Limited Knowledge of Toxoplasmosis-Specific Preventive Behaviors in Pregnant Women: A Survey Study in Northern Italy
Abstract
1. Introduction
2. Materials and Methods
Statistics
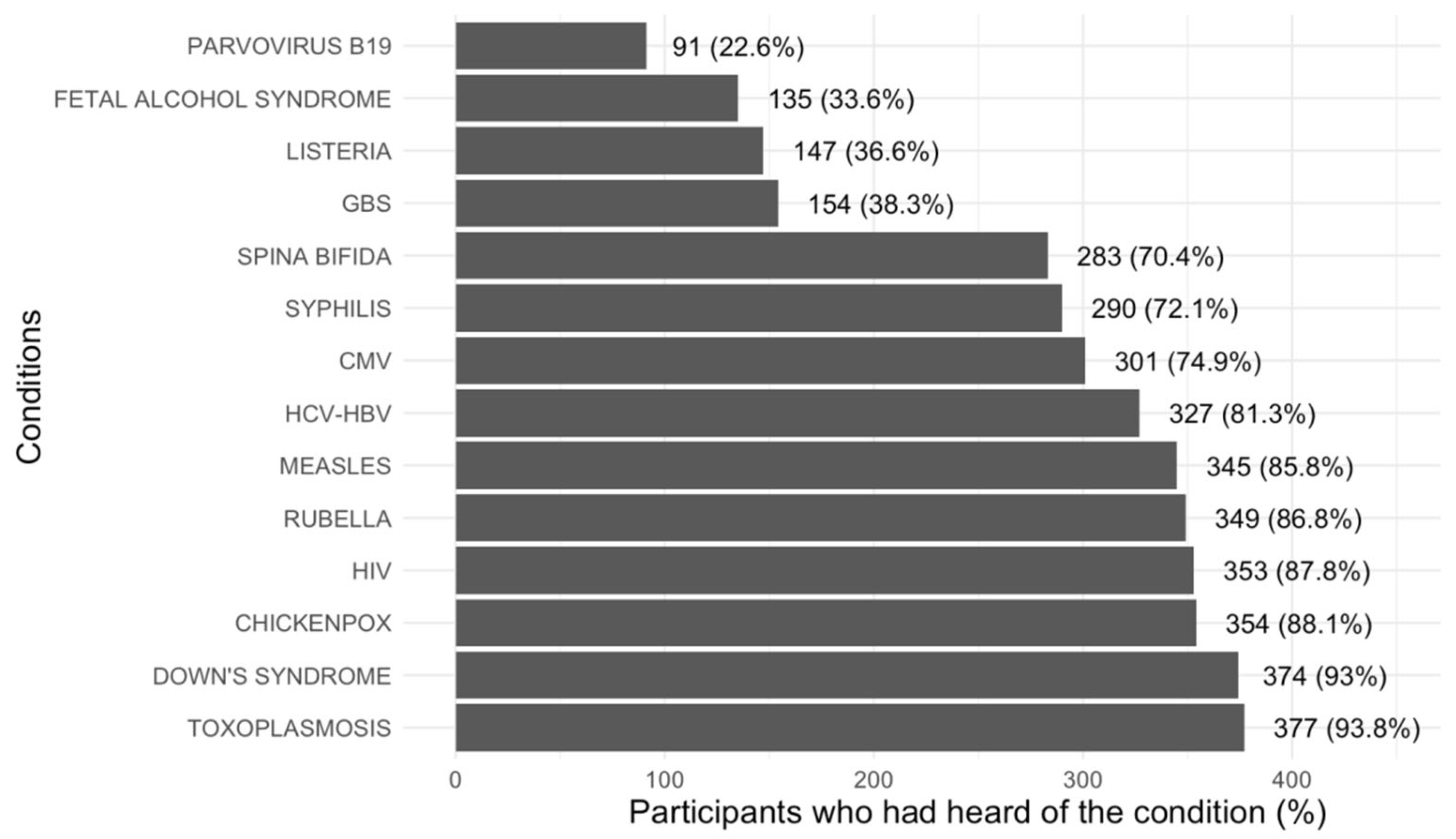
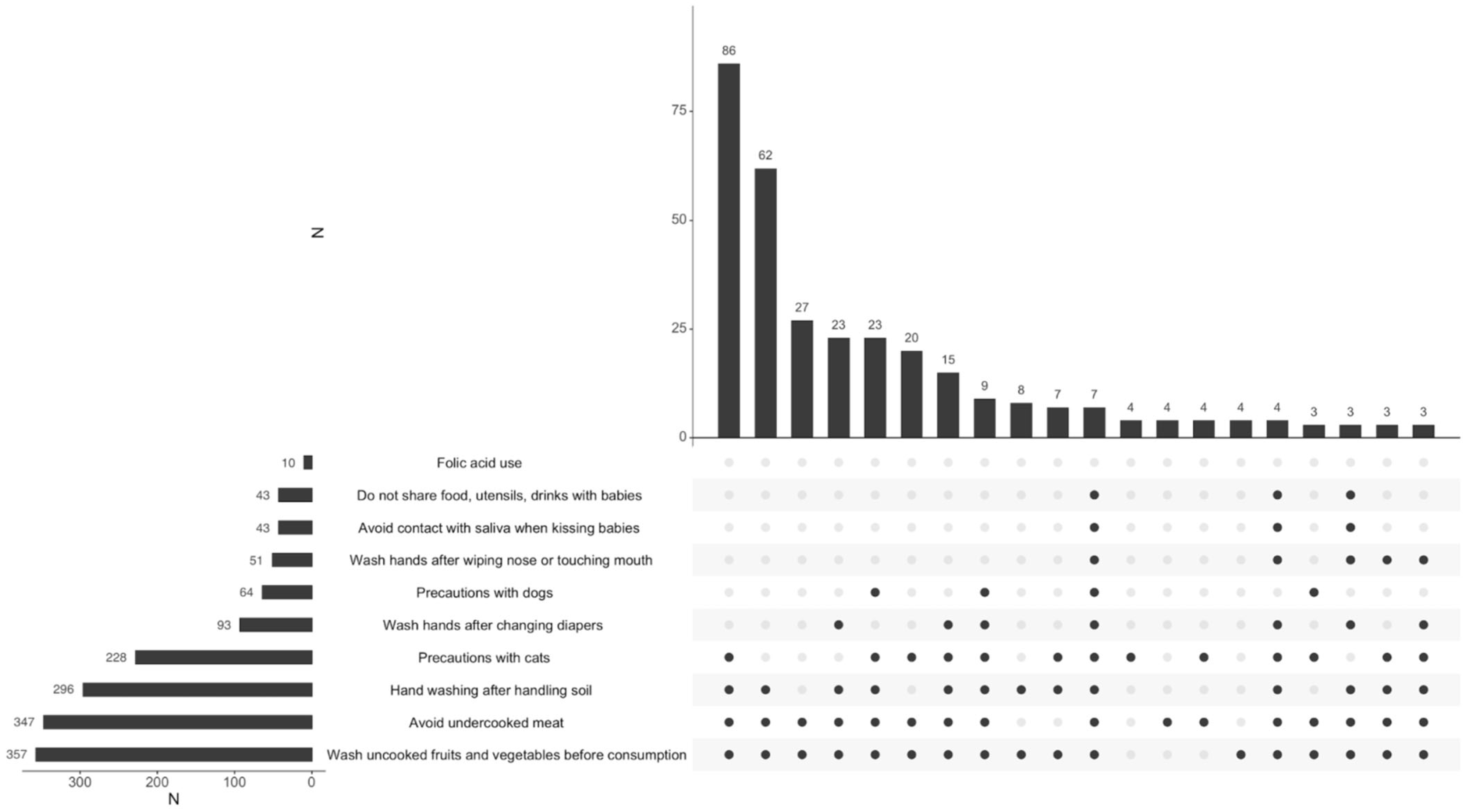
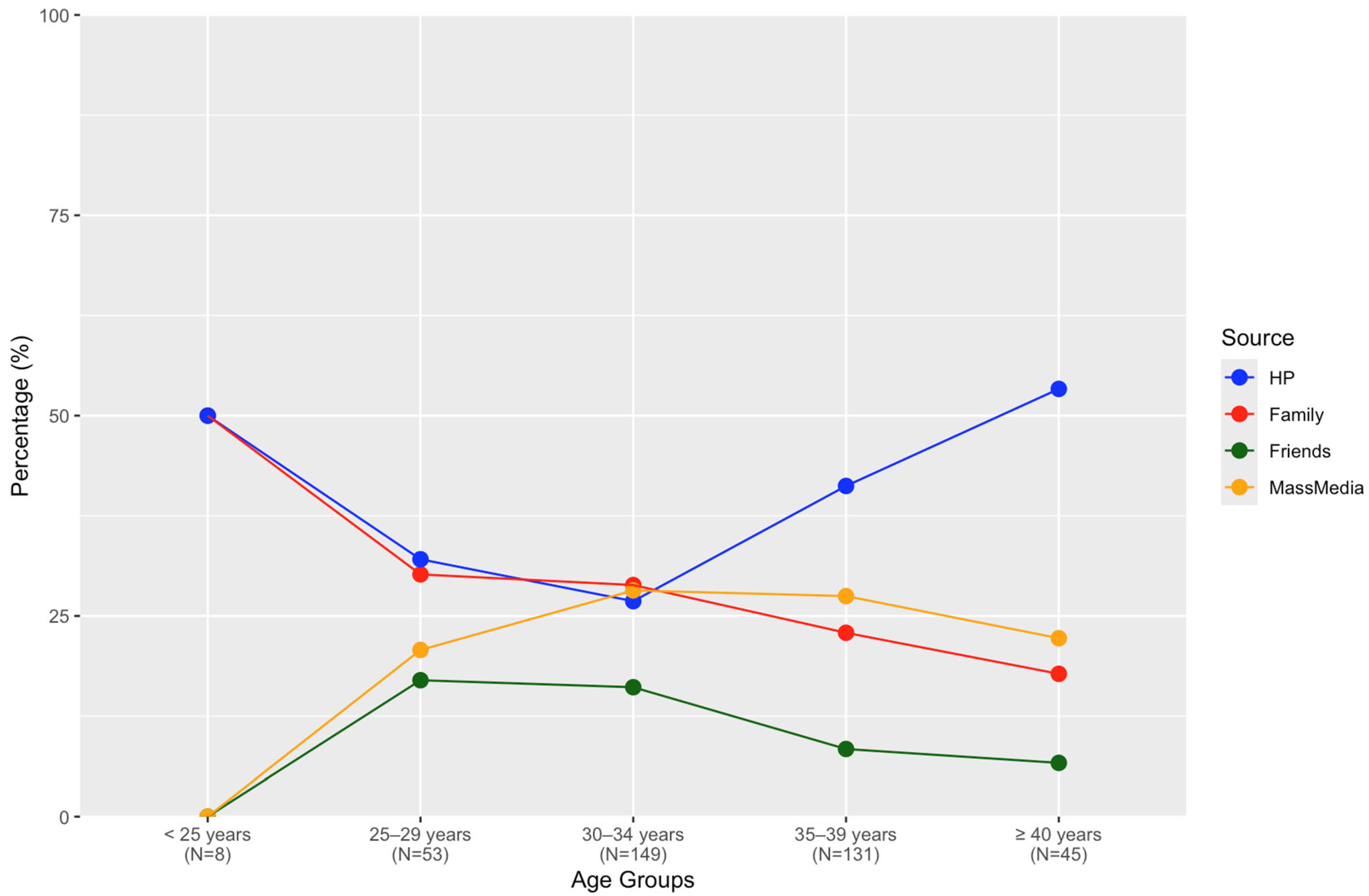
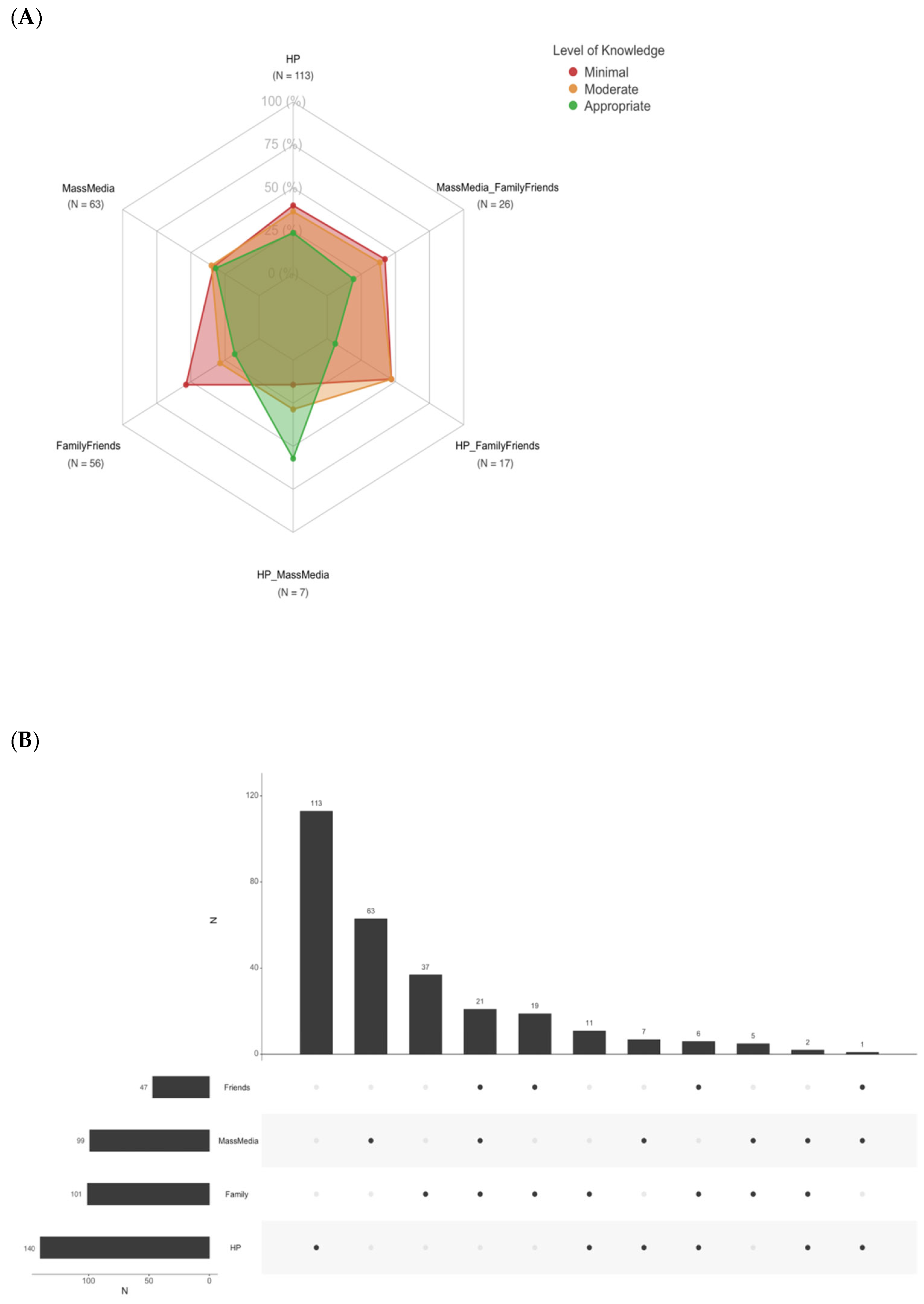
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Skariah, S.; McIntyre, M.K.; Mordue, D.G. Toxoplasmagondii: Determinants of tachyzoite to bradyzoite