A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
- overweight or obesity, i.e., body mass index (BMI) >25, or waist circumference >102 cm (males), >88 cm (females);
- dyslipidemia without pharmacological treatment, i.e., total cholesterol >220 mg/dL, or HDL cholesterol (high-density lipoprotein) <35 mg/dL, or low-density lipoprotein cholesterol (LDL) >130 mg/dL, or triglycerides >200 mg/dL;
- fasting glucose levels >120 mg/dl and/or reduced tolerance to glucose or diabetes mellitus, without pharmacological treatment was determined through HbA1c.
- 10 mL of peripheral blood were drawn in the morning after a fasting night to determine haematological parameters.
2.2. Clinical Parameters
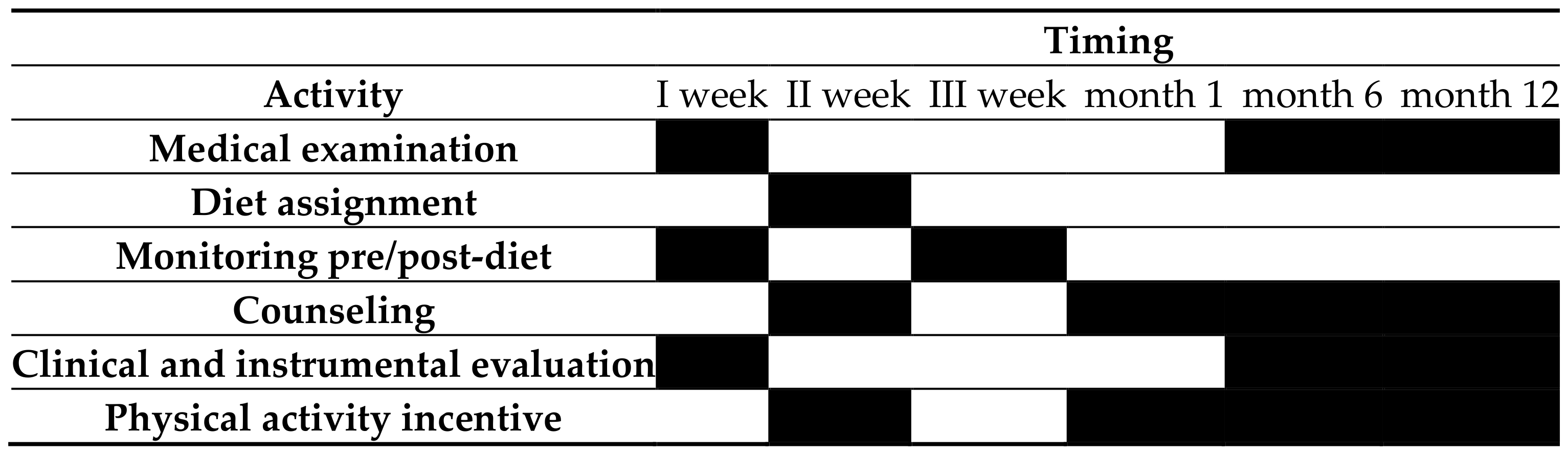
2.3. Investigation Timetable
2.4. Statistical Analysis
3. Results
Characteristics of the Sample at Time Zero (T0)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Backholer, K.; Sacks, G.; Cameron, A.J. Food and beverage price promotions: An untapped policy target for improving population diets and health. Curr. Nutr. Rep. 2019, 8, 250–255. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Chu, L.-L. The health promotion lifestyle of metabolic syndrome individuals with a diet and exercise programme. Int. J. Nurs. Pract. 2014, 20, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Spence, A.C.; Campbell, K.J.; Crawford, D.A.; McNaughton, S.A.; Hesketh, K.D. Mediators of improved child diet quality following a health promotion intervention: The melbourne InFANT program. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 137. [Google Scholar] [CrossRef] [Green Version]
- Samara, A.; Andersen, P.T.; Aro, A.R. Health promotion and obesity in the arab gulf states: Challenges and good practices. J. Obes. 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Perry, L.; Nicholls, R.; Duffield, C.; Gallagher, R. Building expert agreement on the importance and feasibility of workplace health promotion interventions for nurses and midwives: A modified delphi consultation. J. Adv. Nurs. 2017, 73, 2587–2599. [Google Scholar] [CrossRef] [PubMed]
- Mah, C.L.; Luongo, G.; Hasdell, R.; Taylor, N.G.A.; Lo, B.K. A systematic review of the effect of retail food environment interventions on diet and health with a focus on the enabling role of public policies. Curr. Nutr. Rep. 2019, 8, 411–428. [Google Scholar] [CrossRef] [Green Version]
- Muto, G.; Yokoyama, K.; Endo, M. Solutions against declining birthrates confronting japan’s aging society by supporting female workers in harmonizing work with their health and social issues: Fertility, chronic illness, and raising children. Nihon. Eiseigaku Zasshi 2018, 73, 200–209. [Google Scholar] [CrossRef] [Green Version]
- Zigmont, V.A.; Shoben, A.B.; Kaye, G.L.; Snow, R.J.; Clinton, S.K.; Harris, R.E.; Olivo-Marston, S.E. An evaluation of reach for a work site implementation of the national diabetes prevention program focusing on diet and exercise. Am. J. Health Promot. 2018, 32, 1417–1424. [Google Scholar] [CrossRef]
- Syed, I.U.B. Diet, physical activity, and emotional health: What works, what doesn’t, and why we need integrated solutions for total worker health. BMC Public Health 2020, 20, 152. [Google Scholar] [CrossRef] [Green Version]
