Protein Enrichment of Donor Breast Milk and Impact on Growth in Very Low Birth Weight Infants
Abstract
:1. Introduction
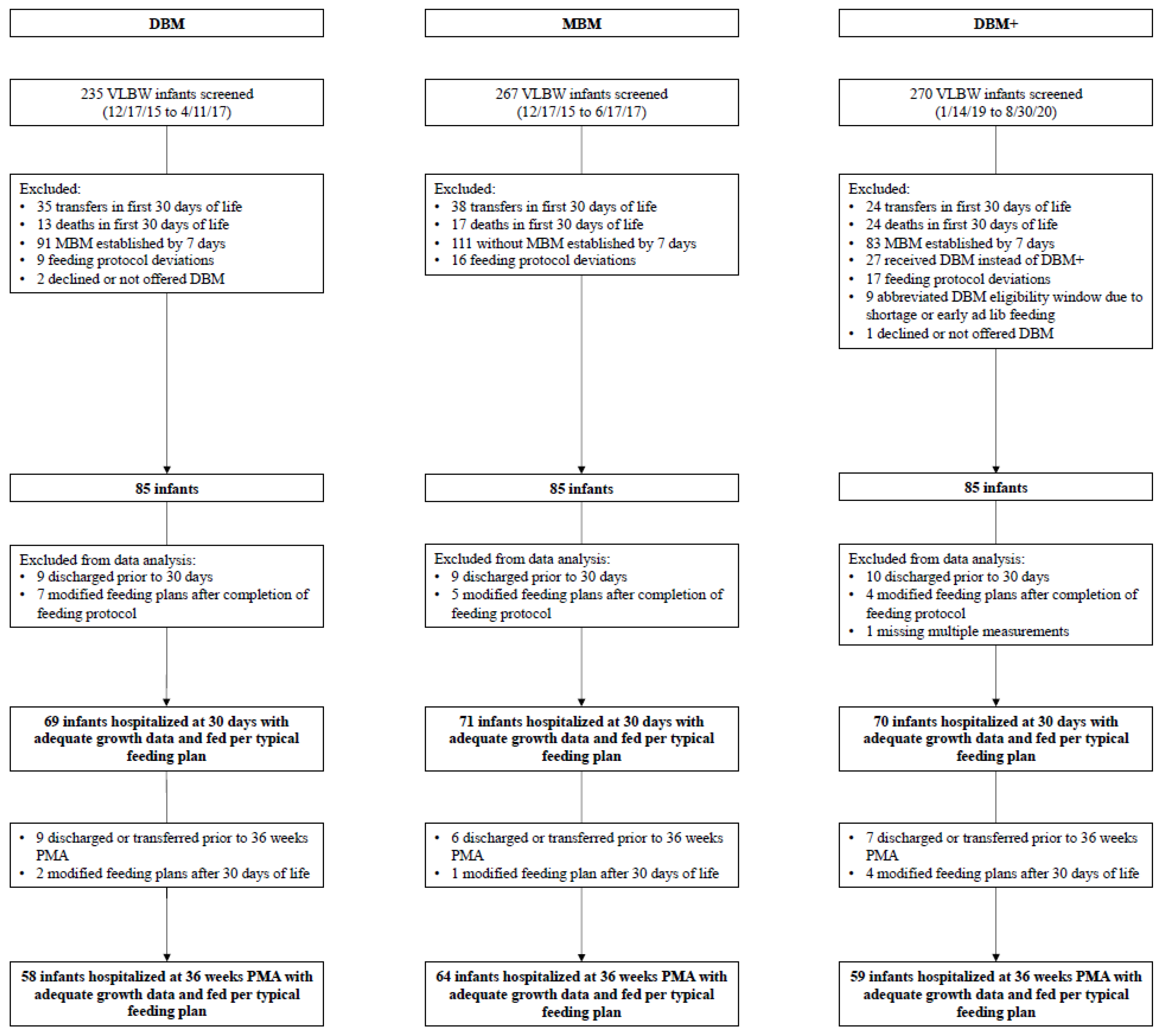
2. Materials and Methods
2.1. Study Population
2.2. Standardized Feeding Approach
2.3. Clinical Data Collection and Outcomes
2.4. Statistical Analysis
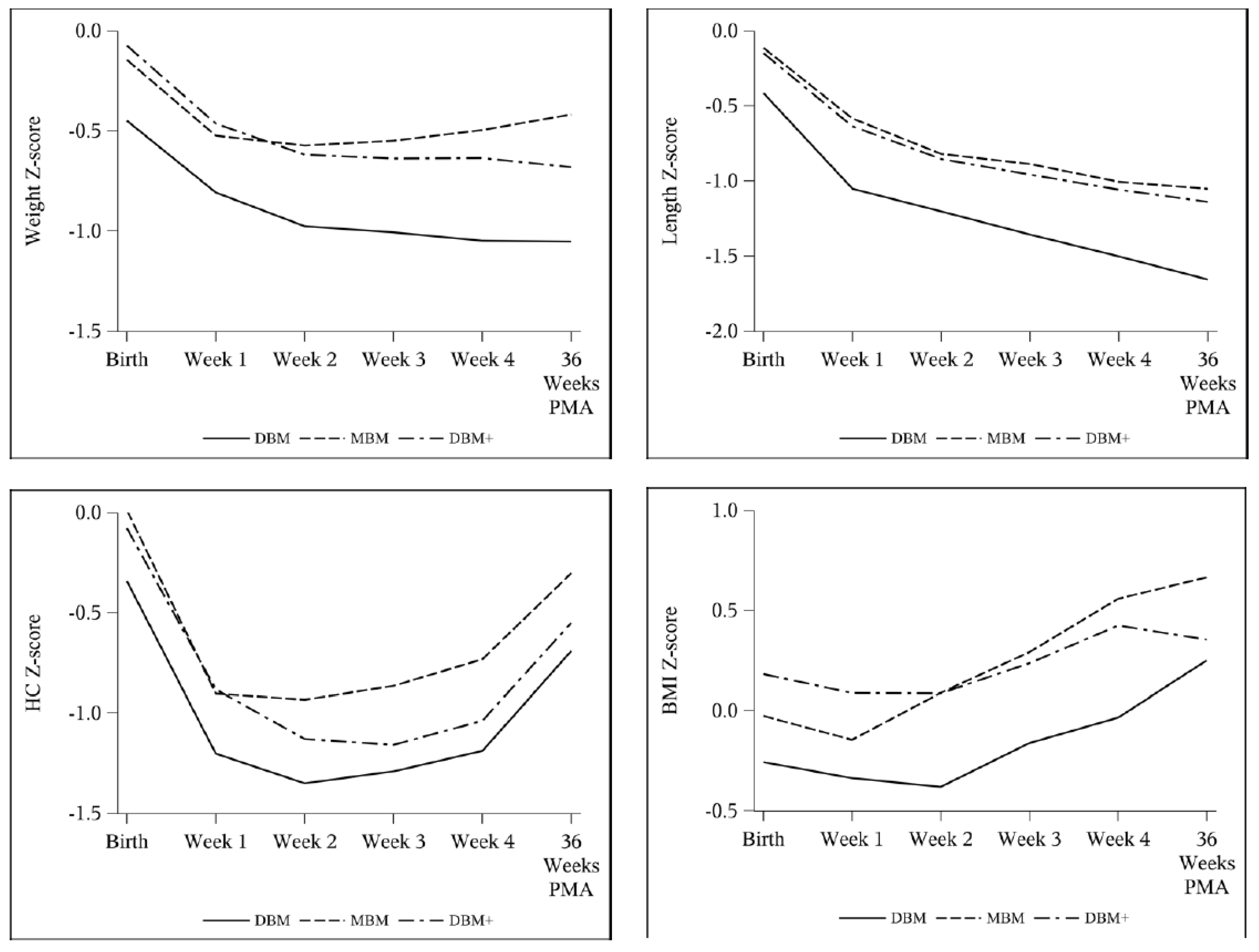
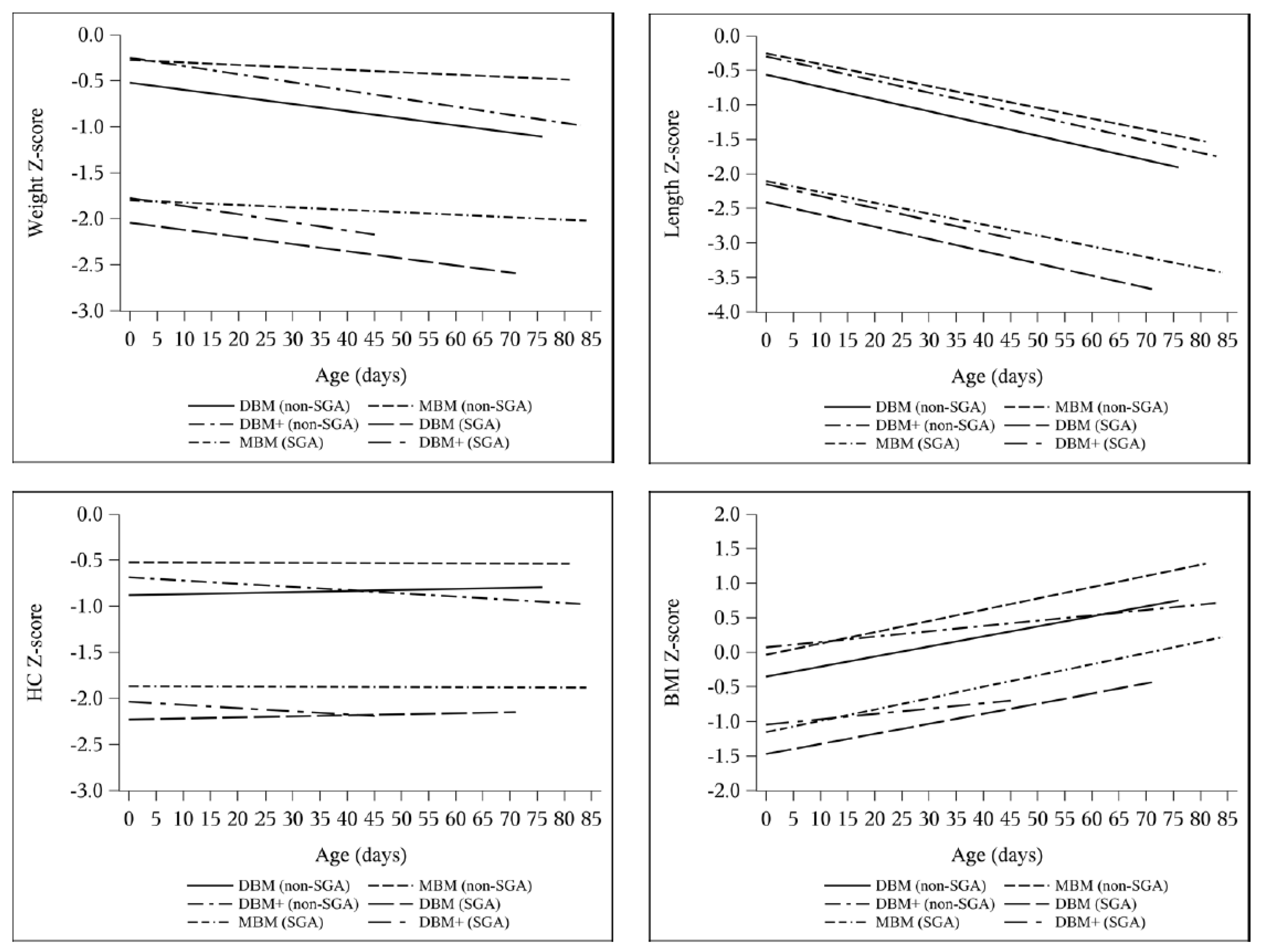
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Committee on Nutrition; Section on Breastfeeding; Committee on Fetus and Newborn. Donor Human Milk for the High-Risk Infant: Preparation, Safety, and Usage Options in the United States. Pediatrics 2017, 139, e20163440. [Google Scholar] [CrossRef] [Green Version]
- Perrin, M.T.; Belfort, M.B.; Hagadorn, J.I.; McGrath, J.M.; Taylor, S.N.; Tosi, L.M.; Brownell, E.A. The Nutritional Composition and Energy Content of Donor Human Milk: A Systematic Review. Adv. Nutr. 2020, 11, 960–970. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.T.; Schroder, P.E.; Poindexter, B.B. Macronutrient Analysis of Target-Pooled Donor Breast Milk and Corresponding Growth in Very Low Birth Weight Infants. Nutrients 2019, 11, 1884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, A.; Sun, R.; Maillart, L.; Schaefer, A.; Hamilton Spence, E.; Perrin, M.T. Macronutrient variability in human milk from donors to a milk bank: Implications for feeding preterm infants. PLoS ONE 2019, 14, e0210610. [Google Scholar] [CrossRef]
- Pfister, K.M.; Ramel, S.E. Linear Growth and Neurodevelopmental Outcomes. Clin. Perinatol. 2014, 41, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Stephens, B.E.; Vohr, B.R. Protein Intake and Neurodevelopmental Outcomes. Clin. Perinatol. 2014, 41, 323–329. [Google Scholar] [CrossRef]
