Effectiveness of a Virtual Reality Head-Mounted Display System-Based Developmental Eye Movement Test
Abstract
:Introduction
DEM and VHD
- The test performance time is revised and recorded in accordance with the number of inaccuracies. Accordingly, the test performance time and the number of inaccuracies are important factors in the evaluation. The DEM test procedure is described below.
- Tests A and B are read aloud in the vertical direction. The time required for reading and the number of inaccurate answers, additional numbers (including repetitions), omissions, and switches is recorded.
- Test C is read aloud in the horizontal direction. The time required for reading and the number of inaccurate answers, additional numbers (including repetitions), omissions, and switches is recorded.
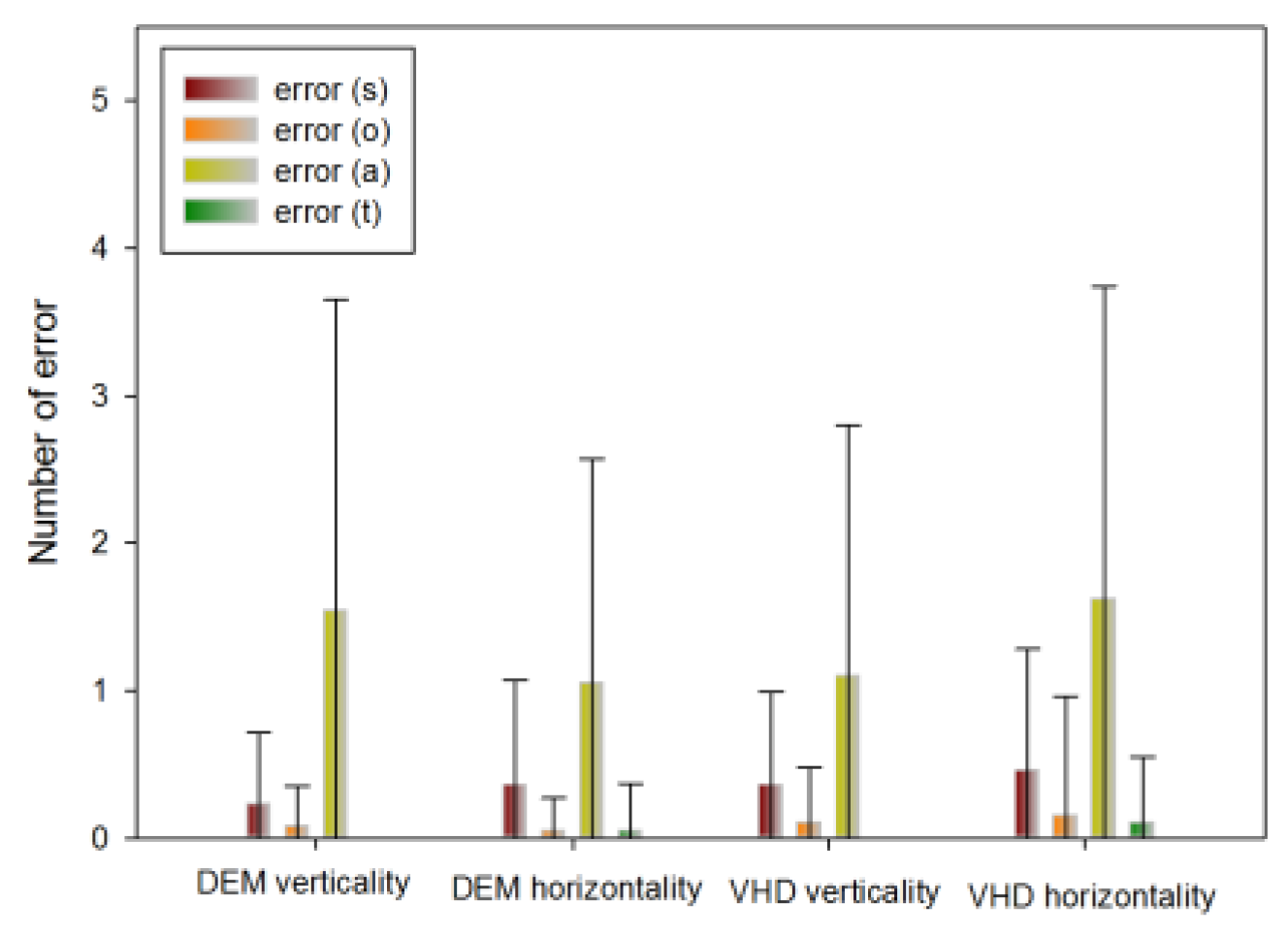
- Check the total number of inaccuracies. Inaccurately read numbers should be marked s, additional numbers should be marked a, omissions should be marked o, and switches in order during reading should be marked t. Therefore, the total number of inaccurate answers is calculated as s+a+o+t.