conversion. Parasitol. Res. 2010, 107, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Borges, M.; Silva, T.M.; Brito, C.; Teixeira, N.; Roberts, C.W. How does toxoplasmosis affect the maternal-foetal immune interface and pregnancy? Parasite Immunol. 2019, 41, e12606. [Google Scholar] [CrossRef] [PubMed]
- Torgerson, P.R.; Mastroiacovo, P. The global burden of congenital toxoplasmosis: A systematic review. Bull. World Health Organ. 2013, 91, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Bénard, A.; Petersen, E.; Salamon, R.; Chêne, G.; Gilbert, R.; Salmi, L.R.; European Toxo Prevention Study Grou. Survey of European programm es for the epidemiological surveillance of congenital toxoplasmosis. Eurosurveillance 2008, 13. [Google Scholar] [CrossRef]
- Barros, M.; Teixeira, D.; Vilanova, M.; Correia, A.; Teixeira, N.; Borges, M. Vaccines in Congenital Toxoplasmosis: Advances and Perspectives. Front. Immunol. 2021, 11, 621997. [Google Scholar] [CrossRef]
- Paquet, C.; Yudin, M.H. No. 285-Toxoplasmosisin Pregnancy: Prevention, Screening, and Treatment. J. Obstet. Gynaecol. Can. 2018, 40, e687–e693. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Antenatal Care for Uncomplicated Pregnancy. PARTONE. Section 1-Information for Pregnant Women. Section 2-Screening for Infections in Pregnancy. Linea Guida 1/2023 SNLG, 8, 248 (In Italian). Available online: https://www.epicentro.iss.it/itoss/pdf/LG-Gravidanza-Fisiologica-Parte1_protetto.pdf (accessed on 15 July 2024).
