Death Related to a Congenital Vascular Anomaly of Pulmonary Hamartoma Type: Malpractice or Tragic Fatality?
Abstract
:1. Introduction
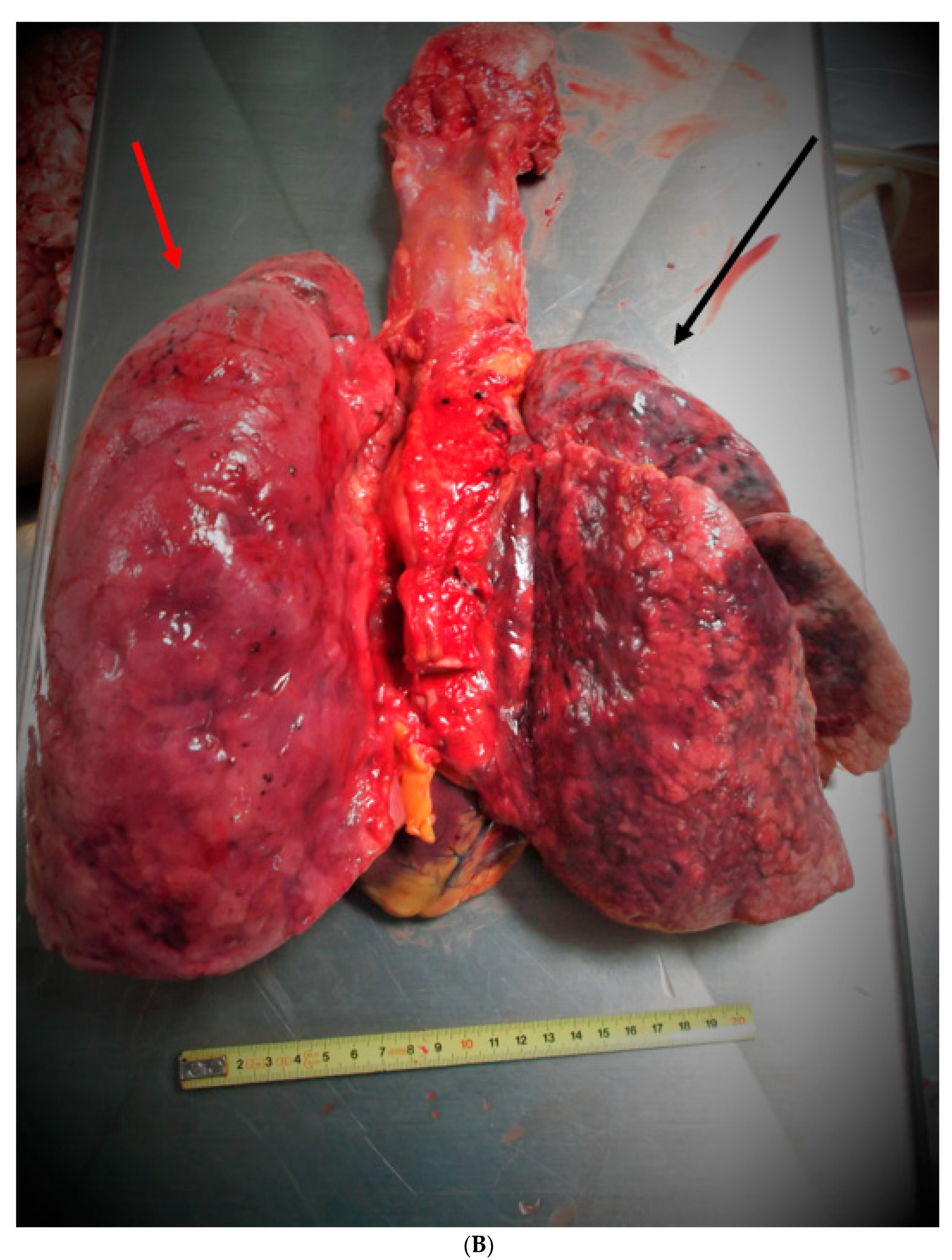
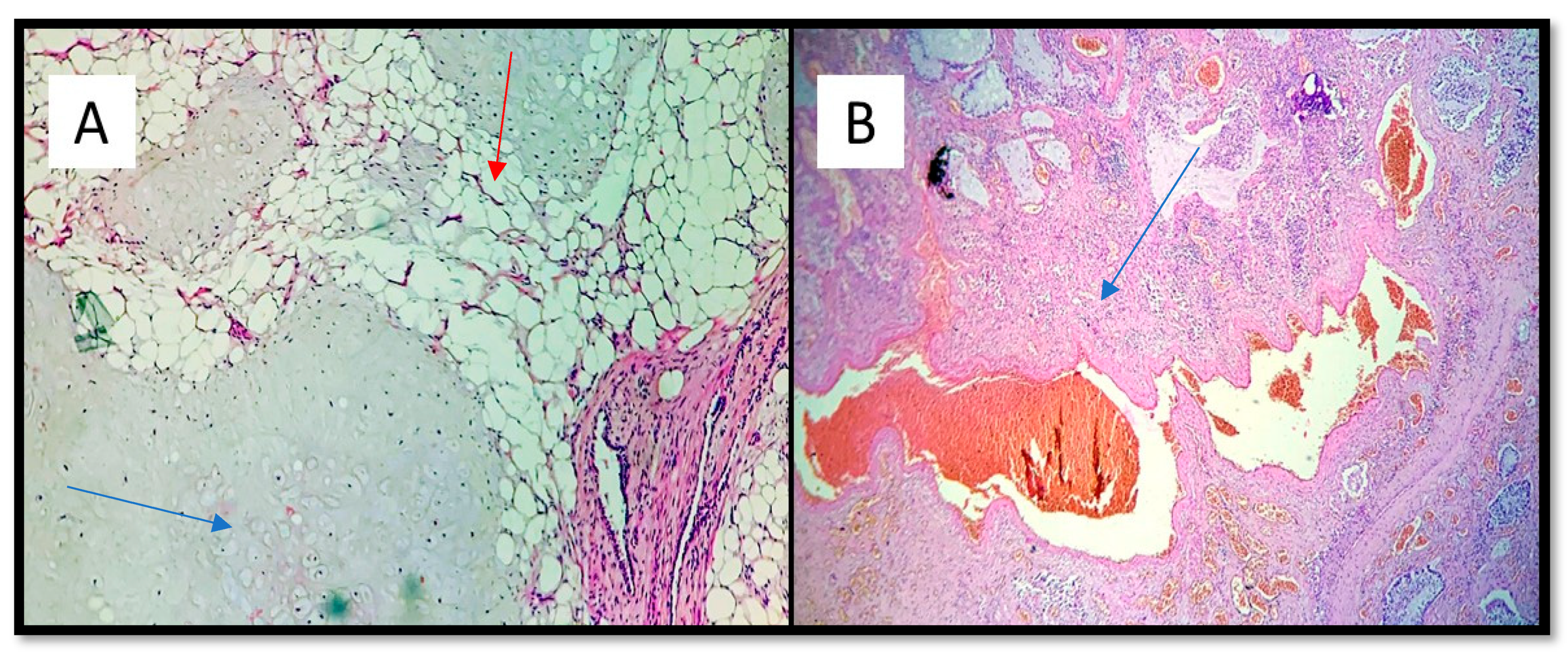
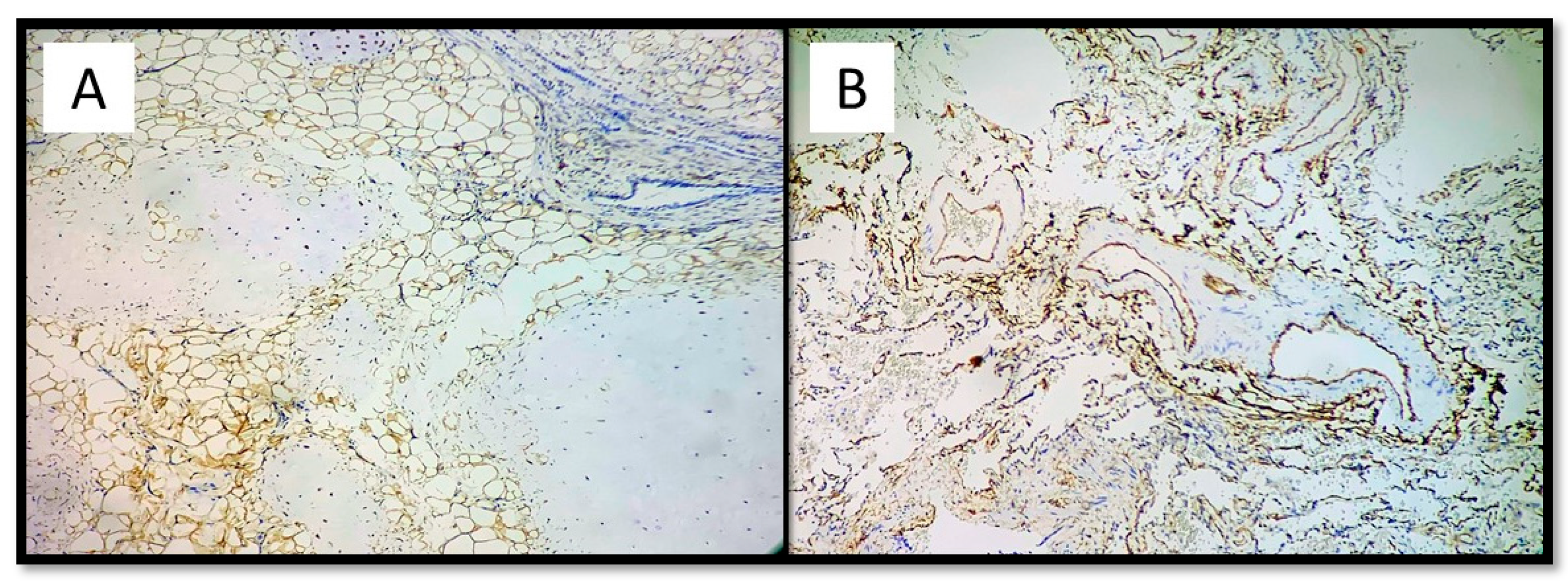
2. Case Presentation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mishra, D.; Gupta, P.; Singh, T. Teaching for reducing diagnostic errors. Indian Pediatr. 2017, 54, 37–45. [Google Scholar] [CrossRef]
- Schoenfeld, E.M.; Mader, S.; Houghton, C.; Wenger, R.; Probst, M.A.; Schoenfeld, D.A.; Lindenauer, P.K.; Mazor, K.M. The Effect of Shared Decisionmaking on Patients’ Likelihood of Filing a Complaint or Lawsuit: A Simulation Study. Ann. Emerg. Med. 2019, 74, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Luján, J.L.; Todt, O. Standards of evidence and causality in regulatory science: Risk and benefit assessment. Stud. Hist. Philos. Sci. Part A 2019, 80, 82–89. [Google Scholar] [CrossRef]
- Jin, F.; Mu, D.; Chu, D.; Fu, E.; Xie, Y.; Liu, T. Severe Complications of Bronchoscopy. Respiration 2008, 76, 429–433. [Google Scholar] [CrossRef]
- Jacomelli, M.; Margotto, S.S.; DeMarzo, S.E.; Scordamaglio, P.R.; Cardoso, P.F.G.; Palomino, A.L.M.; Figueiredo, V.R. Early complications in flexible bronchoscopy at a university hospital. J. Bras. Pneumol. 2020, 46, e20180125. [Google Scholar] [CrossRef]
- Nili, M.; Vidne, B.A.; Avidor, I.; Paz, R.; Levy, M.J. Multiple Pulmonary Hamartomas; A Case Report and Review of the Literature. Scand. J. Thorac. Cardiovasc. Surg. 1979, 13, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.; Condliffe, R.; Donaldson, J.W.; Kiely, D.G.; Wort, S.J. British Thoracic Society Clinical Statement on Pulmonary Arteriovenous Malformations. Thorax 2017, 72, 1154–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tellapuri, S.; Park, H.S.; Kalva, S.P. Pulmonary