The Effect of Target Speed and Verbal Instruction on NPC Measures in a Young, Healthy, and Active Population
Abstract
:Introduction
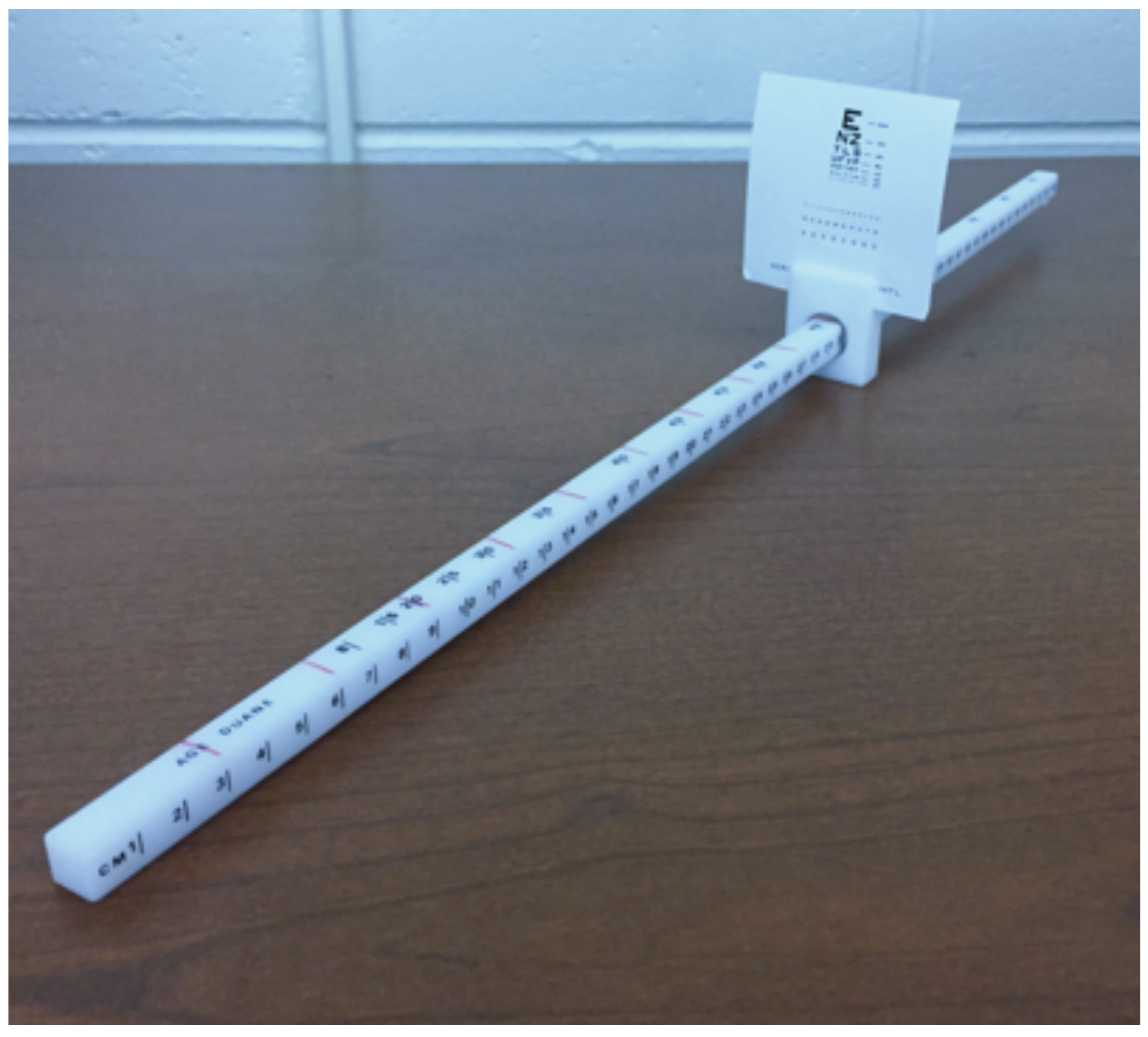
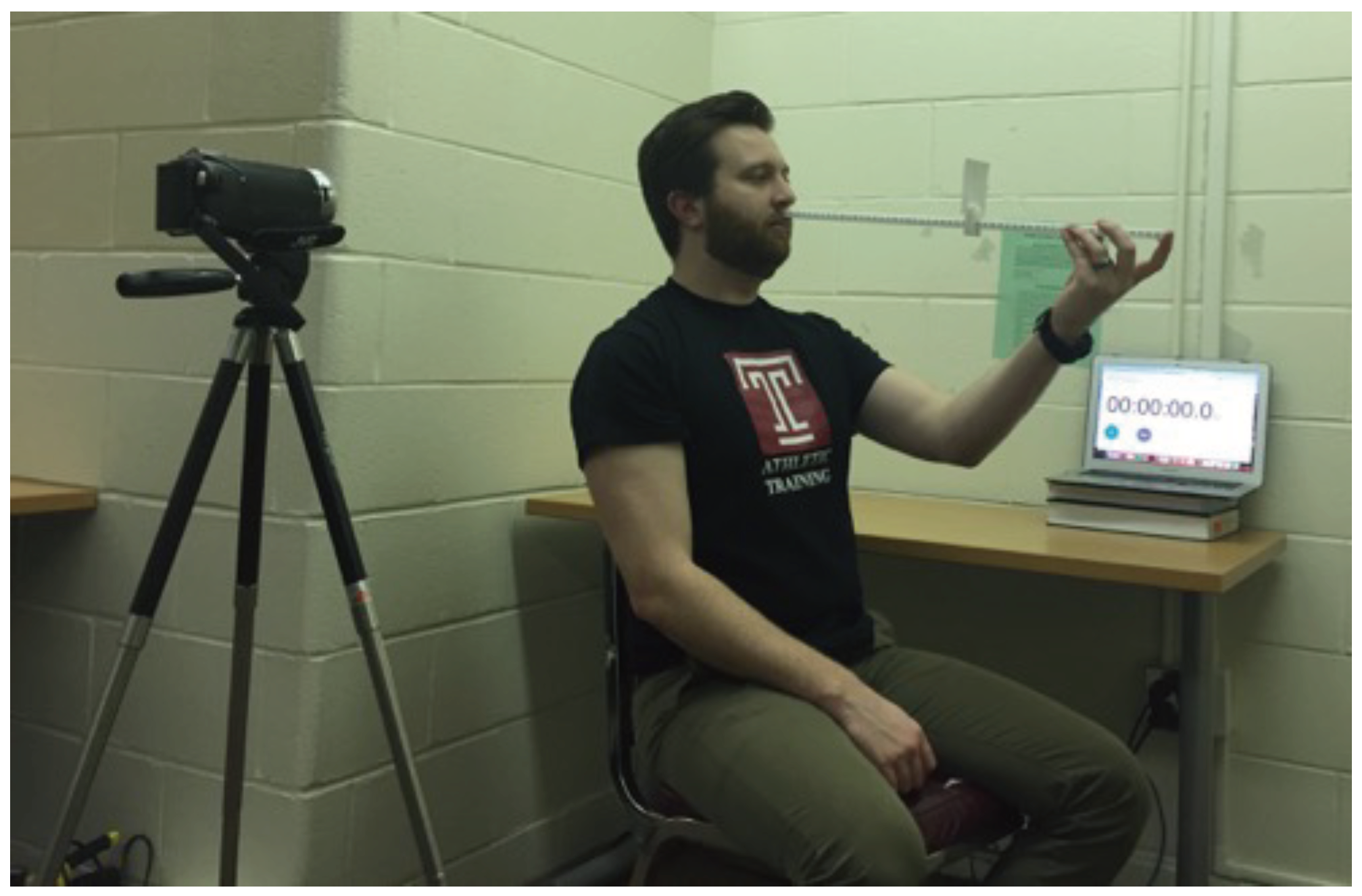
Materials & Methods
Participants
Results
Discussion
Ethics and Conflict of Interest
References
- Adler, P. M., M. Cregg, A. Viollier, and J. M. Woodhouse. 2007. Influence of target type and RAF rule on the measurement of near point of convergence. Opthalmic & Physiologic Optics 27, 1: 22–30. [Google Scholar]
- Anzalone, A. J., D. Blueitt, T. Case, T. McGuffin, K. Pollard, J. C. Garrison, and J. M. Oliver. 2016. A positive Vestibular/Ocular Motor Screening (VOMS) is associated with increased recovery time after sports-related concussion. The American Journal of Sports Medicine 45, 2: 474–479. [Google Scholar] [CrossRef] [PubMed]
- Broglio, S. P., R. C. Cantu, G. A. Gioia, K. M. Guskiewicz, J. Kutcher, M. Palm, and T. C. Valovich McLeod. 2014. National Athletic Trainers’ Association position statement: Management of sport concussion. Journal of Athletic Training 49, 2: 245–265. [Google Scholar] [CrossRef]
- Capó-Aponte, J. E., T. G. Urosevich, L. A. Temme, A. K. Tarbett, and N. K. Sanghera. 2012. Visual dysfunctions and symptoms during the subacute stage of blast induced mild traumatic brain injury. Military Medicine 177, 7: 804–813. [Google Scholar] [CrossRef] [PubMed]
- Capó-Aponte, J. E., T. A. Beltran, D. V. Walsh, and W. R. Cole. 2018. Validation of visual objective biomarkers for acute concussion. Military Medicine 183, 4: 9–17. [Google Scholar] [CrossRef]
- Collins, M. W., A. P. Kontos, E. Reynolds, C. D. Murawski, and F. H. Fu. 2014. A comprehensive, targeted approach to the clinical care of athletes following sport-related concussion. Knee Surgery, Sports Traumatology, Arthroscopy 22, 2: 235–246. [Google Scholar] [CrossRef]
- Cooper, J., and N. Jamal. 2012. Convergence insufficiency–A major review. Optometry 83, 4: 137–158. [Google Scholar]
- Corwin, D. J., M. R. Zonfrillo, C. L. Master, K. B. Arbogast, M. F. Grady, R. L. Robinson, and D. J. Wiebe. 2014. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. Journal of Pediatrics 165, 6: 1207–1215. [Google Scholar] [CrossRef]