- Stephens, B.E.; Walden, R.V.; Gargus, R.A.; Tucker, R.; McKinley, L.; Mance, M.; Nye, J.; Vohr, B.R. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics 2009, 123, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Buonocore, G.; Carnielli, V.P.; De Curtis, M.; Darmaun, D.; Decsi, T.; Domellof, M.; Embleton, N.D.; Fusch, C.; Genzel-Boroviczeny, O.; et al. Enteral nutrient supply for preterm infants: Commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Rochow, N.; Fusch, G.; Ali, A.; Bhatia, A.; So, H.Y.; Iskander, R.; Chessell, L.; El Helou, S.; Fusch, C. Individualized target fortification of breast milk with protein, carbohydrates, and fat for preterm infants: A double-blind randomized controlled trial. Clin. Nutr. 2020, 40, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Bulut, O.; Coban, A.; Uzunhan, O.; Ince, Z. Effects of Targeted Versus Adjustable Protein Fortification of Breast Milk on Early Growth in Very Low-Birth-Weight Preterm Infants: A Randomized Clinical Trial. Nutr. Clin. Pract. 2020, 35, 335–343. [Google Scholar] [CrossRef] [PubMed]
- De Halleux, V.; Pieltain, C.; Senterre, T.; Studzinski, F.; Kessen, C.; Rigo, V.; Rigo, J. Growth Benefits of Own Mother’s Milk in Preterm Infants Fed Daily Individualized Fortified Human Milk. Nutrients 2019, 11, 772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kadioglu Simsek, G.; Alyamac Dizdar, E.; Arayici, S.; Canpolat, F.E.; Sari, F.N.; Uras, N.; Oguz, S.S. Comparison of the Effect of Three Different Fortification Methods on Growth of Very Low Birth Weight Infants. Breastfeed. Med. 2019, 14, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Maas, C.; Mathes, M.; Bleeker, C.; Vek, J.; Bernhard, W.; Wiechers, C.; Peter, A.; Poets, C.F.; Franz, A.R. Effect of Increased Enteral Protein Intake on Growth in Human Milk-Fed Preterm Infants: A Randomized Clinical Trial. JAMA Pediatr. 2017, 171, 16–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLeod, G.; Sherriff, J.; Hartmann, P.E.; Nathan, E.; Geddes, D.; Simmer, K. Comparing different methods of human breast milk fortification using measured v. assumed macronutrient composition to target reference growth: A randomised controlled trial. Br. J. Nutr. 2016, 115, 431–439. [Google Scholar] [CrossRef] [Green Version]
