Readmissions to General ICUs in a Geographic Area of Poland Are Seemingly Associated with Better Outcomes
Abstract
1. Introduction
2. Material and Methods
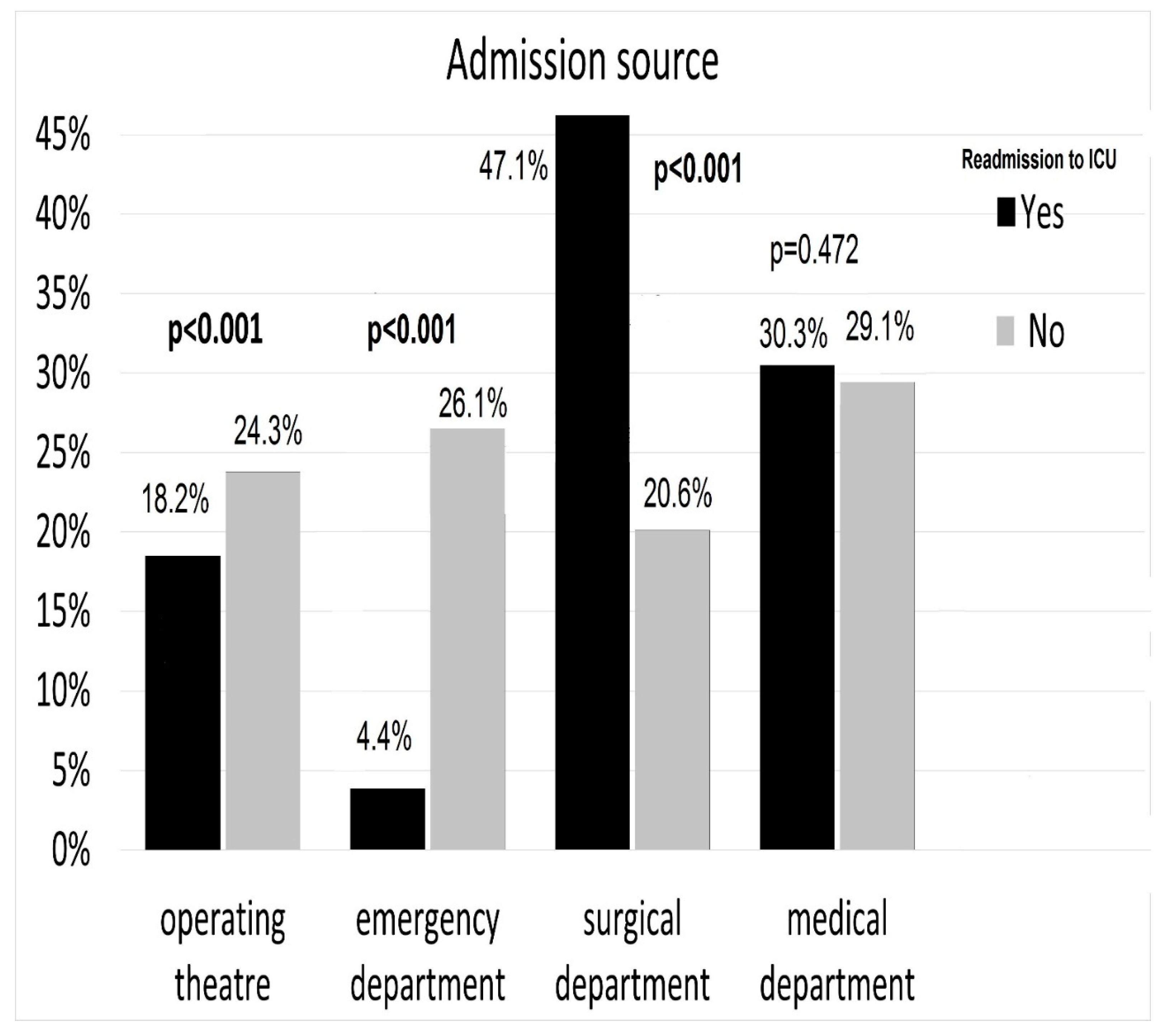
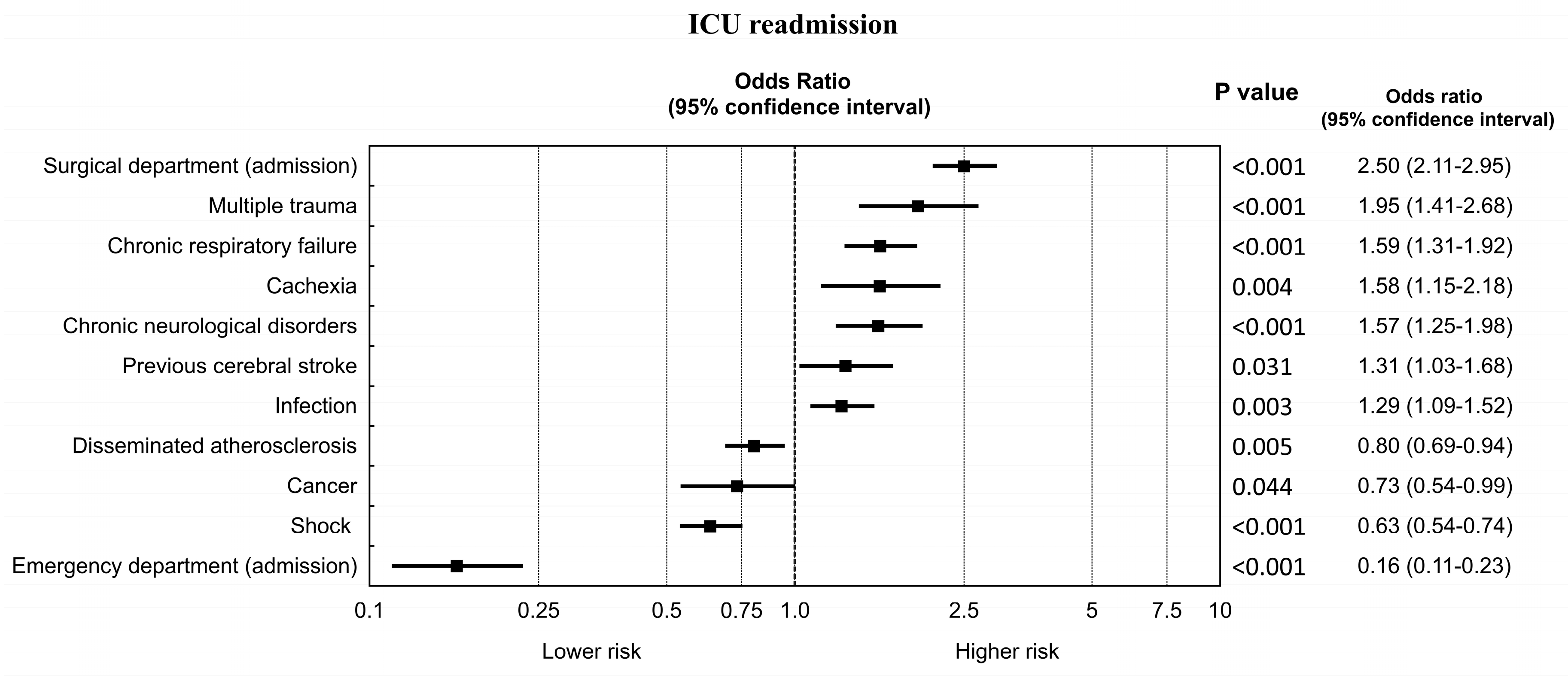
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ICU | Intensive Care Unit |
| APACHE | Acute Physiology Age Chronic Health Evaluation |
| SAPS | Simplified Acute Physiology Score |
| TISS | Therapeutic Intervention Scoring System |
References
- Desautels, T.; Das, R.; Calvert, J.; Trivedi, M.; Summers, C.; Wales, D.J.; Ercole, A. Prediction of early unplanned intensive care unit readmission in a UK tertiary care hospital: A cross-sectional machine learning approach. BMJ Open 2017, 7, e017199. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.A.; Higgins, T.L.; Zimmerman, J.E. The association between ICU readmission rate and patient outcomes. Crit. Care Med. 2013, 41, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, R.; Terblanche, M.; Vlachos, S. The Utility of ICU Readmission as a Quality Indicator and the Effect of Selection. Crit. Care Med. 2018, 46, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Sabbatini, A.K.; Kocher, K.E.; Basu, A.; Hsia, R.Y. In-Hospital Outcomes and Costs Among Patients Hospitalized During a Return Visit to the Emergency Department. JAMA 2016, 315, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Nates, J.L.; Nunnally, M.; Kleinpell, R.; Blosser, S.; Goldner, J.; Birriel, B.; Fowler, C.S.; Byrum, D.; Miles, W.S.; Bailey, H.; et al. ICU Admission, Discharge, and Triage Guidelines: A Framework to Enhance Clinical Operations, Development of Institutional Policies, and Further Research. Crit. Care Med. 2016, 44, 1553–1602. [Google Scholar] [CrossRef] [PubMed]
- Weigl, W.; Adamski, J.; Goryński, P.; Kański, A.; Hultström, M. Mortality rate is higher in Polish intensive care units than in other European countries. Intensive Care Med. 2017, 43, 1730–1732. [Google Scholar] [CrossRef] [PubMed]
- Weigl, W.; Adamski, J.; Goryński, P.; Kański, A.; Hultström, M. ICU mortality and variables associated with ICU survival in Poland: A nationwide database study. Eur. J. Anaesthesiol. 2018, 35, 949–954. [Google Scholar] [CrossRef]