- DuPrey, K., A. Webner, A. Lyons, C. H. Kucuk, J. T. Ellis, and P. F. Cronholm. 2017. Convergence insufficiency identifies athletes at risk of prolonged recovery from sport-related concussion. The American Journal of Sports Medicine 45, 10: 2388–2393. [Google Scholar] [CrossRef]
- Ellis, M. J., D. Cordingley, S. Vis, K. Reimer, J. Leiter, and K. Russell. 2015. Vestibulo-ocular dysfunction in pediatric sports-related concussion. Journal of Neurosurgery: Pediatrics 16: 248–255. [Google Scholar] [CrossRef]
- Ellis, M. J., D. Cordingley, S. Vis, K. Reimer, J. Leiter, and K. Russell. 2017. Clinical predictors of vestibularocular dysfunction in pediatric sports-related concussion. Journal or Neurosurgery: Pediatrics 19: 36–45. [Google Scholar]
- Gessel, L. M., S. K. Fields, C. L. Collins, R. W. Dick, and R. D. Comstock. 2007. Concussions among United States high school and collegiate athletics. Journal of Athletic Training 42, 4: 495–503. [Google Scholar]
- Haines, D. 2006. Fundamental neuroscience for basic and clinical applications. Elsevier: Philadelphia, PA. [Google Scholar]
- Harmon, K. G., J. Drezner, M. Gammons, K. Guskiewicz, M. Halstead, S. Herring, and W. Roberts. 2013. American Medical Society for Sports Medicine position statement: Concussion in sport. Clinical Journal of Sports Medicine 23, 1: 1–18. [Google Scholar] [CrossRef]
- Hayes, G., B. Cohen, M. Rouse, and P. N. De Land. 1998. Normative values for the nearpoint of convergence of elementary school children. Optometry and Vision Science 75, 7: 506–512. [Google Scholar] [CrossRef] [PubMed]
- Hellerstein, L. F., S. Freed, and W. C. Maples. 1995. Vision profile of patients with mild brain injury. Journal of the American Optometric Association 66, 10: 632–639. [Google Scholar]
- Howell, D., M. O’Brien, A. Raghuram, A. S. Shah, and W. P. Meehan. 2017. Near point of convergence and gait deficits in adolescents after sport-related concussion. Clinical Journal of Sports Medicine 28, 3: 262–267. [Google Scholar] [CrossRef]
