Using Wearable Sensors and Machine Learning to Automatically Detect Freezing of Gait during a FOG-Provoking Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
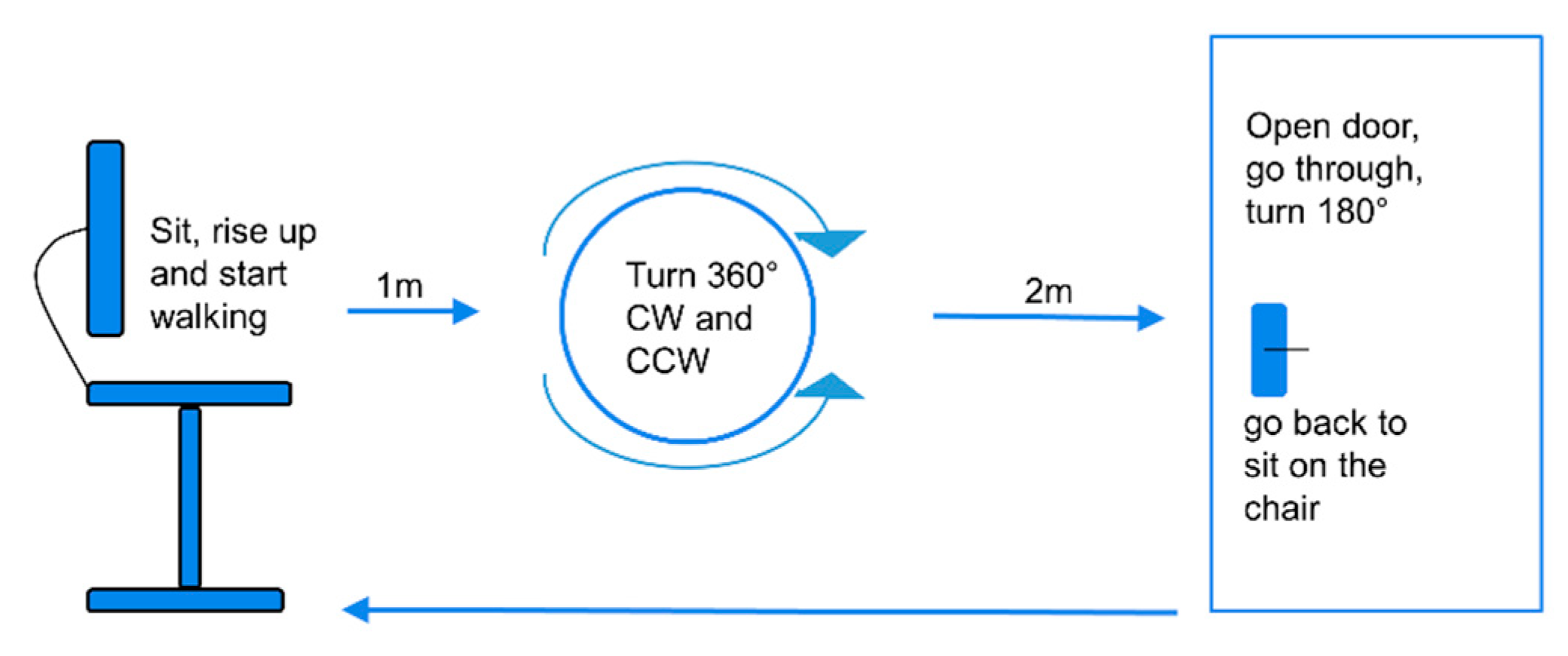
2.2. FOG-Provoking Test and Wearable Sensors
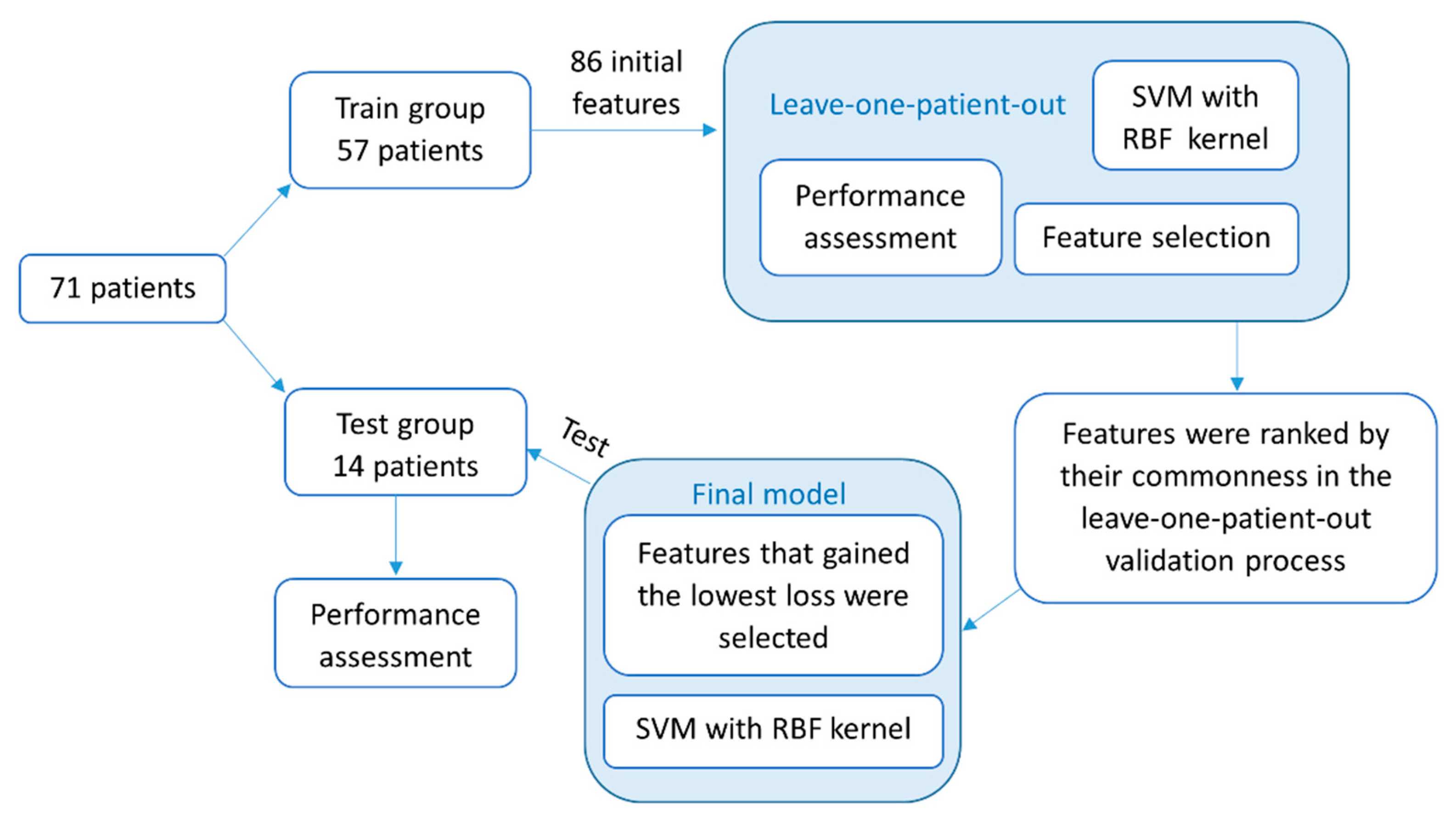
2.3. Machine-Learning Algorithms
2.4. Statistical Analysis
3. Results
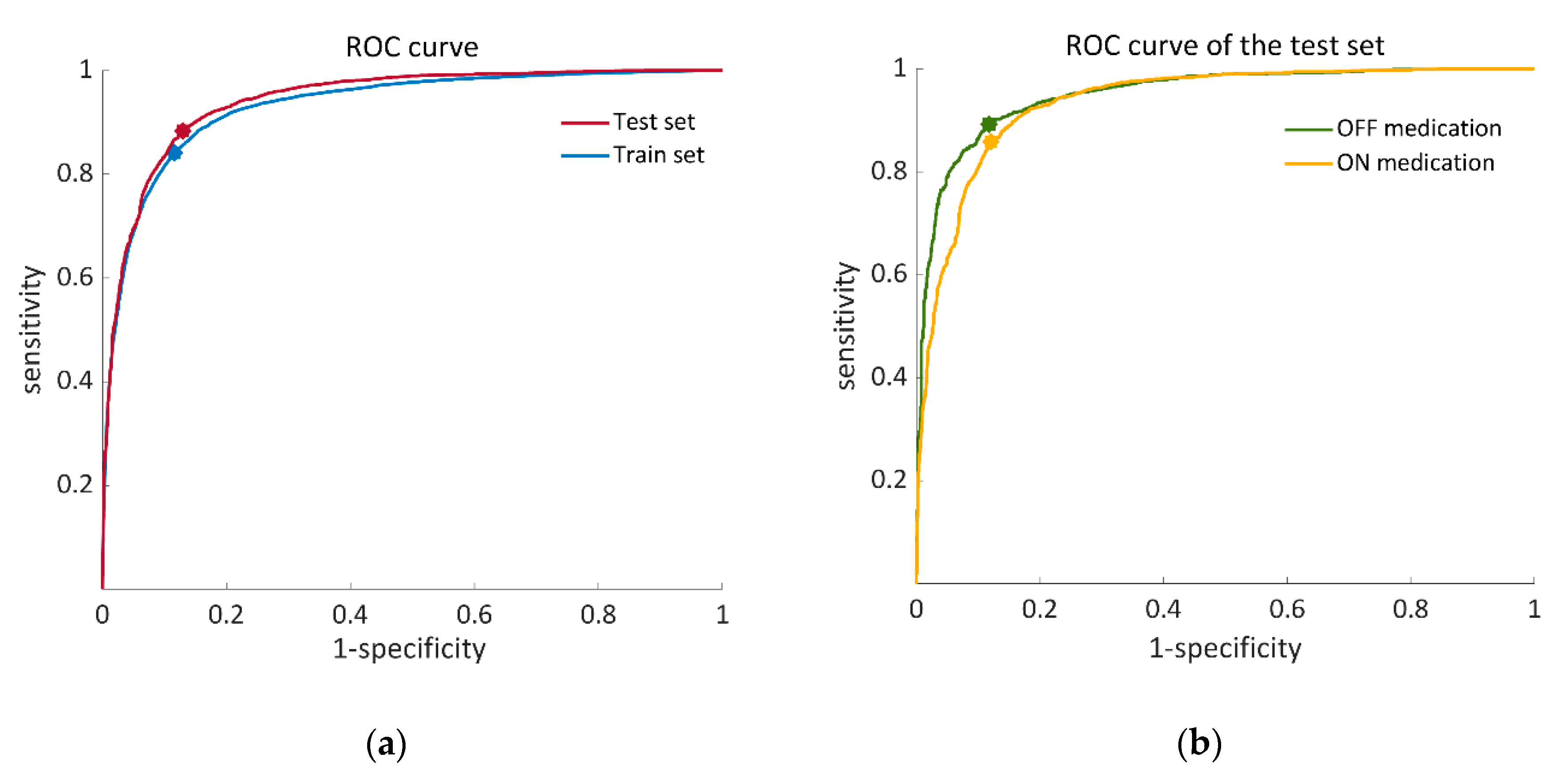
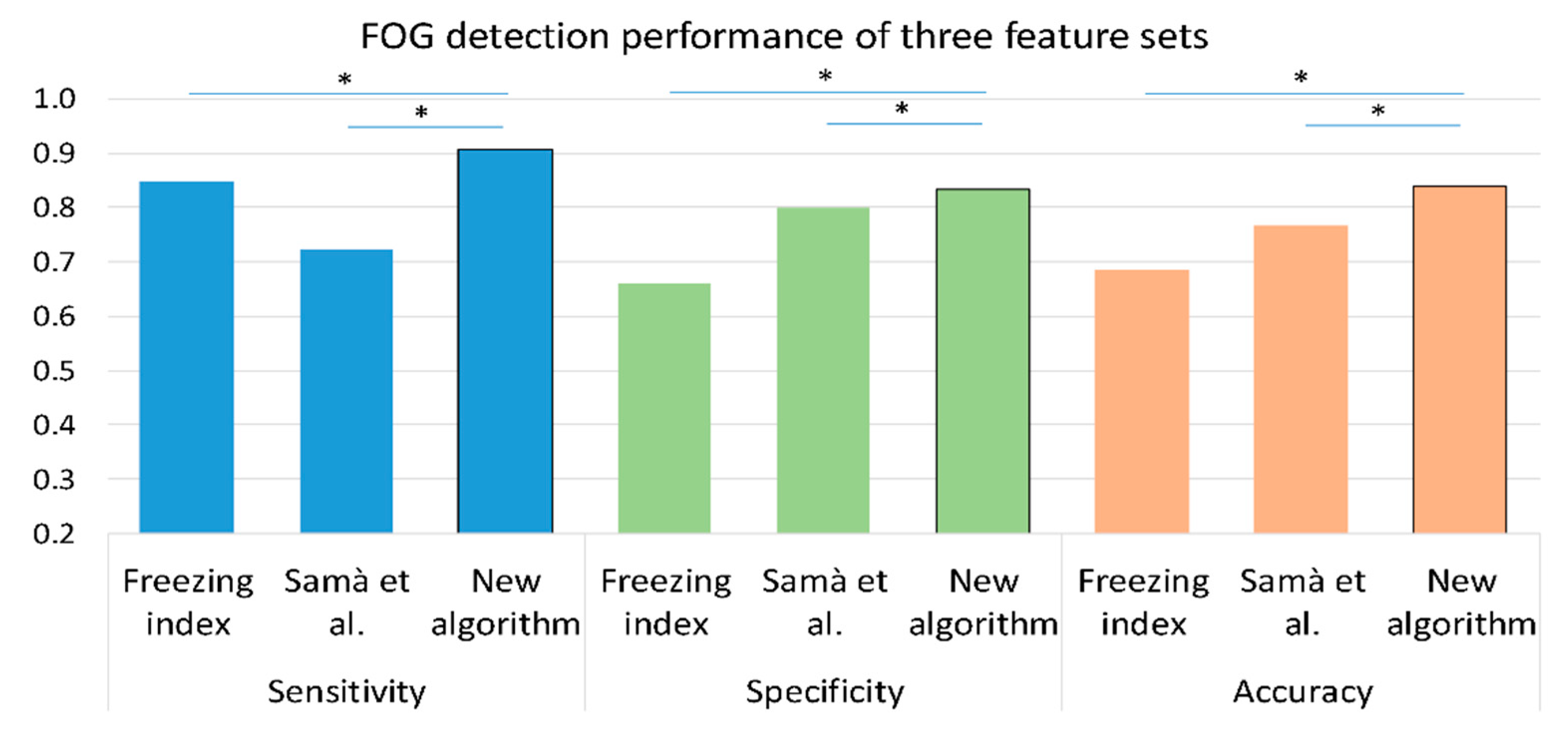
3.1. Detection Performance
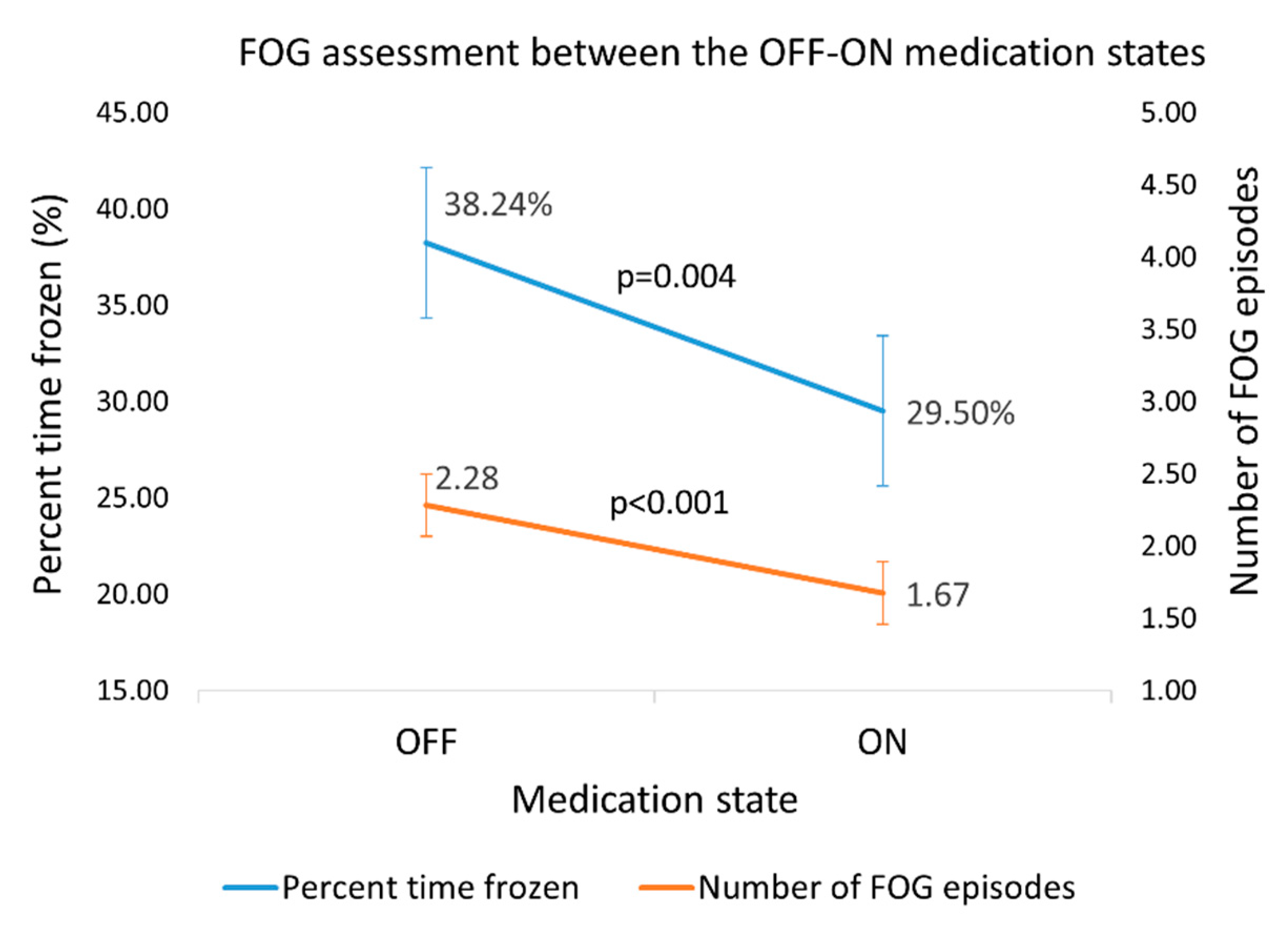
3.2. Responsiveness of the Assessment of FOG Based on the Outcomes of the Algorithm
3.3. Associations of Algorithm Measures of FOG with Related Measures of FOG
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Deposition Information
Appendix A
| No. of Features | Feature Description | Back Sensor | Leg Sensors |
|---|---|---|---|
| Time domain | |||
| 6 | Mean() | Acceleration, | Acceleration, Gyroscope, |
| 6 | SD() | Acceleration, | Acceleration, Gyroscope, |
| 6 | Correlations() | Acceleration, | Gyroscope, } |
| 1 | Correlations between the right and left leg | . | Gyroscope, |
| 7 | Range(cumulative sum ()) | Acceleration, Gyroscope: | Acceleration, Gyroscope, |
| 2 | RMS () | Acceleration, | . |
| 2 | RMS (; total RMS across all axes | Acceleration, | Gyroscope, |
| 1 | Legs: Gyroscope, Back: Acceleration, | ||
| 1 | Legs: Gyroscope, Back: Gyroscope, | ||
| Frequency domain | |||
| 16 | SD(); SD of the frequency amplitude in specific bands | Acceleration, | Acceleration, Gyroscope, |
| 24 | Peak amplitude of and its frequency across all frequencies and in specific bands | Acceleration, | Acceleration, Gyroscope, |
| 3 | Entropy of in specific bands | Acceleration, Gyroscope, | . |
| 1 | Freezing index (); | . | Acceleration, |
| 1 | Total power: the average power of | While turning: Gyroscope, Otherwise: Acceleration, | . |
| 5 | Skewness of in specific bands | Acceleration, Gyroscope, | . |
| 4 | Kurtosis of in specific bands | Acceleration, | . |
References
