First Isolation and Clinical Case of Brevundimonas diminuta in a Newborn with Low Birth Weight, in Democratic Republic of Congo: A Case Report
Abstract
1. Introduction
2. Material and Methods
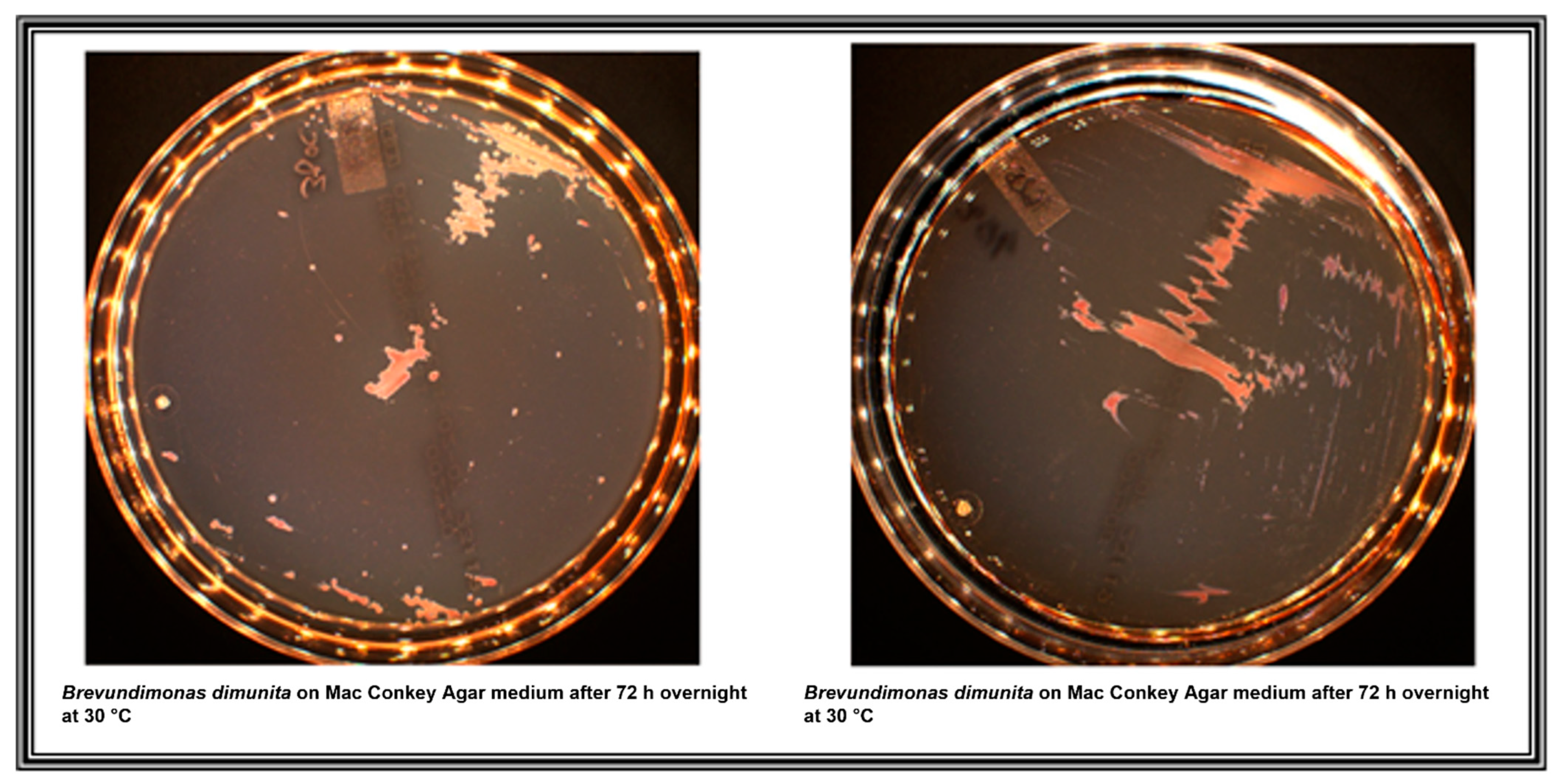
3. Result
3.1. Case Presentation
3.2. Molecular Characterisation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Segers, P.; Vancanneyt, M.; Pot, B.; Torck, U.; Hoste, B.; Dewettinck, D.; Falsen, E.; Kersters, K.; De Vos, P. Classification of Pseudomonas diminuta Leifson and Hugh 1954 and Pseudomonas vesicularis Busing, Doll, and Freytag 1953 in Brevundimonas gen. nov. as Brevundimonas diminuta comb. nov. and Brevundimonas vesicularis comb. nov., Respectively. Int. J. Syst. Bacteriol. 1994, 44, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Bhatia, B.D. Brevundimonas Septicemia: A Rare Infection with Rare Presentation. Indian Pediatr. 2015, 52, 15. [Google Scholar]
- LPSN. Available online: www.bacterio.net/brevundimonas.htm (accessed on 11 April 2019).