- Kawata, K., R. Tierney, J. Phillips, and J. Jeka. 2016. Effect of repetitive sub-concussive head impacts on ocular near point of convergence. International Journal of Sports Medicine 37, 5: 405–410. [Google Scholar] [CrossRef]
- Lavrich, J. B. 2010. Convergence insufficiency and its current treatment. Current Opinion in Ophthamology 21: 356–360. [Google Scholar] [CrossRef]
- Master, C. L., M. Scheiman, M. Gallaway, A. Goodman, R. L. Robinson, S. R. Master, and M. F. Grady. 2016. Vision diagnoses are common after concussion in adolescents. Clinical Pediatrics 55, 3: 260–267. [Google Scholar] [CrossRef]
- Master, C. L., S. R. Master, D. J. Wiebe, E. P. Storey, E. E. Lockyer, O. E. Podolak, and M. F. Grady. 2017. Vision and vestibular system dysfunction predicts prolonged concussion recovery in children. Clinical Journal of Sports Medicine 0: 1–7. [Google Scholar] [CrossRef]
- McRory, P., W. Meeuwisse, J. Dvorak, M. Aubry, J. Bailes, S. Broglio, and P. E. Vos. 2017. Consensus statement on concussion in sport–The 5th international conference on concussion in sport held in Berlin, October, 2016. British Journal of Sports Medicine 51, 11: 838–847. [Google Scholar] [CrossRef] [PubMed]
- McDevitt, J., K. O. Appiah-Kubi, R. Tierney, and W. G. Wright. 2016. Vestibular and oculomotor assessments may increase accuracy of subacute concussion assessment. International Journal of Sports Medicine 37: 738–747. [Google Scholar] [CrossRef]
- Mucha, A., M. W. Collins, R. J. Elbin, J. M. Furman, C. Troutman-Eneski, R. M. DeWolf, and A. P. Kontos. 2014. A brief Vestibular/Ocular Motor Screening (VOMS) assessment to evaluate concussions. The American Journal of Sports Medicine 42, 10: 2479–2486. [Google Scholar] [CrossRef] [PubMed]
- Patricios, J., G. W. Fuller, R. Ellenbogen, S. Herring, J. S. Kutcher, M. Loosemore, and K. J. Schneider. 2017. What are the critical elements of sideline screening that can be used to establish a diagnosis of concussion? A systematic review. British Journal of Sports Medicine 51, 11: 888–894. [Google Scholar] [CrossRef]
- Pearce, K. L., A. Sufrinko, B. C. Lau, L. Henry, M. W. Collins, and M. P. Kontos. 2016. Near point of convergence after sport-related concussion. The American Journal of Sports Medicine 34, 5: 352–359. [Google Scholar] [CrossRef]