- Morlacchi, L.; Mallardi, D.; Gianni, M.L.; Roggero, P.; Amato, O.; Piemontese, P.; Consonni, D.; Mosca, F. Is targeted fortification of human breast milk an optimal nutrition strategy for preterm infants? An interventional study. J. Transl. Med. 2016, 14, 195. [Google Scholar] [CrossRef] [Green Version]
- Parat, S.; Raza, P.; Kamleh, M.; Super, D.; Groh-Wargo, S. Targeted Breast Milk Fortification for Very Low Birth Weight (VLBW) Infants: Nutritional Intake, Growth Outcome and Body Composition. Nutrients 2020, 12, 1156. [Google Scholar] [CrossRef]
- Reali, A.; Greco, F.; Marongiu, G.; Deidda, F.; Atzeni, S.; Campus, R.; Dessi, A.; Fanos, V. Individualized fortification of breast milk in 41 Extremely Low Birth Weight (ELBW) preterm infants. Clin. Chim. Acta. 2015, 451 Pt A, 107–110. [Google Scholar] [CrossRef]
- Polberger, S.; Räihä, N.C.; Juvonen, P.; Moro, G.E.; Minoli, I.; Warm, A. Individualized protein fortification of human milk for preterm infants: Comparison of ultrafiltrated human milk protein and a bovine whey fortifier. J. Pediatr. Gastroenterol. Nutr. 1999, 29, 332–338. [Google Scholar] [CrossRef]
- Kwan, C.; Fusch, G.; Rochow, N.; Fusch, C.; Kwan, C.; Fusch, G.; Rochow, N.; el-Helou, S.; Belfort, M.; Festival, J.; et al. Milk analysis using milk analyzers in a standardized setting (MAMAS) study: A multicentre quality initiative. Clin. Nutr. 2020, 39, 2121–2128. [Google Scholar] [CrossRef]
- Olsen, I.E.; Lawson, M.L.; Ferguson, A.N.; Cantrell, R.; Grabich, S.C.; Zemel, B.S.; Clark, R.H. BMI Curves for Preterm Infants. Pediatrics 2015, 135, e572–e581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziegler, E.E. Human milk and human milk fortifiers. World Rev. Nutr. Diet. 2014, 110, 215–227. [Google Scholar] [PubMed]
- Senterre, T. Practice of enteral nutrition in very low birth weight and extremely low birth weight infants. World Rev. Nutr. Diet. 2014, 110, 201–214. [Google Scholar] [PubMed]
- Thanigainathan, S.; Abiramalatha, T. Early fortification of human milk versus late fortification to promote growth in preterm infants. Cochrane Database Syst. Rev. 2020, 7, Cd013392. [Google Scholar] [CrossRef]
