Determination of Blood NOTCH3 Extracellular Domain and Jagged-1 Levels in Healthy Subjects
Abstract
:1. Introduction
2. Results
2.1. Participant Characteristics
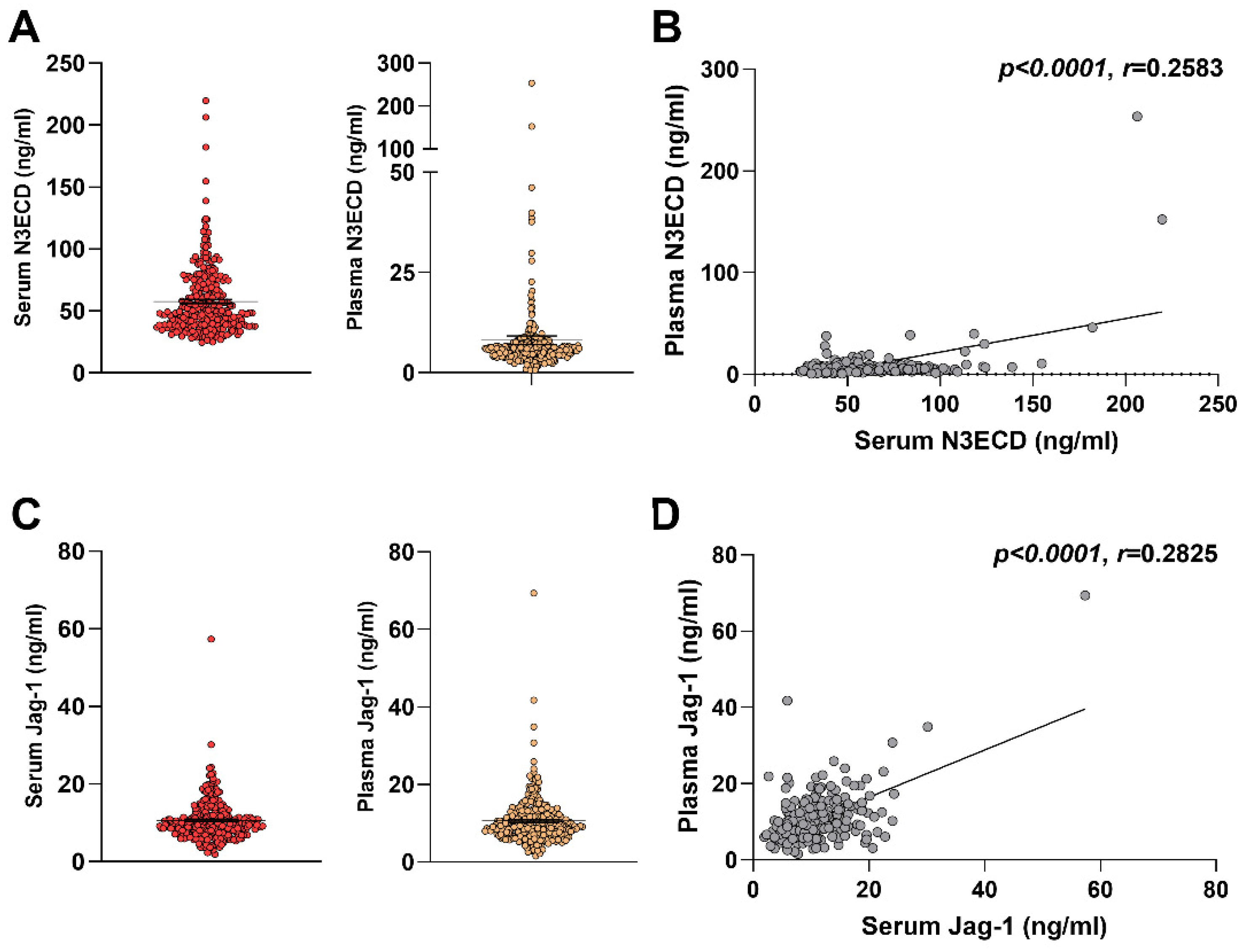
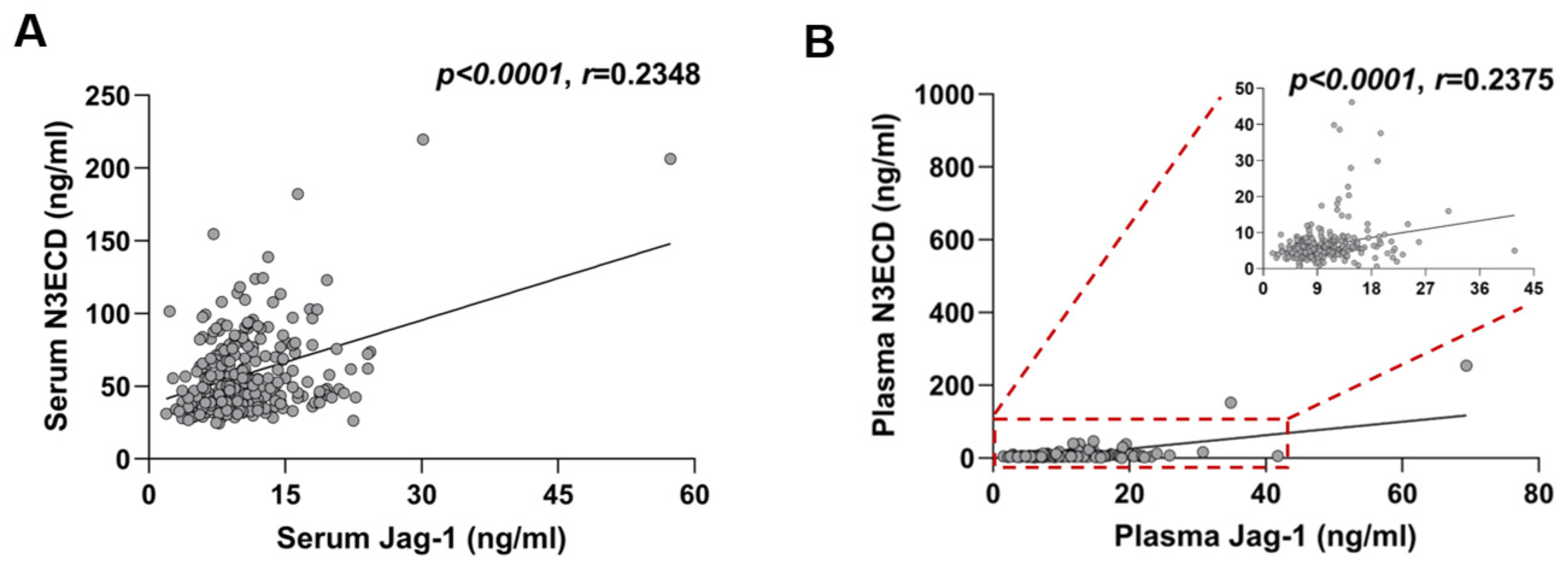
2.2. Determination of Serum and Plasma Levels of N3ECD and Jagged-1
2.3. Associations between N3ECD or Jagged-1 Levels and Clinical Characteristics
3. Discussion
4. Materials and Methods
4.1. Study Participants
4.2. Biochemical Analysis
4.3. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gridley, T. Notch signaling in vascular development and physiology. Development 2007, 134, 2709–2718. [Google Scholar] [CrossRef]
- Boucher, J.; Gridley, T.; Liaw, L. Molecular pathways of notch signaling in vascular smooth muscle cells. Front. Physiol. 2012, 3, 81. [Google Scholar] [CrossRef] [PubMed]
- Baeten, J.T.; Lilly, B. Notch Signaling in Vascular Smooth Muscle Cells. Adv. Pharm. 2017, 78, 351–382. [Google Scholar]
- Joutel, A.; Corpechot, C.; Ducros, A.; Vahedi, K.; Chabriat, H.; Mouton, P.; Alamowitch, S.; Domenga, V.; Cecillion, M.; Marechal, E.; et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature 1996, 383, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.C. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy: A genetic cause of cerebral small vessel disease. J. Clin. Neurol. 2010, 6, 1–9. [Google Scholar] [CrossRef]
- Chabriat, H.; Joutel, A.; Dichgans, M.; Tournier-Lasserve, E.; Bousser, M.G. Cadasil. Lancet Neurol. 2009, 8, 643–653. [Google Scholar] [CrossRef]
- Choi, J.C. Genetics of cerebral small vessel disease. J. Stroke 2015, 17, 7–16. [Google Scholar] [CrossRef]
- Artavanis-Tsakonas, S.; Rand, M.D.; Lake, R.J. Notch signaling: Cell fate control and signal integration in development. Science 1999, 284, 770–776. [Google Scholar] [CrossRef]
- High, F.A.; Zhang, M.; Proweller, A.; Tu, L.; Parmacek, M.S.; Pear, W.S.; Epstein, J.A. An essential role for Notch in neural crest during cardiovascular development and smooth muscle differentiation. J. Clin. Investig. 2007, 117, 353–363. [Google Scholar] [CrossRef]