- Phillips, J., and R. Tierney. 2015. Effect of target type on near point of convergence in a healthy, active, young adult population. Journal of Eye Movement Research 8, 3: 1–6. [Google Scholar] [CrossRef]
- Rouse, M. W., E. Borsting, and P. N. DeLand. 2002. Reliability of binocular vision measurements used in the classification of convergence insufficiency. Optometry and Vision Science 79, 4: 254–264. [Google Scholar] [CrossRef]
- Scheiman, M., M. Gallaway, K. A. Frantz, R. J. Peters, S. Hatch, M. Cuff, and G. L. Mitchell. 2003. Near-point of convergence: Test procedure, target selection, and normative data. Optometry and Vision Science 80, 3: 214–225. [Google Scholar] [CrossRef]
- Siderov, J., S. C. Chiu, and S. J. Waugh. 2001. Differences in the nearpoint of convergence with target type. Opthalmic and Physiological Optics 21, 5: 356–360. [Google Scholar] [CrossRef]
- Storey, E. P., S. R. Master, J. E. Lockyer, O. E. Podolak, M. F. Grady, and C. L. Master. 2017. Near point of convergence after concussion in children. Optometry and Vision Science 94, 1: 96–100. [Google Scholar] [CrossRef]
- Szymanowicz, D., K. J. Ciuffreda, P. Thiagarajan, D. P. Ludlam, W. Green, and N. Kapoor. 2012. Vergence in mild traumatic brain injury: A pilot study. The Journal of Rehabilitation Research and Development 49, 7: 1083. [Google Scholar] [CrossRef] [PubMed]
- Temme, L. A., and A. Morris. 1988. Speed of accommodation and age. Optometry and Vision Science 66, 2: 106–112. [Google Scholar] [CrossRef] [PubMed]
- Ventura, R. E., L. J. Balcer, and S. L. Galetta. 2014. The neuro-ophthalmology of head trauma. The Lancet Neurology 13: 1006–1016. [Google Scholar] [CrossRef] [PubMed]
- Ventura, E. R., J. M. Jancuska, L. J. Balcer, and S. L. Galetta. 2015. Diagnostic tests for concussion: Is vision part of the puzzle? Journal of Neuro-Ophthamology 35: 73–81. [Google Scholar] [CrossRef]
- Yorke, A. M., L. Smith, M. Babcock, and B. Alsalaheen. 2017. Validity and reliability of the Vestibular/Ocular Motor Screening and associations with common concussion screening tools. Sports Health 9, 2: 174–180. [Google Scholar] [CrossRef]