- Peyron, F.; L’ollivier, C.; Mandelbrot, L.; Wallon, M.; Piarroux, R.; Kieffer, F.; Hadjadj, E.; Paris, L.; Garcia-Meric, P. Maternal and Congenital Toxoplasmosis: Diagnosis and Treatment Recommendations of a French Multidisciplinary Working Group. Pathogens 2019, 8, 24. [Google Scholar] [CrossRef]
- Breugelmans, M.; Naessens, A.; Foulon, W. Prevention of toxoplasmosis during pregnancy—An epidemiologic survey over 22 consecutive years. J. Perinat. Med. 2004, 32, 211–214. [Google Scholar] [CrossRef]
- Foulon, W.; Naessens, A.; Ho-Yen, D. Prevention of congenital toxoplasmosis. J. Perinat. Med. 2000, 28, 337–345. [Google Scholar] [CrossRef]
- Smereka, J.; Szarpak, L.; Ruetzler, K.; Schacham, Y.; Smereka, A.; Dabrowski, M.; Terpilowska, M.; Terpilowski, L.; Adam, I. A multicenter survey on toxoplasmosis knowledgeamong pregnant women in Poland (the TOWER study). BMC Pregnancy Childbirth 2018, 18, 389. [Google Scholar] [CrossRef]
- Jones, J.L.; Ogunmodede, F.; Scheftel, J.; Kirkland, E.; Lopez, A.; Schulkin, J.; Lynfield, R. Toxoplasmosis-Related Knowledge and Practices Among Pregnant Women in the UnitedStates. Infect. Dis. Obstet. Gynecol. 2003, 11, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Pereboom, M.T.R.; Manniën, J.; Spelten, E.R.; Schellevis, F.G.; Hutton, E.K. Observation al study to assess pregnant women’s knowledge and behaviour to prevent toxoplasmosis, listeriosis and cytomegalovirus. BMC Pregnancy Childbirth 2013, 13, 98. [Google Scholar] [CrossRef] [PubMed]
- DeMoura, F.L.; Millar, P.R.; Fonseca, A.B.M.; Amendoeira, M.R.R. Congenital toxoplasmosis: The importance of implementing clinical practice guidelines. Sci. Med. 2017, 27, 25389. [Google Scholar] [CrossRef][Green Version]
- Willame, A.; Blanchard-Rohner, G.; Combescure, C.; Irion, O.; Posfay-Barbe, K.; DeTejada, B.M. Awareness of Cytomegalovirus Infection Among Pregnant Women in Geneva, Switzerland: A Cross-sectional Study. Int. J. Environ. Res. Public Health 2015, 12, 15285–15297. [Google Scholar] [CrossRef]
- Martini, A.; Pietrafesa, E.; Rondinone, B.M.; Iavicoli, S.; D’amelio, S.; Cavallero, S.; Bonafede, M. Toxoplasmosis and knowledge:What do the Italian women know about? Epidemiol. Infect. 2020, 148, e256. [Google Scholar] [CrossRef]
- Sample Size Calculator. Calculator. net. Available online: https://www.calculator.net/sample-size-calculator.html (accessed on 26 June 2024).
- CittadinieICT-Anno. 2022. Available online: https://www.istat.it/it/archivio/282257 (accessed on 15 July 2024).
- AMCLIETS. Percorso Diagnostico‘Infezionea Trasmissione Verticale TOXOPLASMAGONDII. rev.2023-08. Available online: https://www.amcli.it/documenti/percorsi-diagnostici/ (accessed on 30 June 2024).
- Angelici, M.C.; Buffolano, W.; Grandolfo, M.E.; Gramiccia, M.; Majori, G. Ilcontrollodella Toxoplasmosicongenitain Italia: Ilprogettodell’Istituto Superioredi Sanità. Ann. Ist. Super. Sanità 1999, 35, 329–333. [Google Scholar]
- ISS. Linee Guida della Gravidanzafisiologica, SNLG. Available online: https://www.salute.gov.it/new/ (accessed on 15 June 2024).