- Lu, B.; Shi, Y.; Zhu, F.; Xu, X. Pleuritis due to Brevundimonas diminuta in a previously healthy man. J. Med. Microbiol. 2013, 62, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Karadag, N.; Karagol, B.S.; Kundak, A.A.; Dursun, A.; Okumus, N.; Tanır, G.; Zencıroglu, A. Spectrum of Brevundimonas vesicularis infections in neonatal period: A case series at a tertiary referral center. Infection 2012, 40, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Almuzara, M.N.; Barberis, C.M.; Rodríguez, C.H.; Famiglietti, A.M.R.; Ramirez, M.S.; Vay, C.A. First Report of an Extensively Drug-Resistant VIM-2 Metallo-β-Lactamase-Producing Brevundimonas diminuta Clinical Isolate. J. Clin. Microbiol. 2012, 50, 2830–2832. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cao, H.; Li, M.; Yang, X.; Zhang, C. Brevundimonas diminuta bacteremia in a man with myelodysplastic syndromes. Indian J. Pathol. Microbiol. 2015, 58, 384–386. [Google Scholar] [CrossRef]
- Han, X.Y.; Andrade, R.A. Brevundimonas diminuta infections and its resistance to fluoroquinolones. J. Antimicrob. Chemother. 2005, 55, 853–859. [Google Scholar] [CrossRef]
- Menuet, M.; Bittar, F.; Stremler, N.; Dubus, J.-C.; Sarles, J.; Raoult, D.; Rolain, J.-M. First isolation of two colistin-resistant emerging pathogens, Brevundimonas diminuta and Ochrobactrum anthropi, in a woman with cystic fibrosis: A case report. J. Med. Case Rep. 2008, 2, 373. [Google Scholar] [CrossRef]
- Pandit, R.T. Brevundimonas Diminuta Keratitis. Eye Contact Lens Sci. Clin. Pr. 2012, 38, 63–65. [Google Scholar] [CrossRef]
- Adesoji, A.T.; Olatoye, I.O.; Ogunjobi, A.A. Genotypic Characterization of Aminoglycoside Resistance Genes from Bacteria Isolates in Selected Municipal Drinking Water Distribution Sources in Southwestern Nigeria. Ethiop. J. Health Sci. 2019, 29, 321–332. [Google Scholar]
- Mahjoubi, M.; Jaouani, A.; Guesmi, A.; Amor, S.B.; Jouini, A.; Cherif, H.; Najjari, A.; Boudabous, A.; Koubaa, N.; Cherif, A. Hydro-carbonoclastic bacteria isolated from petroleum contaminated sites in Tunisia: Isolation, identification and characterization of the biotechnological potential. New Biotechnol. 2013, 30, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Lukhele, T.; Nyoni, H.; Mamba, B.B.; Msagati, T.A.M. Unraveling bacterial diversity in oil refinery effluents. Arch. Microbiol. 2021, 203, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Mansur, A.A.; Adetutu, E.M.; Kadali, K.K.; Morrison, P.D.; Nurulita, Y.; Ball, A. Assessing the hydrocarbon degrading potential of indigenous bacteria isolated from crude oil tank bottom sludge and hydrocarbon-contaminated soil of Azzawiya oil refinery, Libya. Environ. Sci. Pollut. Res. 2014, 21, 10725–10735. [Google Scholar] [CrossRef]
- Matuschek, E.; Brown, D.F.J.; Kahlmeter, G. Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin. Microbiol. Infect. 2014, 20, O255–O266. [Google Scholar] [CrossRef]
- Ly, T.D.A.; Hadjadj, L.; Hoang, V.T.; Louni, M.; Dao, T.L.; Badiaga, S.; Dupont, H.T.; Raoult, D.; Rolain, J.M.; Gautret, P. Low prevalence of resistance genes in sheltered homeless population in Marseille, France, 2014–2018. Infect. Drug Resist. 2019, 12, 1139–1151. [Google Scholar] [CrossRef]
- Chandra, A.; Das, A.; Sen, M.; Sharma, M. Brevundimonas diminuta infection in a case of nephrotic syndrome. Indian J. Pathol. Microbiol. 2017, 60, 279. [Google Scholar] [CrossRef]