arteriovenous malformations. Int. J. Cardiovasc. Imaging 2018, 35, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Kamath, S.G.; Vivek, G.; Borkar, S.; Ramachandran, P. Pulmonary arteriovenous malformation presenting as a large aneurysm. BMJ Case Rep. 2012, 2012, bcr2012006811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, Y.; Li, X.-X.; Mu, X.-D.; Li, N.; Wang, Y.; Li, T. [Pulmonary capillary hemangiomatosis: A case report and literature review]. Beijing Da Xue Xue Bao 2015, 47, 865–869. [Google Scholar]
- Giampalmo, A. The arteriovenous angiomatosis of the lung with hypoxaemia. Acta Medica Scand. 2009, 138, 1–67. [Google Scholar] [CrossRef]
- Chen, Q.-R.; Li, H.; Hu, B.; Jin, M.-L.; Guo, J. Multiple Cavernous Hemangiomas of the Lung. Ann. Thorac. Surg. 2014, 98, 1835–1837. [Google Scholar] [CrossRef] [PubMed]
- Lundeen, K.S.; Raj, M.S.; Rajasurya, V.; Ludhwani, D. Pulmonary Hamartoma; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Sylvester, J.T.; Shimoda, L.A.; Aaronson, P.I.; Ward, J.P.T. Hypoxic Pulmonary Vasoconstriction. Physiol. Rev. 2012, 92, 367–520. [Google Scholar] [CrossRef]
- Martini, K.; Eberhard, M.; Frauenfelder, T. Lungenrundherde–Ein Überblick. Ther. Umsch. 2020, 77, 75–80. [Google Scholar] [CrossRef]
- Whyte, R.I.; Donington, J.S. Hamartomas of the lung. Semin. Thorac. Cardiovasc. Surg. 2003, 15, 301–304. [Google Scholar] [CrossRef]
- Shin, M.S.; McElvein, R.B.; Ho, K.J. Radiographic evidence of calcification in pulmonary hamartomas. J. Natl. Med. Assoc. 1992, 84, 329–331. [Google Scholar] [PubMed]
- Basile, A.; Gregoris, A.; Antoci, B.; Romanelli, M. Malignant change in a benign pulmonary hamartoma. Thorax 1989, 44, 232–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siegelman, S.S.; Khouri, N.F.; Scott, W.W.; Leo, F.P.; Hamper, U.M.; Fishman, E.K.; Zerhouni, E.A. Pulmonary hamartoma: CT findings. Radiology 1986, 160, 313–317. [Google Scholar] [CrossRef]
