Development of a Novel, Genome Subtraction-Derived, SARS-CoV-2-Specific COVID-19-nsp2 Real-Time RT-PCR Assay and Its Evaluation Using Clinical Specimens
Abstract
:1. Introduction
2. Results
2.1. Species-Specific SARS-CoV-2 Genomic Regions Identified by GolayMetaMiner
2.2. Primer Selection for the SARS-CoV-2-Specific Real-Time RT-PCR Assay
2.3. Analytical Sensitivity of the Novel COVID-19-nsp2 Real-Time RT-PCR Assay
2.4. Analytical Specificity of the COVID-19-nsp2 Assay
2.5. Imprecision of the COVID-19-nsp2 Assay
2.6. Diagnostic Performance Evaluation of the COVID-19-nsp2 Assay for the Detection of SARS-CoV-2 RNA in Clinical Specimens
3. Discussion
4. Materials and Methods
4.1. SARS-CoV-2 Genome Subtraction Using GolayMetaMiner
4.2. Viruses and Clinical Specimens
4.3. Nucleic Acid Extraction and RT-PCR for SARS-CoV-2
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| COVID-19 | Novel coronavirus infection |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| WHO | World Health Organization |
| HCoV | Human coronavirus |
| SARS-CoV | Severe acute respiratory syndrome coronavirus |
| MERS-CoV | Middle East respiratory syndrome coronavirus |
| RT-PCR | Reverse transcription-polymerase chain reaction |
| NCBI | National Center for Biotechnology Information, USA |
| U-score(s) | Uniqueness score(s) |
| C-score(s) | Conservedness score(s) |
| LOD | Limit of detection |
| TNAnt | Total nucleic acidnucleotide |
References
- Chan, J.F.-W.; To, K.K.-W.; Tse, H.; Jin, D.-Y.; Yuen, K.-Y. Interspecies transmission and emergence of novel viruses: Lessons from bats and birds. Trends Microbiol. 2013, 21, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.C.; Lau, S.K.P.; Woo, P.C.Y.; Yuen, K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin. Microbiol. Rev. 2007, 20, 660–694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.W.; Lau, S.K.P.; To, K.K.W.; Cheng, V.C.C.; Woo, P.C.Y.; Yuen, K.-Y. Middle East respiratory syndrome coronavirus: Another zoonotic betacoronavirus causing SARS-like disease. Clin. Microbiol. Rev. 2015, 28, 465–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- WHO Announces COVID-19 Outbreak a pandemic. Available online: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 21 March 2020).
- Mizumoto, K.; Chowell, G. Estimating Risk for Death from 2019 Novel Coronavirus Disease, China, January-February 2020. Emerging Infect. Dis. 2020, 26, 6. [Google Scholar] [CrossRef]