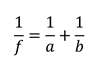
- The adjusted time isHere, the measurement time is the time required to read the horizontally arranged numbers aloud, o is the quantity of numbers omitted during reading, and a is the quantity of repeated or additional numbers.
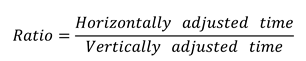
- Calculate the horizontally adjusted versus vertically adjusted time as follows:

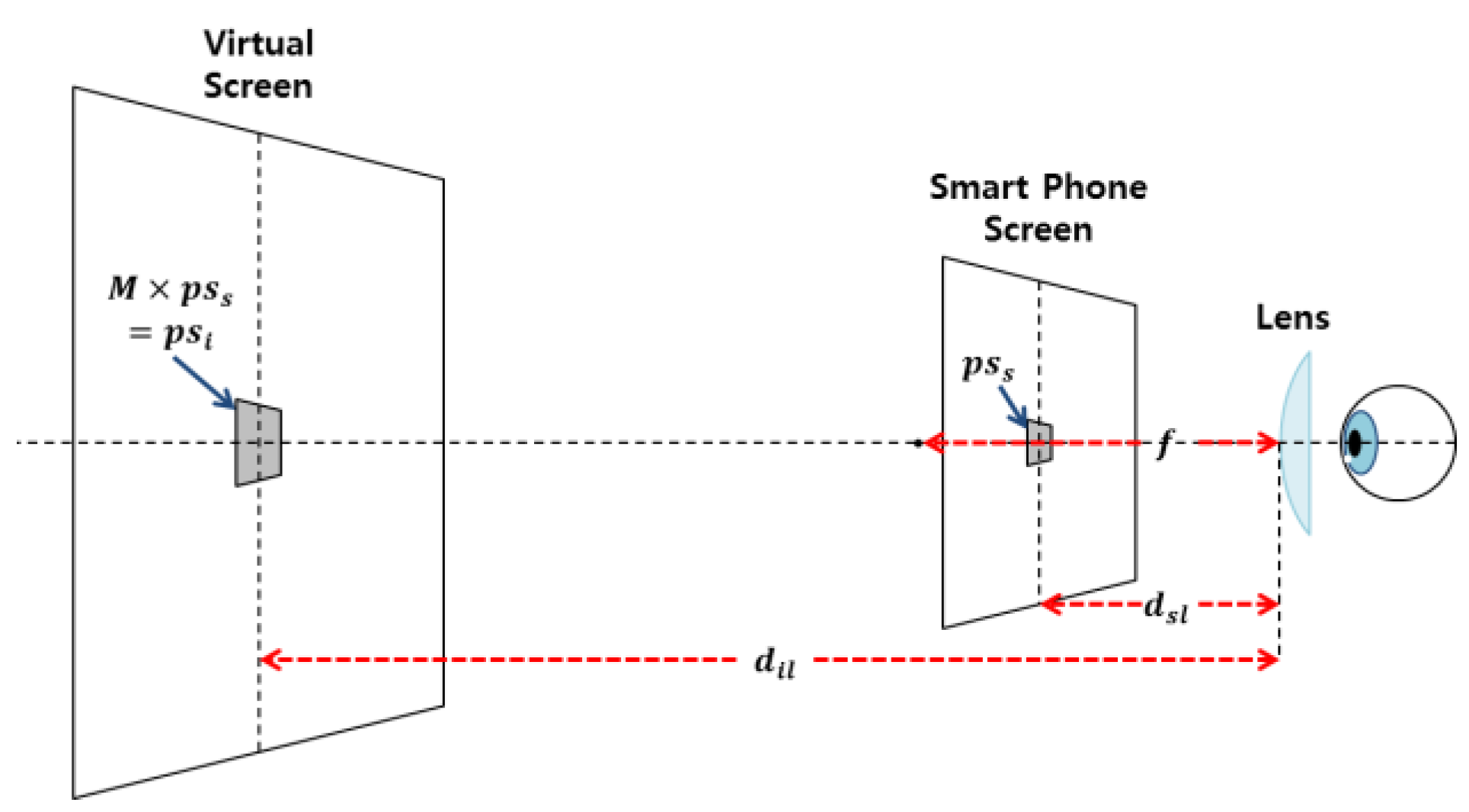
VR HMD
Optical system
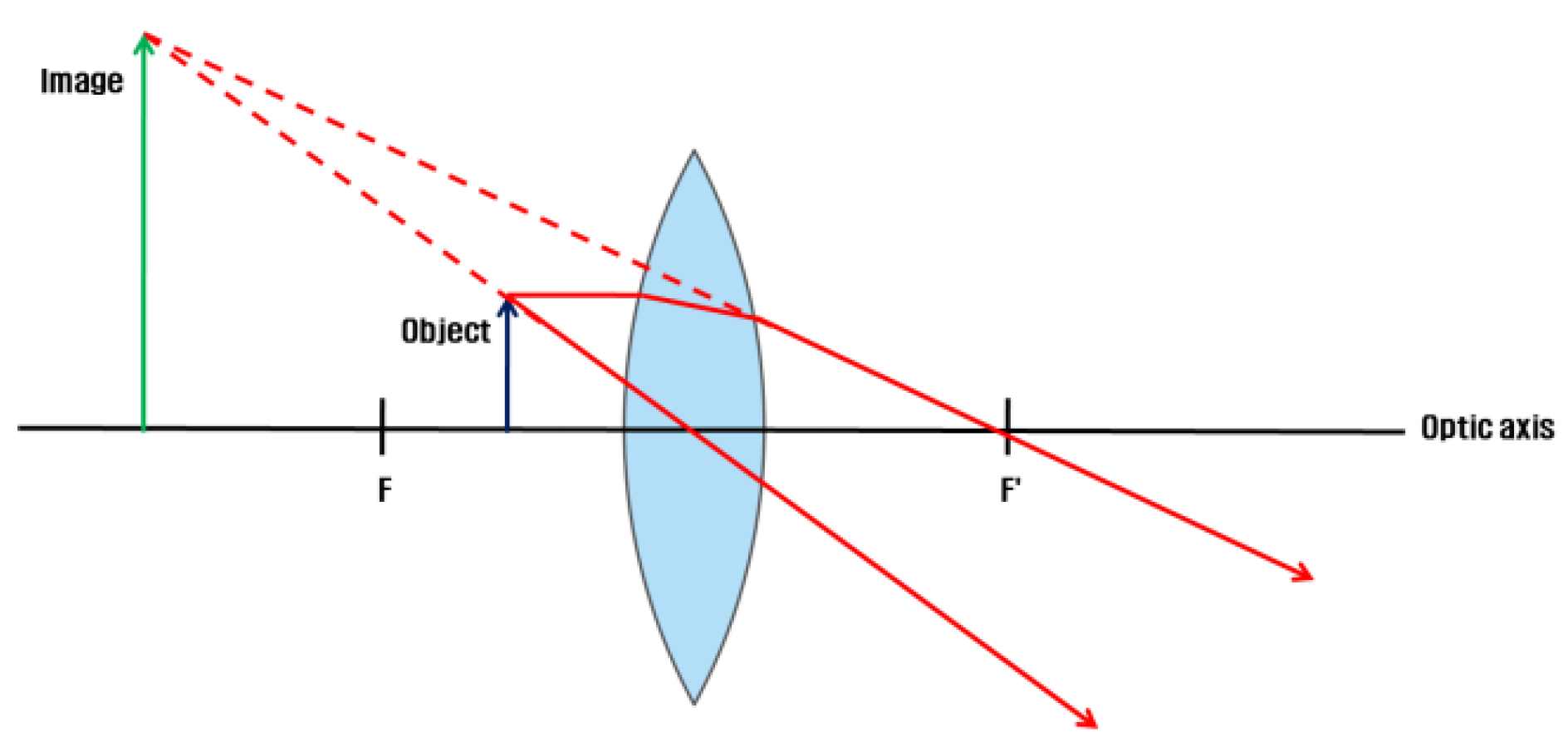
Image formation on the convex lens
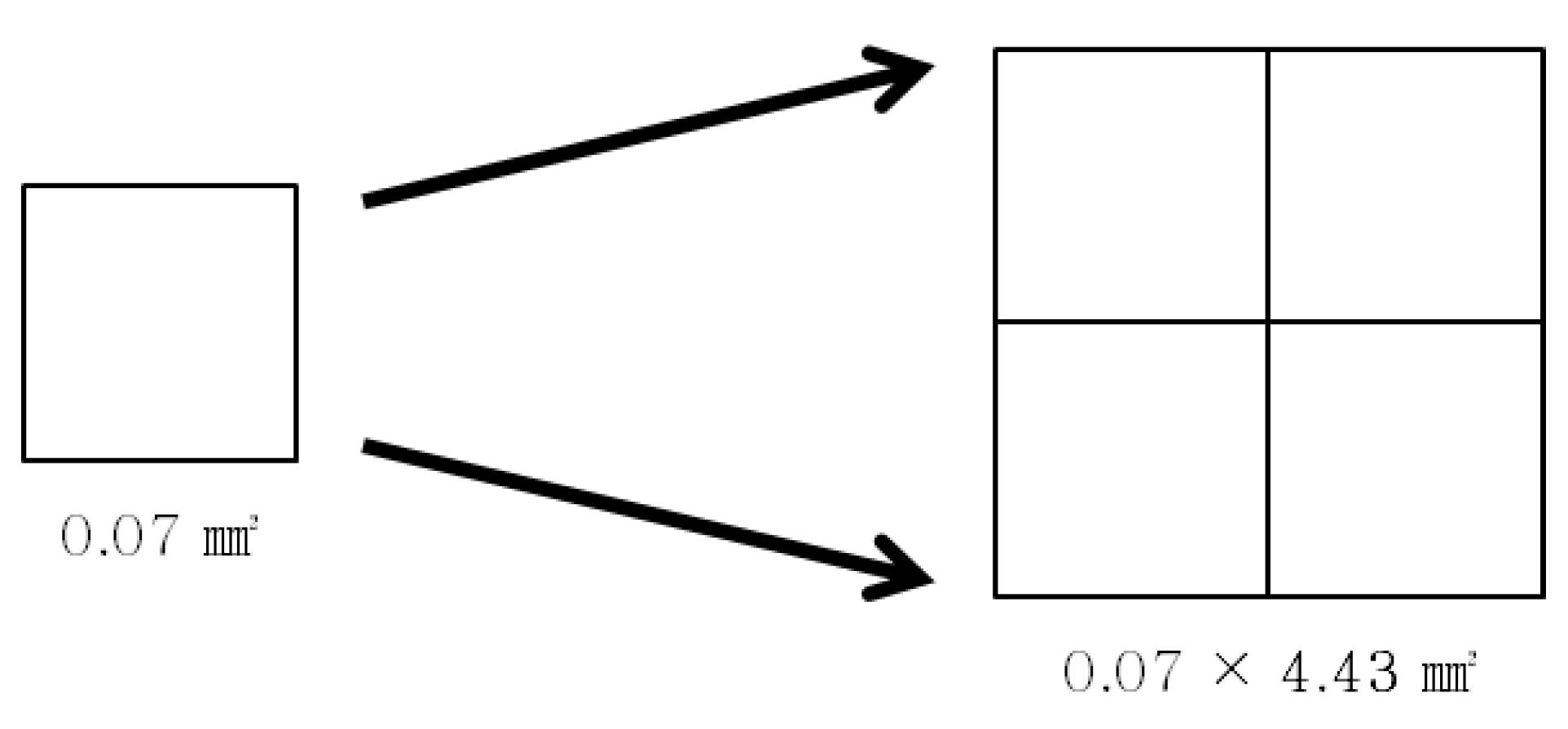
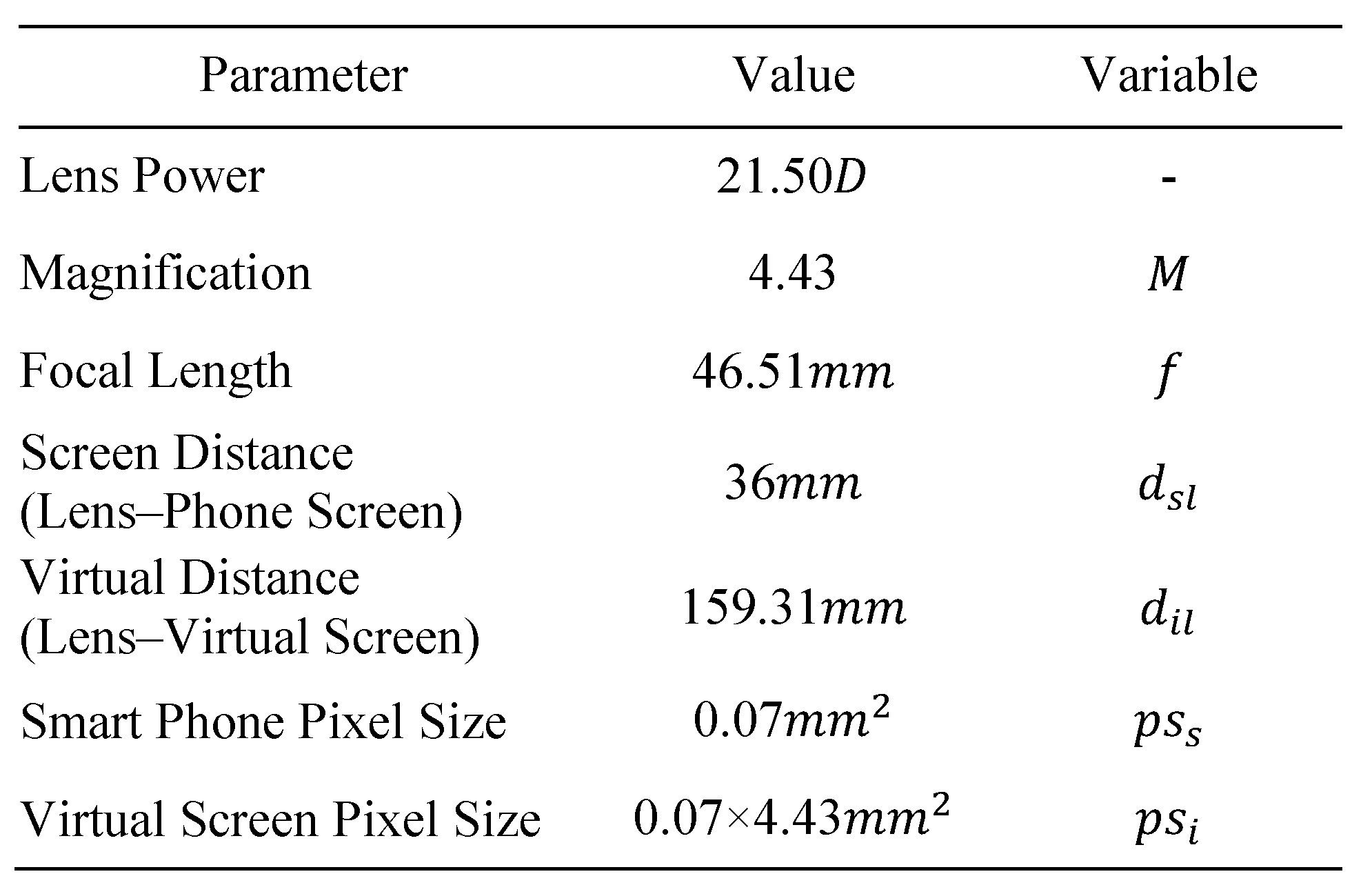
VR HMD parameters
Methods
Participants
Procedure
Medical questionnaire and prior eye movement tes
Visual function test
VHD chart production

Survey of subjective symptoms
Data analysis
Results
Near point test
Change in NPC
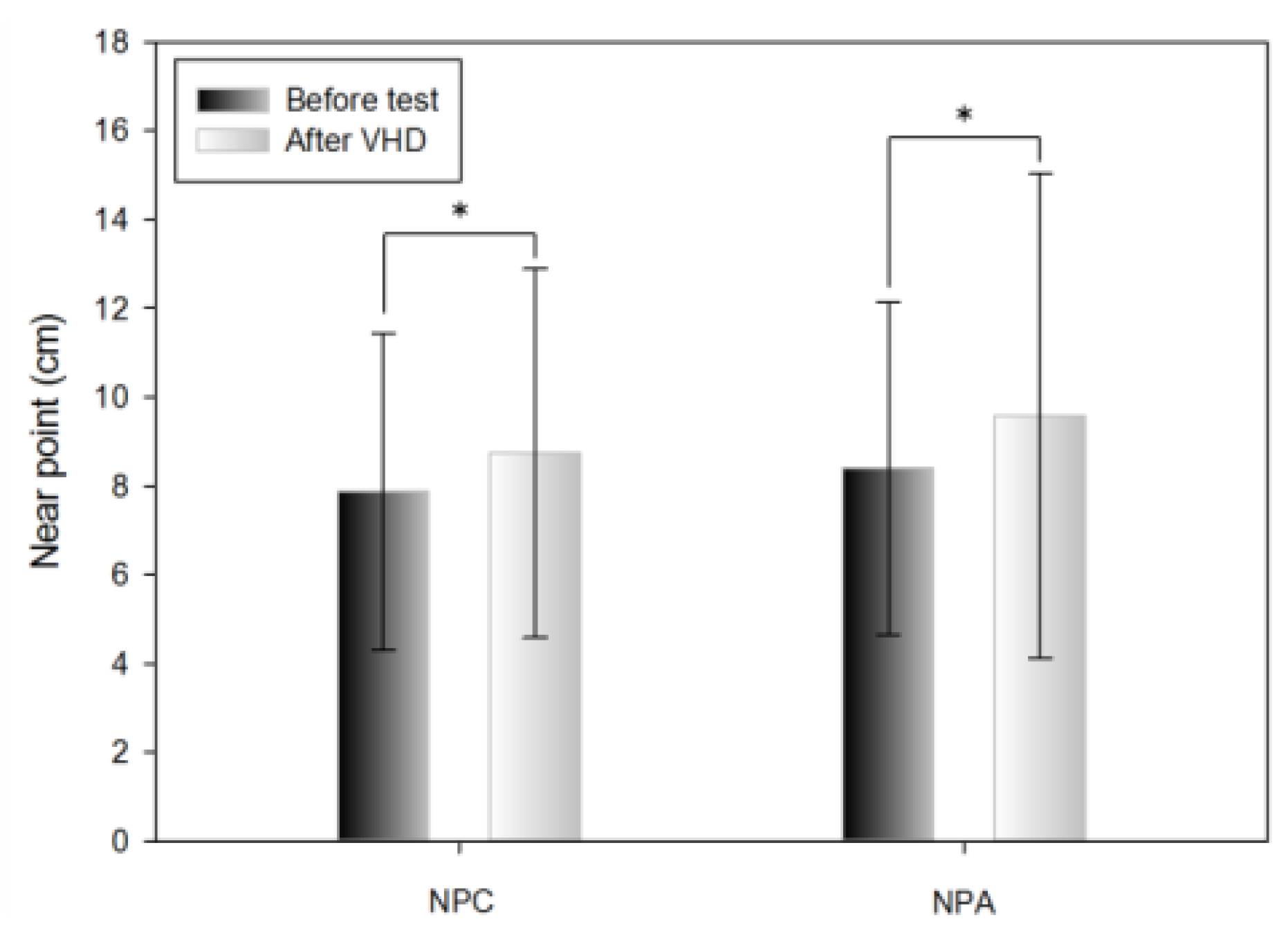
Change in NPA