- Anderson, D.M. Nutritional assessment and therapeutic interventions for the preterm infant. Clin. Perinatol. 2002, 29, 313–326. [Google Scholar] [CrossRef]
- Greer, F.R.; Olsen, I.E. How Fast Should the Preterm Infant Grow? Curr. Pediatr. Rep. 2013, 1, 240–246. [Google Scholar] [CrossRef] [Green Version]
- Martin, C.R.; Brown, Y.F.; Ehrenkranz, R.A.; O’Shea, T.M.; Allred, E.N.; Belfort, M.B.; McCormick, M.C.; Leviton, A. Nutritional practices and growth velocity in the first month of life in extremely premature infants. Pediatrics 2009, 124, 649–657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olsen, I.E.; Harris, C.L.; Lawson, M.L.; Berseth, C.L. Higher protein intake improves length, not weight, z scores in preterm infants. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 409–416. [Google Scholar] [CrossRef]
- Fenton, T.R.; Anderson, D.; Groh-Wargo, S.; Hoyos, A.; Ehrenkranz, R.A.; Senterre, T. An Attempt to Standardize the Calculation of Growth Velocity of Preterm Infants-Evaluation of Practical Bedside Methods. J. Pediatr. 2018, 196, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Belfort, M.; Cherkerzian, S.; Bell, K.; Soldateli, B.; Cordova Ramos, E.; Palmer, C.; Steele, T.; Pepin, H.; Ellard, D.; Drouin, K.; et al. Macronutrient Intake from Human Milk, Infant Growth, and Body Composition at Term Equivalent Age: A Longitudinal Study of Hospitalized Very Preterm Infants. Nutrients 2020, 12, 2249. [Google Scholar] [CrossRef]
- Meyers, J.M.; Tan, S.; Bell, E.F.; Duncan, A.F.; Guillet, R.; Stoll, B.J.; D’Angio, C.T. Neurodevelopmental outcomes among extremely premature infants with linear growth restriction. J. Perinatol. 2019, 39, 193–202. [Google Scholar] [CrossRef]
- Ramel, S.E.; Demerath, E.W.; Gray, H.L.; Younge, N.; Boys, C.; Georgieff, M.K. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology 2012, 102, 19–24. [Google Scholar] [CrossRef]