- Manderfield, L.J.; High, F.A.; Engleka, K.A.; Liu, F.; Li, L.; Rentschler, S.; Epstein, J.A. Notch activation of Jagged1 contributes to the assembly of the arterial wall. Circulation 2012, 125, 314–323. [Google Scholar] [CrossRef]
- Breikaa, R.M.; Denman, K.; Ueyama, Y.; McCallinhart, P.E.; Khan, A.Q.; Agarwal, G.; Trask, A.J.; Garg, V.; Lilly, B. Loss of Jagged1 in mature endothelial cells causes vascular dysfunction with alterations in smooth muscle phenotypes. Vasc. Pharmacol. 2022, 145, 107087. [Google Scholar] [CrossRef] [PubMed]
- Liem, M.K.; van der Grond, J.; Haan, J.; van den Boom, R.; Ferrari, M.D.; Knaap, Y.M.; Breuning, M.H.; van Buchem, M.A.; Middelkoop, H.A.; Lesnik Oberstein, S.A. Lacunar infarcts are the main correlate with cognitive dysfunction in CADASIL. Stroke 2007, 38, 923–928. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, M.; Jarosz, J.M.; Martin, R.J.; Deasy, N.; Powell, J.F.; Markus, H.S. MRI hyperintensities of the temporal lobe and external capsule in patients with CADASIL. Neurology 2001, 56, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Chabriat, H.; Herve, D.; Duering, M.; Godin, O.; Jouvent, E.; Opherk, C.; Alili, N.; Reyes, S.; Jabouley, A.; Zieren, N.; et al. Predictors of Clinical Worsening in Cerebral Autosomal Dominant Arteriopathy With Subcortical Infarcts and Leukoencephalopathy: Prospective Cohort Study. Stroke 2016, 47, 4–11. [Google Scholar] [CrossRef]
- Jickling, G.C.; Sharp, F.R. Biomarker panels in ischemic stroke. Stroke 2015, 46, 915–920. [Google Scholar] [CrossRef]
- Vilar-Bergua, A.; Riba-Llena, I.; Nafria, C.; Bustamante, A.; Llombart, V.; Delgado, P.; Montaner, J. Blood and CSF biomarkers in brain subcortical ischemic vascular disease: Involved pathways and clinical applicability. J. Cereb. Blood Flow Metab. 2016, 36, 55–71. [Google Scholar] [CrossRef]
- Pescini, F.; Donnini, I.; Cesari, F.; Nannucci, S.; Valenti, R.; Rinnoci, V.; Poggesi, A.; Gori, A.M.; Giusti, B.; Rogolino, A.; et al. Circulating Biomarkers in Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy Patients. J. Stroke Cerebrovasc. Dis. 2017, 26, 823–833. [Google Scholar] [CrossRef]
- Gravesteijn, G.; Rutten, J.W.; Verberk, I.M.W.; Bohringer, S.; Liem, M.K.; van der Grond, J.; Aartsma-Rus, A.; Teunissen, C.E.; Lesnik Oberstein, S.A.J. Serum Neurofilament light correlates with CADASIL disease severity and survival. Ann. Clin. Transl. Neurol. 2019, 6, 46–56. [Google Scholar] [CrossRef]