- Knapik, P.; Krzych, Ł.J.; Weigl, W.; Adamski, J.; Hultstöm, M. Mortality rate in Polish intensive care units is lower than predicted according to the APACHE II scoring system. Intensive Care Med. 2017, 43, 1745–1746. [Google Scholar] [CrossRef][Green Version]
- Knapik, P.; Misiewska-Kaczur, A.; Gierek, D.; Rychlik, W.; Czekaj, M.; Łowicka, M.; Jezienicki, M. Day and time of admissions to intensive care units—Does it matter? Anaesthesiol. Intensive Ther. 2018, 50, 27–33. [Google Scholar] [CrossRef]
- Jarząbek, R.; Bugajski, P.; Greberski, K.; Błaszczyński, J.; Słowińska-Jarząbek, B.; Kalawski, R. Readmission to an intensive care unit after cardiac surgery: Reasons and outcomes. Kardiol. Pol. 2014, 72, 740–747. [Google Scholar] [CrossRef]
- Litwinowicz, R.; Bartus, K.; Drwila, R.; Kapelak, B.; Konstanty-Kalandyk, J.; Sobczynski, R.; Wierzbicki, K.; Bartuś, M.; Chrapusta, A.; Timek, T.; et al. In-hospital mortality in cardiac surgery patients after readmission to the intensive care unit: A single-center experience with 10,992 patients. J. Cardiothorac. Vasc. Anesth. 2015, 29, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Krzych, Ł.J.; Czempik, P.F.; Kucewicz-Czech, E.; Knapik, P. Silesian Registry of Intensive Care Units. Anaesthesiol. Intensive Ther. 2017, 49, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Knapik, P.; Trejnowska, E.; Knapik, M.; Kręt, M.; Cieśla, D.; Krzych, Ł.J.; Kucewicz-Czech, E. Young Adults Among Patients Admitted to Polish Intensive Care Units in the Silesian ICU Registry. Med. Sci. Monit. 2019, 25, 5727–5737. [Google Scholar] [CrossRef] [PubMed]
- Czempik, P.; Cieśla, D.; Knapik, P.; Krzych, Ł. Mortality of patients with acute kidney injury requiring renal replacement therapy. Adv. Clin. Exp. Med. 2018, 27, 327–333. [Google Scholar] [CrossRef] [PubMed]
- van Sluisveld, N.; Bakhshi-Raiez, F.; de Keizer, N.; Holman, R.; Wester, G.; Wollersheim, H.; van der Hoeven, J.G.; Zegers, M. Variation in rates of ICU readmissions and post-ICU in-hospital mortality and their association with ICU discharge practices. BMC Health Serv. Res. 2017, 17, 281. [Google Scholar] [CrossRef]