- Cao, B.; Wang, Y.; Wen, D.; Liu, W.; Wang, J.; Fan, G.; Ruan, L.; Song, B.; Cai, Y.; Wei, M.; et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Li, H.; Wang, Y.M.; Xu, J.Y.; Cao, B. Potential antiviral therapeutics for 2019 Novel Coronavirus. Zhonghua Jie He He Hu Xi Za Zhi 2020, 43, 170–172. [Google Scholar]
- Martinez, M.A. Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob. Agents Chemother. 2020. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef]
- Roosa, K.; Lee, Y.; Luo, R.; Kirpich, A.; Rothenberg, R.; Hyman, J.M.; Yan, P.; Chowell, G. Real-time forecasts of the COVID-19 epidemic in China from February 5th to February 24th, 2020. Infect. Dis. Model. 2020, 5, 256–263. [Google Scholar] [CrossRef]
- Al-qaness, M.A.A.; Ewees, A.A.; Fan, H.; Abd El Aziz, M. Optimization Method for Forecasting Confirmed Cases of COVID-19 in China. J. Clin. Med. 2020, 9, 674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goh, G.K.-M.; Dunker, A.K.; Foster, J.A.; Uversky, V.N. Rigidity of the Outer Shell Predicted by a Protein Intrinsic Disorder Model Sheds Light on the COVID-19 (Wuhan-2019-nCoV) Infectivity. Biomolecules 2020, 10, 331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirouz, B.; Shaffiee Haghshenas, S.; Shaffiee Haghshenas, S.; Piro, P. Investigating a Serious Challenge in the Sustainable Development Process: Analysis of Confirmed cases of COVID-19 (New Type of Coronavirus) Through a Binary Classification Using Artificial Intelligence and Regression Analysis. Sustainability 2020, 12, 2427. [Google Scholar] [CrossRef] [Green Version]
- Salzberger, B.; Glück, T.; Ehrenstein, B. Successful containment of COVID-19: The WHO-Report on the COVID-19 outbreak in China. Infection 2020, 48, 151–153. [Google Scholar] [CrossRef] [Green Version]
- Cheng, V.C.C.; Wong, S.-C.; Chen, J.H.K.; Yip, C.C.Y.; Chuang, V.W.M.; Tsang, O.T.Y.; Sridhar, S.; Chan, J.F.W.; Ho, P.-L.; Yuen, K.-Y. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control. Hosp. Epidemiol. 2020, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.; Du, R.-H.; Li, B.; Zheng, X.-S.; Yang, X.-L.; Hu, B.; Wang, Y.-Y.; Xiao, G.-F.; Yan, B.; Shi, Z.-L.; et al. Molecular and serological investigation of 2019-nCoV infected patients: Implication of multiple shedding routes. Emerg. Microbes Infect. 2020, 9, 386–389. [Google Scholar] [CrossRef] [Green Version]
- Ling, Y.; Xu, S.-B.; Lin, Y.-X.; Tian, D.; Zhu, Z.-Q.; Dai, F.-H.; Wu, F.; Song, Z.-G.; Huang, W.; Chen, J.; et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin. Med. J. 2020. [Google Scholar] [CrossRef]