- Moore, O.; Peretz, C.; Giladi, N. Freezing of gait affects quality of life of peoples with Parkinson’s disease beyond its relationships with mobility and gait. Mov. Disord. 2007, 22, 2192–2195. [Google Scholar] [CrossRef] [PubMed]
- Nutt, J.G.; Bloem, B.R.; Giladi, N.; Hallett, M.; Horak, F.B.; Nieuwboer, A. Freezing of gait: Moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011, 10, 734–744. [Google Scholar] [CrossRef]
- Bloem, B.R.; Hausdorff, J.M.; Visser, J.E.; Giladi, N. Falls and freezing of Gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Mov. Disord. 2004, 19, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Amboni, M.; Stocchi, F.; Abbruzzese, G.; Morgante, L.; Onofrj, M.; Ruggieri, S.; Tinazzi, M.; Zappia, M.; Attar, M.; Colombo, D.; et al. Prevalence and associated features of self-reported freezing of gait in Parkinson disease: The DEEP FOG study. Parkinsonism. Relat. Disord. 2015, 21, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Schaafsma, J.D.; Balash, Y.; Gurevich, T.; Bartels, A.L.; Hausdorff, J.M.; Giladi, N. Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur. J. Neurol. 2003, 10, 391–398. [Google Scholar] [CrossRef]
- Mancini, M.; Bloem, B.R.; Horak, F.B.; Lewis, S.J.G.; Nieuwboer, A.; Nonnekes, J. Clinical and methodological challenges for assessing freezing of gait: Future perspectives. Mov. Disord. 2019, 34, 783–790. [Google Scholar] [CrossRef]
- Barthel, C.; Mallia, E.; Debû, B.; Bloem, B.R.; Ferraye, M.U. The Practicalities of Assessing Freezing of Gait. J. Parkinsons. Dis. 2016, 6, 667–674. [Google Scholar] [CrossRef]
- Delval, A.; Tard, C.; Rambour, M.; Defebvre, L.; Moreau, C. Characterization and quantification of freezing of gait in Parkinson’s disease: Can detection algorithms replace clinical expert opinion? Neurophysiol. Clin. 2015, 45, 305–313. [Google Scholar] [CrossRef]
- Hulzinga, F.; Nieuwboer, A.; Dijkstra, B.W.; Mancini, M.; Strouwen, C.; Bloem, B.R.; Ginis, P. The New Freezing of Gait Questionnaire: Unsuitable as an Outcome in Clinical Trials? Mov. Disord. Clin. Pract. 2020, 7, 199–205. [Google Scholar] [CrossRef]