- Chu, C.C.; Liu, C.J.; Shih, C.M.; Kung, P.T.; Tsai, Y.S.; Tsai, W.C. The Risk and Related Factors for Readmission to an ICU Within 7 Days in Mechanically Ventilated Subjects—A Nationwide Population-Based Cohort Study. Respir. Care. 2015, 60, 1786–1795. [Google Scholar] [CrossRef]
- Wong, E.G.; Parker, A.M.; Leung, D.G.; Brigham, E.P.; Arbaje, A.I. Association of severity of illness and intensive care unit readmission: A systematic review. Heart Lung 2016, 45, 3–9. [Google Scholar] [CrossRef]
- Hosein, F.S.; Bobrovitz, N.; Berthelot, S.; Zygun, D.; Ghali, W.A.; Stelfox, H.T. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit. Care 2013, 17, R102. [Google Scholar] [CrossRef]
- Ponzoni, C.R.; Corrêa, T.D.; Filho, R.R.; Neto, A.S.; Assunção, M.S.; Pardini, A.; Schettino, G.P. Readmission to Intensive Care Unit: Incidence, Risk Factors, Resource Use and Outcomes: A Retrospective Cohort Study. Ann. Am. Thorac. Soc. 2017, 14, 1312–1319. [Google Scholar] [CrossRef]
- Adamski, J.; Goraj, R.; Onichimowski, D.; Gawlikowska, E.; Weigl, W. The differences between two selected intensive care units located in central and northern Europe-preliminary observation. Anaesthesiol. Intensive Ther. 2015, 47, 117–124. [Google Scholar] [CrossRef]
- Kübler, A.; Siewiera, J.; Durek, G.; Kusza, K.; Piechota, M.; Szkulmowski, Z. Guidelines regarding the ineffective maintenance of organ functions (futile therapy) in ICU patients incapable of giving informed statements of will. Anaesthesiol. Intensive Ther. 2014, 46, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Capuzzo, M.; Volta, C.; Tassinati, T.; Moreno, R.; Valentin, A.; Guidet, B.; Iapichino, G.; Martin, C.; Perneger, T.; Combescure, C.; et al. Working Group on Health Economics of the European Society of Intensive Care Medicine. Hospital mortality of adults admitted to Intensive Care Units in hospitals with and without Intermediate Care Units: A multicentre European cohort study. Crit. Care 2014, 18, 551. [Google Scholar] [CrossRef] [PubMed]
- Piechota, A.; Piechota, M. Adult intensive therapy services contracted by the National Health Fund in 2012. Anaesthesiol. Intensive Ther. 2012, 44, 123–139. [Google Scholar] [PubMed]
- Woldhek, A.L.; Rijkenberg, S.; Bosman, R.J.; van der Voort, P.H. Readmission of ICU patients: A quality indicator? J. Crit. Care 2017, 38, 328–334. [Google Scholar] [CrossRef]