- Hamou, S.A.; Laboudi, M. Ananalytical study on the awareness and practice relating toxoplasmosis among pregnant women in Casablanca, Morocco. BMC Public Health 2021, 21, 507. [Google Scholar] [CrossRef]
- Baril, L.; Ancelle, T. Risk Factors for Toxoplasma Infection in Pregnancy: A Case-Control Study in France. Scand. J. Infect. Dis. 1999, 31, 305–309. [Google Scholar] [CrossRef]
- Thaller, R.; Tammaro, F.; Pentimalli, H. Risk factors for toxoplasmosis in pregnant women in central Italy. Infez. Med. 2011, 19, 241–247. [Google Scholar]
- Vasarri, M.V.; Fernicola, F.; Arienti, F.; Carli, A.; Colciago, E.; Locatelli, A.; Trotta, M.; Procopio, A.; Zammarchi, L.; Ornaghi, S. Indirect impact of SARS-CoV-2 pandemic onincidence of maternal primary cytomegalovirus and Toxoplasma gondii infection in pregnancy. Int. J. Gynecol. Obstet. 2024, 166, 1218–1224. [Google Scholar] [CrossRef]
- Ogunmodede, F.; Scheftel, J.; Jones, J.L.; Lynfield, R. Toxoplasmosis prevention knowledge among pregnant women in Minnesota. Minn. Med. 2005, 88, 32–34. [Google Scholar] [PubMed]
- Bashir, S.; Ansari, A.H.; Sultana, A. Knowledge, Attitude, and Practiceon Antenatal Care Among Pregnant Women and Its Association with Sociodemographic Factors: A Hospital-Based Study. J. Patient Exp. 2023, 10, 23743735231183578. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Smith, A.D.; Chadwick, P.; Croker, H.; Llewellyn, C.H. Exclusively Digital Health Interventions Targeting Diet, Physical Activity, and Weight Gainin Pregnant Women: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2020, 8, e18255. [Google Scholar] [CrossRef]
- VanLonkhuijzen, R.M.; Rustenhoven, H.; DeVries, J.H.M.; Wagemakers, A. The role of the partnerin the support of a pregnant woman’s healthy diet: An explorative qualitative study. BMC Pregnancy Childbirth 2023, 23, 760. [Google Scholar] [CrossRef]
- Karamolahi, P.F.; Khalesi, Z.B.; Niknami, M. Efficacy of mobile app-based training on health literacy among pregnant women: A randomized controlled trial study. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2021, 12, 100133. [Google Scholar] [CrossRef]
- Lupton, D. The use and value of digital media for information about pregnancy and early motherhood: A focus group study. BMC Pregnancy Childbirth 2016, 16, 171. [Google Scholar] [CrossRef]
- Free, C.; Phillips, G.; Galli, L.; Watson, L.; Felix, L.; Edwards, P.; Patel, V.; Haines, A. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLoS Med. 2013, 10, e1001362. [Google Scholar] [CrossRef]
- Peyton, D.; Hiscock, H.; Sciberras, E. Do Digital Health Interventions Improve Mental Health Literacy or Help-seeking Among Parents of Children Aged 2–12 Years? A Scoping Review. Stud. Health Technol. Inform. 2019, 266, 156–161. [Google Scholar] [CrossRef]
- Maaß, L.; Freye, M.; Pan, C.-C.; Dassow, H.-H.; Niess, J.; Jahnel, T. The Definitions of Health Apps and Medical Apps from the Perspective of Public Health and Law: Qualitative Analysis of an Interdisciplinary Literature Overview. JMIR mHealth uHealth 2022, 10, e37980. [Google Scholar] [CrossRef]
- Brown, H.M.; Bucher, T.; Collins, C.E.; Rollo, M.E. A review of pregnancy iPhone apps assessing their quality, inclusion of behaviour change techniques, and nutritionin formation. Matern. Child. Nutr. 2019, 15, e12768. [Google Scholar] [CrossRef]