- To, K.K.-W.; Tsang, O.T.-Y.; Chik-Yan Yip, C.; Chan, K.-H.; Wu, T.-C.; Chan, J.M.C.; Leung, W.-S.; Chik, T.S.-H.; Choi, C.Y.-C.; Kandamby, D.H.; et al. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Woo, P.C.Y.; Lau, S.K.P.; Tsoi, H.; Chan, K.; Wong, B.H.L.; Che, X.; Tam, V.K.P.; Tam, S.C.F.; Cheng, V.C.C.; Hung, I.F.N.; et al. Relative rates of non-pneumonic SARS coronavirus infection and SARS coronavirus pneumonia. Lancet 2004, 363, 841–845. [Google Scholar] [CrossRef] [Green Version]
- Chan, J.F.-W.; Choi, G.K.-Y.; Tsang, A.K.-L.; Tee, K.-M.; Lam, H.-Y.; Yip, C.C.-Y.; To, K.K.-W.; Cheng, V.C.-C.; Yeung, M.-L.; Lau, S.K.-P.; et al. Development and Evaluation of Novel Real-Time Reverse Transcription-PCR Assays with Locked Nucleic Acid Probes Targeting Leader Sequences of Human-Pathogenic Coronaviruses. J. Clin. Microbiol. 2015, 53, 2722–2726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.-W.; Kok, K.-H.; Zhu, Z.; Chu, H.; To, K.K.-W.; Yuan, S.; Yuen, K.-Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 2020, 9, 221–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.-W.; Yip, C.C.-Y.; To, K.K.-W.; Tang, T.H.-C.; Wong, S.C.-Y.; Leung, K.-H.; Fung, A.Y.-F.; Ng, A.C.-K.; Zou, Z.; Tsoi, H.-W.; et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J. Clin. Microbiol. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, Z.; Xiao, Y.; Kang, L.; Ma, W.; Shi, L.; Zhang, L.; Zhou, Z.; Yang, J.; Zhong, J.; Yang, D.; et al. Genomic diversity of SARS-CoV-2 in Coronavirus Disease 2019 patients. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.W.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020, 25, 2000045. [Google Scholar] [CrossRef] [Green Version]
- Chu, D.K.W.; Pan, Y.; Cheng, S.M.S.; Hui, K.P.Y.; Krishnan, P.; Liu, Y.; Ng, D.Y.M.; Wan, C.K.C.; Yang, P.; Wang, Q.; et al. Molecular Diagnosis of a Novel Coronavirus (2019-nCoV) Causing an Outbreak of Pneumonia. Clin. Chem. 2020, 66, 549–555. [Google Scholar] [CrossRef] [Green Version]
- Yip, C.C.Y.; Sridhar, S.; Leung, K.-H.; Cheng, A.K.W.; Chan, K.-H.; Chan, J.F.W.; Cheng, V.C.C.; Yuen, K.-Y. Evaluation of RealStar® Alpha Herpesvirus PCR Kit for Detection of HSV-1, HSV-2, and VZV in Clinical Specimens. Biomed. Res. Int. 2019, 2019, 5715180. [Google Scholar] [CrossRef] [Green Version]
- Yip, C.C.Y.; Sridhar, S.; Cheng, A.K.W.; Fung, A.M.Y.; Cheng, V.C.C.; Chan, K.-H.; Yuen, K.-Y. Comparative evaluation of a laboratory developed real-time PCR assay and the RealStar® HHV-6 PCR Kit for quantitative detection of human herpesvirus 6. J. Virol. Methods 2017, 246, 112–116. [Google Scholar] [CrossRef]