- Rosa, R.G.; Roehrig, C.; Oliveira, R.P.; Maccari, J.G.; Antônio, A.C.; de Souza Castro, P.; Neto, F.L.; de Campos Balzano, P.; Teixeira, C. Comparison of Unplanned Intensive Care Unit Readmission Scores: A Prospective Cohort Study. PLoS ONE 2015, 10, e0143127. [Google Scholar] [CrossRef]
- Lai, J.I.; Lin, H.Y.; Lai, Y.C.; Lin, P.C.; Chang, S.C.; Tang, G.J. Readmission to the intensive care unit: A population-based approach. J. Formos. Med. Assoc. 2012, 111, 504–509. [Google Scholar] [CrossRef]
- Timmers, T.K.; Verhofstad, M.H.; Moons, K.G.; Leenen, L.P. Patients’ characteristics associated with readmission to a surgical intensive care unit. Am. J. Crit. Care 2012, 21, e120–e128. [Google Scholar] [CrossRef]
- Kastrup, M.; Powollik, R.; Balzer, F.; Röber, S.; Ahlborn, R.; von Dossow-Hanfstingl, V.; Wernecke, K.D.; Spies, C.D. Predictive ability of the stability and workload index for transfer score to predict unplanned readmissions after ICU discharge. Crit. Care Med. 2013, 41, 1608–1615. [Google Scholar] [CrossRef]
- Kareliusson, F.; De Geer, L.; Tibblin, A.O. Risk prediction of ICU readmission in a mixed surgical and medical population. J. Intensive Care 2015, 3, 30. [Google Scholar] [CrossRef]
- van Diepen, S.; Graham, M.M.; Nagendran, J.; Norris, C.M. Predicting cardiovascular intensive care unit readmission after cardiac surgery: Derivation and validation of the Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease (APPROACH) cardiovascular intensive care unit clinical prediction model from a registry cohort of 10,799 surgical cases. Crit. Care 2014, 18, 651. [Google Scholar] [CrossRef]
| Group of Variables | Readmitted | Non-Readmitted | p | |||
|---|---|---|---|---|---|---|
| (n = 839) | (n = 20.656) | |||||
| Co-morbidities | Coronary artery disease | 373 | (44.5%) | 8600 | (41.6%) | 0.112 |
| Heart failure | 308 | (36.7%) | 7247 | (35.1%) | 0.352 | |
| Arterial hypertension | 415 | (49,5%) | 10.548 | (51.1%) | 0.382 | |
| Disseminated atherosclerosis | 266 | (31.7%) | 7046 | (34.1%) | 0.160 | |
| Chronic respiratory failure | 144 | (17.2%) | 2435 | (11.8%) | <0.001 | |
| Home oxygen therapy | 14 | (1.7%) | 274 | (1.3%) | 0.489 | |
