Late Diagnosis of Swyer Syndrome in a Patient with Bilateral Germ Cell Tumor Treated with a Contraceptive Due to Primary Amenorrhea
Abstract
1. Introduction
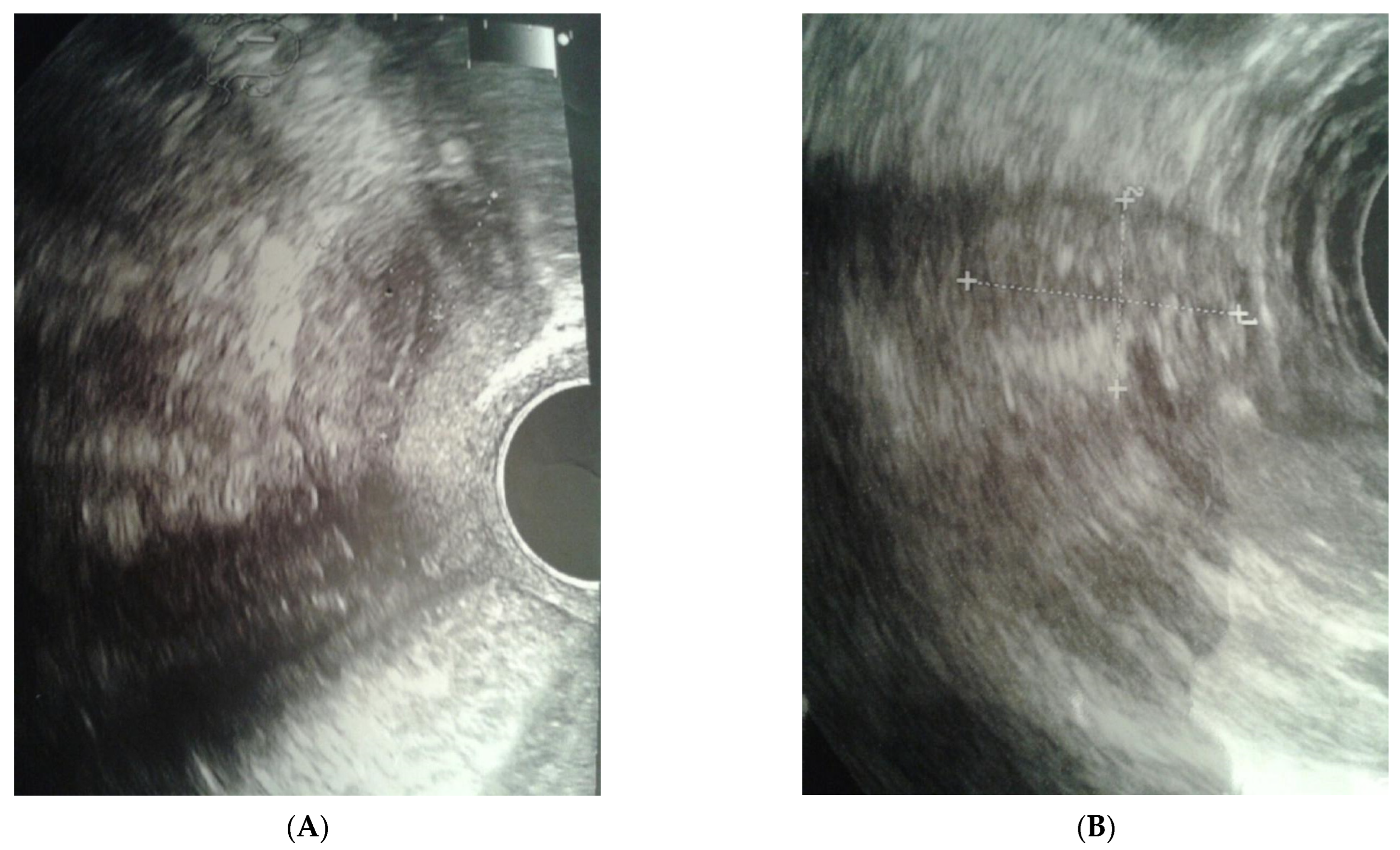
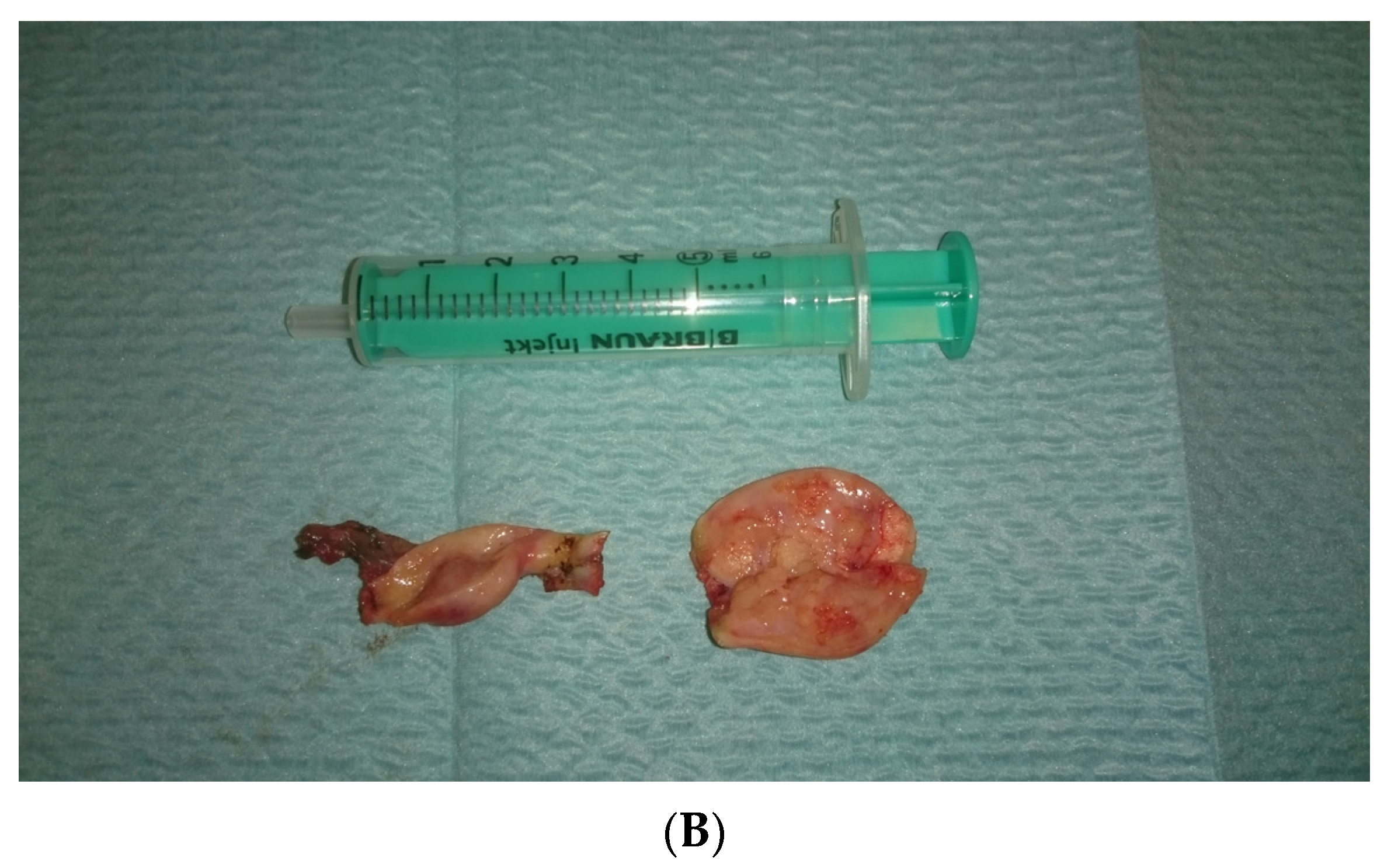
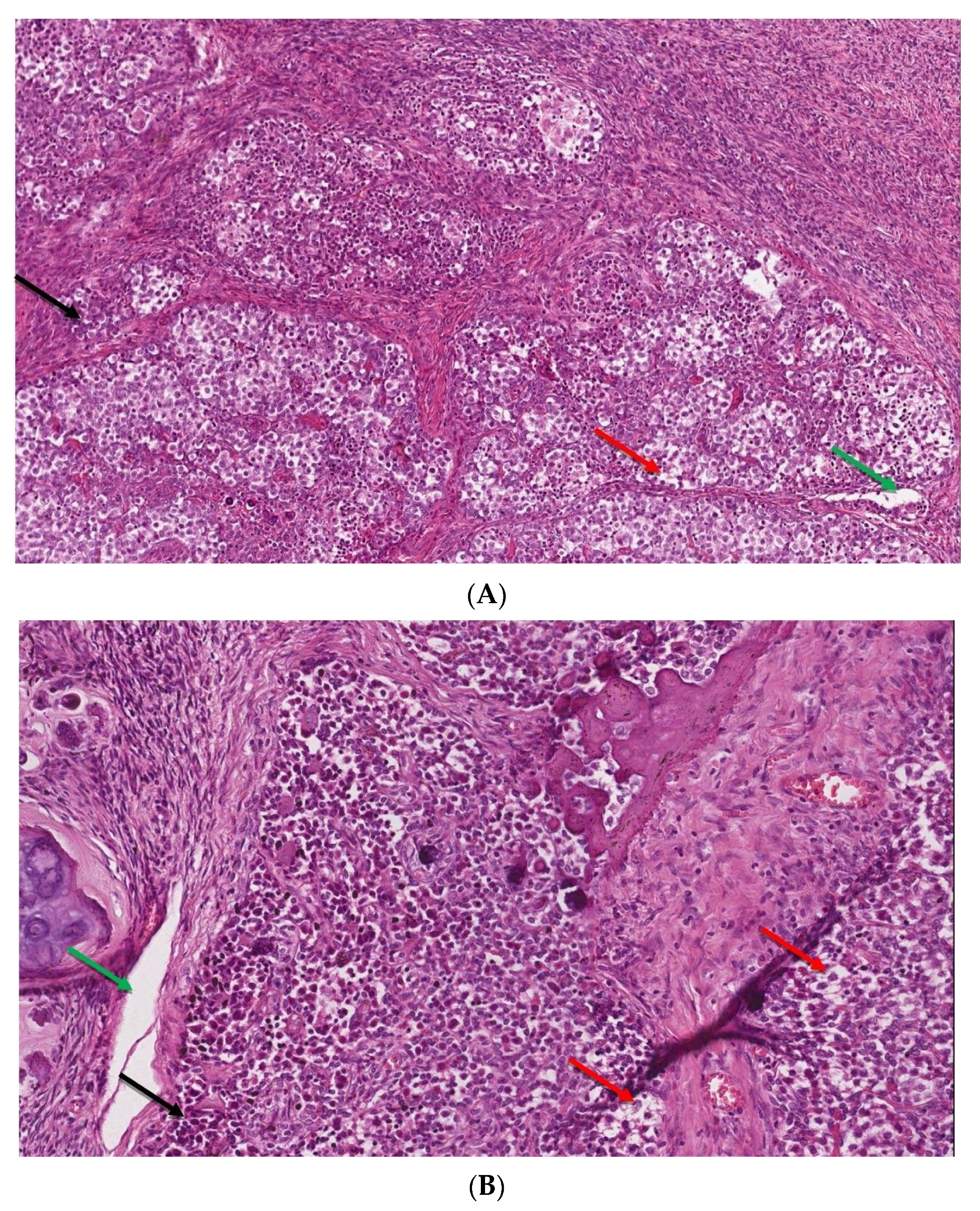
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, P.A.; Houk, C.P.; Ahmed, S.F.; Hughes, I.A.; Achermann, J.; Baskin, L.; Berenbaum, S.; Bertelloni, S.; Brock, J.; Carmichael, P.; et al. Consensus statement on management of intersex disorders. Pediatrics 2006, 118, e488–e500. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Harley, V.R. Disorders of sex development: New genes, new concepts. Nat. Rev. Endocrinol. 2013, 9, 79–91. [Google Scholar] [CrossRef] [PubMed]
- King, T.F.J.; Conway, G.S. Swyer syndrome. Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Loke, J.; Pearlman, A.; Radi, O.; Zuffardi, O.; Giussani, U.; Pallotta, R.; Camerino, G.; Ostrer, H. Mutations in MAP3K1 tilt the balance from SOX9/FGF9 to WNT/β-catenin signaling. Hum. Mol. Genet. 2014, 23, 1073–1083. [Google Scholar] [CrossRef] [PubMed]
- Cools, M.; Drop, S.L.S.; Wolffenbuttel, K.P.; Oosterhuis, J.W.; Looijenga, L.H.J. Germ cell tumors in the intersex gonad: Old paths, new directions, moving frontiers. Endocr. Rev. 2006, 27, 468–484. [Google Scholar] [CrossRef] [PubMed]
- Hughes, I.A.; Houk, C.; Ahmed, S.F.; Lee, P.A. Consensus statement on management of intersex disorders. J. Pediatr. Urol. 2006, 2, 148–162. [Google Scholar] [CrossRef] [PubMed]