- Himpe, U.; Deroose, C.M.; De Leyn, P.; Verbeken, E.; Vansteenkiste, J. Unexpected Slight Fluorodeoxyglucose-Uptake on Positron Emission Tomography in a Pulmonary Hamartoma. J. Thorac. Oncol. 2009, 4, 107–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.; Yu, D. PI(3)King Apart PTEN’s Role in Cancer: Figure 1. Clin. Cancer Res. 2010, 16, 4325–4330. [Google Scholar] [CrossRef] [Green Version]
- Hobert, J.A.; Eng, C. PTEN hamartoma tumor syndrome: An overview. Genet. Med. 2009, 11, 687–694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nieuwenhuis, M.H.; Kets, C.M.; Murphy-Ryan, M.; Yntema, H.G.; Evans, G.; Colas, C.; Møller, P.; Hes, F.J.; Hodgson, S.V.; Olderode-Berends, M.J.W.; et al. Cancer risk and genotype–phenotype correlations in PTEN hamartoma tumor syndrome. Fam. Cancer 2014, 13, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Pilarski, R.; Burt, R.; Kohlman, W.; Pho, L.; Shannon, K.M.; Swisher, E. Cowden Syndrome and the PTEN Hamartoma Tumor Syndrome: Systematic Review and Revised Diagnostic Criteria. J. Natl. Cancer Inst. 2013, 105, 1607–1616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalra, J. Medical errors: An introduction to concepts. Clin. Biochem. 2004, 37, 1043–1051. [Google Scholar] [CrossRef]
- Legemaate, J.; Akkermans, A.J.; Friele, R.D. [Disclosing medical errors: The current situation]. Ned. Tijdschr. Geneeskd. 2015, 159, 9089. [Google Scholar]
- Oyebode, F. Clinical Errors and Medical Negligence. Med. Princ. Pract. 2013, 22, 323–333. [Google Scholar] [CrossRef]
- Papavramidou, N.; Voultsos, P. Medical malpractice cases in Hippocratic collection: A review and today’s perspective. Hippokratia 2020, 23, 99–105. [Google Scholar]
