Biomedical Applications of Scutellaria edelbergii Rech. f.: In Vitro and In Vivo Approach
Abstract
1. Introduction
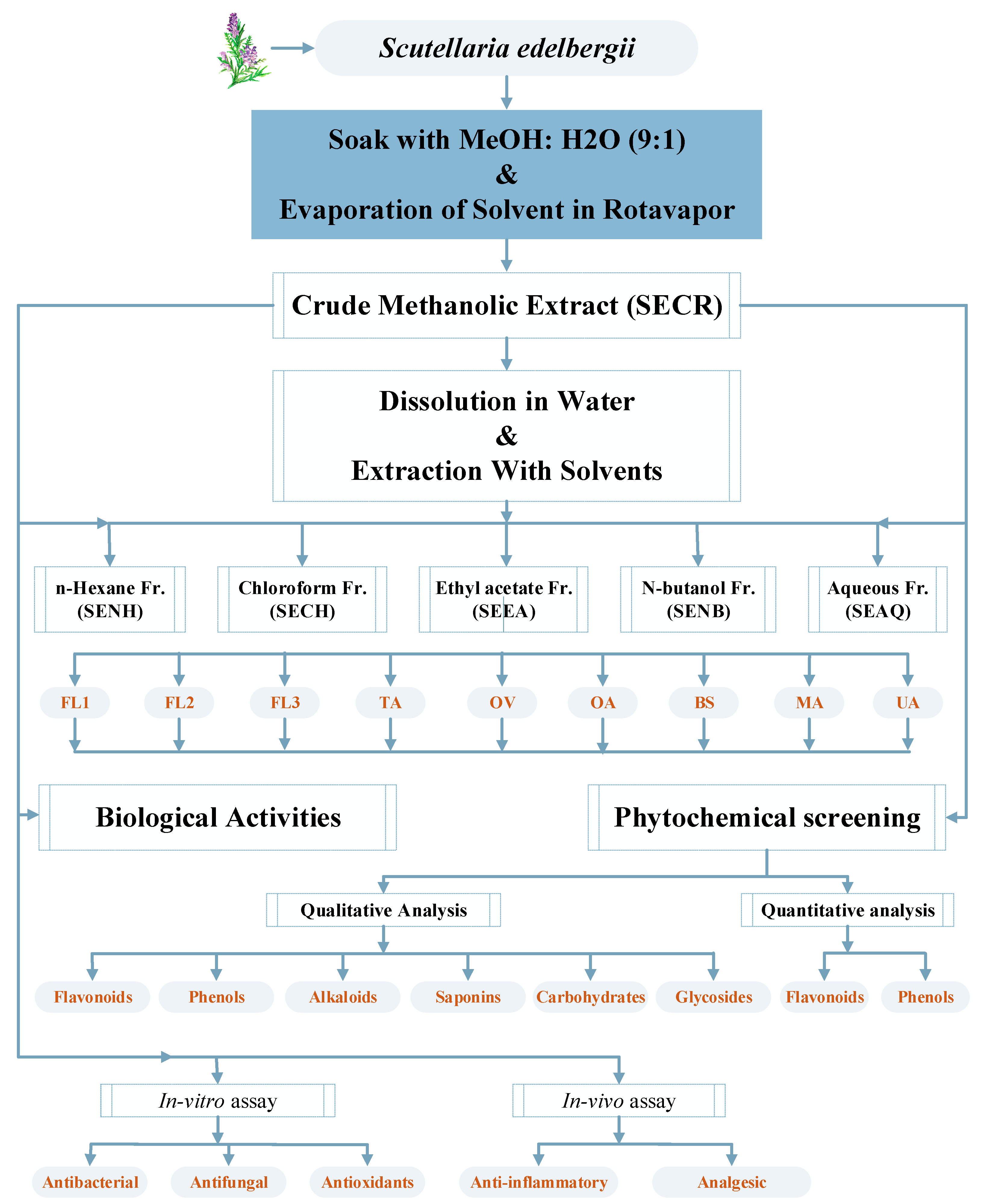
2. Results and Discussion
2.1. Qualitative Phytochemical Analysis of Extracts
2.2. Phenolic and Flavonoids Contents
2.3. Antibacterial Activity
2.4. Antifungal Activities
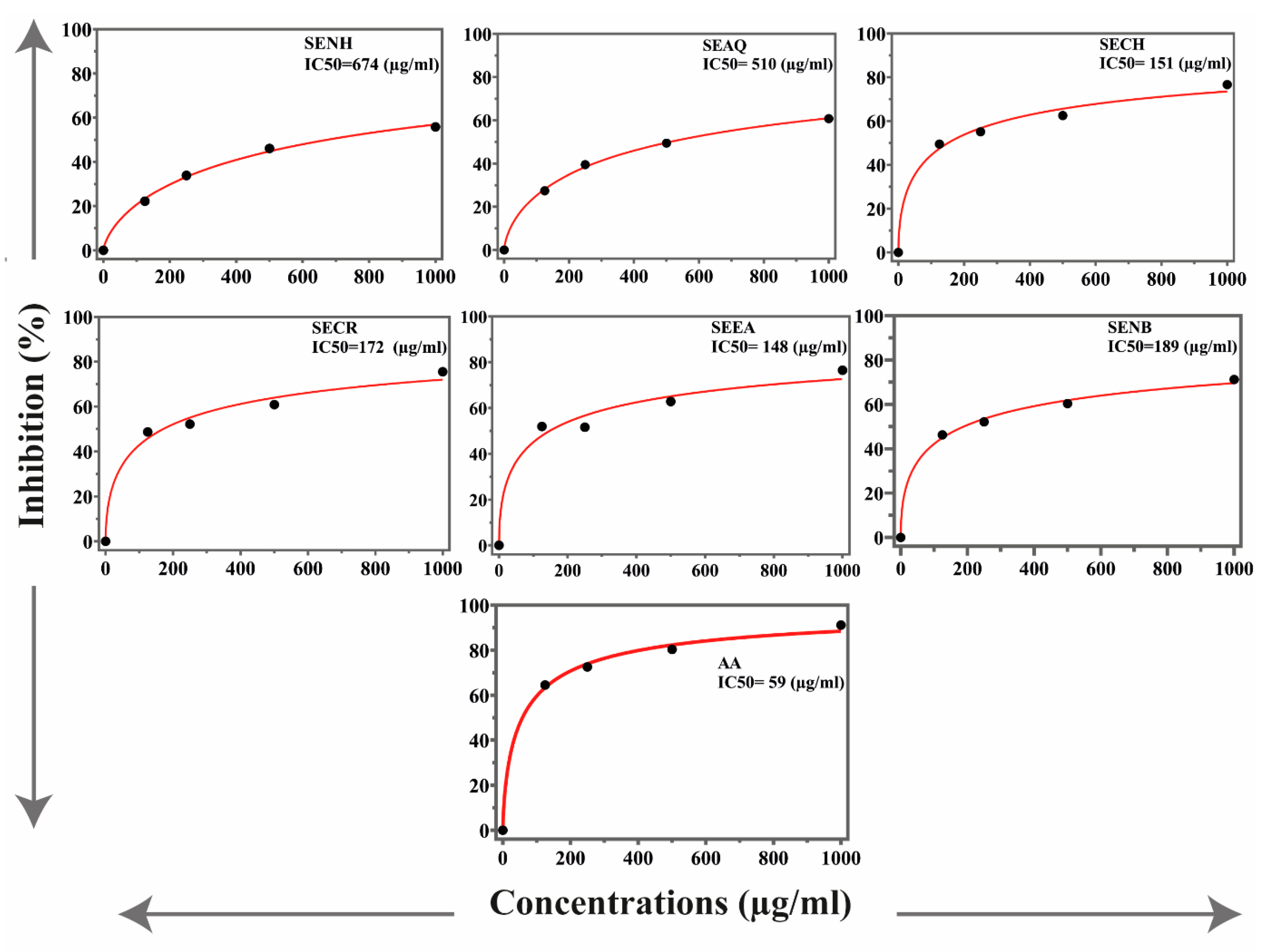
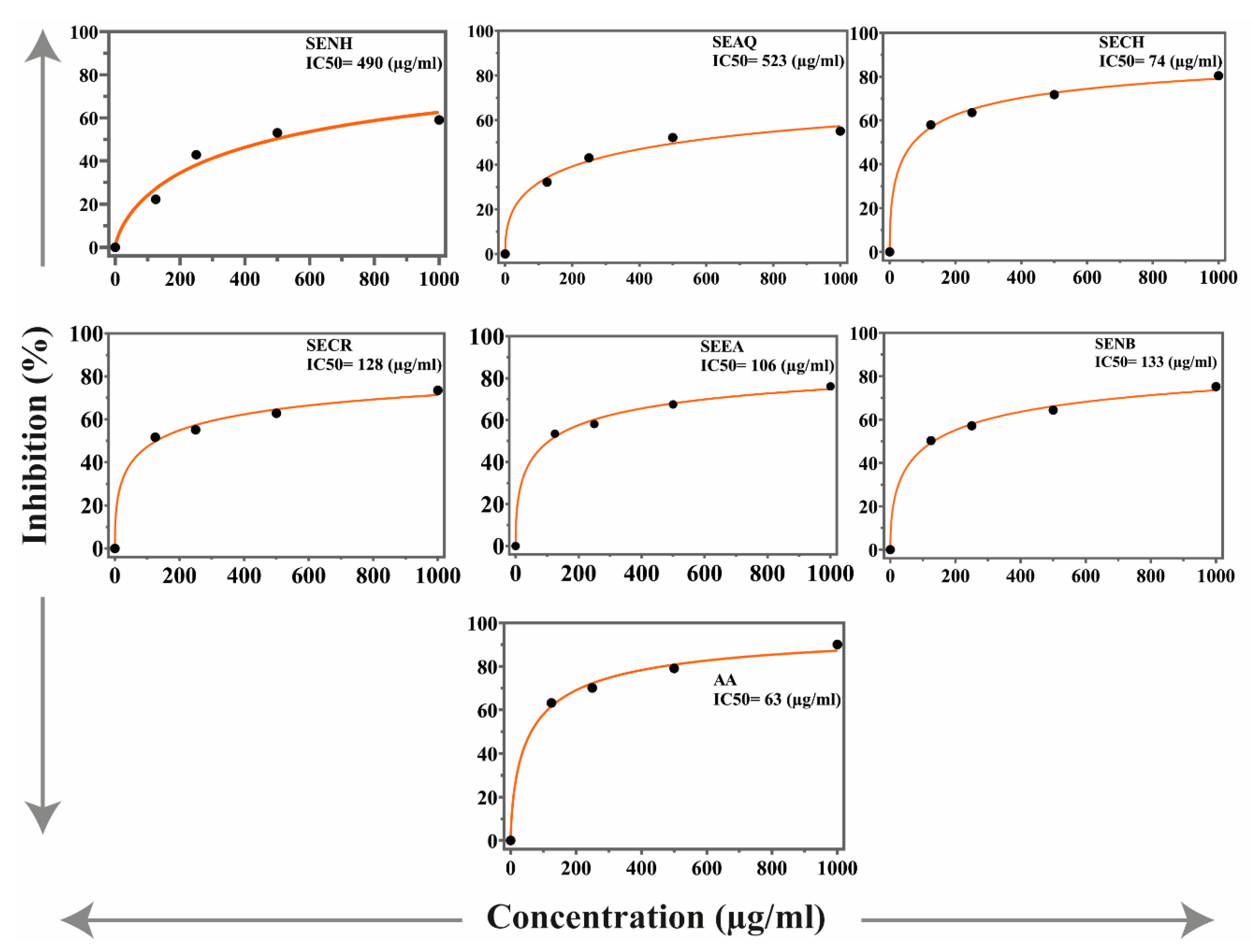
2.5. Antioxidant Activities
2.6. Anti-Inflammatory Activities
2.7. Analgesic Activity
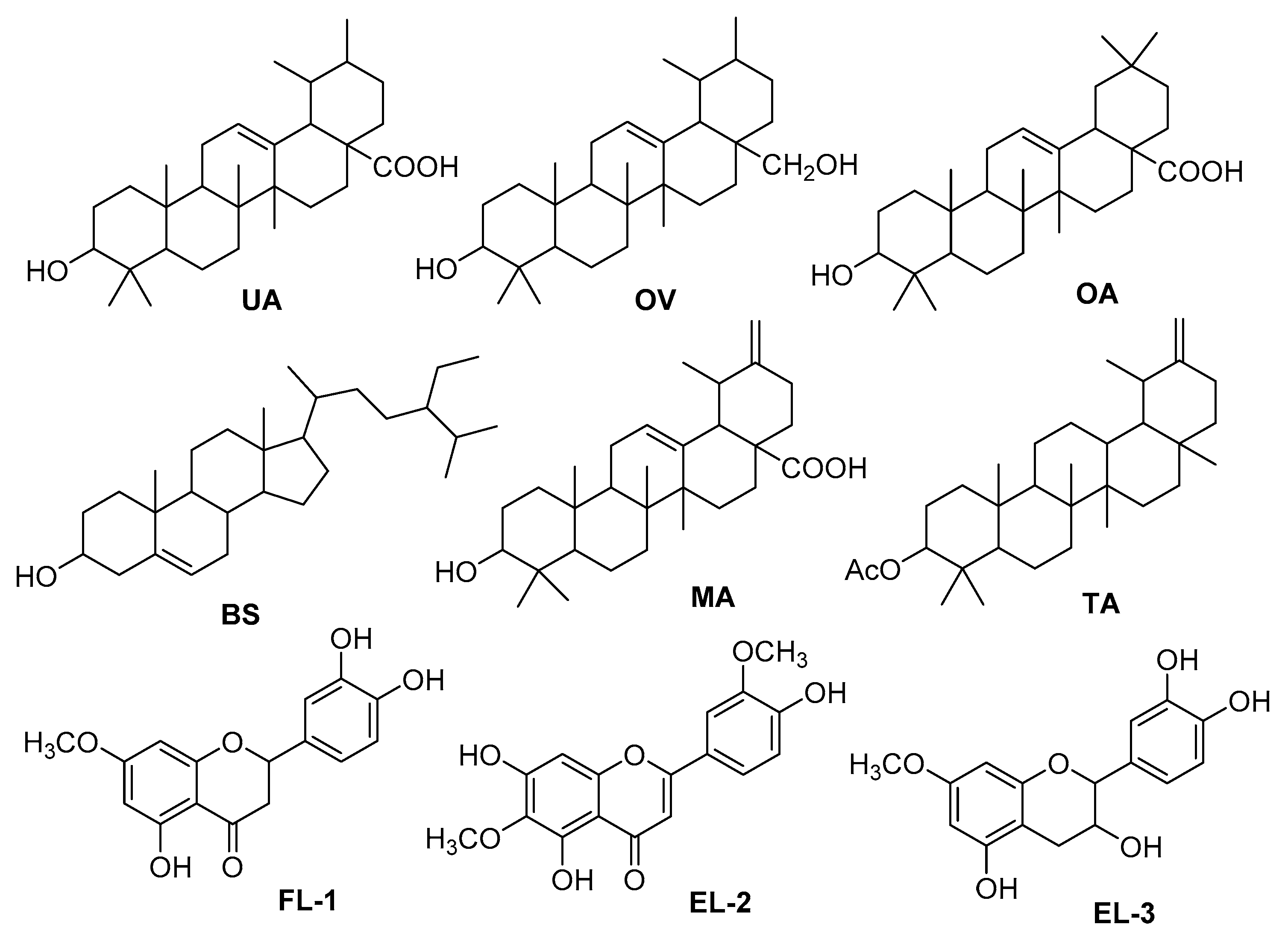
2.8. Isolation of Known Compounds
3. Material and Methods
3.1. General Instrumentation
3.2. Plant Collection and Identification
3.3. Extraction and Fractionation
3.4. Preliminary Phytochemical Analysis
3.4.1. Flavonoids
3.4.2. Phenols
3.4.3. Alkaloids
3.4.4. Saponins
3.4.5. Carbohydrates
3.4.6. Glycosides
3.4.7. Flavonoids and Phenolic Contents
3.4.8. Estimation of Total Phenolic Contents
3.4.9. Quantification of Total Flavonoid Contents
3.5. In Vitro Biological Activities
3.5.1. Antibacterial Activities
3.5.2. Antifungal Activity
3.5.3. Antioxidant Activity (DPPH and ABTS)
3.6. In Vivo Pharmacological Activities
3.6.1. Experimental Animals
3.6.2. Anti-Inflammatory Activities
3.6.3. Analgesic Activities
3.7. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Khan, I.; Zahoor, M.; Zeb, A.; Ul Bari, W. In Vitro Antioxidant, Antidiabetic, and Anticholinesterase, and In Vivo Toxicological, Hypoglycemic, and Antilipidemic Potentials of Ziziphus oxyphylla. Lat. Am. J. Pharm. 2020, 39, 7–21. [Google Scholar]
- Khan, H.; Saeed, M.; Mehmood, M.H.; Rehman, N.U.; Muhammad, N.; Haq, I.U.; Ashraf, N.; El-Tahir, K.E.H.; Gilani, A.-H. Studies on tracheorelaxant and anti-inflammatory activities of rhizomes of Polygonatum verticillatum. BMC Complement. Altern. Med. 2013, 13, 197. [Google Scholar] [CrossRef] [PubMed]
- Zahoor, M.; Khan, I.; Zeb, A.; Sahibzada, M.U.; Naz, S.; Bari, W.U.; Kamran, A.W. Pharmacological evaluation and in-silico modeling study of compounds isolated from Ziziphus oxyphylla. Heliyon 2021, 7, e06367. [Google Scholar] [CrossRef] [PubMed]
- Zahoor, M.; Bari, W.U.; Zeb, A.; Khan, I. Toxicological, anticholinesterase, antilipidemic, antidiabetic and antioxidant potentials of Grewia optiva Drummond ex Burret extracts. J. Basic Clin. Physiol. Pharmacol. 2020, 31. [Google Scholar] [CrossRef] [PubMed]
- Nazir, N.; Zahoor, M.; Nisar, M.; Karim, N.; Latif, A.; Ahmad, S.; Uddin, Z. Evaluation of neuroprotective and anti-amnesic effects of Elaeagnus umbellata Thunb. On scopolamine-induced memory impairment in mice. BMC Complement. Med. Ther. 2020, 20, 143. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.N.M.; Delazar, A.; Nazemiyeh, H.; Khodaie, L. Biological Activity and Phytochemical Study of Scutellaria platystegia. Iran. J. Pharm. Res. 2015, 14, 215–223. [Google Scholar]