- Fenton, T.R.; Groh-Wargo, S.; Gura, K.; Martin, C.R.; Taylor, S.N.; Griffin, I.J.; Rozga, M.; Moloney, L. Effect of Enteral Protein Amount on Growth and Health Outcomes in Very-Low-Birth-Weight Preterm Infants: Phase II of the Pre-B Project and an Evidence Analysis Center Systematic Review. J. Acad. Nutr. Diet. 2020. [Google Scholar] [CrossRef] [PubMed]
- Jo, D.B.; Hagadorn, J.I.; Smith, K.C.; Esposito, P.A.; Brownell, E.A. Macronutrient analysis of donor human milk labelled as 24 kcal/oz. J. Perinatol. 2020, 40, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Perrin, M.T.; Spence, E.H.; Belfort, M.B.; Parker, M.G.; Bode, L. A comparison of macronutrient-based methods for deriving energy values in human milk. J. Perinatol. 2020, 40, 1688–1693. [Google Scholar] [CrossRef]
- Andersson, Y.; Savman, K.; Blackberg, L.; Hernell, O. Pasteurization of mother’s own milk reduces fat absorption and growth in preterm infants. Acta Paediatr. 2007, 96, 1445–1449. [Google Scholar] [CrossRef] [PubMed]
- McManaman, J.L.; Martin Carli, J.F.; Monks, J. Chapter 4—Human milk lipids: An overview. In Human Milk; McGuire, M.K., O’connor, D.l., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 91–102. [Google Scholar]
- Takahashi, K.; Mizuno, K.; Itabashi, K. The freeze-thaw process and long intervals after fortification denature human milk fat globules. Am. J. Perinatol. 2012, 29, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Henderson, T.R.; Fay, T.N.; Hamosh, M. Effect of pasteurization on long chain polyunsaturated fatty acid levels and enzyme activities of human milk. J. Pediatr. 1998, 132, 876–878. [Google Scholar] [CrossRef]
- Peila, C.; Moro, G.E.; Bertino, E.; Cavallarin, L.; Giribaldi, M.; Giuliani, F.; Cresi, F.; Coscia, A. The Effect of Holder Pasteurization on Nutrients and Biologically-Active Components in Donor Human Milk: A Review. Nutrients 2016, 8, 477. [Google Scholar] [CrossRef] [Green Version]
- Ewaschuk, J.B.; Unger, S.; Harvey, S.; O’Connor, D.L.; Field, C.J. Effect of pasteurization on immune components of milk: Implications for feeding preterm infants. Appl. Physiol. Nutr. Metab. 2011, 36, 175–182. [Google Scholar] [CrossRef] [PubMed]