- Duering, M.; Konieczny, M.J.; Tiedt, S.; Baykara, E.; Tuladhar, A.M.; Leijsen, E.V.; Lyrer, P.; Engelter, S.T.; Gesierich, B.; Achmuller, M.; et al. Serum Neurofilament Light Chain Levels Are Related to Small Vessel Disease Burden. J. Stroke 2018, 20, 228–238. [Google Scholar] [CrossRef]
- Gao, D.; Shang, J.; Sun, R.; Shi, Y.; Jiang, H.; Ma, M.; Zhang, J. Changes in the Morphology, Number, and Protein Levels of Plasma Exosomes in CADASIL Patients. J. Alzheimers Dis. 2021, 81, 221–229. [Google Scholar] [CrossRef]
- Lu, C.H.; Macdonald-Wallis, C.; Gray, E.; Pearce, N.; Petzold, A.; Norgren, N.; Giovannoni, G.; Fratta, P.; Sidle, K.; Fish, M.; et al. Neurofilament light chain: A prognostic biomarker in amyotrophic lateral sclerosis. Neurology 2015, 84, 2247–2257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergman, J.; Dring, A.; Zetterberg, H.; Blennow, K.; Norgren, N.; Gilthorpe, J.; Bergenheim, T.; Svenningsson, A. Neurofilament light in CSF and serum is a sensitive marker for axonal white matter injury in MS. Neurol. Neuroimmunol. Neuroinflamm. 2016, 3, e271. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Cheng, Y.W.; Chen, Y.F.; Tang, S.C.; Jeng, J.S. Plasma neurofilament light chain and glial fibrillary acidic protein predict stroke in CADASIL. J. Neuroinflamm. 2020, 17, 124. [Google Scholar] [CrossRef]
- Ebke, M.; Dichgans, M.; Bergmann, M.; Voelter, H.U.; Rieger, P.; Gasser, T.; Schwendemann, G. CADASIL: Skin biopsy allows diagnosis in early stages. Acta. Neurol. Scand. 1997, 95, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M.; Straube, A.; Bruening, R.; Uttner, I.; Pongratz, D.; Gasser, T.; Dichgans, M.; Muller-Hocker, J. Muscle and skin biopsies are a sensitive diagnostic tool in the diagnosis of CADASIL. J. Neurol. 1999, 246, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Primo, V.; Graham, M.; Bigger-Allen, A.A.; Chick, J.M.; Ospina, C.; Quiroz, Y.T.; Manent, J.; Gygi, S.P.; Lopera, F.; D’Amore, P.A.; et al. Blood biomarkers in a mouse model of CADASIL. Brain Res. 2016, 1644, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Di Maio, G.; Formichi, P.; Radi, E.; Bianchi, S.; Onnis, A.; Tarquini, E.; Leoncini, L.; Federico, A. Human peripheral blood lymphocytes and fibroblasts as Notch3 expression models. J. Cell. Physiol. 2012, 227, 1771–1775. [Google Scholar] [CrossRef]