- Ziegler, K.; Schroeteler, F.; Ceballos-Baumann, A.O.; Fietzek, U.M. A new rating instrument to assess festination and freezing gait in Parkinsonian patients. Mov. Disord. 2010, 25, 1012–1018. [Google Scholar] [CrossRef]
- Herman, T.; Dagan, M.; Shema-Shiratzky, S.; Reches, T.; Brozgol, M.; Giladi, N.; Manor, B.; Hausdorff, J.M. Advantages of timing the duration of a freezing of gait-provoking test in individuals with Parkinson’s disease. J. Neurol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Morris, T.R.; Cho, C.; Dilda, V.; Shine, J.M.; Naismith, S.L.; Lewis, S.J.G.; Moore, S.T. A comparison of clinical and objective measures of freezing of gait in Parkinson’s disease. Parkinsonism Relat. Disord. 2012, 18, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Pardoel, S.; Kofman, J.; Nantel, J.; Lemaire, E.D. Wearable-sensor-based detection and prediction of freezing of gait in parkinson’s disease: A review. Sensors 2019, 19, 5141. [Google Scholar] [CrossRef]
- Moore, S.T.; Yungher, D.A.; Morris, T.R.; Dilda, V.; Macdougall, H.G.; Shine, J.M.; Naismith, S.L.; Lewis, S.J. Autonomous identification of freezing of gait in Parkinson’s disease from lower-body segmental accelerometry. J. Neuroeng. Rehabil. 2013, 10, 19. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.T.; Moore, S.T.; Lewis, S.J.G.; Nguyen, D.N.; Dutkiewicz, E.; Fuglevand, A.J.; McEwan, A.L.; Leong, P.H.W. Freezing of Gait Detection in Parkinson’s Disease: A Subject-Independent Detector Using Anomaly Scores. IEEE Trans. Biomed. Eng. 2017, 64, 2719–2728. [Google Scholar]
- Moore, S.T.; MacDougall, H.G.; Ondo, W.G. Ambulatory monitoring of freezing of gait in Parkinson’s disease. J. Neurosci. Methods 2008, 167, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; Smulders, K.; Cohen, R.G.; Horak, F.B.; Giladi, N.; Nutt, J.G. The clinical significance of freezing while turning in Parkinson’s disease. Neuroscience 2017, 343, 222–228. [Google Scholar] [CrossRef]
- Kwon, Y.; Park, S.H.; Kim, J.-W.; Ho, Y.; Jeon, H.-M.; Bang, M.-J.; Jung, G.-I.; Lee, S.-M.; Eom, G.-M.; Koh, S.-B.; et al. A practical method for the detection of freezing of gait in patients with Parkinson’s disease. Clin. Interv. Aging 2014, 9, 1709–1719. [Google Scholar]