| Extreme obesity | 50 | (6.0%) | 1131 | (5.5%) | 0.599 | |
| Cachexia | 45 | (5.4%) | 719 | (3.5%) | 0.005 | |
| Alcoholism | 62 | (7.4%) | 1920 | (9.3%) | 0.070 | |
| Diabetes | 209 | (24.9%) | 5098 | (24.7%) | 0.912 | |
| Chronic renal failure | 117 | (14.0%) | 2996 | (14.5%) | 0.688 | |
| Dialysis dependency | 12 | (1.4%) | 257 | (1.2%) | 0.751 | |
| Previous cerebral stroke | 79 | (9.4%) | 1488 | (7.2%) | 0.019 | |
| Chronic neurological disorders | 93 | (11.1%) | 1544 | (7.5%) | <0.001 | |
| Systemic autoimmune diseases | 9 | (1.1%) | 244 | (1.2%) | 0.902 | |
| Post-transplant | 2 | (0.2%) | 45 | (0.2%) | 0.801 | |
| Cancer | 48 | (5.7%) | 1594 | (7.7%) | 0.039 | |
| Pregnancy | 0 | (0.0%) | 40 | (0.2%) | 0.386 | |
| None | 68 | (8.1%) | 2029 | (9.8%) | 0.113 | |
| Primary Reason of ICU Admission | Readmitted | Non-Readmitted | p | |||
|---|---|---|---|---|---|---|
| (n = 839) | (n = 20.656) | |||||
| Shock | 213 | (25.4%) | 6375 | (30.9%) | 0.001 | |
| Cardiac arrest | 186 | (22.2%) | 5168 | (25.0%) | 0.067 | |
| Postoperative | 269 | (32.1%) | 6157 | (29.8%) | 0.174 | |
| Multiple trauma | 48 | (5.7%) | 765 | (3.7%) | 0.004 | |
| Craniocerebral trauma | 45 | (5.4%) | 1000 | (4.8%) | 0.543 | |
| Acute pancreatitis | 15 | (1.8%) | 320 | (1.6%) | 0.686 | |
| Obstetric complications | 1 | (0.1%) | 75 | (0.4%) | 0.384 | |
| Acute neurological disorders | 57 | (6.8%) | 1572 | (7.6%) | 0.418 | |
| Intoxication | 4 | (0.5%) | 337 | (1.6%) | 0.013 | |
| Severe metabolic disorders | 35 | (4.2%) | 1148 | (5.6%) | 0.099 | |
| Sepsis | 62 | (7.4%) | 1448 | (7.0%) | 0.724 | |
| Infection | 203 | (24.2%) | 3802 | (18.4%) | <0.001 | |
| Advanced monitoring | 447 | (53.3%) | 11.317 | (55.6%) | 0.409 | |
| ICU Treatment | Readmitted | Non-Readmitted | p | ||
|---|---|---|---|---|---|
| (n = 839) | (n = 20.656) | ||||
| Catecholamines | 580 | (69.1%) | 14.992 | (72.6%) | 0.031 |
| Intubation | 476 | (56.7%) | 13.333 | (64.6%) | <0.001 |
| Tracheostomy | 217 | (25.9%) | 3306 | (16.0%) | <0.001 |
| Renal replacement therapy | 73 | (8.7%) | 1938 | (9.4%) | 0.546 |
| Operation while in the ICU | 86 | (10.3%) | 1866 | (9.0%) | 0.254 |
| Intra-aortic balloon pump | 20 | (2.4%) | 537 | (2.6%) | 0.783 |
| ECMO | 5 | (0.6%) | 58 | (0.3%) | 0.184 |