- Conboy, I.M.; Conboy, M.J.; Smythe, G.M.; Rando, T.A. Notch-mediated restoration of regenerative potential to aged muscle. Science 2003, 302, 1575–1577. [Google Scholar] [CrossRef]
- Balistreri, C.R.; Madonna, R.; Melino, G.; Caruso, C. The emerging role of Notch pathway in ageing: Focus on the related mechanisms in age-related diseases. Ageing Res. Rev. 2016, 29, 50–65. [Google Scholar] [CrossRef]
- Tiao, J.Y.; Semmens, J.B.; Masarei, J.R.; Lawrence-Brown, M.M. The effect of age on serum creatinine levels in an aging population: Relevance to vascular surgery. Cardiovasc. Surg. 2002, 10, 445–451. [Google Scholar] [CrossRef]
- Rowe, J.W.; Andres, R.; Tobin, J.D.; Norris, A.H.; Shock, N.W. The effect of age on creatinine clearance in men: A cross-sectional and longitudinal study. J. Gerontol. 1976, 31, 155–163. [Google Scholar] [CrossRef] [PubMed]


| Healthy Subjects (n = 279) | |||
|---|---|---|---|
| Male (n = 131) | Female (n = 148) | p-Value * | |
| Demographic characteristics | |||
| Age—yr(mean ± SD) | 49.7 ± 11.0 | 47.8 ± 10.1 | 0.1319 * |
| Height—cm(mean ± SD) | 171.2 ± 5.9 | 160.1 ± 5.4 | <0.0001 * |
| Weight—kg(mean ± SD) | 73.3 ± 8.7 | 57.1 ± 7.5 | <0.0001 * |
| Medical history—no.(%) | |||
| Smoking | 60 (45.8) | 9 (6.1) | <0.0001 † |
| Drinking | 111 (84.7) | 95 (64.2) | <0.0001 † |
| Laboratory values—mean ± SD | |||
| Systolic blood pressure—mmHg | 122.3 ± 9.6 | 112.7 ± 11.9 | <0.0001 * |
| Diastolic blood pressure—mmHg | 78.0 ± 6.9 | 71.6 ± 7.6 | <0.0001 * |
| WBC | 5.6 ± 1.2 | 5.1 ± 1.3 | 0.0027 * |
| Hemoglobin | 15.3 ± 1.0 | 12.8 ± 1.2 | <0.0001 * |
| Platelet | 235.8 ± 47.1 | 258.3 ± 59.6 | 0.0007 * |
| BUN | 13.1 ± 3.8 | 10.8 ± 3.5 | <0.0001 * |
| Creatinine | 1.1 ± 0.2 | 0.8 ± 0.1 | <0.0001 * |
| FBS | 92.7 ± 8.9 (n = 128) | 88.2 ± 8.0 (n = 146) | <0.0001 * |
| HbA1c-% | 5.5 ± 0.5 (n = 102) | 5.3 ± 0.3 (n = 118) | 0.0078 * |
| CRP | 0.1 ± 0.3 (n = 123) | 0.1 ± 0.1 (n = 44) | 0.2013 * |