- Kita, A.; Lorenzi, P.; Rao, R.; Irrera, F. Reliable and Robust Detection of Freezing of Gait Episodes With Wearable Electronic Devices. IEEE Sens. J. 2017, 17, 1899–1908. [Google Scholar] [CrossRef]
- Delval, A.; Snijders, A.H.; Weerdesteyn, V.; Duysens, J.E.; Defebvre, L.; Giladi, N.; Bloem, B.R. Objective detection of subtle freezing of gait episodes in Parkinson’s disease. Mov. Disord. 2010, 25, 1684–1693. [Google Scholar] [CrossRef]
- Rodríguez-Martín, D.; Samà, A.; Pérez-López, C.; Català, A.; Arostegui, J.M.M.; Cabestany, J.; Bayés, À.; Alcaine, S.; Mestre, B.; Prats, A.; et al. Home detection of freezing of gait using Support Vector Machines through a single waist-worn triaxial accelerometer. PLoS ONE 2017, 12, e0171764. [Google Scholar] [CrossRef] [PubMed]
- Ahlrichs, C.; Samà, A.; Lawo, M.; Cabestany, J.; Rodríguez-Martín, D.; Pérez-López, C.; Sweeney, D.; Quinlan, L.R.; Laighin, G.; Counihan, T.; et al. Detecting freezing of gait with a tri-axial accelerometer in Parkinson’s disease patients. Med. Biol. Eng. Comput. 2016, 54, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Samà, A.; Rodríguez-Martín, D.; Pérez-López, C.; Català, A.; Alcaine, S.; Mestre, B.; Prats, A.; Crespo, M.C.; Bayés, À. Determining the optimal features in freezing of gait detection through a single waist accelerometer in home environments. Pattern Recognit. Lett. 2018, 105, 135–143. [Google Scholar] [CrossRef]
- Tahafchi, P.; Molina, R.; Roper, J.A.; Sowalsky, K.; Hass, C.J.; Gunduz, A.; Okun, M.S.; Judy, J.W. Freezing-of-Gait Detection Using Temporal, Spatial, and Physiological Features with a Support-Vector-Machine Classifier. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo, Korea, 11–15 July 2017; pp. 2867–2870. [Google Scholar]
- Aich, S.; Pradhan, P.M.; Park, J.; Sethi, N.; Vathsa, V.S.S.; Kim, H.C. A validation study of freezing of gait (FoG) detection and machine-learning-based FoG prediction using estimated gait characteristics with a wearable accelerometer. Sensors 2018, 18, 3287. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, H.J.; Lee, W.; Kwon, S.; Kim, S.K.; Jeon, H.S.; Park, H.; Shin, C.W.; Yi, W.J.; Jeon, B.S.; et al. Unconstrained Detection of Freezing of Gait in Parkinson’s Disease Patients Using Smartphone. In Proceedings of the Engineering in Medicine and Biology Society (EMBC), 2015 37th Annual International Conference of the IEEE, Milan, Italy, 25–29 August 2015; pp. 3751–3754. [Google Scholar]
- Mazilu, S.; Hardegger, M.; Zhu, Z.; Roggen, D.; Troester, G.; Plotnik, M.; Hausdorff, J. Online Detection of Freezing of Gait with Smartphones and Machine Learning Techniques. In Proceedings of the 2012 6th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops, San Diego, CA, USA, 21–24 May 2012; pp. 123–130. [Google Scholar]
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Giladi, N.; Hausdorff, J.M. An instrumented timed up and go: The added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol. Meas 2011, 32, 2003–2018. [Google Scholar] [CrossRef] [PubMed]
- Vervoort, D.; Vuillerme, N.; Kosse, N.; Hortobágyi, T.; Lamoth, C.J.C. Multivariate analyses and classification of inertial sensor data to identify aging effects on the timed-Up-and-Go test. PLoS ONE 2016, 11, e0155984. [Google Scholar] [CrossRef] [PubMed]
- Bernard, B.A.; Goldman, J.G. MMSE—Mini-Mental State Examination. In Encyclopedia of Movement Disorders; Elsevier Inc.: London, UK, 2010; pp. 187–189. [Google Scholar]
- Nieuwboer, A.; Rochester, L.; Herman, T.; Vandenberghe, W.; Emil, G.E.; Thomaes, T.; Giladi, N. Reliability of the new freezing of gait questionnaire: Agreement between patients with Parkinson’s disease and their carers. Gait Posture 2009, 30, 459–463. [Google Scholar] [CrossRef]
- Horak, F.B.; Mancini, M.; Carlson-Kuhta, P.; Nutt, J.G.; Salarian, A. Balance and Gait Represent Independent Domains of Mobility in Parkinson Disease. Phys. Ther. 2016, 96, 1364–1371. [Google Scholar] [CrossRef]
- Orphanidou, N.K.; Hussain, A.; Keight, R.; Lishoa, P.; Hind, J.; Al-Askar, H. Predicting Freezing of Gait in Parkinsons Disease Patients Using Machine Learning. In Proceedings of the 2018 IEEE Congress on Evolutionary Computation (CEC), Rio de Janeiro, Brazil, 8–13 July 2018. [Google Scholar]