| Discharge and Outcome | Readmitted | Non-Readmitted | p | |||
|---|---|---|---|---|---|---|
| (n = 839) | (n = 20.656) | |||||
| General status at ICU discharge | Good | 212 | (25.3%) | 5577 | (27.0%) | 0.285 |
| Average | 257 | (30.6%) | 5135 | (24.9%) | <0.001 | |
| Severe | 41 | (4.9%) | 800 | (3.9%) | 0.163 | |
| Death | 329 | (39.2%) | 9144 | (44.4%) | 0.004 | |
| Neurological status (Glasgow Outcome Score) | Good | 256 | (30.5%) | 6588 | (31.9%) | 0.421 |
| Moderate disability | 120 | (14.3%) | 2558 | (12.4%) | 0.110 | |
| Severe disability | 90 | (10.7%) | 1465 | (7.1%) | <0.001 | |
| Minimally conscious or vegetative | 44 | (5.2%) | 901 | (4.4%) | 0.256 | |
| Death | 329 | (39.2%) | 9144 | (44.4%) | 0.004 | |
| Discharge to | Same hospital—another department | 328 | (39.1%) | 8142 | (39.4%) | 0.879 |
| Other hospital | 140 | (16.7%) | 2820 | (13.7%) | 0.014 | |
| Long-term facility | 20 | (2.4%) | 215 | (1.0%) | <0.001 | |
| Home | 22 | (2.6%) | 335 | (1.6%) | 0.037 | |
| Death | 329 | (39.2%) | 9144 | (44.4%) | 0.004 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grochla, M.; Saucha, W.; Ciesla, D.; Knapik, P. Readmissions to General ICUs in a Geographic Area of Poland Are Seemingly Associated with Better Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 565. https://doi.org/10.3390/ijerph17020565
Grochla M, Saucha W, Ciesla D, Knapik P. Readmissions to General ICUs in a Geographic Area of Poland Are Seemingly Associated with Better Outcomes. International Journal of Environmental Research and Public Health. 2020; 17(2):565. https://doi.org/10.3390/ijerph17020565
Chicago/Turabian StyleGrochla, Marek, Wojciech Saucha, Daniel Ciesla, and Piotr Knapik. 2020. "Readmissions to General ICUs in a Geographic Area of Poland Are Seemingly Associated with Better Outcomes" International Journal of Environmental Research and Public Health 17, no. 2: 565. https://doi.org/10.3390/ijerph17020565
APA StyleGrochla, M., Saucha, W., Ciesla, D., & Knapik, P. (2020). Readmissions to General ICUs in a Geographic Area of Poland Are Seemingly Associated with Better Outcomes. International Journal of Environmental Research and Public Health, 17(2), 565. https://doi.org/10.3390/ijerph17020565