- Angeletti, S.; Benvenuto, D.; Bianchi, M.; Giovanetti, M.; Pascarella, S.; Ciccozzi, M. COVID-2019: The role of the nsp2 and nsp3 in its pathogenesis. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [Green Version]
- To, K.K.-W.; Tsang, O.T.-Y.; Leung, W.-S.; Tam, A.R.; Wu, T.-C.; Lung, D.C.; Yip, C.C.-Y.; Cai, J.-P.; Chan, J.M.-C.; Chik, T.S.-H.; et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 2020, S1473309920301961. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Yi, Y.; Luo, X.; Xiong, N.; Liu, Y.; Li, S.; Sun, R.; Wang, Y.; Hu, B.; Chen, W.; et al. Development and Clinical Application of A Rapid IgM-IgG Combined Antibody Test for SARS-CoV-2 Infection Diagnosis. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Ren, L.; Yang, S.; Xiao, M.; Chang, D.; Yang, F.; Dela Cruz, C.S.; Wang, Y.; Wu, C.; Xiao, Y.; et al. Profiling Early Humoral Response to Diagnose Novel Coronavirus Disease (COVID-19). Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.-F.; Yan, K.; Ye, H.-H.; Lin, J.; Zheng, J.-J.; Cai, T. SARS-CoV-2 turned positive in a discharged patient with COVID-19 arouses concern regarding the present standard for discharge. Int. J. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Legido-Quigley, H.; Mateos-García, J.T.; Campos, V.R.; Gea-Sánchez, M.; Muntaner, C.; McKee, M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health 2020. [Google Scholar] [CrossRef] [Green Version]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020. [Google Scholar] [CrossRef]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Yip, C.C.Y.; Lam, C.S.F.; Luk, H.K.H.; Wong, E.Y.M.; Lee, R.A.; So, L.-Y.; Chan, K.-H.; Cheng, V.C.C.; Yuen, K.-Y.; Woo, P.C.Y.; et al. A six-year descriptive epidemiological study of human coronavirus infections in hospitalized patients in Hong Kong. Virol. Sin. 2016, 31, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Ho, C.-C.; Wu, A.K.L.; Tse, C.W.S.; Yuen, K.-Y.; Lau, S.K.P.; Woo, P.C.Y. Automated pangenomic analysis in target selection for PCR detection and identification of bacteria by use of ssGeneFinder Webserver and its application to Salmonella enterica serovar Typhi. J. Clin. Microbiol. 2012, 50, 1905–1911. [Google Scholar] [CrossRef] [Green Version]
- Ho, C.-C.; Yuen, K.-Y.; Lau, S.K.P.; Woo, P.C.Y. Rapid identification and validation of specific molecular targets for detection of Escherichia coli O104:H4 outbreak strain by use of high-throughput sequencing data from nine genomes. J. Clin. Microbiol. 2011, 49, 3714–3716. [Google Scholar] [CrossRef] [Green Version]