Phoria test
Change in horizontal far phoria
Change in the horizontal near phoria

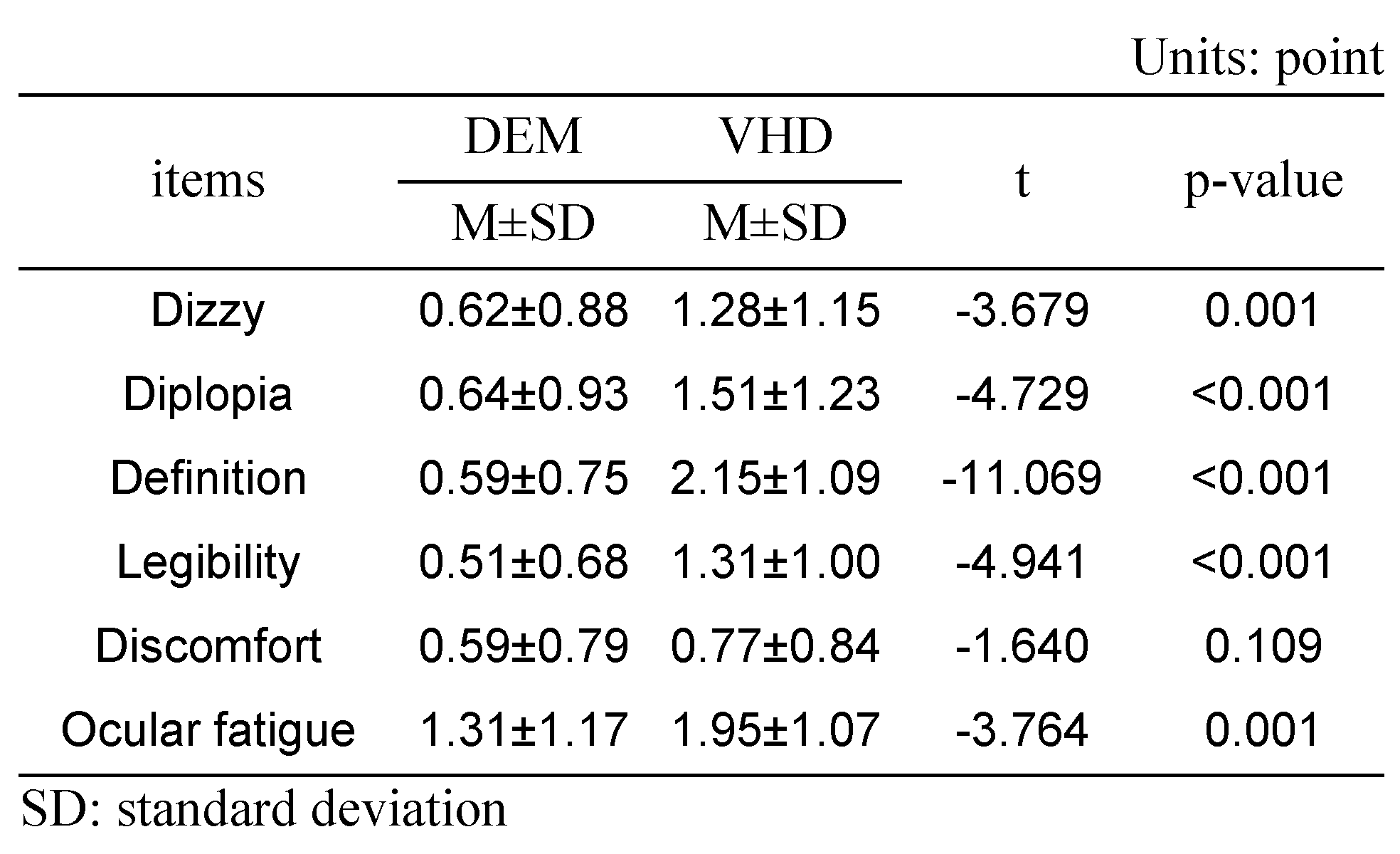
Subjective symptoms
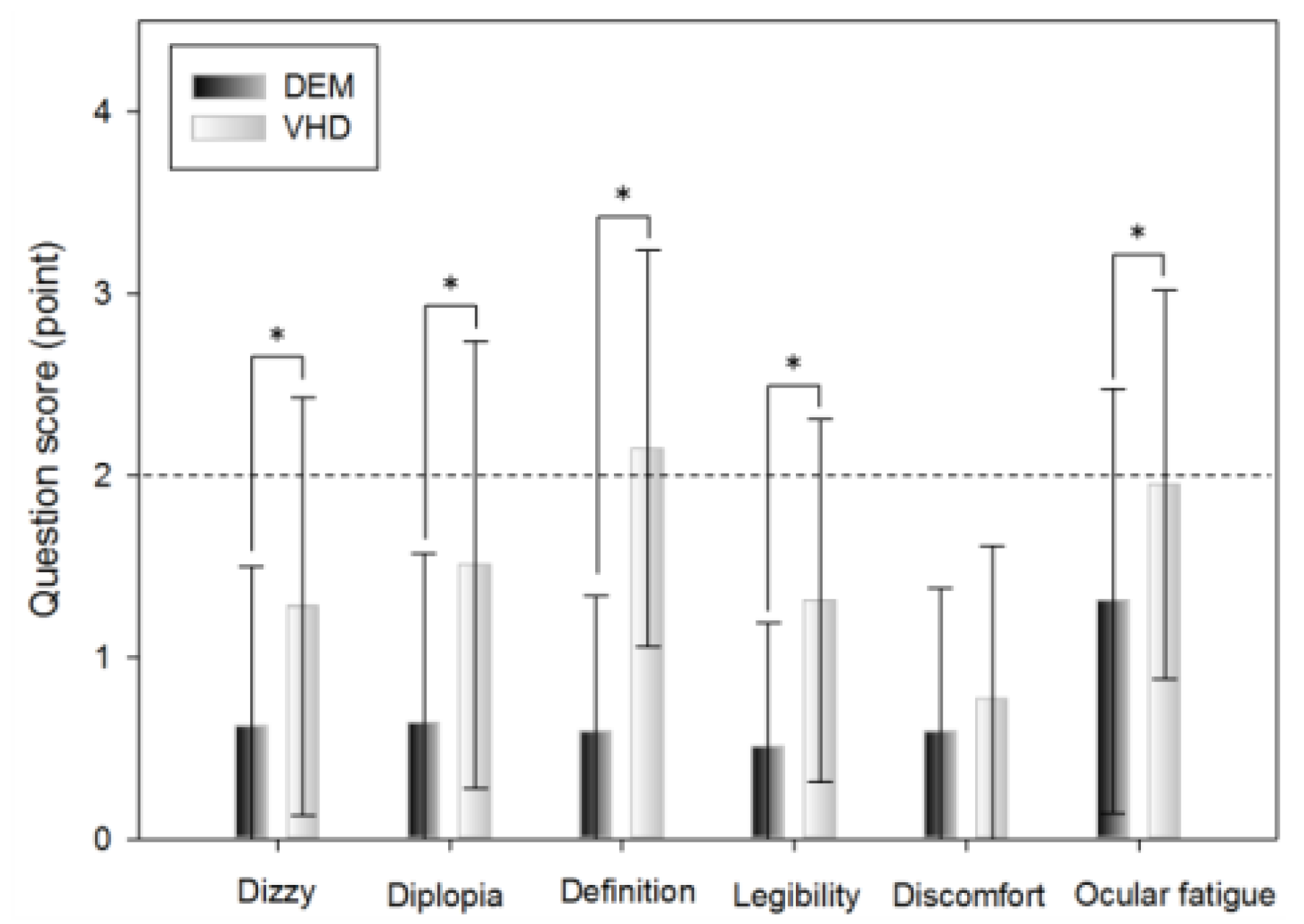
DEM and VHD
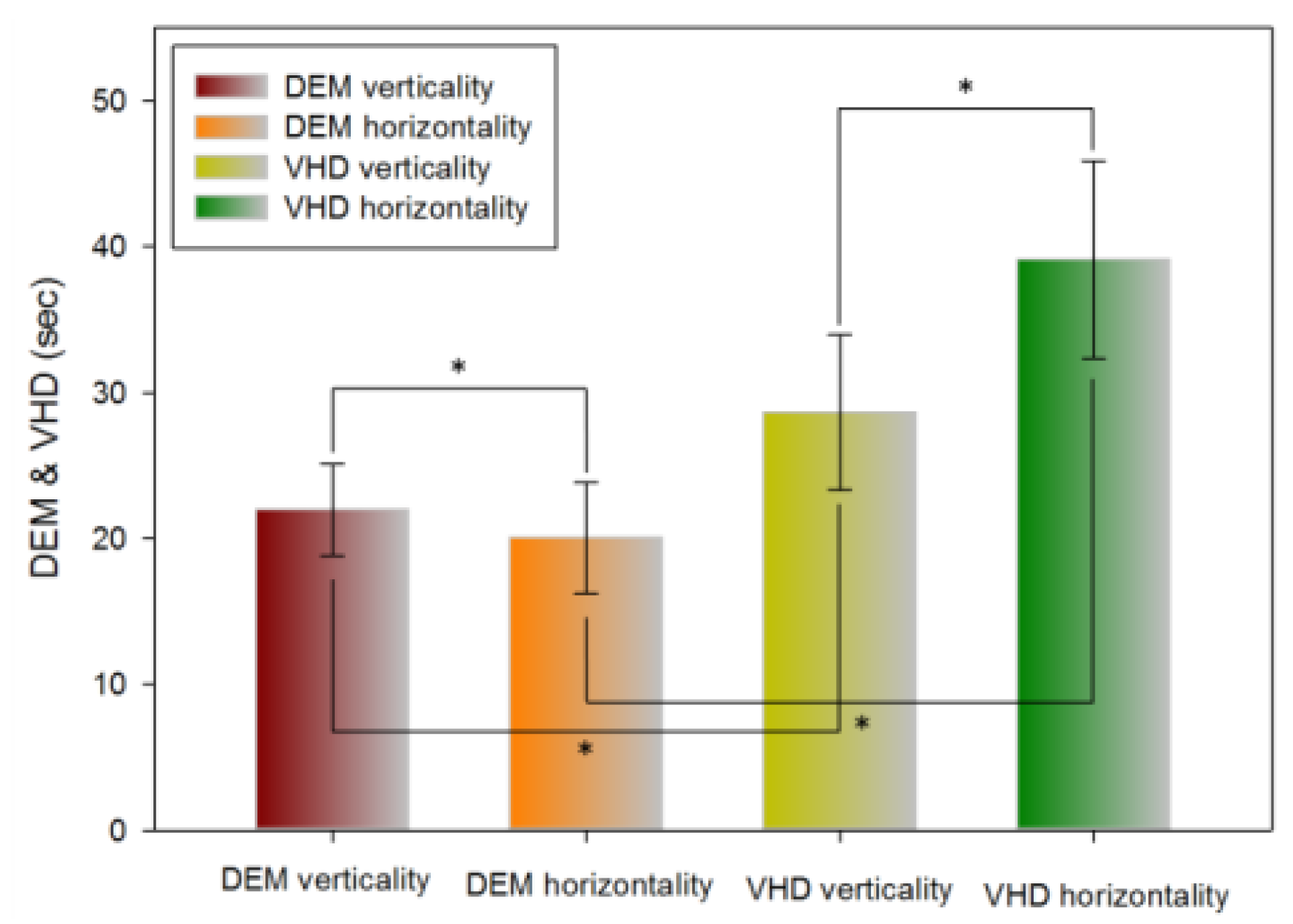
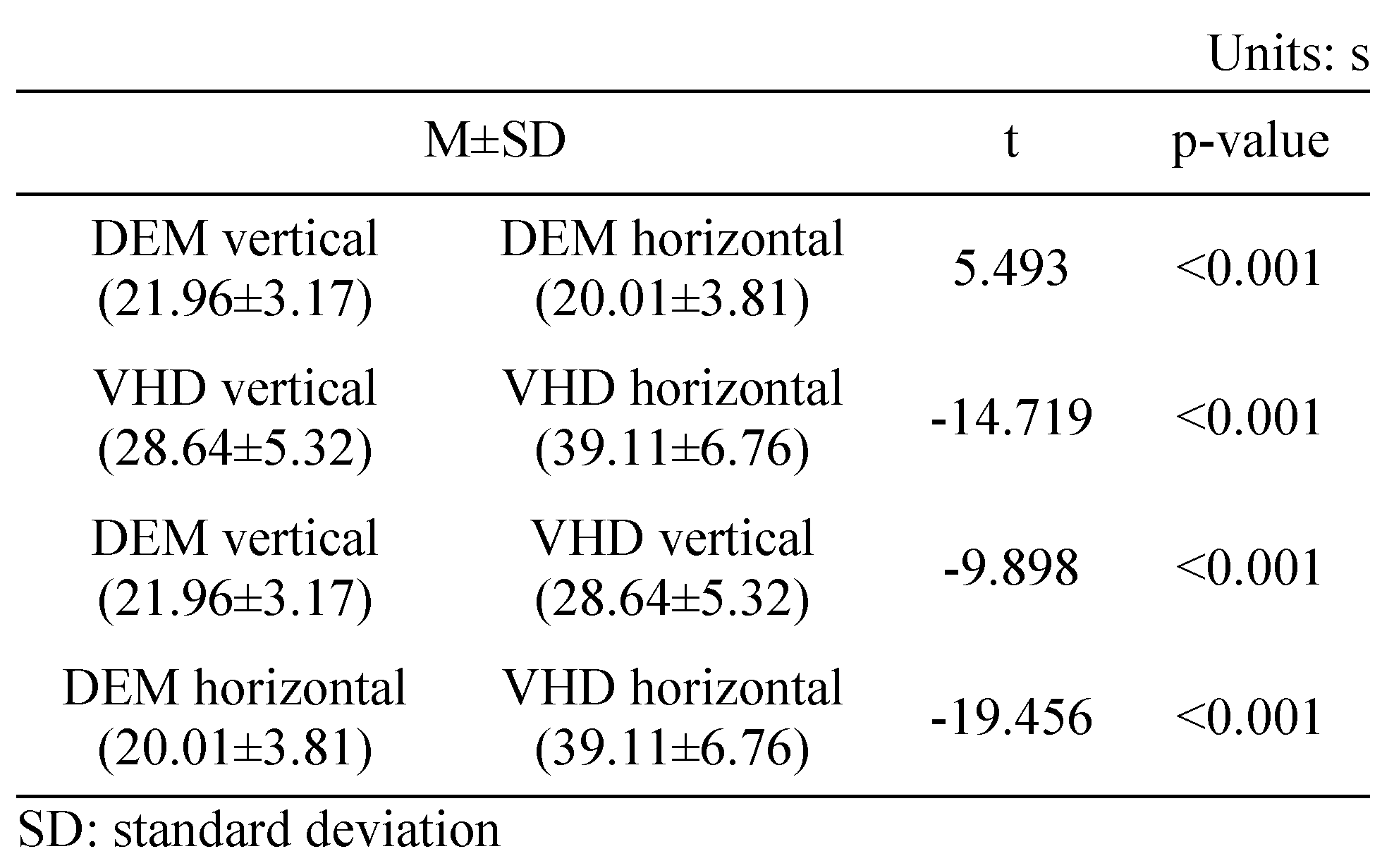
DEM
Comparison of DEM and VHD
Correlation analysis of DEM and VHD
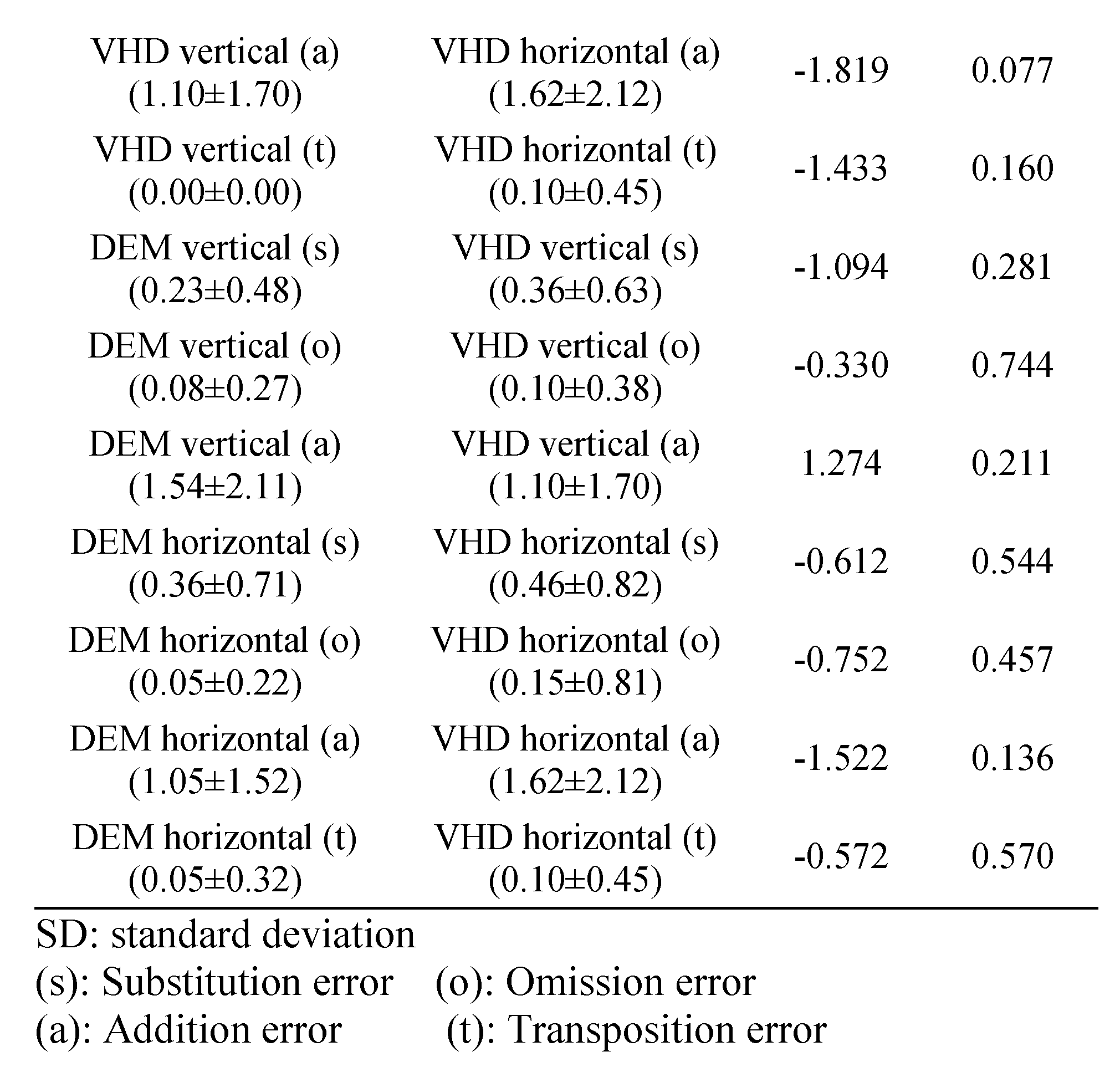
Error frequency comparison of each type between DEM and VHD
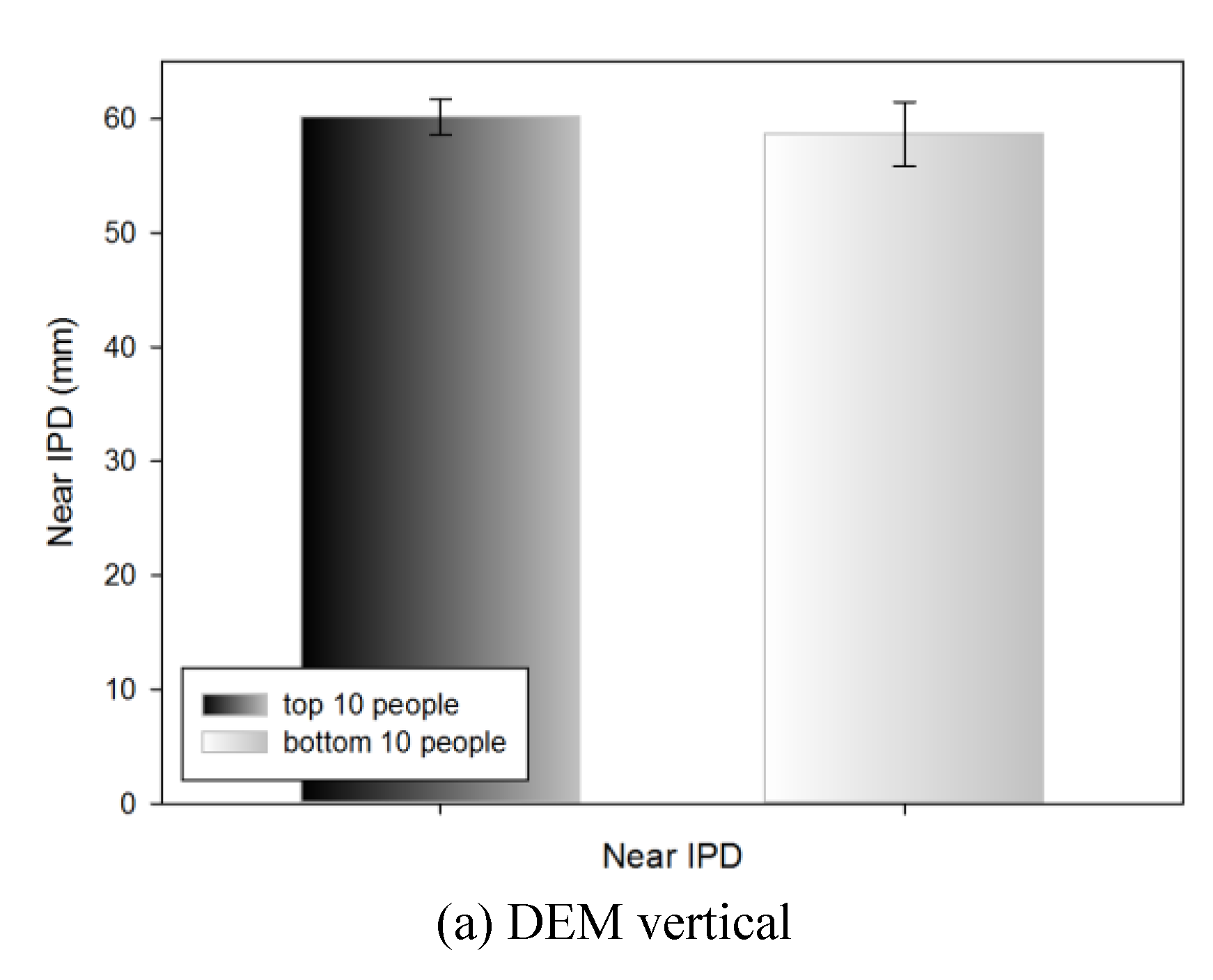
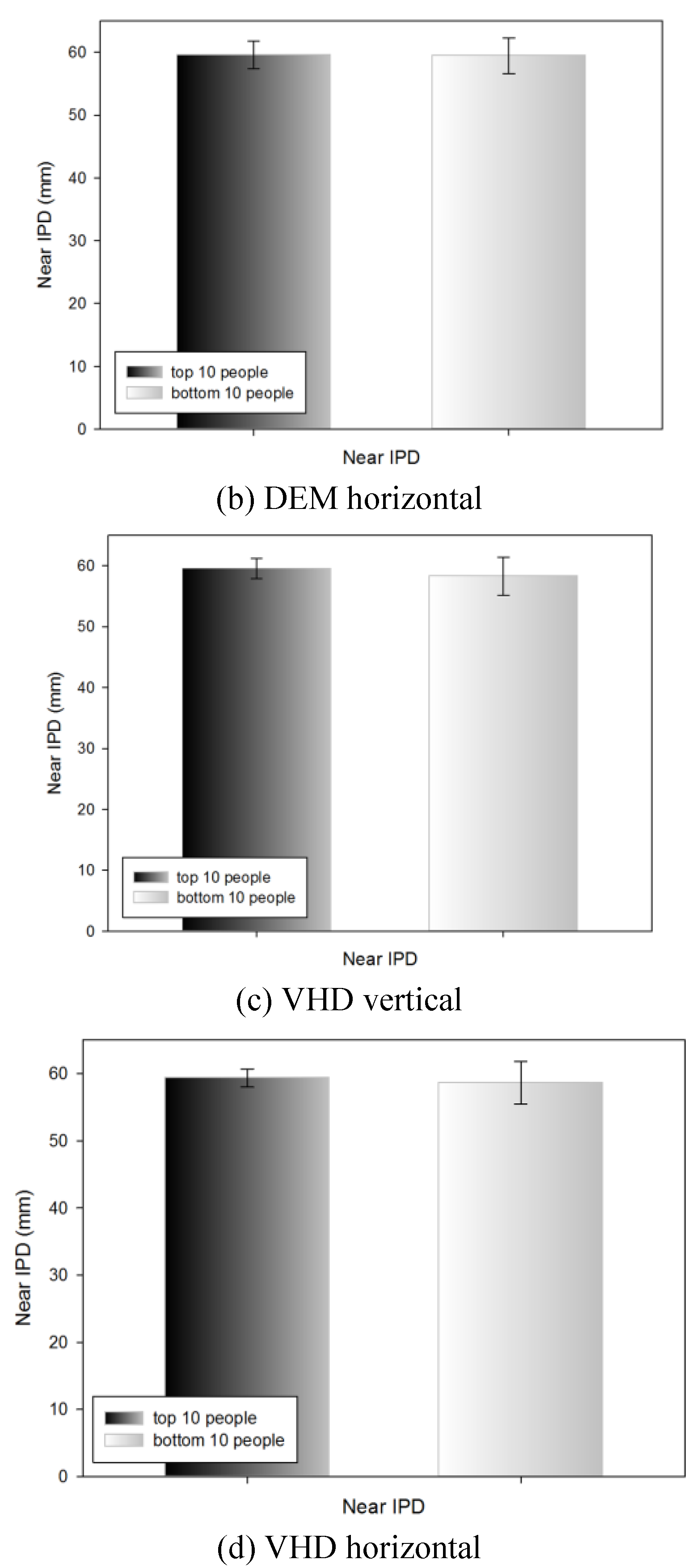
Near IPD of the top 10 and bottom 10 people by DEM and VHD test
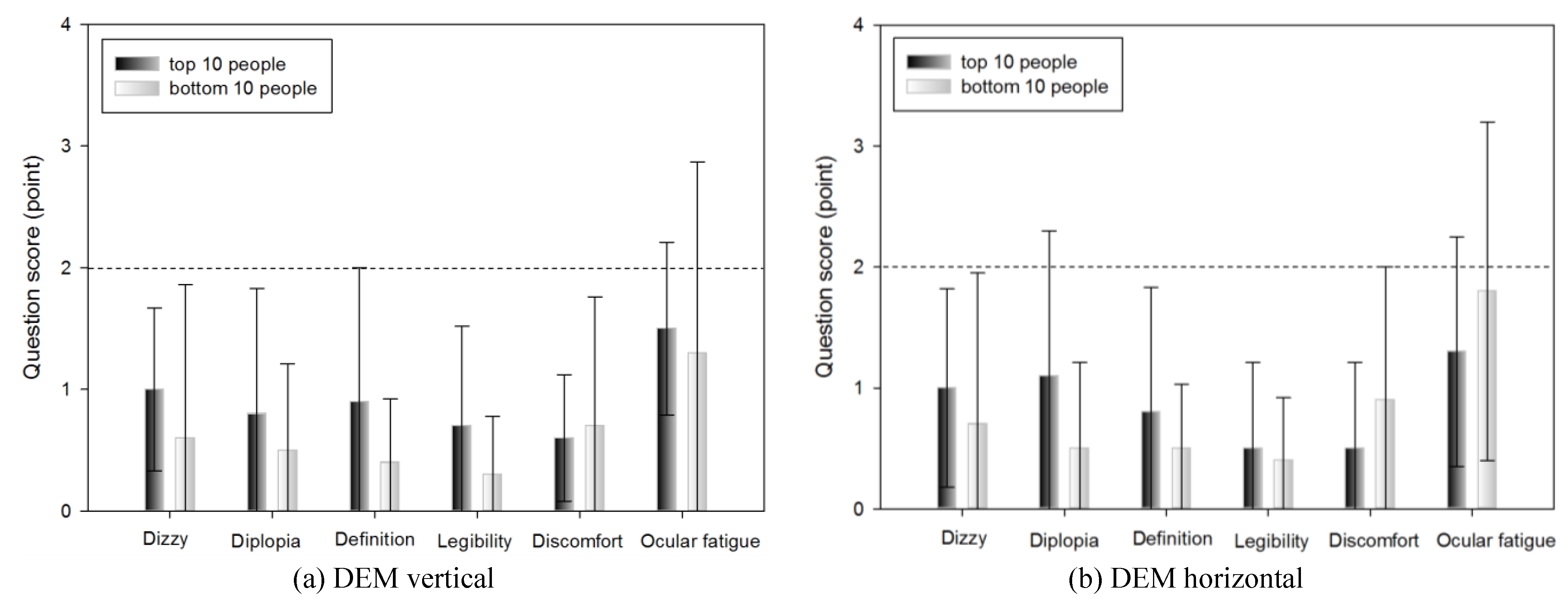
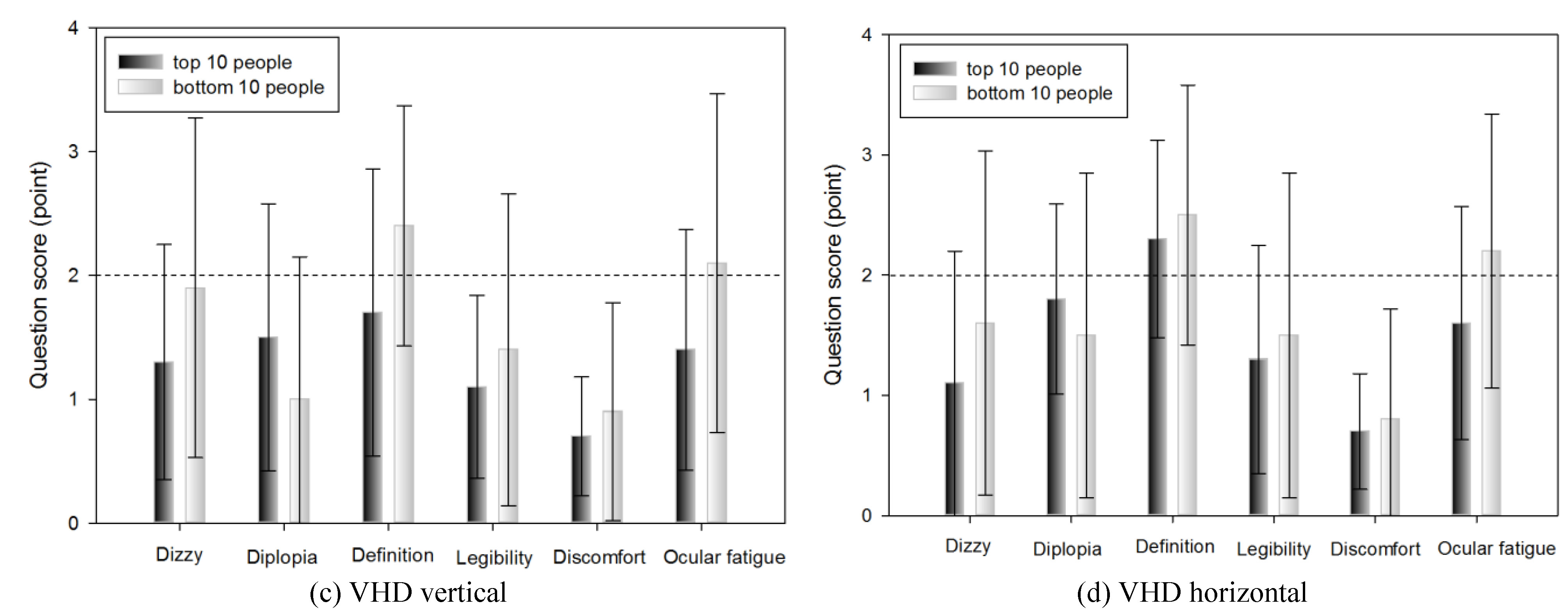
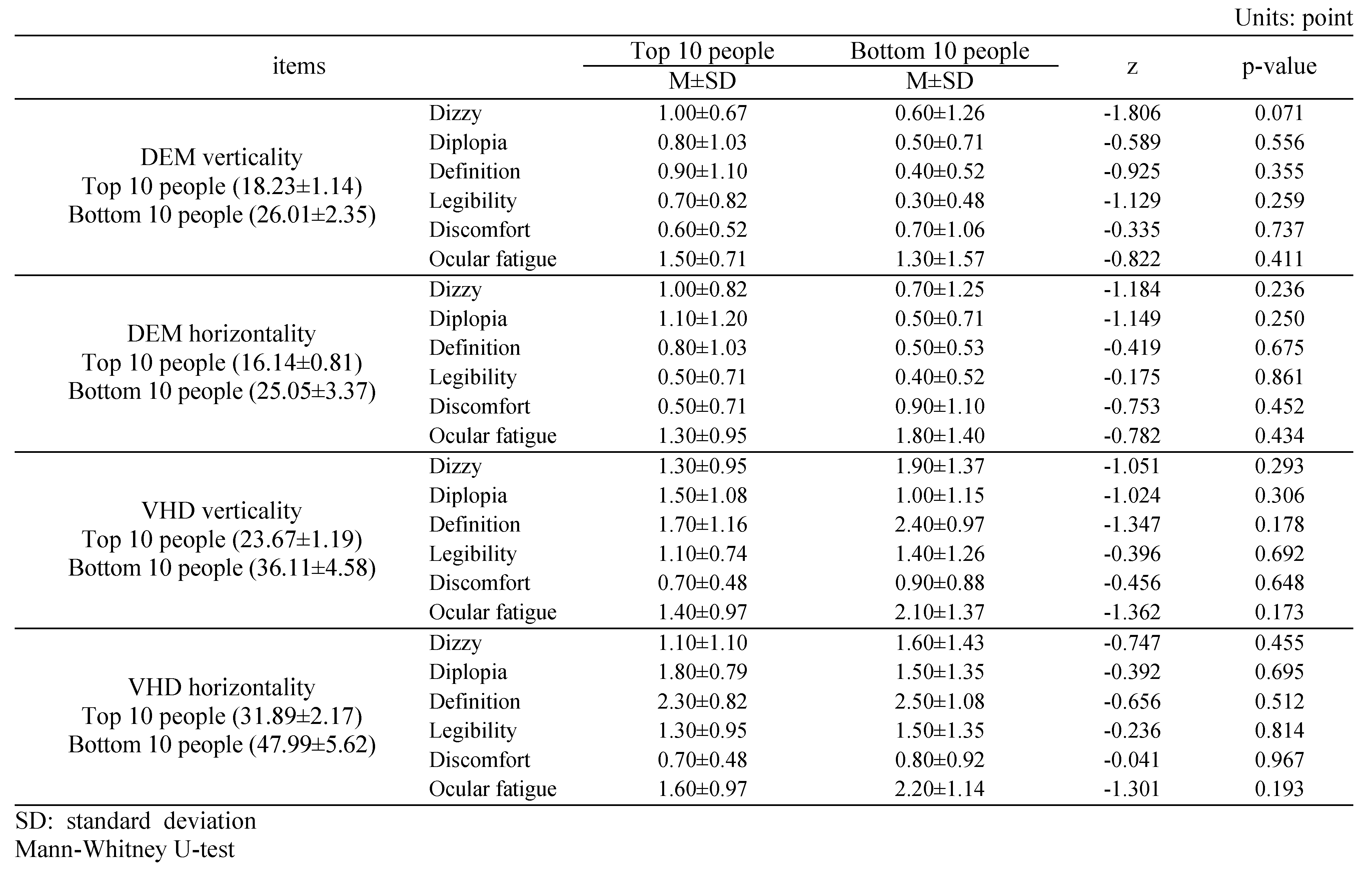
Subjective symptoms of the top 10 and bottom 10 people in DEM and VHD tests
Discussion
Acknowledgments
References
- Akinori, U., O. Yuji, and U. Yoshinori. 2006. A noncontact measurement of saccadic eye movement with two high-speed cameras. Proceedings of the 28th IEEE EMBS Annual International Conference 1: 5583–5586. [Google Scholar]