- Iqbal, N.; Hussain, S.; Ahmed, Z.; Yang, F.; Wang, X.; Liu, W.; Yong, T.; Du, J.; Shu, K.; Yang, W.; et al. Comparative analysis of maize–soybean strip intercropping systems: A review. Plant Prod. Sci. 2019, 22, 131–142. [Google Scholar] [CrossRef]
- Herridge, W.P.; Shibu, P.; O’Shea, J.; Brook, T.C.; Hoyles, L. Bacteriophages of Klebsiella spp., their diversity and potential therapeutic uses. J. Med. Microbiol. 2020, 69, 176–194. [Google Scholar] [PubMed]
- Ikram, M.; Beshbishy, A.M.; Kifayatullah, M.; Olukanni, A.; Zahoor, M.; Naeem, M.; Amin, M.; Shah, M.; Abdelaziz, A.S.; Ullah, R.; et al. Chemotherapeutic potential of carthamus oxycantha root extract as antidiarrheal and in vitro antibacterial activities. Antibiotics 2020, 9, 226. [Google Scholar] [CrossRef]
- Kim, M.; Jo, Y.; Hwang, Y.J.; Hong, H.W.; Hong, S.S.; Park, K.; Myung, H. Phage-antibiotic synergy via delayed lysis. Appl. Environ. Microbiol. 2018, 84, e02085-18. [Google Scholar] [CrossRef]
- Zahoor, M.; Ahmed, M.; Naz, S.; Ayaz, M. Cytotoxic, Antibacterial and antioxidant activities of extracts of the bark of Melia azedarach (China Berry). Nat. Prod. Res. 2015, 29, 1170–1172. [Google Scholar] [CrossRef]
- Nazir, N.; Jan, M.R.; Ali, A.; Asif, M.; Idrees, M.; Nisar, M.; Zahoor, M.; Abd El-Salam, N.M. Prevalence of hepatitis-C virus genotypes and potential transmission risks in Malakand Khyber Pakhtunkhwa, Pakistan. Virol. J. 2017, 14, 160. [Google Scholar] [CrossRef] [PubMed]
- Bari, W.U.; Zahoor, M.; Zeb, A.; Khan, I.; Nazir, Y.; Khan, A.; Rehman, N.U.; Ullah, R.; Shahat, A.A.; Mahmood, H.M. Anticholinesterase, Antioxidant potentials, and molecular docking studies of isolated bioactive compounds from Grewia optiva. Int. J. Food Prop. 2019, 22, 1386–1396. [Google Scholar] [CrossRef]
- Hassan, G.S.; Abdel Rahman, D.E.; Abdelmajeed, E.A.; Refaey, R.H.; Alaraby Salem, M.; Nissan, Y.M. New pyrazole derivatives: Synthesis, Anti-inflammatory activity, cyclooxygenase inhibition assay and evaluation of mPGES. Eur. J. Med. Chem. 2019, 171, 332–342. [Google Scholar] [CrossRef] [PubMed]
- Bardakci, H.; Türköz Acar, E.; Kırmızıbekmez, H. Simultaneous quantification of six phenylethanoid glycosides in some Turkish Scutellaria species by a new HPLC-DAD method. Nat. Prod. Res. 2019, 33, 2116–2119. [Google Scholar] [CrossRef]
- Swati Paul, D.S. Analgesic Activity of Methanol Extract of Plumbago indica (L.) by Acetic Acid-Induced Writhing Method. Asian J. Pharm. Tech. 2012, 2, 74–76. [Google Scholar]
- Miyaichi, Y.; Imoto, Y.; Tomimori, T.; Lin, C.C. Studies on the constituents of Scutellaria species. IX. On the flavonoid constituents of the root of Scutellaria indica L. Chem. Pharm. Bull. 1987, 35, 3720–3725. [Google Scholar] [CrossRef]
- Gupta, D.; Dubey, J.; Kumar, M. Phytochemical analysis and antimicrobial activity of some medicinal plants against selected common human pathogenic microorganisms. Asian Pac. J. Trop. Dis. 2016, 6, 15–20. [Google Scholar] [CrossRef]