| Homocysteine-umol/L | 9.9 ± 2.8 (n = 50) | 7.1 ± 1.6 (n = 73) | <0.0001 * |
| Total cholesterol—mg/dL | 193.6 ± 23.1 | 185.4 ± 25.9 | 0.0062 * |
| LDL cholesterol—mg/dL | 124.7 ± 20.4 (n = 119) | 105.4 ± 22.7 (n = 144) | <0.0001 * |
| HDL cholesterol—mg/dL | 52.8 ± 9.9 | 66.3 ± 15.2 | <0.0001 * |
| N3ECD | Serum | Plasma | ||||
|---|---|---|---|---|---|---|
| r * | p Value | p Value † | r * | p Value | p Value † | |
| Demographic characteristics | ||||||
| Age | 0.1246 | 0.0376 | 0.4983 | −0.0684 | 0.2545 | 0.9836 |
| Sex | 0.2927 | 0.9869 | 0.8529 | 0.9992 | ||
| Height | −0.0588 | 0.3279 | 0.9874 | −0.0341 | 0.5704 | 0.9992 |
| Weight | −0.0790 | 0.1884 | 0.9644 | −0.0256 | 0.6696 | 0.9992 |
| Medical history | ||||||
| Smoking | 0.3366 | 0.9874 | 0.1253 | 0.9102 | ||
| Drinking | 0.9733 | 0.9989 | 0.5277 | 0.9992 | ||
| Laboratory values | ||||||
| Systolic blood pressure | −0.0809 | 0.1781 | 0.9644 | −0.0080 | 0.8898 | 0.9992 |
| Diastolic blood pressure | −0.0795 | 0.1853 | 0.9644 | −0.0380 | 0.5175 | 0.9992 |
| WBC | −0.0105 | 0.8619 | 0.9989 | 0.1056 | 0.0782 | 0.8038 |
| Hemoglobin | −0.1262 | 0.0352 | 0.4938 | −0.1076 | 0.2038 | 0.9672 |
| Platelet | 0.0228 | 0.7047 | 0.9989 | 0.0321 | 0.5925 | 0.9992 |
| BUN | 0.0337 | 0.5749 | 0.9989 | 0.0628 | 0.2958 | 0.9895 |
| Creatinine | 0.1579 | 0.0083 | 0.1535 | 0.0393 | 0.5130 | 0.9992 |
| FBS | −0.0409 | 0.4998 | 0.9980 | −0.0879 | 0.1467 | 0.9326 |
| HbA1c (ngsp) | −0.0070 | 0.9180 | 0.9989 | −0.0419 | 0.5361 | 0.9992 |
| CRP | 0.0330 | 0.5909 | 0.9989 | −0.0521 | 0.3952 | 0.9976 |
| Homocysteine | −0.0974 | 0.2837 | 0.9869 | −0.0710 | 0.4319 | 0.9980 |
| Total cholesterol | −0.0272 | 0.6506 | 0.9989 | −0.0819 | 0.1752 | 0.9541 |
| LDL cholesterol | −0.0788 | 0.2025 | 0.9644 | −0.0981 | 0.1100 | 0.8908 |
| HDL cholesterol | 0.0218 | 0.7170 | 0.9989 | 0.0141 | 0.8061 | 0.9992 |
| Jag-1 | Serum | Plasma | ||||
|---|---|---|---|---|---|---|
| r * | p Value | p Value † | r * | p Value | p Value † | |
| Demographic characteristics | ||||||
| Age | −0.1713 | 0.0041 | 0.0789 | −0.0129 | 0.0437 | 0.5722 |
| Sex | 0.9165 | 0.9914 | 0.3162 | 0.9895 | ||
| Height | −0.1027 | 0.0867 | 0.7340 | 0.0223 | 0.5808 | 0.9996 |