- Alessio, F., M. Silvio, and C. Tony. 2011. Validity reassessment of developmental eye movement (DEM) test in the Italian population. Optometry and Vision Development 42, 3: 155–167. [Google Scholar]
- Atchison, D. A., G. Smith, and N. Efron. 1979. The effect of pupil size on visual acuity in uncorrected and corrected myopia. American Journal of Optometry and Physiological Optics 56, 5: 315–323. [Google Scholar] [CrossRef]
- Ayton, L. N., L. A. Abel, T. R. Fricks, and N. A. McBrien. 2009. Developmental eye movement test: what is it really measuring? Optometry and Vision Science 86, 6: 722–730. [Google Scholar] [CrossRef]
- Bebguigui, N., and H. Ripoll. 1998. Effects of tennis practice in the coincidence timing accuracy of adults and children. Research Quarterly for Exercise and Sport 69: 217–223. [Google Scholar] [CrossRef]
- Berman, A. M. 1993. Clinical evaluation of the athlete. Optometry Clinics 3, 1: 1–26. [Google Scholar]
- Campbell, F. W., and D. G. Green. 1965. Optical and retinal factors affecting visual resolution. Journal of Physiology 181, 3: 576–593. [Google Scholar] [CrossRef]
- Coffey, B., and A. W. Reichow. 1990. Optometric evaluation of the elite athletes: the pacific sports visual performance profile. Problems in Optometry 1, 2: 32–58. [Google Scholar]
- Eugene, H. 2001. Optics, 4th edition. Addison Wesley: Reading, Ma. [Google Scholar]
- Gardner, J. J., and A. Sherman. 1995. Edited by DFC Loran and CJ MacEwan. Vision requirements in sport. In Sports Vision. Butterworth-Heinemann: London. [Google Scholar]
- Graham, B. E. 2007. Sports Vision: Vision care for the enhancement of sports performance. London: Butterworth-Heinemann. [Google Scholar]
- Hoffman, L. G., M. W. Rouse, and J. B. Ryan. 1981. Dynamic visual acuity: a review. Journal of the American Optometric Association 52: 883–887. [Google Scholar]