- Zeng, J.; Ma, R.-J.; Wang, L.; Zhang, S.-N.; Song, H.-Z.; Yang, Y.; Tan, Q.-G. Chemical constituents from the leaves of Melia azedarach. Nat. Prod. Res. 2019, 33, 2860–2863. [Google Scholar] [CrossRef]
- Dai, S.J.; Tao, J.Y.; Liu, K.; Jiang, Y.T.; Shen, L. neo-Clerodane diterpenoids from Scutellaria barbata with cytotoxic activities. Phytochemistry 2006, 67, 1326–1330. [Google Scholar] [CrossRef]
- Wang, Z.L.; Wang, S.; Kuang, Y.; Hu, Z.M.; Qiao, X.; Ye, M. A comprehensive review on phytochemistry, Pharmacology, and flavonoid biosynthesis of Scutellaria baicalensis. Pharm. Biol. 2018, 56, 465–484. [Google Scholar] [CrossRef]
- Kowalczyk, E.; Krzesiński, P.; Kura, M.; Niedworok, J.; Blaszczyk, J. Pharmacological effects of flavonoids from Scutellaria baicalensis. Prz. Lek. 2006, 63, 95–96. [Google Scholar]
- Zahoor, M.; Shah, A.; Gul, S.; Amin, S. HPLC-UV analysis of antioxidants in Citrus sinensis stem and root extracts. J. Chem. Soc. Pak. 2018, 40, 595–601. [Google Scholar]
- Zahoor, M. Biological and phytochemical evaluation of Cotoneaster microphyllus, Ficus auriculata and Calotropis procera. Lat. Am. J. Pharm. 2019, 38, 945–953. [Google Scholar]
- Marrero Delange, D.; Morales Rico, C.; Canavaciolo, C.V.L.; Oliver, E.S.; Pérez, R.C.; Rodríguez-Leyes, E.; Vicente Murillo, R. Phytochemical screening of Scutellaria havanensis Jacq. Rev. Cuba. Plantas Med. 2012, 17, 402–407. [Google Scholar]
- Liu, H.-L.; Kao, T.-H.; Shiau, C.-Y.; Chen, B.-H. Functional components in Scutellaria barbata D. Don with anti-inflammatory activity on RAW 264.7 cells. J. Food Drug Anal. 2018, 26, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Gharari, Z.; Aghajanzadeh, M.; Sharafi, A. Scutellaria orientalis subsp. Bornmuelleri: Phytochemical composition and biological activities. Nat. Prod. Res. 2021, 1–6. [Google Scholar] [CrossRef]
- Ozkul, C.; Renda, G.; Ekizoglu, M.; EZER, N.; Arıtuluk, Z. Antimicrobial activity of three Scutellaria L. species from Turkey. J. Res. Pharm. 2019, 23, 552–558. [Google Scholar] [CrossRef]
- Yilmaz, G.; Şimşek, D.; Altanlar, N.; Çiçek, M. Comparison of the antimicrobial activity of some Scutellaria orientalis L. taxa growing in Turkey. Int. J. Second. Metab. 2020, 192–199. [Google Scholar] [CrossRef]
- Shi, G.-X.; Shao, J.; Wang, T.-M.; Wang, C.Z. New advance in studies on antimicrobal activity of Scutellaria baicalensis and its effective ingredients. Zhongguo Zhong Yao Za Zhi 2014, 39, 3713–3718. [Google Scholar]
- Vergun, O.; Svydenko, L.; Grygorieva, O.; Shymanska, O.; Rakhmetov, D.; Brindza, J.; Ivanišová, E. Antioxidant capacity of plant raw material of Scutellaria baicalensis Georgi. Potravin. Slovak J. Food Sci. 2019, 1, 614–621. [Google Scholar] [CrossRef]