- Michala, L.; Goswami, D.; Creighton, S.M.; Conway, G.S. Swyer syndrome: Presentation and outcomes. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Seppä, S.; Kuiri, T.H.; Holopainen, E.; Voutilainen, R. Diagnosis and management of primary amenorrhea and female delayed puberty. Eur. J. Endocrinol. 2021, 184, R225–R242. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.A.; Paradise, S.L.; Reeder, R.M. Amenorrhea: A systematic approach to diagnosis and management. Am. Fam. Physician 2019, 100, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Reindollar, R.H.; Byrd, J.R.; McDonough, P.G. Delayed sexual development: A study of 252 patients. Am. J. Obstet. Gynecol. 1981, 140, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.M.; Arboleda, V.A.; Lee, H.; Barseghyan, H.; Adam, M.P.; Fechner, P.Y.; Bargman, R.; Keegan, C.; Travers, S.; Schelley, S.; et al. Exome sequencing for the diagnosis of 46, XY disorders of sex development. J. Clin. Endocrinol. Metab. 2015, 100, E333–E344. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yi, Y.; Yao, H.; Yang, Z.; Hu, H.; Liu, J.; Gao, C.; Zhang, M.; Zhou, L.; Yi, X.; et al. Targeted next-generation sequencing identification of mutations in patients with disorders of sex development. BMC Med. Genet. 2016, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.Y.; Cheon, C.K. Evaluation and management of amenorrhea related to congenital sex hormonal disorders. Ann. Pediatr. Endocrinol. Metab. 2019, 24, 149. [Google Scholar] [CrossRef] [PubMed]