- Bonaiuti, R.; Zammarchi, L.; Giaché, S.; Modi, G.; Borchi, B.; Campolmi, I.; Trotta, M.; Ravaldi, C.; Ornaghi, S.; Di Tommaso, M.; et al. Prevention, diagnosis and pharmacological treatment of infectionsin pregnancy: Themobile app GAIA! For healthcare providers and patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 299, 96–104. [Google Scholar] [CrossRef] [PubMed]
| Overall (n = 383) | Minimum Level of Knowledge (n = 163; 42.5%) | Moderate Level of Knowledge (n = 134; 35.0%) | Appropriate Level of Knowledge (n = 86; 22.5%) | Overall p-Value * | 1. p-Value Minimun vs. Moderate 2. p-Value Minimun vs. Appropriate 3. p-Value Moderate vs. Appropriate | ||
|---|---|---|---|---|---|---|---|
| Education level | Primary school | 21 (5.6) | 9 (5.7) | 11 (8.4) | 1 (1.2) | 0.025 | 1. 0.932 2. 0.005 3. 0.005 |
| Secondary school | 138 (36.7) | 66 (41.5) | 48 (36.6) | 24 (27.9) | |||
| University | 217 (57.7) | 84 (52.8) | 72 (55.0) | 61 (70.9) | |||
| At least 1 previous child | No | 205 (53.5) | 89 (54.6) | 75 (56.0) | 41 (47.7) | 0.454 | |
| Yes | 178 (46.5) | 74 (45.4) | 59 (44.0) | 45 (52.3) | |||
| Maternal age (mean ± SD) | 33.34 ± 4.48 | 33.31 ± 4.40 | 33.54 ± 4.78 | 33.09 ± 4.17 | 0.766 | ||
| Maternal age | <25 years | 10 (2.5) | 4 (2.2) | 2 (1.5) | 4 (4.7) | 0.126 | |
| 25–29 years | 52 (13.0) | 25 (14.0) | 22 (16.2) | 5 (5.8) | |||
| 30–34 years | 156 (38.9) | 70 (39.1) | 45 (33.1) | 41 (47.7) | |||
| 35–39 years | 133 (33.2) | 59 (33.0) | 45 (33.1) | 29 (33.7) | |||
| ≥40 years | 50 (12.5) | 21 (11.7) | 22 (16.2) | 7 (8.1) | |||
| Nationality | European | 354 (94.1) | 144 (90.6) | 127 (96.9) | 83 (96.5) | 0.040 | 1. 0.021 2. 0.058 3. 0.893 |
| Non-European | 22 (5.9) | 15 (9.4) | 4 (3.1) | 3 (3.5) | |||
| Data collection time | 1st trimester | 41 (12.3) | 19 (14.0) | 15 (12.9) | 7 (8.5) | 0.765 | |
| 2nd trimester | 91 (27.2) | 34 (25.0) | 33 (28.4) | 24 (29.3) | |||
| 3rd trimester | 202 (60.5) | 83 (61.0) | 68 (58.6) | 51 (62.2) | |||
| Antenatal care setting | Academic maternity center | 289 (75.9) | 131 (80.9) | 94 (70.7) | 64 (74.4) | 0.103 | |
| Community | 24 (6.3) | 5 (3.1) | 13 (9.8) | 6 (7.0) | |||
| First-level hospital | 9 (2.4) | 2 (1.2) | 6 (4.5) | 1 (1.2) | |||
| Private HP | 59 (15.5) | 24 (14.8) | 20 (15.0) | 15 (17.4) | |||
| Information on preventive measures before conception | No | 71 (18.5) | 34 (20.9) | 25 (18.7) | 12 (14.0) | 0.411 | |
| Yes | 312 (81.5) | 129 (79.1) | 109 (81.3) | 74 (86.0) | |||
| Information on preventive measures during pregnancy | No | 11 (2.9) | 6 (3.7) | 3 (2.2) | 2 (2.3) | 0.716 | |
| Yes | 372 (97.1) | 157 (96.3) | 131 (97.8) | 84 (97.7) | |||
| When the information on preventive measures has been received | 1st antenatal appointment | 280 (75.9) | 114 (73.1) | 104 (80.0) | 62 (74.7) | 0.605 | |
| 1st scan | 54 (14.6) | 26 (16.7) | 14 (10.8) | 14 (16.9) | |||
| At one antenatal appointment during pregnancy | 35 (9.5) | 16 (10.3) | 12 (9.2) | 7 (8.4) | |||
| Yes | 288 (75.6) | 114 (70.4) | 101 (75.9) | 73 (84.9) |
| Overall (n = 383) | Minimum Level of Knowledge (n = 163; 42.5%) | Moderate Level of Knowledge (n = 134; 35.0%) | Appropriate Level of Knowledge (n = 86; 22.5%) | Overall p-Value * | 1. p-Value Minimun vs. Moderate 2. p-Value Minimun vs. Appropriate 3. p-Value Moderate vs. Appropriate | ||
|---|---|---|---|---|---|---|---|
| Use of folic acid | No | 58 (15.1) | 25 (15.3) | 15 (11.2) | 18 (20.9) | 0.144 | |
| Yes | 325 (84.9) | 138 (84.7) | 119 (88.8) | 68 (79.1) | |||
| Use of folic acid | Before pregnancy | 171 (52.6) | 73 (52.9) | 60 (50.4) | 38 (55.9) | 0.292 | |