- Grzegorczyk-Karolak, I.; Kuźma, Ł.; Wysokińska, H. Study on the chemical composition and antioxidant activity of extracts from shoot culture and regenerated plants of Scutellaria altissima L. Acta Physiol. Plant. 2015, 37, 1736. [Google Scholar] [CrossRef]
- Delazar, A.; Nazemiyeh, H.; Afshar, F.H.; Barghi, N.; Esnaashari, S.; Asgharian, P. Chemical compositions and biological activities of Scutellaria pinnatifida A. Hamilt aerial parts. Res. Pharm. Sci. 2017, 12, 187–195. [Google Scholar] [PubMed]
- Zengin, G.; Llorent-Martínez, E.; García, L.; de Cordova, M.L.; Aktumsek, A.; Uysal, S.; Rengasamy, K.; Aumeeruddy, M.; Bahadori, M.B.; Mahomoodally, F. Chemical profile, Antioxidant, and enzyme inhibitory properties of two Scutellaria species: S. orientalis L. and S. salviifolia Benth. J. Pharm. Pharmacol. 2019, 71, 270–280. [Google Scholar] [CrossRef]
- Lee, J.K.; Song, Y.K.; Lim, H.H. Analgesic and anti-Inflammatory effect of Scutellaria baicalensis. J. Korean Med. 2007, 28, 124–135. [Google Scholar]
- Kim, E.H.; Shim, B.; Kang, S.; Jeong, G.; Lee, J.; Yu, Y.-B.; Chun, M. Anti-inflammatory effects of Scutellaria baicalensis extract via suppression of immune modulators and MAP kinase signaling molecules. J. Ethnopharmacol. 2009, 126, 320–331. [Google Scholar] [CrossRef]
- Yimam, M.; Brownell, L.; Hodges, M.; Jia, Q. Analgesic effects of a standardized bioflavonoid composition from Scutellaria baicalensis and Acacia catechu. J. Diet. Suppl. 2012, 9, 155–165. [Google Scholar] [CrossRef]
- Miyaichi, Y.; Ishii, K.; Kuno, T.; Tomimori, T. Studies on the Constituents of Scutellaria Species XX: Constituents of roots of Scutellaria strigillosa Hemsley. Nat. Med. 1999, 53, 237–241. [Google Scholar]
- Miyaichi, Y.; Morimoto, T.; Yaguchi, K.; Kizu, H. Studies on the constituents of Scutellaria species (XXI): Constituents of the leaves of Scutellaria strigillosa Hemsley. J. Nat. Med. 2006, 60, 157–158. [Google Scholar] [CrossRef]
- Stojakowska, A.; Kisiel, W. Secondary metabolites from a callus culture of Scutellaria columnae. Fitoterapia 1999, 70, 324–325. [Google Scholar] [CrossRef]
- Shang, X.; He, X.; He, X.; Li, M.; Zhang, R.; Fan, P.; Zhang, Q.; Jia, Z. The genus Scutellaria an ethnopharmacological and phytochemical review. J. Ethnopharmacol. 2010, 128, 279–313. [Google Scholar] [CrossRef]
- Altinier, G.; Sosa, S.; Aquino, R.P.; Mencherini, T.; Loggia, R.D.; Tubaro, A. Characterization of topical antiinflammatory compounds in Rosmarinus officinalis L. J. Agric. Food Chem. 2007, 55, 1718–1723. [Google Scholar] [CrossRef]
- Maria, F.; Kabouche, Z.; Fujimoto, Y.; Araya, H. Two new triterpenes and other compounds from Mentha aquatica (Lamiaceae). Nat. Prod. Commun. 2017, 12, 483–486. [Google Scholar] [CrossRef]
- Babaamer, Z.; Sekhri, L.; Al-Jaber, H.; Al-Qudah, M.; Abu Zarga, M. Extraction and identification of triterpenoids from Pergularia Tomentosa L. Ann. Sci. Technol. 2013, 5, 1–5. [Google Scholar] [CrossRef]