- Janet, M. P., M. Y. Fan, J. K. Pamela, T. B. Andrea, and R. Jack. 2006. A Comparison of the Developmental Eye Movement Test (DEM) and a Modified Version of the Adult Developmental Eye Movements Test (ADEM) with Older Adults. Journal of Behavioral Optometry 17, 3: 59–64. [Google Scholar]
- Janet, M. P., B. Kimberly, H. C. Emily, and A. C. Marcia. 2005. The need for adult norms on the developmental eye movement test (dem). Journal of Behavioral Optometry 16, 2: 38–41. [Google Scholar]
- Jason, J. 2015. The VR Book: Human-Centered Design for Virtual Reality. In ACM BOOKS, 1st Ed. ed. pp. 85–109. [Google Scholar]
- Joanne, M. W., and A. Bruce. 1997. An assessment of the Efficacy of sports vision training programs. Optometry and vision science 74, 8: 646–659. [Google Scholar]
- Kim, H. M. 2007. A Study on the Characteristics in Multi-sensory Communication Channel of Visual Information classified by the Human Senses. Korea Society of Basic Design & Art 8, 4: 801–811. [Google Scholar]
- Kim, J. H., K. N. Lee, and I. H. Ra. 2002. New Image Editor based on Combination of Bitmap and Vector Method. Journal of Korea Institute of Information and Communication Engineering 6, 2: 288–293. [Google Scholar]
- Kim, T. Y., S. H. Ryu, and Y. J. Hur. 2004. Research about CAVE Practical Use Way Through Culture Content’s Restoration Process that Utilize CAVE. Journal of Korea Game Society 4, 3: 11–20. [Google Scholar]
- Kim, Y. H., and Y. B. Lee. 2002. A study of improve vectorising technique on the internet. Journal of Korea Institute of Information and Communication Engineering 6, 2: 271–281. [Google Scholar]
- Kulp, M. T., and P. P. Schmidt. 1997. The relation of clinical saccadic eye movement testing to reading in kindergartners and first graders. Optometry and Vision Science 74, 1: 37–42. [Google Scholar]
- Kulp, M. T., and P. P. Schmidt. 1998. Relationship between visual skills and performance on saccadic eye movement testing. Optometry and Vision Science 75, 4: 284–287. [Google Scholar] [CrossRef]
- Kuppers, H. 1992. Schule der Farben: Grundzüge der Farbentheorie fur Computeranwender und andere. Köln: DuMont.