- Chi, C.-Y.; Fung, C.-P.; Wong, W.-W.; Liu, C.-Y. Brevundimonas bacteremia: Two case reports and literature review. Scand. J. Infect. Dis. 2004, 36, 59–61. [Google Scholar] [CrossRef]
- Lee, M.-R.; Huang, Y.T.; Liao, C.-H.; Chuang, T.Y.; Lin, C.-K.; Lee, S.W.; Lai, C.C.; Yu, C.-J.; Hsueh, P.R. Bacteremia caused by Brevundimonas species at a tertiary care hospital in Taiwan, 2000–2010. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 30, 1185–1191. [Google Scholar] [CrossRef]
- Mazzola, P.G.; Martins, A.M.; Penna, T.C. Chemical resistance of the gram-negative bacteria to different sanitizers in a water purification system. BMC Infect. Dis. 2006, 6, 131. [Google Scholar] [CrossRef] [PubMed]
- Coffey, P.S.; Brown, S.C. Umbilical cord-care practices in low- and middle-income countries: A systematic review. BMC Pregnancy Childbirth 2017, 17, 1–21. [Google Scholar] [CrossRef]
- Sazawal, S.; Dhingra, U.; Ali, S.M.; Dutta, A.; Deb, S.; Ame, S.M.; Mkasha, M.H.; Yadav, A.; Black, R.E. Efficacy of chlorhexidine application to umbilical cord on neonatal mortality in Pemba, Tanzania: A community-based randomised controlled trial. Lancet Glob. Health 2016, 4, e837–e844. [Google Scholar] [CrossRef]
- Turyasiima, M.; Nduwimana, M.; Kiconco, G.; Egesa, W.I.; Manuel, S.A.; Kalubi, P.; Ortiz, Y.E.A. Bacteriology and Antibiotic Suscepti-bility Patterns among Neonates Diagnosed of Omphalitis at a Tertiary Special Care Baby Unit in Western Uganda. Int. J. Pediatr. 2020, 2020, 4131098. [Google Scholar] [CrossRef] [PubMed]
- Sawardekar, K.P. Changing spectrum of neonatal omphalitis. Pediatr. Infect. Dis. J. 2004, 23, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Burch, J.; Tatineni, S.; Enofe, I.; Laird-Fick, H. Brevundimonas diminuta coinfection as source of pyogenic liver abscess. BMJ Case Rep. 2021, 14, e236235. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lupande-Mwenebitu, D.; Tshiyongo, R.K.; Lunguya-Metila, O.; Lavigne, J.-P.; Rolain, J.-M.; Diene, S.M. First Isolation and Clinical Case of Brevundimonas diminuta in a Newborn with Low Birth Weight, in Democratic Republic of Congo: A Case Report. Medicina 2021, 57, 1227. https://doi.org/10.3390/medicina57111227
Lupande-Mwenebitu D, Tshiyongo RK, Lunguya-Metila O, Lavigne J-P, Rolain J-M, Diene SM. First Isolation and Clinical Case of Brevundimonas diminuta in a Newborn with Low Birth Weight, in Democratic Republic of Congo: A Case Report. Medicina. 2021; 57(11):1227. https://doi.org/10.3390/medicina57111227
Chicago/Turabian StyleLupande-Mwenebitu, David, Raphael Kavul Tshiyongo, Octavie Lunguya-Metila, Jean-Philippe Lavigne, Jean-Marc Rolain, and Seydina M. Diene. 2021. "First Isolation and Clinical Case of Brevundimonas diminuta in a Newborn with Low Birth Weight, in Democratic Republic of Congo: A Case Report" Medicina 57, no. 11: 1227. https://doi.org/10.3390/medicina57111227
APA StyleLupande-Mwenebitu, D., Tshiyongo, R. K., Lunguya-Metila, O., Lavigne, J.-P., Rolain, J.-M., & Diene, S. M. (2021). First Isolation and Clinical Case of Brevundimonas diminuta in a Newborn with Low Birth Weight, in Democratic Republic of Congo: A Case Report. Medicina, 57(11), 1227. https://doi.org/10.3390/medicina57111227