- Silva, L.; Strapasson, R.; Riva, D.; Salvador, M.; Stefanello, M.É. Triterpenes from the flowers of Gochnatia polymorpha subsp. floccosa. Rev. Bras. Farmacogn. 2011, 21, 556–559. [Google Scholar] [CrossRef]
- Bano, Z.; Begum, S.; Ali, S.S.; Kiran, Z.; Siddiqui, B.S.; Ahmed, A.; Khawaja, S.; Fatima, F.; Jabeen, A. Phytochemicals from Carissa carandas with potent cytotoxic and anti-inflammatory activities. Nat. Prod. Res. 2021, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, e47. [Google Scholar] [CrossRef] [PubMed]
- Hussain, J.; Rehman, N.U.; Khan, A.L.; Ali, L.; Kim, J.-S.; Zakarova, A.; Al-Harrasi, A.; Shinwari, Z.K. Phytochemical and biological assessment of medicinally important plant Ochradenus arabicus. Pak. J. Bot. 2014, 46, 2027–2034. [Google Scholar]
- Havsteen, B. The biochemistry and medical significance of the flavonoids. Pharmacol. Ther. 2002, 96, 67–202. [Google Scholar] [CrossRef]
- Georgieva, Y.; Katsarova, M.; Stoyanov, P.; Mladenov, R.; Denev, P.; Teneva, D.; Plotnikov, E.; Bozov, P.; Dimitrova, S. Metabolite profile and antioxidant activity of some species of Genus Scutellaria growing in Bulgaria. Plants 2021, 10, 45. [Google Scholar] [CrossRef]
- Chen, S.; Yuan, Y.; Luo, Y.; Huang, L.; Chen, P.; Li, X. Effects of light on flavonoids accumulation and related gene expression in suspension cultures of Scutellaria baicalensis. Zhongguo Zhong Yao Za. Zhi. 2010, 35, 682–685. [Google Scholar]
- Vaidya, B.N.; Brearley, T.A.; Joshee, N. Antioxidant capacity of fresh and dry leaf extracts of sixteen Scutellaria species. J. Med. Act. Plants 2014, 2, 42–49. [Google Scholar]
- Matsa, M.; Bardakci, H.; Gousiadou, C.; Kirmizibekmez, H.; Skaltsa, H. Secondary metabolites from Scutellaria albida L. ssp. velenovskyi (Rech. f.) Greuter & Burdet. Biochem. Syst. Ecol. 2019, 83, 71–76. [Google Scholar]
- Marzouk, A. Hepatoprotective Triterpenes from Hairy Root Cultures of Ocimum basilicum L. Z. Naturforschung C 2009, 64, 201–209. [Google Scholar] [CrossRef]
- Ododo, M.M.; Choudhury, M.K.; Dekebo, A.H. Structure elucidation of β-sitosterol with antibacterial activity from the root bark of Malva parviflora. Springerplus 2016, 5, 1210. [Google Scholar] [CrossRef]
- Vasconcelos, J.M.J.; Silva, A.M.S.; Cavaleiro, J.A.S. Chromones and flavanones from artemisia campestris subsp. maritima. Phytochemistry 1998, 49, 1421–1424. [Google Scholar] [CrossRef]
- Chuang, T.-H.; Chan, H.-H.; Wu, T.-S.; Li, C.-F. Chemical constituents and biological studies of the leaves of Grevillea robusta. Molecules 2011, 16, 9331–9339. [Google Scholar] [CrossRef] [PubMed]
- Mossa, J.S.; Sattar, E.A.; Abou-Shoer, M.; Galal, A.M. Free Flavonoids from Rhus retinorrhoea Steud, ex Olive. Int. J. Pharmacogn. 1996, 34, 198–201. [Google Scholar] [CrossRef]