- Marsh, C.A.; Grimstad, F.W. Primary amenorrhea: Diagnosis and management. Obstet. Gynecol. Surv. 2014, 69, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Hughes, I.A.; Houk, C.; Ahmed, S.F.; Lee, P.A. Consensus statement on management of intersex disorders. Arch. Dis. Child. 2006, 91, 554–563. [Google Scholar] [CrossRef]
- Kersemaekers, A.M.; Honecker, F.; Stoop, H.; Cools, M.; Molier, M.; Wolffenbuttel, K.; Bokemeyer, C.; Li, Y.; Lau, Y.F.; Oosterhuis, J.W.; et al. Identification of germ cells at risk for neoplastic transformation in gonadoblastoma: An immunohistochemical study for OCT3/4 and TSPY. Hum. Pathol. 2005, 36, 512–521. [Google Scholar] [CrossRef] [PubMed]
- de Jong, J.; Stoop, H.; Dohle, G.R.; Bangma, C.H.; Kliffen, M.; van Esser, J.W.; van den Bent, M.; Kros, J.M.; Oosterhuis, J.W.; Looijenga, L.H. Diagnostic value of OCT3/4 for pre-invasive and invasive testicular germ cell tumours. J. Pathol. 2005, 262, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Wang, C.; Tian, Q. Gonadal tumour risk in 292 phenotypic female patients with disorders of sex development containing Y chromosome or Y-derived sequence. Clin. Endocrinol. 2017, 86, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Bandala-Jacques, A.; Estrada-Rivera, F.; Cantu, D.; Prada, D.; Montalvo-Esquivel, G.; González-Enciso, A.; Barquet-Munoz, S.A. Role of optimal cytoreduction in patients with dysgerminoma. Int. J. Gynecol. Cancer 2019, 29, 1405–1410. [Google Scholar] [CrossRef] [PubMed]