- Ding, C.; Peng, H. Minimum redundancy feature selection from microarray gene expression data. In Proceedings of the 2003 IEEE Bioinformatics Conference. CSB, Stanford, CA, USA, 11 August 2003; Volume 3, pp. 523–528. [Google Scholar]
- Hausdorff, J.M.; Balash, Y.; Giladi, N. Time series analysis of leg movements during freezing of gait in Parkinson’s disease: Akinesia, rhyme or reason? Phys. A Stat. Mech. Its Appl. 2003, 321, 565–570. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Sigcha, L.; Costa, N.; Pav, I.; Costa, S.; Arezes, P.; Manuel, J.; Arcas, G. De Deep Learning Approaches for Detecting Freezing of Gait in Parkinson’s Disease Patients through On-Body Acceleration Sensors. Sensors 2020, 20, 1895. [Google Scholar] [CrossRef]
- Mazzetta, I.; Zampogna, A.; Suppa, A.; Gumiero, A.; Pessione, M.; Irrera, F. Wearable sensors system for an improved analysis of freezing of gait in Parkinson’s disease using electromyography and inertial signals. Sensors 2019, 19, 948. [Google Scholar] [CrossRef] [PubMed]
- Mazilu, S.; Calatroni, A.; Gazit, E.; Mirelman, A.; Hausdorff, J.M.; Tröster, G. Prediction of freezing of gait in Parkinson’s from physiological wearables: An exploratory study. IEEE J. Biomed. Heal. Inform. 2015, 19, 1843–1854. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Bindels, H.; Ketheeswaran, M.; Brodie, M.A.; Lawrence, A.D.; Close, J.C.T.; Whone, A.L.; Ben-Shlomo, Y.; Henderson, E.J. Freezing of Gait in People with Parkinson’s Disease: Nature, Occurrence, and Risk Factors. J. Parkinsons. Dis. 2020, 10, 631–640. [Google Scholar] [CrossRef] [PubMed]

| Feature | Axis/Frequency |
|---|---|
| Time domain | |
| Difference of the mean | AP, V-ML, AP-ML |
| SD | AP, V, ML |
| Correlation | V-AP, AP-ML, V-ML |
| Skewness | AP, V, ML |
| Skewness of the RMS | . |
| Frequency domain All features were calculated for the sum of the three axes vectors | |
| SD in different bands | 0.04–0.68 Hz, 0.68–3 Hz, 3–8 Hz, 8–20 Hz, 0.1–8 Hz |
| Max harmonic and its frequency | . |
| Distance between the first and second max harmonics | . |