- Wang, Y.; Qing, W.-X.; Li, L.-X.; Zhao, D.-B.; Liu, X.-H. Isolation and identification of 5,3’,4’-Trihydroxy-7-methoxyflavanone from Artemisia sphaerocephala Kraschen. Jiegou Huaxue 2014, 33, 199–203. [Google Scholar]
- Medjroubi, K.; Mezhoud, S.; Benayache, F.; Seguin, E.; Tillequin, F. Flavonoids of the aerial part of Centaurea pullata. Chem. Nat. Compd. 2005, 41, 226–227. [Google Scholar] [CrossRef]
- Sadhu, S.K.; Hirata, K.; Li, X.; Ohtsuki, T.; Koyano, T.; Preeprame, S.; Kowithayakorn, T.; Ishibashi, M. Flavonoids and sesquiterpenoids, constituents from Eupatorium capillifolium, found in a screening study guided by cell growth inhibitory activity. J. Nat. Med. 2006, 60, 325–328. [Google Scholar] [CrossRef]
- Martínez, V.; Barberá, O.; Sánchez-Parareda, J.; Alberto Marco, J. Phenolic and acetylenic metabolites from Artemisia assoana. Phytochemistry 1987, 26, 2619–2624. [Google Scholar] [CrossRef]
- Ara, A.; Saleh-E-In, M.M.; Ahmad, M.; Hashem, M.A.; Hasan, C.M. Isolation and Characterization of Compounds from the Methanolic Bark Extract of Adenanthera pavonina L. Anal. Chem. Lett. 2020, 10, 49–59. [Google Scholar] [CrossRef]
- Bilia, A.R.; Morelli, I.; Hamburger, M.; Hostetmann, K. Flavans and A-type proanthocyanidins from Prunus prostrata. Phytochemistry 1996, 43, 887–892. [Google Scholar] [CrossRef]
- Kang, J.; Price, W.E.; Ashton, J.; Tapsell, L.C.; Johnson, S. Identification and characterization of phenolic compounds in hydromethanolic extracts of sorghum wholegrains by LC-ESI-MSn. Food Chem. 2016, 211, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Gul, R.; Jan, S.U.; Faridullah, S.; Sherani, S.; Jahan, N. Preliminary Phytochemical screening, quantitative analysis of alkaloids, and antioxidant activity of crude plant extracts from Ephedra intermedia indigenous to Balochistan. Sci. World J. 2017, 2017, 5873648. [Google Scholar] [CrossRef]
- Auwal, M.S.; Saka, S.; Mairiga, I.; Sanda, K.A.; Shuaibu, A.; Ibrahim Dirar, A. Preliminary phytochemical and elemental analysis of aqueous and fractionated pod extracts of Acacia nilotica (Thorn mimosa). Vet. Res. Forum. 2014, 5, 95–100. [Google Scholar]
- Mohamed amine, G.; Telli, A.; Hiba, G.; Aminata, K. Phytochemical screening, antifungal, and antioxidant activities of three medicinal plants from Algerian steppe and Sahara (preliminary screening studies). SN Appl. Sci. 2019, 1, 1–13. [Google Scholar] [CrossRef]
- Saleem, A.; Saleem, M.; Akhtar, M.; Sharif, A.; Javaid, Z.; Sohail, K. In vitro and in vivo anti-arthritic evaluation of Polystichum braunii to validate its folkloric claim. Pak. J. Pharm. Sci. 2019, 32, 1167–1173. [Google Scholar]
- Cazella, L.N.; Glamoclija, J.; Soković, M.; Gonçalves, J.E.; Linde, G.A.; Colauto, N.B.; Gazim, Z.C. Antimicrobial activity of essential oil of Baccharis dracunculifolia DC (Asteraceae) aerial parts at flowering period. Front. Plant Sci. 2019, 10, 27. [Google Scholar] [CrossRef]