- Ho, C.-C.; Lau, C.C.Y.; Martelli, P.; Chan, S.-Y.; Tse, C.W.S.; Wu, A.K.L.; Yuen, K.-Y.; Lau, S.K.P.; Woo, P.C.Y. Novel pan-genomic analysis approach in target selection for multiplex PCR identification and detection of Burkholderia pseudomallei, Burkholderia thailandensis, and Burkholderia cepacia complex species: A proof-of-concept study. J. Clin. Microbiol. 2011, 49, 814–821. [Google Scholar] [CrossRef] [Green Version]
- Chu, H.; Chan, J.F.-W.; Yuen, T.T.; Shuai, H.; Yuan, S.; Wang, Y.; Hu, B.; Yip, C.C.-Y.; Tsang, J.O.-L.; Huang, X.; et al. An observational study on the comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV: Implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19. Lancet Microbe 2020, in press. [Google Scholar]
- Chan, J.F.-W.; Zhang, A.J.; Yuan, S.; Poon, V.K.-M.; Chan, C.C.-S.; Lee, A.C.-Y.; Chan, W.-M.; Fan, Z.; Tsoi, H.-W.; Wen, L.; et al. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamster model: Implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. 2020, ciaa325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yip, C.C.-Y.; Chan, W.-M.; Ip, J.D.; Seng, C.W.-M.; Leung, K.-H.; Poon, R.W.-S.; Ng, A.C.-K.; Wu, W.-L.; Zhao, H.; Chan, K.-H.; et al. Nanopore sequencing reveals novel targets for the diagnosis and surveillance of human and avian influenza A virus. J. Clin. Microbiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.S.Y.; Yip, C.C.Y.; Sridhar, S.; Leung, K.-H.; Cheng, A.K.W.; Fung, A.M.Y.; Lam, H.-Y.; Chan, K.-H.; Chan, J.F.W.; Cheng, V.C.C.; et al. Comparative evaluation of a laboratory-developed real-time PCR assay and RealStar® Adenovirus PCR Kit for quantitative detection of human adenovirus. Virol. J. 2018, 15, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, J.F.-W.; Yip, C.C.-Y.; Tee, K.-M.; Zhu, Z.; Tsang, J.O.-L.; Chik, K.K.-H.; Tsang, T.G.-W.; Chan, C.C.-S.; Poon, V.K.-M.; Sridhar, S.; et al. Improved detection of Zika virus RNA in human and animal specimens by a novel, highly sensitive and specific real-time RT-PCR assay targeting the 5′-untranslated region of Zika virus. Trop. Med. Int. Health 2017, 22, 594–603. [Google Scholar] [CrossRef] [PubMed]
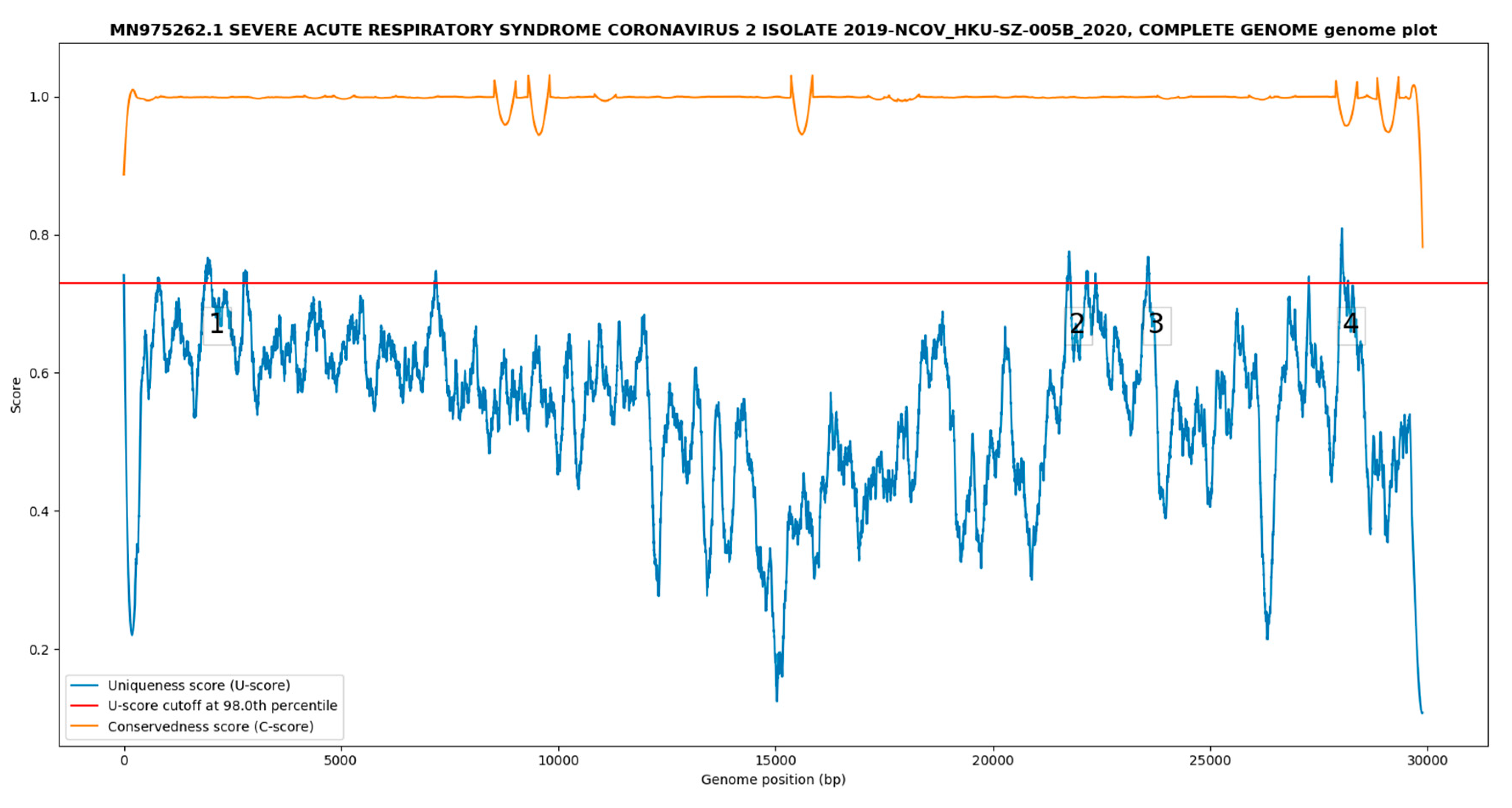
| Target | Nucleotide Position 1 | Target Length (nt) | Genomic Region |
|---|---|---|---|
| 1 | 1865–2018 | 154 | nsp2 |
| 2 | 21,731–21,788 | 58 | Spike |
| 3 | 23,536–23,598 | 63 | Spike |
| 4 | 27,997–28,909 | 93 | ORF8 |
| Virus Quantity (TCID50/mL) | Cp (Intra-Run) | Cp (Inter-Run) | ||||