| Unfortified | Fortified to 24 kcal/oz | |||
|---|---|---|---|---|
| Protein (g/dL) | Energy (kcal/oz) | Protein (g/dL) | Energy (kcal/oz) | |
| DBM (purchased from OMMB) | 0.9 * | 20 * | 2.4 | 23.6 |
| DBM+ (90 mL DBM with 6 mL LPF) | 1.9 | 20.0 | 3.2 | 23.4 |
| Infants with Growth Data through 30 Days of Life | Infants with Growth Data through 36 Weeks PMA | |||||
|---|---|---|---|---|---|---|
| DBM | MBM | DBM+ | DBM | MBM | DBM+ | |
| n = 69 | n = 71 | n = 70 | n = 58 | n = 64 | n = 59 | |
| Male (%) | 38 (55%) | 43 (61%) | 32 (46%) | 36 (57%) | 41 (64%) | 26 (44%) * |
| Gestational age (weeks) | 28.9 ± 2.0 | 28.6 ± 1.8 | 29.0 ± 1.7 | 29.0 ± 2.0 | 28.6 ± 1.8 | 29.1 ± 1.7 |
| Birth weight (g) ^ | 1064.4 ± 260.0 | 1109.0 ± 241.9 | 1166.3 ± 230.1 ** | 1053.6 ± 258.5 | 1108.6 ± 230.9 | 1169.1 ± 228.6 ** |
| SGA at birth (%) | 11 (16%) | 6 (8%) | 4 (6%) ** | 11 (19%) | 5 (8%) | 4 (7%) ** |
| Days on donor milk ^ | 30 (28–30) * | 3 (2–4) | 30 (28–30) * | 30 (28–30) * | 3 (2–4) | 30 (29–30) * |
| Received > 24 kcal/oz in first 30 days (%) ^ | 54 (78%) * | 43 (61%) | 54 (77%) * | 44 (76%) | 40 (63%) | 48 (81%) * |
| % donor milk intake | 80.6 (22.8–94.7) | 85.0 (47.8–100) ** | 78.3 (21.9–96.3) | 88.7 (43.6–100) ** | ||
| Transitioned off donor milk early due to growth | 5 (7%) | 5 (7%) | 3 (5%) | 4 (7%) | ||
| 2015–2017 | 2019–2020 | p-Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| VLBW infants | 235 | 270 | |||||||||
| Stage 2 or 3 NEC | 14 (6.0%) | 15 (5.6%) | 0.85 | ||||||||
| MBM | DBM | Formula | MBM | DBM+ | DBM | Formula | |||||
| Stage 2 NEC | 3 | 7 | 1 | 3 | 1 | 0 | 5 | ||||
| Stage 3 NEC | 2 | 1 | 0 | 3 | 2 | 1 | 0 | ||||
| Total | 7 | 8 | 1 | 8 | 3 | 1 | 5 | ||||
| MBM | DBM | MBM | DBM+ | DBM | |||||||
| Feeding Intolerance | 5 | 4 | 4 | 3 | 1 | ||||||
| Total | 9 (3.8%) | 8 (3.0%) | 0.73 | ||||||||
| DBM (n = 69) | MBM (n = 71) | DBM+ (n = 70) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| All Groups | DBM vs. MBM | DBM vs. DBM+ | MBM vs. DBM+ | ||||
| Weight (g/kg/day) | |||||||