| Center of Mass | . |
| Skewness in different bands | 0.04–0.68 Hz, 0.68–3 Hz, 3–8 Hz, |
| First three components of PCA | 0.04–8 Hz |
| No. of subjects * (N) | 71 |
| Age (years) | 69.9 ± 7.8 |
| Gender (M:F) | (57:14) |
| Disease duration (years) | 9.2 ± 5.7 |
| Education (%) | 22% High school or equivalent 23.9% Bachelors 32% Masters or higher |
| New FOG Questionnaire | 19.4 ± 4.3 |
| Mini Mental Status Exam | 28.0 ± 1.8 |
| MDS-UPDRS part III (motor) OFF | 43.1 ± 16.9 |
| MDS-UPDRS part III (motor) ON | 37.1 ± 14.5 |
| TUG time OFF (s) | 15.3 ± 10.2 |
| TUG time ON (s) | 13.6 ± 7.9 |
| FOG-provoking test total score OFF | 15.8 ± 7.0 |
| FOG-provoking test total score ON | 12.5 ± 6.6 |
| Gait speed (cm/s) OFF | 100.3 ± 22.8 |
| Gait speed (cm/s) ON | 104.6 ± 25.2 |
| Domain | Feature Description | Sensor Location | Accelerometer/Gyroscope | |
|---|---|---|---|---|
| 1 | Time | Legs and back | Legs: Gyroscope, Back: Acceleration, | |
| 2 | Frequency | Freezing index ( | Legs | Acceleration, |
| 3 | Frequency | Peak frequency of between 3–8 Hz | Legs; max between both legs | Acceleration, |
| 4 | Frequency | Entropy of between 0.5–3 Hz | Back | Gyroscope, |
| 5 | Frequency | Peak frequency of between 0.5–3 Hz | Legs; | Gyroscope, |
| 6 | Time | Range(cumulative sum ()) | Back | Gyroscope, |
| 7 | Frequency | Entropy of in specific bands 0.5–3 Hz | Back | Acceleration, |
| 8 | Time | Range(cumulative sum ()) | Legs; min between both legs | Acceleration, |
| 9 | Time | Mean () | Legs; | Gyroscope, |
| 10 | Frequency | Skewness of between 0.5–3 Hz | Back | Gyroscope, |
| 11 | Time | Correlations between the right and left leg | Legs; | Gyroscope, |
| 12 | Time | Legs and back | Gyroscope, | |
| 13 | Time | Range(cumulative sum ()) | Legs; | Gyroscope, |
| 14 | Time | RMS | Legs; | Gyroscope, |
| No. of Subjects | Easiest Level | Most Challenging Level | Effect Size | p-Value | |
|---|---|---|---|---|---|
| OFF medication | 41 | ||||
| Percent time frozen (%) | 35.7 (7.2–51.1) | 36.5 (17.4–69.8) | 0.4 | 0.017 | |
| Total time frozen (s) | 15.0 (3.0–24.8) | 24.0 (9.0–69.8) | 0.6 | <0.001 | |
