8.2 | 7.3 (m = 1) | 0.4–14.1 | p = 0.465 (Fisher’s exact test) |
| Smoker (current/previous) | 22.7 | 14.3–31.0 | 32.2 | 19.9–44.4 | X2 = 1.646, p = 0.199 |
| Current alcohol | 50.0 (m = 27) | 38.3–61.7 | 62.9 (m = 21) | 46.8–78.9 | X2 = 1.554, p = 0.213 |
| Hypercholesterolaemia | 38.5 (m = 6) | 28.5–48.5 | 24.0 (m = 6) | 12.2–35.8 | X2 = 3.037, p = 0.081 |
| Variable | HAND (n = 102) | No HAND (n = 51) | Statistical Comparison |
|---|---|---|---|
| Vascular risk factors (VRFs) | |||
| Median BMI [kg/m2 (IQR)] | 21.9 (19.7–25.8) | 23.7 (20.0–27.1) | U = 2164.5, Z = −1.689, p = 0.091 |
| Obesity [n (%)] | 10 (9.8) | 6 (11.8) | X2= 0.140, p = 0.709 |
| Mean WHR ± SD | 0.87 ± 0.09 (m = 3) | 0.88 ± 0.06 (m = 2) | T = 1.173, p = 0.243 |
| Abdominal obesity [n (%)] | 50 (50.5) (m = 3) | 31 (63.3) (m = 2) | X2 = 2.154, p = 0.142 |
| Mean systolic BP ± SD (mmHg) | 132.4 ± 27.5 | 137.0 ± 26.7 (m = 1) | T = 0.972, p = 0.333 |
| Mean diastolic BP ± SD (mmHg) | 79.2 ± 12.0 | 83.9 ± 12.5 (m = 1) | T = 2.247, p = 0.026 ** |
| Hypertension [n (%)] | 32 (31.4) | 20 (39.2) | X2 = 0.932, p = 0.334 |
| Diabetes mellitus [n (%)] | 6 (6.0) (m = 2) | 2 (4.0) (m = 1) | p = 0.719 (Fisher’s exact test) |
| Smoker (current/previous) [n (%)] | 28 (27.5) | 12 (23.5) | X2 = 0.271, p = 0.603 |
| Current alcohol consumption [n (%)] | 35 (55.6) (m = 39) | 22 (52.4) (m = 9) | X2 = 0.102, p = 0.749 |
| Mean serum cholesterol ± SD [mmol/L] | 4.7 ± 1.3 (m = 6) | 4.9 ± 1.1 (m = 6) | T = 0.908, p = 0.365 |
| Hypercholesterolaemia [n (%)] | 31 (32.3) (m = 6) | 16 (35.6) (m = 6) | X2 = 0.147, p = 0.702 |
| Vascular End organ damage (EOD) | |||
| Previous stroke [n (%)] | 5 (4.9) | 3 (5.9) | p = 1.000 (Fisher’s exact test) |
| Prior MI [n (%)] | 1 (1.0) | 1 (2.1) (m = 3) | X2 = 0.302, p = 0.583 |
| LVH [n (%)] | 10 (9.9) (m = 1) | 9 (17.6) | X2 = 1.859, p = 0.173 |
| Proteinuria [n (%)] | 4 (4.0) (m = 1) | 1 (2.0) | p = 0.454 (Fisher’s exact test) |
| CKD [n (%)] | 7 (7.3) (m = 6) | 1 (2.2) (m = 6) | p = 0.211 (Fisher’s exact test) |
| Median creatinine [μol/L (IQR)] | 66.0 (56.0–77.75) (m = 6) | 68.0 (56.0–76.5) (m = 6) | U = 2220.5, Z = 0.268, p = 0.789 |
| Mean ABPI ± SD | 1.08 ± 0.19 (m = 3) | 1.08 ± 0.12 | T = −0.250, p = 0.803 |
| PAD [n (%)] | 4 (4.0) (m = 3) | 1 (2.0) | p = 0.445 (Fisher’s exact test) |
| Arterial stiffening [n (%)] | 4 (4.0) (m = 3) | 2 (3.9) | p = 0.669 (Fisher’s exact test) |
| Median pulse pressure [mmHg (IQR)] | 48.0 (38.0–61.3) | 49.0 (40.0–64.0) | X2 = 2557.5, Z = −0.168, p = 0.866 |
| Mean AVR ± SD | 0.76 ± 0.08 (m = 25) | 0.73 ± 0.08 (m = 7) | T = −1.587, p = 0.115 |
| WMD rating [n (%)] None Mild Moderate Severe | (m = 45) | (m = 18) | U = 937, Z = −0.031, p = 0.975 |
| 26 (45.6) | 13 (39.4) | ||
| 9 (15.8) | 9 (27.3) | ||
| 21 (36.8) | 11 (33.3) | ||
| 1 (1.8) | 0 (0.0) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flack, K.A.; Rainey, E.S.; Urasa, S.J.; Koipapi, S.; Kalaria, R.N.; Howlett, W.P.; Mukaetova-Ladinska, E.B.; Dekker, M.C.J.; Gray, W.K.; Walker, R.W.; et al. Lack of Association of Vascular Risk Factors with HIV-Associated Neurocognitive Disorders in cART-Treated Adults Aged ≥ 50 Years in Tanzania. Viruses 2024, 16, 819. https://doi.org/10.3390/v16060819
Flack KA, Rainey ES, Urasa SJ, Koipapi S, Kalaria RN, Howlett WP, Mukaetova-Ladinska EB, Dekker MCJ, Gray WK, Walker RW, et al. Lack of Association of Vascular Risk Factors with HIV-Associated Neurocognitive Disorders in cART-Treated Adults Aged ≥ 50 Years in Tanzania. Viruses. 2024; 16(6):819. https://doi.org/10.3390/v16060819
Chicago/Turabian StyleFlack, Katherine A., Emma S. Rainey, Sarah J. Urasa, Sengua Koipapi, Rajesh N. Kalaria, William P. Howlett, Elizabeta B. Mukaetova-Ladinska, Marieke C. J. Dekker, William K. Gray, Richard W. Walker, and et al. 2024. "Lack of Association of Vascular Risk Factors with HIV-Associated Neurocognitive Disorders in cART-Treated Adults Aged ≥ 50 Years in Tanzania" Viruses 16, no. 6: 819. https://doi.org/10.3390/v16060819
APA StyleFlack, K. A., Rainey, E. S., Urasa, S. J., Koipapi, S., Kalaria, R. N., Howlett, W. P., Mukaetova-Ladinska, E. B., Dekker, M. C. J., Gray, W. K., Walker, R. W., Dotchin, C. L., Mtwaile, H., Lewis, T. C. D., Stone, L. G., McNally, R. J. Q., Makupa, P. C., & Paddick, S.-M. (2024). Lack of Association of Vascular Risk Factors with HIV-Associated Neurocognitive Disorders in cART-Treated Adults Aged ≥ 50 Years in Tanzania. Viruses, 16(6), 819. https://doi.org/10.3390/v16060819