- Kedare, S.B.; Singh, R.P. Genesis and development of DPPH method of antioxidant assay. J. Food Sci. Technol. 2011, 48, 412–422. [Google Scholar] [CrossRef] [PubMed]
- Du Sert, N.P.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; Emerson, M.; et al. Reporting animal research: Explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. 2020, 18, e3000411. [Google Scholar] [CrossRef]
| Fractions | Flavonoids | Phenols | Alkaloids | Saponins | Carbohydrates | Glycosides |
|---|---|---|---|---|---|---|
| SENH | - | + | - | - | - | - |
| SEAQ | + | + | + | + | + | + |
| SECH | + | + | + | - | - | - |
| SENB | + | + | + | + | + | + |
| SEEA | + | + | + | + | + | + |
| SECR | + | + | + | + | + | + |
| Fractions | Total Phenolic Contents (mg GAE/g) Dry Fractions Mean ± SEM | Total Flavonoid Contents (mg QE/mg) of Dry Fractions Mean ± SEM |
|---|---|---|
| SENH | 36.5 ± 0.11 ** | 41.0 ± 0.29 ** |
| SEAQ | 49.3 ± 0.11 ** | 52.5 ± 0.37 ** |
| SECH | 58.1 ± 0.14 ** | 64.0 ± 0.37 ** |
| SENB | 64.5 ± 0.17 ** | 75.4 ± 0.28 ** |
| SEEA | 79.2 ± 0.30 ** | 84.0 ± 0.39 ** |
| SECR | 69.9 ± 0.13 ** | 80.5 ± 0.42 ** |
| Antibacterial Activities of Extracts and Fractions against Gram-Negative Bacterial Strains | ||||
| Fractions | Escherichia coli | Klebsiella pneumonia | ||
| C1 | C2 | C1 | C2 | |
| SECR | 12.3 ± 0.02 * | 16.3 ± 0.03 * | 13.6 ± 0.04 * | 16.6 ± 0.05 * |
| SEEA | 14.5 ± 0.04 * | 17.9 ± 0.03 * | 14.3 ± 0.02 * | 17.3 ± 0.02 * |
| SECH | 13.6 ± 0.01 * | 16.3 ± 0.02 * | 13.9 ± 0.05 * | 16.6 ± 0.01 * |
| SENB | 13.3 ± 0.03 * | 16.6 ± 0.04 * | 12.6 ± 0.03 * | 16.3 ± 0.04 * |
| SENH | 12.6 ± 0.02 * | 15.6 ± 0.01 * | 12.3 ± 0.04 * | 15.3 ± 0.01 * |
| SEAQ | 12.3 ± 0.01 * | 15.3 ± 0.01 * | 11.9 ± 0.01 * | 14.3 ± 0.02 * |
| Levofloxacin | 17.6 ± 0.03 | 24.3 ± 0.02 | 16.3 ± 0.04 | 21.3 ± 0.04 |
| DMSO | - | - | - | - |
| Antibacterial activities of extract and fractions against Gram-positive bacterial strains | ||||
| Fractions | Staphylococcus aureus | Bacillus subtilis | ||
| C1 | C2 | C1 | C2 | |
| SECR | 14.03 ± 0.03 * | 18.03 ± 0.01 * | 13.07 ± 0.03 * | 18.21 ± 0.03 * |
| SEEA | 15.03 ± 0.01 * | 19.07 ± 0.02 * | 14.97 ± 0.01 * | 18.87 ± 0.04 * |
| SECH | 14.57 ± 0.03 * | 17.03 ± 0.03 * | 14.07 ± 0.03 * | 17.09 ± 0.01 * |
| SENB | 13.87 ± 0.02 * | 16.71 ± 0.02 * | 14.07 ± 0.04 * | 16.27 ± 0.03 * |
| SENH | 13.03 ± 0.04 * | 16.03 ± 0.01 * | 12.03 ± 0.01 * | 15.81 ± 0.01 * |
| SEAQ | 12.03 ± 0.01 * | 15.11 ± 0.04 * | 11.87 ± 0.02 * | 14.51 ± 0.01 * |
| Erythromycin | 17.03 ± 0.03 | 22.09 ± 0.03 | 16.90 ± 0.05 | 22.03 ± 0.04 |
| DMSO | - | - | - | - |
| Paw Volume Changes (Mean ± SEM) | ||||||
|---|---|---|---|---|---|---|
| Treatment | Dose (mg/kg) | 1 h | 2 h | 3 h | Average Reading | % Inhibition |
| Carrageenan | 1 mL | 1.07 ± 0.03 | 1.31 ± 0.01 | 1.63 ± 0.02 | 1.33 ± 0.02 | |