- Zuckerman, S. L., Z. Y. Kerr, A. Yengo-Kah, E. Wasserman, T. Covassin, and G. S. Colomon. 2015. Epidemiology of sports-related concussion in NCAA athletes from 2009-2010 to 2013-2014: Incidence, recurrence, and mechanisms. The American Journal of Sports Medicine 43, 11: 2654–2662. [Google Scholar] [CrossRef]
| Speed | N | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| 1 cm/s | 20 | 6.72 | 2.39 | 2.67 | 13.67 |
| 3 cm/s | 20 | 6.10 | 2.36 | 2.83 | 11.67 |
| 5 cm/s | 20 | 5.44 | 2.01 | 2.67 | 11.00 |
| Self-paced | 20 | 6.63 | 2.26 | 2.67 | 11.33 |
| 1 cm/s "blurry" | 20 | 10.82 | 3.08 | 6.67 | 20.33 |
| Pair | t | df | p |
|---|---|---|---|
| 1 cm/s - 3 cm/s | 1.69 | 19 | .108 |
| 1 cm/s - 5 cm/s | 3.47 | 19 | .003* |
| 1 cm/s - self-paced | 0.257 | 19 | .80 |
| 3 cm/s - 5 cm/s | 2.30 | 19 | .03* |
| 3 cm/s - self-paced | -1.24 | 19 | .23 |
| 5 cm/s - self paced | -3.19 | 19 | .005* |
| 1 cm/s - 1 cm/s "blurry" | -5.89 | 19 | <.001* |
Copyright © 2019. This article is licensed under a Creative Commons Attribution 4.0 International License.
Share and Cite
McGinnis, I.; Tierney, R.; Mansell, J.; Phillips, J. The Effect of Target Speed and Verbal Instruction on NPC Measures in a Young, Healthy, and Active Population. J. Eye Mov. Res. 2019, 12, 1-8. https://doi.org/10.16910/jemr.12.4.5
McGinnis I, Tierney R, Mansell J, Phillips J. The Effect of Target Speed and Verbal Instruction on NPC Measures in a Young, Healthy, and Active Population. Journal of Eye Movement Research. 2019; 12(4):1-8. https://doi.org/10.16910/jemr.12.4.5
Chicago/Turabian StyleMcGinnis, Ian, Ryan Tierney, Jamie Mansell, and Jacqueline Phillips. 2019. "The Effect of Target Speed and Verbal Instruction on NPC Measures in a Young, Healthy, and Active Population" Journal of Eye Movement Research 12, no. 4: 1-8. https://doi.org/10.16910/jemr.12.4.5
APA StyleMcGinnis, I., Tierney, R., Mansell, J., & Phillips, J. (2019). The Effect of Target Speed and Verbal Instruction on NPC Measures in a Young, Healthy, and Active Population. Journal of Eye Movement Research, 12(4), 1-8. https://doi.org/10.16910/jemr.12.4.5