| Weight | −0.1035 | 0.0845 | 0.7340 | 0.0478 | 0.2362 | 0.9770 |
| Medical history | ||||||
| Smoking | 0.0726 | 0.7223 | 0.8214 | 0.9999 | ||
| Drinking | 0.5385 | 0.9903 | 0.7700 | 0.9999 | ||
| Laboratory values | ||||||
| Systolic blood pressure | −0.1268 | 0.0342 | 0.4838 | 0.0138 | 0.7355 | 0.9999 |
| Diastolic blood pressure | −0.1075 | 0.0730 | 0.7223 | 0.0248 | 0.5449 | 0.9996 |
| WBC | −0.0868 | 0.1483 | 0.8655 | 0.0273 | 0.5033 | 0.9995 |
| Hemoglobin | −0.0879 | 0.1430 | 0.8655 | 0.0479 | 0.2381 | 0.9770 |
| Platelet | 0.0878 | 0.1437 | 0.8655 | 0.0159 | 0.6939 | 0.9999 |
| BUN | −0.0424 | 0.4808 | 0.9898 | 0.0011 | 0.9785 | 0.9999 |
| Creatinine | 0.0182 | 0.7619 | 0.9914 | 0.1020 | 0.0132 | 0.2334 |
| FBS | −0.0141 | 0.8164 | 0.9914 | −0.0108 | 0.7942 | 0.9999 |
| HbA1c (ngsp) | −0.1340 | 0.0471 | 0.5804 | −0.0916 | 0.0532 | 0.6262 |
| CRP | −0.0712 | 0.2456 | 0.9403 | 0.0130 | 0.7601 | 0.9999 |
| Homocysteine | −0.0357 | 0.6954 | 0.9914 | −0.0071 | 0.9095 | 0.9999 |
| Total cholesterol | −0.0358 | 0.5516 | 0.9903 | 0.0547 | 0.1765 | 0.9457 |
| LDL cholesterol | −0.0551 | 0.3734 | 0.9762 | 0.0684 | 0.1012 | 0.8370 |
| HDL cholesterol | 0.0624 | 0.2992 | 0.9592 | −0.0622 | 0.1266 | 0.8853 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Jang, B.; Kim, Y.-J.; Choi, J.C. Determination of Blood NOTCH3 Extracellular Domain and Jagged-1 Levels in Healthy Subjects. Int. J. Mol. Sci. 2022, 23, 10547. https://doi.org/10.3390/ijms231810547
Kim H, Jang B, Kim Y-J, Choi JC. Determination of Blood NOTCH3 Extracellular Domain and Jagged-1 Levels in Healthy Subjects. International Journal of Molecular Sciences. 2022; 23(18):10547. https://doi.org/10.3390/ijms231810547
Chicago/Turabian StyleKim, Hyesung, Bogun Jang, Yang-Ji Kim, and Jay Chol Choi. 2022. "Determination of Blood NOTCH3 Extracellular Domain and Jagged-1 Levels in Healthy Subjects" International Journal of Molecular Sciences 23, no. 18: 10547. https://doi.org/10.3390/ijms231810547
APA StyleKim, H., Jang, B., Kim, Y.-J., & Choi, J. C. (2022). Determination of Blood NOTCH3 Extracellular Domain and Jagged-1 Levels in Healthy Subjects. International Journal of Molecular Sciences, 23(18), 10547. https://doi.org/10.3390/ijms231810547