| Week 1 | 9.53 ± 7.52 | 9.07 ± 7.65 | 9.82 ± 8.07 | 0.85 | 0.94 | 0.97 | 0.83 |
| Week 2 | 13.69 ± 6.38 | 16.70 ± 6.39 | 13.28 ± 5.72 | 0.002 | 0.01 | 0.92 | 0.003 |
| Week 3 | 17.71 ± 5.84 | 18.84 ± 5.15 | 17.75 ± 5.19 | 0.37 | 0.43 | 1.00 | 0.45 |
| Week 4 | 17.16 ± 5.18 | 19.20 ± 5.77 | 17.75 ± 5.74 | 0.09 | 0.08 | 0.81 | 0.27 |
| Average | 13.79 ± 2.97 | 15.13 ± 2.99 | 14.03 ± 2.34 | 0.01 | 0.01 | 0.87 | 0.05 |
| Length (cm/week) | |||||||
| Week 1 | 0.59 ± 0.85 | 0.74 ± 0.75 | 0.90 ± 0.71 | 0.09 | 0.55 | 0.07 | 0.47 |
| Week 2 | 0.97 ± 0.72 | 0.81 ± 0.71 | 0.81 ± 0.81 | 0.35 | 0.42 | 0.43 | 1.00 |
| Week 3 | 0.95 ± 0.78 | 1.18 ± 0.69 | 1.10 ± 0.61 | 0.16 | 0.15 | 0.42 | 0.81 |
| Week 4 | 1.03 ± 0.64 | 1.03 ± 0.59 | 1.08 ± 0.58 | 0.86 | 1.00 | 0.89 | 0.88 |
| Average | 0.90 ± 0.26 | 0.95 ± 0.23 | 0.97 ± 0.28 | 0.24 | 0.45 | 0.22 | 0.89 |
| HC (cm/week) | |||||||
| Week 1 | 0.14 ± 0.77 | 0.04 ± 0.81 | 0.18 ± 0.77 | 0.58 | 0.77 | 0.93 | 0.56 |
| Week 2 | 0.67 ± 0.55 | 0.85 ± 0.55 | 0.59 ± 0.58 | 0.03 | 0.18 | 0.68 | 0.03 |
| Week 3 | 1.01 ± 0.54 | 1.00 ± 0.51 | 0.84 ± 0.48 | 0.10 | 0.99 | 0.13 | 0.17 |
| Week 4 | 1.01 ± 0.60 | 1.07 ± 0.58 | 1.03 ± 0.63 | 0.83 | 0.82 | 0.98 | 0.92 |
| Average | 0.70 ± 0.30 | 0.74 ± 0.29 | 0.67 ± 0.27 | 0.36 | 0.71 | 0.80 | 0.33 |
| DBM (n = 58) | MBM (n = 64) | DBM+ (n = 59) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| All Groups | DBM vs. MBM | DBM vs. DBM+ | MBM vs. DBM+ | ||||
| Weight | −0.50 ± 0.47 | −0.26 ± 0.51 | −0.59 ± 0.40 | <0.001 | 0.01 | 0.58 | <0.001 |
| Length | −1.00 ± 0.57 | −0.94 ± 0.55 | −0.97 ± 0.50 | 0.87 | 0.85 | 0.95 | 0.97 |
| HC | −0.22 ± 0.70 | −0.30 ± 0.77 | −0.46 ± 0.70 | 0.20 | 0.84 | 0.19 | 0.43 |
| BMI | 0.60 ± 0.94 | 0.74 ± 0.79 | 0.24 ± 0.72 | 0.005 | 0.66 | 0.06 | 0.004 |
| MBM (Reference) | DBM Parameter Estimate | p-Value | DBM+ Parameter Estimate | p-Value | |
|---|---|---|---|---|---|
| Weight velocity (g/kg/day) | |||||
| Average | 14.85 | −1.59 (−2.46, −0.72) | <0.001 | −1.02 (−1.88, −0.15) | 0.02 |
| Length velocity (cm/week) | |||||