| Following positive pregnancy test | 104 (32.0) | 43 (31.2) | 36 (30.3) | 25 (36.8) | |||
| Following 1st antenatal appointment | 50 (15.4) | 22 (15.9) | 23 (19.3) | 5 (7.4) | |||
| Smoking in pregnancy | No | 349 (91.8) | 152 (93.3) | 118 (89.4) | 79 (92.9) | 0.444 | |
| Yes | 31 (8.2) | 11 (6.7) | 14 (10.6) | 6 (7.1) | |||
| Alcohol in pregnancy | No | 341 (89.0) | 147 (90.2) | 123 (91.8) | 71 (82.6) | 0.084 | |
| Yes | 42 (11.0) | 16 (9.8) | 11 (8.2) | 15 (17.4) | |||
| Heard about toxoplasmosis | No | 11 (2.9) | 7 (4.3) | 3 (2.3) | 1 (1.2) | 0.318 | |
| Yes | 370 (97.1) | 155 (95.7) | 130 (97.7) | 85 (98.8) | |||
| Heard about CMV | No | 84 (22.0) | 48 (29.6) | 23 (17.3) | 13 (15.1) | 0.008 | 1. 0.011 2. 0.009 3. 0.703 |
| Yes | 297 (78.0) | 114 (70.4) | 110 (82.7) | 73 (84.9) | |||
| Heard about spina bifida | No | 100 (26.2) | 52 (32.1) | 36 (27.1) | 12 (14.0) | 0.008 | 1. 0.325 2. 0.002 3. 0.030 |
| Yes | 281 (73.8) | 110 (67.9) | 97 (72.9) | 74 (86.0) | |||
| Heard about parvovirus B19 | No | 291 (76.4) | 133 (82.1) | 100 (75.2) | 58 (67.4) | 0.033 | 1. 0.163 2. 0.010 3. 0.186 |
| Yes | 90 (23.6) | 29 (17.9) | 33 (24.8) | 28 (32.6) | |||
| Heard about fetal alcohol spectrum disorders | No | 247 (64.8) | 119 (73.5) | 86 (64.7) | 42 (48.8) | 0.001 | 1. 0.111 2. <0.001 3. 0.015 |
| Yes | 134 (35.2) | 43 (26.5) | 47 (35.3) | 44 (51.2) | |||
| Heard about Down syndrome | No | 18 (4.7) | 13 (8.0) | 4 (3.0) | 1 (1.2) | 0.027 | 1. 0.043 2. 0.015 3. 0.528 |
| Yes | 363 (95.3) | 149 (92.0) | 129 (97.0) | 85 (98.8) | |||
| Heard about HIV | No | 34 (8.9) | 22 (13.6) | 10 (7.5) | 2 (2.3) | 0.010 | 1. 0.068 2. 0.003 3. 0.185 |
| Yes | 347 (91.1) | 140 (86.4) | 123 (92.5) | 84 (97.7) | |||
| Heard about syphilis | No | 93 (24.4) | 48 (29.6) | 32 (24.1) | 13 (15.1) | 0.040 | 1. 0.266 2. 0.011 3. 0.131 |
| Yes | 288 (75.6) | 114 (70.4) | 101 (75.9) | 73 (84.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernicola, F.; Colciago, E.; Capitoli, G.; Merelli, E.; Arienti, F.; Poletti De Chaurand, V.; Scandella, G.; Carli, A.; Ornaghi, S. Limited Knowledge of Toxoplasmosis-Specific Preventive Behaviors in Pregnant Women: A Survey Study in Northern Italy. Int. J. Environ. Res. Public Health 2025, 22, 517. https://doi.org/10.3390/ijerph22040517
Fernicola F, Colciago E, Capitoli G, Merelli E, Arienti F, Poletti De Chaurand V, Scandella G, Carli A, Ornaghi S. Limited Knowledge of Toxoplasmosis-Specific Preventive Behaviors in Pregnant Women: A Survey Study in Northern Italy. International Journal of Environmental Research and Public Health. 2025; 22(4):517. https://doi.org/10.3390/ijerph22040517
Chicago/Turabian StyleFernicola, Federica, Elisabetta Colciago, Giulia Capitoli, Elisa Merelli, Francesca Arienti, Valeria Poletti De Chaurand, Gaia Scandella, Anna Carli, and Sara Ornaghi. 2025. "Limited Knowledge of Toxoplasmosis-Specific Preventive Behaviors in Pregnant Women: A Survey Study in Northern Italy" International Journal of Environmental Research and Public Health 22, no. 4: 517. https://doi.org/10.3390/ijerph22040517
APA StyleFernicola, F., Colciago, E., Capitoli, G., Merelli, E., Arienti, F., Poletti De Chaurand, V., Scandella, G., Carli, A., & Ornaghi, S. (2025). Limited Knowledge of Toxoplasmosis-Specific Preventive Behaviors in Pregnant Women: A Survey Study in Northern Italy. International Journal of Environmental Research and Public Health, 22(4), 517. https://doi.org/10.3390/ijerph22040517