- Wünsch, L.; Holterhus, P.M.; Wessel, L.; Hiort, O. Patients with disorders of sex development (DSD) at risk of gonadal tumour development: Management based on laparoscopic biopsy and molecular diagnosis. BJU Int. 2012, 110, E958–E965. [Google Scholar] [CrossRef] [PubMed]


| Group of Risk | Malignancy Risk [%] | Disorder | Procedure |
|---|---|---|---|
| High | 15–35 | gonadal dysgenesis (Y +, intraabdominal gonads) | gonadectomy (during the diagnosis period) |
| 50 | PAIS (testicles outside the scrotum) | ||
| 40–60 | Frasier, Denys Drash (Y+) | ||
| Middle | 12 | Turner (Y+) | gonadectomy (during the diagnosis period) |
| 28 | 17ß HSD deficiency | Monitoring | |
| ? | Gonadal dysgenesis (Y +, gonads in the scrotum) | Biopsy during puberty and irradiation ? | |
| ? | PAIS—partial insensitivity to androgens (gonads in the scrotum) | Biopsy during puberty and irradiation ? | |
| Low | 3 | CAIS—complete insensitivity to androgens | Biopsy during puberty and ? |
| 2 | Ovarian-nuclear DSD | Testis tissue removal ? | |
| 1 | Turner (Y-) | None |
| Parameter | Score | Sr |
|---|---|---|
| FSH | 56.7 mIU/mL | 2.8–11.3 |
| LH | 19.8 mIU/mL | 1.2–11.6 |
| Estradiol | <5 pg/mL | 10–160 |
| Testosteron | 0.348 ng/mL | 0.006–0.8 |
| ACTH | 28.6 pg/mL | 7.2–63.3 |
| Cortisol | 16.9 µg/dL | 6.2–19.4 |
| TSH | 3.7 mIU/mL | 0.2–4.0 |
| fT4 | 1.03 ng/dL | 0.9–1.7 |
| LDH | 118.0 U/L | 120–230 |
| beta-hCG | 0.753 IU/mL | <10 |
| AFP | 3.8 IU/mL | <6 |