| Average | 0.94 | −0.060 (−0.15, 0.031) | 0.20 | 0.022 (−0.067, 0.11) | 0.63 |
| HC velocity (cm/week) | |||||
| Average | 0.72 | −0.053 (−0.15, 0.042) | 0.27 | −0.065 (−0.16, 0.029) | 0.18 |
| DBM (vs. MBM) Parameter Estimate | p-Value | DBM+ (vs. MBM) Parameter Estimate | p-Value | |
|---|---|---|---|---|
| Weight | −0.0051 (−0.0086, −0.0016) | 0.004 | −0.0062 (−0.0095, −0.0029) | <0.001 |
| Length | −0.0019 (−0.0052, 0.0014) | 0.25 | −0.0017 (−0.0048, 0.0014) | 0.29 |
| HC | 0.0013 (−0.0031, 0.0057) | 0.57 | −0.0033 (−0.0078, 0.0012) | 0.15 |
| BMI | −0.0018 (−0.007, 0.0035) | 0.51 | −0.0086 (−0.0132, −0.004) | <0.001 |
| DBM (Reference) | DBM+ Parameter Estimate | p-Value | |
|---|---|---|---|
| Weight velocity (g/kg/day) | |||
| Average | 13.27 | 0.57 (−0.30, 1.45) | 0.20 |
| Length velocity (cm/week) | |||
| Week 1 | 0.59 | 0.31 (0.035, 0.58) | 0.03 |
| Average | 0.88 | 0.082 (−0.0085, 0.17) | 0.08 |
| HC velocity (cm/week) | |||
| Average | 0.67 | −0.012 (−0.11, 0.083) | 0.80 |
| DBM+ (vs. DBM) Parameter Estimate | p-Value | |
|---|---|---|
| Weight | −0.0011 (−0.0046, 0.0024) | 0.54 |
| Length | 0.0003 (−0.0032, 0.0037) | 0.88 |
| HC | −0.0046 (−0.0093, 0.0001) | 0.05 |
| BMI | −0.0068 (−0.0121, −0.0015) | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fu, T.T.; Kaplan, H.C.; Fields, T.; Folger, A.T.; Gordon, K.; Poindexter, B.B. Protein Enrichment of Donor Breast Milk and Impact on Growth in Very Low Birth Weight Infants. Nutrients 2021, 13, 2869. https://doi.org/10.3390/nu13082869
Fu TT, Kaplan HC, Fields T, Folger AT, Gordon K, Poindexter BB. Protein Enrichment of Donor Breast Milk and Impact on Growth in Very Low Birth Weight Infants. Nutrients. 2021; 13(8):2869. https://doi.org/10.3390/nu13082869
Chicago/Turabian StyleFu, Ting Ting, Heather C. Kaplan, Trayce Fields, Alonzo T. Folger, Katelyn Gordon, and Brenda B. Poindexter. 2021. "Protein Enrichment of Donor Breast Milk and Impact on Growth in Very Low Birth Weight Infants" Nutrients 13, no. 8: 2869. https://doi.org/10.3390/nu13082869