| Diclofenac | 50 | 0.51 ± 0.02 | 0.35 ± 0.05 | 0.19 ± 0.03 | 0.35 ± 0.05 | 74 |
| SECR | 50 | 0.91 ± 0.07 | 0.82 ± 0.01 | 0.69 ± 0.05 | 0.80 ± 0.04 * | 39 |
| 100 | 0.79 ± 0.04 | 0.66 ± 0.02 | 0.53 ± 0.06 | 0.66 ± 0.04 * | 50 | |
| SEEA | 50 | 0.82 ± 0.06 | 0.73 ± 0.03 | 0.60 ± 0.01 | 0.71 ± 0.03 * | 47 |
| 100 | 0.74 ± 0.03 | 0.61 ± 0.02 | 0.49 ± 0.03 | 0.61 ± 0.02 * | 54 | |
| SECH | 50 | 0.88 ± 0.05 | 0.79 ± 0.02 | 0.65 ± 0.04 | 0.77 ± 0.03 * | 42 |
| 100 | 0.79 ± 0.02 | 0.68 ± 0.04 | 0.56 ± 0.01 | 0.67 ± 0.02 * | 50 | |
| SENB | 50 | 0.89 ± 0.03 | 0.78 ± 0.05 | 0.70 ± 0.02 | 0.79 ± 0.03 * | 41 |
| 100 | 0.81 ± 0.04 | 0.70 ± 0.02 | 0.62 ± 0.01 | 0.71 ± 0.02 * | 47 | |
| SENH | 50 | 0.93 ± 0.01 | 0.83 ± 0.06 | 0.74 ± 0.03 | 0.83 ± 0.03 * | 38 |
| 100 | 0.86 ± 0.03 | 0.77 ± 0.03 | 0.68 ± 0.02 | 0.77 ± 0.03 * | 42 | |
| SEAQ | 50 | 0.95 ± 0.02 | 0.87 ± 0.02 | 0.79 ± 0.03 | 0.87 ± 0.02 * | 35 |
| 100 | 0.88 ± 0.03 | 0.81 ± 0.02 | 0.75 ± 0.01 | 0.81 ± 0.02 * | 39 | |
| Treatment | Dose (mg/kg) | No of Writhes Mean ± SEM | % Reduction in Writhing |
|---|---|---|---|
| Acetic acid | 1 mL | 29.6 ± 0.02 | |
| Aspirin | 1 mL | 9.3 ± 0.02 | 68 |
| SECR | 50 | 21.4± 0.07 ** | 28 |
| 100 | 17.3 ± 0.04 ** | 42 | |
| SEEA | 50 | 18.6 ± 0.06 ** | 37 |
| 100 | 13.3 ± 0.03 ** | 55 | |
| SECH | 50 | 21.2 ± 0.05 ** | 29 |
| 100 | 15.3 ± 0.02 ** | 48 | |
| SENB | 50 | 21.3 ± 0.03 ** | 28 |
| 100 | 17.3 ± 0.04 ** | 42 | |
| SENH | 50 | 20.3 ± 0.01 ** | 31 |
| 100 | 17.3 ± 0.03 ** | 41 | |
| SEAQ | 50 | 22.3 ± 0.02 ** | 25 |
| 100 | 17.6 ± 0.03 ** | 40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shah, M.; Murad, W.; Ur Rehman, N.; Halim, S.A.; Ahmed, M.; Rehman, H.; Zahoor, M.; Mubin, S.; Khan, A.; Nassan, M.A.; et al. Biomedical Applications of Scutellaria edelbergii Rech. f.: In Vitro and In Vivo Approach. Molecules 2021, 26, 3740. https://doi.org/10.3390/molecules26123740
Shah M, Murad W, Ur Rehman N, Halim SA, Ahmed M, Rehman H, Zahoor M, Mubin S, Khan A, Nassan MA, et al. Biomedical Applications of Scutellaria edelbergii Rech. f.: In Vitro and In Vivo Approach. Molecules. 2021; 26(12):3740. https://doi.org/10.3390/molecules26123740
Chicago/Turabian StyleShah, Muddaser, Waheed Murad, Najeeb Ur Rehman, Sobia Ahsan Halim, Manzoor Ahmed, Hazir Rehman, Muhammed Zahoor, Sidra Mubin, Ajmal Khan, Mohamed A. Nassan, and et al. 2021. "Biomedical Applications of Scutellaria edelbergii Rech. f.: In Vitro and In Vivo Approach" Molecules 26, no. 12: 3740. https://doi.org/10.3390/molecules26123740
APA StyleShah, M., Murad, W., Ur Rehman, N., Halim, S. A., Ahmed, M., Rehman, H., Zahoor, M., Mubin, S., Khan, A., Nassan, M. A., Batiha, G. E.-S., & Al-Harrasi, A. (2021). Biomedical Applications of Scutellaria edelbergii Rech. f.: In Vitro and In Vivo Approach. Molecules, 26(12), 3740. https://doi.org/10.3390/molecules26123740