|---|---|---|---|---|---|---|
| Test 1 | Test 2 | Test 3 | Test 1 | Test 2 | Test 3 | |
| 1.8 × 102 | 29.91 | 30.12 | 29.90 | 29.23 | 29.54 | 29.28 |
| 1.8 × 101 | 33.55 | 33.49 | 33.78 | 32.41 | 32.95 | 32.69 |
| 1.8 × 100 | 37.39 | 37.31 | 37.20 | 36.72 | 36.25 | 37.20 |
| 1.8 × 10−1 | - | - | - | - | 38.96 | - |
| Virus Quantity (TCID50/mL) | Intra-Assay | Inter-Assay | |
|---|---|---|---|
| No. of Positive Replicates | Mean Cp ± SD (% Coefficient of Variation) | Mean Cp ± SD (% Coefficient of Variation) | |
| 1.8 × 102 | 3 | 29.98 ± 0.12 (0.41) | 29.66 ± 0.37 (1.24) |
| 1.8 × 101 | 3 | 33.61 ± 0.15 (0.46) | 33.15 ± 0.54 (1.64) |
| 1.8 × 100 | 3 | 37.30 ± 0.10 (0.26) | 37.01 ± 0.44 (1.19) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yip, C.C.-Y.; Ho, C.-C.; Chan, J.F.-W.; To, K.K.-W.; Chan, H.S.-Y.; Wong, S.C.-Y.; Leung, K.-H.; Fung, A.Y.-F.; Ng, A.C.-K.; Zou, Z.; et al. Development of a Novel, Genome Subtraction-Derived, SARS-CoV-2-Specific COVID-19-nsp2 Real-Time RT-PCR Assay and Its Evaluation Using Clinical Specimens. Int. J. Mol. Sci. 2020, 21, 2574. https://doi.org/10.3390/ijms21072574
Yip CC-Y, Ho C-C, Chan JF-W, To KK-W, Chan HS-Y, Wong SC-Y, Leung K-H, Fung AY-F, Ng AC-K, Zou Z, et al. Development of a Novel, Genome Subtraction-Derived, SARS-CoV-2-Specific COVID-19-nsp2 Real-Time RT-PCR Assay and Its Evaluation Using Clinical Specimens. International Journal of Molecular Sciences. 2020; 21(7):2574. https://doi.org/10.3390/ijms21072574
Chicago/Turabian StyleYip, Cyril Chik-Yan, Chi-Chun Ho, Jasper Fuk-Woo Chan, Kelvin Kai-Wang To, Helen Shuk-Ying Chan, Sally Cheuk-Ying Wong, Kit-Hang Leung, Agnes Yim-Fong Fung, Anthony Chin-Ki Ng, Zijiao Zou, and et al. 2020. "Development of a Novel, Genome Subtraction-Derived, SARS-CoV-2-Specific COVID-19-nsp2 Real-Time RT-PCR Assay and Its Evaluation Using Clinical Specimens" International Journal of Molecular Sciences 21, no. 7: 2574. https://doi.org/10.3390/ijms21072574
APA StyleYip, C. C.-Y., Ho, C.-C., Chan, J. F.-W., To, K. K.-W., Chan, H. S.-Y., Wong, S. C.-Y., Leung, K.-H., Fung, A. Y.-F., Ng, A. C.-K., Zou, Z., Tam, A. R., Chung, T. W.-H., Chan, K.-H., Hung, I. F.-N., Cheng, V. C.-C., Tsang, O. T.-Y., Tsui, S. K. W., & Yuen, K.-Y. (2020). Development of a Novel, Genome Subtraction-Derived, SARS-CoV-2-Specific COVID-19-nsp2 Real-Time RT-PCR Assay and Its Evaluation Using Clinical Specimens. International Journal of Molecular Sciences, 21(7), 2574. https://doi.org/10.3390/ijms21072574