- Lee, M. A., J. M. Oh, and J. H. Jeong. 2010. The Effects of Sports Vision Training on Baseball Player’s Visual Performance and Base ball Records. Journal of Korean Ophthalmic Optics Society 15, 1: 87–97. [Google Scholar]
- Lee, M. H., and J. H. Sin. 2005. A Study on the Measurement of Dynamic Visual Acuity for Visual Acuity Chart Size. Korean Journal of Vision Science 7, 1: 129–133. [Google Scholar]
- Lee, M. H., K. C. Mah, and C. H. Won. 2000. A Studyon the Measurement of Dynamic Visual Acuity for Athletes and Nonathletes. Korean Journal of Vision Science 2, 1: 1–6. [Google Scholar]
- Lee, S. H., G. T. Ha, J. K. Cha, J. H. Kim, H. J. Lee, and S. H. Kim. 2015. CyberTouch—Touch and Cursor Interface for VR HMD. COMMUNICATIONS IN COMPUTER AND INFORMATION SCIENCE 528: 503–507. [Google Scholar]
- Maples, W. C., R. S. Savoy, B. J. Harville, L. R. Golden, and R. Hoenes. 2009. Comparison of Distance and Near Heterophoria by Two Clinical Methods. Optometry and Vision Development 40, 2: 100–106. [Google Scholar]
- Medland, C., H. Walter, and J. M. Woodhouse. 2010. Eye movements and poor reading: does the Developmental Eye Movement test measure cause or effect? Ophthalmic and Physiological Optics 30, 6: 740–747. [Google Scholar]
- Michael, S., G. Steve, E. Martin, E. Elmar, and M. Marcus. 2015. An Affordable Solution for Binocular Eye Tracking and Calibration in Head-mounted Displays. Proceedings of ACM Multimedia 2015. [Google Scholar]
- Mitsuru, N., T. Minoru, and K. Daisuke. 2005. Effects of aging and regular exercise on the visual function. Juntendo Medical Journal 51, 2: 153–159. [Google Scholar]
- Palter, S. F., O. Sobko-Koziupa, T. Gilhuly, and C. Pyer. 2000. Use of a Head Mounted Display (HMD) Virtual Reality (VR) Headset as a Patient Distraction Device for Surgical Procedures Under Local Anesthesia/Sedation. Fertility and sterility 74, 3: s203. [Google Scholar]
- Rizzo, A., A. Hartholt, M. Grimani, A. Leeds, and M. Liewer. 2014. Virtual Reality Exposure Therapy for Combat-Related Posttraumatic Stress Disorder. IEEE Computer Society 47, 7: 31–37. [Google Scholar]
- Schuemie, M. J., P. van der Straaten, M. Krijn, and C.A. van der Mast. 2001. Research on Presence in Virtual Reality: A Survey. CyberPsychology and Behavior 4, 2: 183–201. [Google Scholar]
- Sebastian, S., and M. Daniel. 2012. The impact of a sports vision training program in youth field hockey players. Journal of Sports Science and Medicine 11, 4: 624–631. [Google Scholar]
- Thomas, A. W., and F. Jeff. 2004. Sports Vision: Training for better performance. Human Kinetics 85. [Google Scholar]
- Webber, A., J. Wood, G. Gole, and B. Brown. 2011. DEM test, visagraph eye movement recordings, and reading ability in children. Optometry and Vision Science 88, 2: 295–302. [Google Scholar] [PubMed]
- WIKIPEDIA. Lens(optics). Available online: https://en.wikipedia.org/wiki/Lens_(optics).
- William, J. B. 2006. Borish’s Clinical Refraction. In BUTTERWORTH HEINEMANN, 2nd Ed. ed. pp. 217–246. [Google Scholar]
- Wills, J., R. Gillett, E. Eastwell, R. Abraham, K. Coffey, A. Webber, and J. Wood. 2012. Effect of simulated astigmatic refractive error on reading performance in the young. Optometry and Vision Science 89, 3: 271–276. [Google Scholar] [PubMed]
- Won, C. H., and K. C. Mah. 1993. Sports Vision Training. In DAIHAKS, 1st Ed. ed. pp. 23–24. [Google Scholar]
- Yamaguchi, C., K. Hasebe, S. Ohkubo, M. Takaba, Y. Sira, S. Hasebe, and H. Ohtsuki. 2012. Measurement of the AC/A Ratio Using Howell Phoria Card. Japanese Orthoptic Journal 41: 83–87. [Google Scholar]
- Yoshimitsu, K., and Y. Hiroshi. 2004. Training effects of visual function on college baseball players. Human Performance Measurement 1: 15–23. [Google Scholar]
- Zhao, Q. L., Z. Q. Wang, H. Q. Guo, Q. Sun, and Z. W. Lu. 2004. Head-mounted display with LCOS using diffractive optical element. Optik 115, 1: 11–14. [Google Scholar]






Copyright © 2016. This article is licensed under a Creative Commons Attribution 4.0 International License.
Share and Cite
Kim, J.-H.; Son, H.-J.; Lee, S.-J.; Yun, D.-Y.; Kwon, S.-C.; Lee, S.-H. Effectiveness of a Virtual Reality Head-Mounted Display System-Based Developmental Eye Movement Test. J. Eye Mov. Res. 2016, 9, 1-14. https://doi.org/10.16910/jemr.9.6.4
Kim J-H, Son H-J, Lee S-J, Yun D-Y, Kwon S-C, Lee S-H. Effectiveness of a Virtual Reality Head-Mounted Display System-Based Developmental Eye Movement Test. Journal of Eye Movement Research. 2016; 9(6):1-14. https://doi.org/10.16910/jemr.9.6.4
Chicago/Turabian StyleKim, Jung-Ho, Ho-Jun Son, Sung-Jin Lee, Deok-Young Yun, Soon-Chul Kwon, and Seung-Hyun Lee. 2016. "Effectiveness of a Virtual Reality Head-Mounted Display System-Based Developmental Eye Movement Test" Journal of Eye Movement Research 9, no. 6: 1-14. https://doi.org/10.16910/jemr.9.6.4
APA StyleKim, J.-H., Son, H.-J., Lee, S.-J., Yun, D.-Y., Kwon, S.-C., & Lee, S.-H. (2016). Effectiveness of a Virtual Reality Head-Mounted Display System-Based Developmental Eye Movement Test. Journal of Eye Movement Research, 9(6), 1-14. https://doi.org/10.16910/jemr.9.6.4