| Number of FOG episodes | 1.0 (1.0–3.0) | 3.0 (1.5–4.0) | 0.7 | <0.001 | |
| ON medication | 62 | ||||
| Percent time frozen (%) | 21.0 (0–43.4) | 37.8 (11.2–50.4) | 0.6 | <0.001 | |
| Total time frozen (s) | 9.0 (0.0–20.3) | 18.0 (4.5–38.1) | 0.7 | <0.001 | |
| Number of FOG episodes | 1.0 (0.0–2.0) | 2.0 (1.0–4.0) | 0.7 | <0.001 |
| NFOGQ Total | TUG Time | MDS-UPDRS Part III | Disease Duration | |
|---|---|---|---|---|
| OFF medication | ||||
| Percent time frozen (%) | 0.489 ** | 0.263 | 0.074 | −0.253 |
| Total time frozen (s) | 0.485 ** | 0.392 ** | 0.116 | −0.176 |
| Number of episodes | 0.391 ** | 0.420 ** | 0.210 | 0.029 |
| ON medication | ||||
| Percent time frozen (%) | 0.375 ** | 0.379 ** | 0.496 ** | −0.042 |
| Total time frozen (s) | 0.405 ** | 0.471 ** | 0.565 ** | −0.007 |
| Number of episodes | 0.416 ** | 0.583 ** | 0.565 ** | 0.071 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reches, T.; Dagan, M.; Herman, T.; Gazit, E.; Gouskova, N.A.; Giladi, N.; Manor, B.; Hausdorff, J.M. Using Wearable Sensors and Machine Learning to Automatically Detect Freezing of Gait during a FOG-Provoking Test. Sensors 2020, 20, 4474. https://doi.org/10.3390/s20164474
Reches T, Dagan M, Herman T, Gazit E, Gouskova NA, Giladi N, Manor B, Hausdorff JM. Using Wearable Sensors and Machine Learning to Automatically Detect Freezing of Gait during a FOG-Provoking Test. Sensors. 2020; 20(16):4474. https://doi.org/10.3390/s20164474
Chicago/Turabian StyleReches, Tal, Moria Dagan, Talia Herman, Eran Gazit, Natalia A. Gouskova, Nir Giladi, Brad Manor, and Jeffrey M. Hausdorff. 2020. "Using Wearable Sensors and Machine Learning to Automatically Detect Freezing of Gait during a FOG-Provoking Test" Sensors 20, no. 16: 4474. https://doi.org/10.3390/s20164474
APA StyleReches, T., Dagan, M., Herman, T., Gazit, E., Gouskova, N. A., Giladi, N., Manor, B., & Hausdorff, J. M. (2020). Using Wearable Sensors and Machine Learning to Automatically Detect Freezing of Gait during a FOG-Provoking Test. Sensors, 20(16), 4474. https://doi.org/10.3390/s20164474