- Hureau, J.; Hubinois, P. Medical liability. Comparative compensation for personal injury in Europe. Bull. L’académie Natl. Méd. 2005, 189, 815. [Google Scholar] [CrossRef]
- Panella, M.; Leigheb, F.; Rinaldi, C.; Donnarumma, C.; Tozzi, Q.; Di Stanislao, F. Defensive Medicine: Defensive Medicine: Overview of the literature. Ig. Sanita Pubblica 2015, 71, 335–351. [Google Scholar]
- Hermer, L.D.; Brody, H. Defensive Medicine, Cost Containment, and Reform. J. Gen. Intern. Med. 2010, 25, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, R.; Gupta, A.; Gupta, S. The impact of tort reform on defensive medicine, quality of care, and physician supply: A systematic review. Health Serv. Res. 2019, 54, 851–859. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marrone, M.; Marrone, L.; Cazzato, G.; Baldassarra, S.L.; Ingravallo, G.; Stellacci, A. Death Related to a Congenital Vascular Anomaly of Pulmonary Hamartoma Type: Malpractice or Tragic Fatality? Medicina 2021, 57, 1231. https://doi.org/10.3390/medicina57111231
Marrone M, Marrone L, Cazzato G, Baldassarra SL, Ingravallo G, Stellacci A. Death Related to a Congenital Vascular Anomaly of Pulmonary Hamartoma Type: Malpractice or Tragic Fatality? Medicina. 2021; 57(11):1231. https://doi.org/10.3390/medicina57111231
Chicago/Turabian StyleMarrone, Maricla, Laura Marrone, Gerardo Cazzato, Stefania Lonero Baldassarra, Giuseppe Ingravallo, and Alessandra Stellacci. 2021. "Death Related to a Congenital Vascular Anomaly of Pulmonary Hamartoma Type: Malpractice or Tragic Fatality?" Medicina 57, no. 11: 1231. https://doi.org/10.3390/medicina57111231
APA StyleMarrone, M., Marrone, L., Cazzato, G., Baldassarra, S. L., Ingravallo, G., & Stellacci, A. (2021). Death Related to a Congenital Vascular Anomaly of Pulmonary Hamartoma Type: Malpractice or Tragic Fatality? Medicina, 57(11), 1231. https://doi.org/10.3390/medicina57111231