| Ca-125 | 8.21 U/mL | <35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sowińska-Przepiera, E.; Krzyścin, M.; Przepiera, A.; Brodowska, A.; Malanowska, E.; Kozłowski, M.; Cymbaluk-Płoska, A. Late Diagnosis of Swyer Syndrome in a Patient with Bilateral Germ Cell Tumor Treated with a Contraceptive Due to Primary Amenorrhea. Int. J. Environ. Res. Public Health 2023, 20, 2139. https://doi.org/10.3390/ijerph20032139
Sowińska-Przepiera E, Krzyścin M, Przepiera A, Brodowska A, Malanowska E, Kozłowski M, Cymbaluk-Płoska A. Late Diagnosis of Swyer Syndrome in a Patient with Bilateral Germ Cell Tumor Treated with a Contraceptive Due to Primary Amenorrhea. International Journal of Environmental Research and Public Health. 2023; 20(3):2139. https://doi.org/10.3390/ijerph20032139
Chicago/Turabian StyleSowińska-Przepiera, Elżbieta, Mariola Krzyścin, Adam Przepiera, Agnieszka Brodowska, Ewelina Malanowska, Mateusz Kozłowski, and Aneta Cymbaluk-Płoska. 2023. "Late Diagnosis of Swyer Syndrome in a Patient with Bilateral Germ Cell Tumor Treated with a Contraceptive Due to Primary Amenorrhea" International Journal of Environmental Research and Public Health 20, no. 3: 2139. https://doi.org/10.3390/ijerph20032139
APA StyleSowińska-Przepiera, E., Krzyścin, M., Przepiera, A., Brodowska, A., Malanowska, E., Kozłowski, M., & Cymbaluk-Płoska, A. (2023). Late Diagnosis of Swyer Syndrome in a Patient with Bilateral Germ Cell Tumor Treated with a Contraceptive Due to Primary Amenorrhea. International Journal of Environmental Research and Public Health, 20(3), 2139. https://doi.org/10.3390/ijerph20032139