- Stanulewicz, N.; Knox, E.; Narayanasamy, M.; Shivji, N.; Khunti, K.; Blake, H. Effectiveness of lifestyle health promotion interventions for nurses: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 17. [Google Scholar] [CrossRef] [Green Version]
- Ni Mhurchu, C.; Aston, L.M.; Jebb, S.A. Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health 2010, 10, 62. [Google Scholar] [CrossRef] [Green Version]
- Song, Z.; Baicker, K. Effect of a workplace wellness program on employee health and economic outcomes: A randomized clinical trial. JAMA 2019, 321, 1491–1501. [Google Scholar] [CrossRef] [PubMed]
- Sharman, M.J.; Jose, K.A.; Venn, A.J.; Banks, S.; Ayton, J.; Cleland, V.J. I love having a healthy lifestyle A qualitative study investigating body mass index trajectories from childhood to mid-adulthood. BMC Obes. 2019, 6, 16. [Google Scholar] [CrossRef]
- Bracci, M.; Zabaleta, M.E.; Tartaglione, M.F.; Ledda, C.; Rapisarda, V.; Santarelli, L. Exosomal miR-92a concentration in the serum of shift workers. Appl. Sci. 2020, 10, 430. [Google Scholar] [CrossRef] [Green Version]
- Lafranconi, A.; Ray, S.; Grosso, G. Editorial: Public health nutrition: Assessing evidence to determine policy and practice. Front. Public Health 2019, 7, 21. [Google Scholar] [CrossRef] [Green Version]
- Reddy, P.; Lent-Schochet, D.; Ramakrishnan, N.; McLaughlin, M.; Jialal, I. Metabolic syndrome is an inflammatory disorder: A conspiracy between adipose tissue and phagocytes. Clin. Chim. Acta 2019, 496, 35–44. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, P.G.; Kowalczyk, C.; Bindeman, J.; Taylor, A.J. The impact of cardiovascular risk factor case management on the metabolic syndrome in a primary prevention population: Results from a randomized controlled trial. J. Cardiometab. Syndr. 2006, 1, 6–12. [Google Scholar] [CrossRef]
- Hricik, D.E. Metabolic syndrome in kidney transplantation: Management of risk factors. Clin. J. Am. Soc. Nephrol. 2011, 6, 1781–1785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassells, H.B.; Haffner, S.M. The metabolic syndrome: Risk factors and management. J. Cardiovasc. Nurs. 2006, 21, 306–313. [Google Scholar] [CrossRef]
- Ledda, C.; Loreto, C.; Rapisarda, V. Telomere length as a biomarker of biological aging in shiftworkers. Appl. Sci. 2020, 10, 2764. [Google Scholar] [CrossRef]
- Bracci, M.; Copertaro, A.; Ciarapica, V.; Barbaresi, M.; Esposito, S.; Albanesi, A.; Valentino, M.; Ledda, C.; Rapisarda, V.; Santarelli, L. Nocturnin gene diurnal variation in healthy volunteers and expression levels in shift workers. BioMed Res. Int. 2019, 2019, 7582734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramaci, T.; Rapisarda, V.; Bellini, D.; Mucci, N.; De Giorgio, A.; Barattucci, M. Mindfulness as a Protective Factor for Dissatisfaction in HCWs: The Moderating Role of Mindful Attention between Climate Stress and Job Satisfaction. Int. J. Environ. Res. Public Health 2020, 17, 3818. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Ledda, C.; Genovese, C.; Contrino, E.; Vitale, E.; Maida, C.M.; Squeri, R.; Vitale, F.; Rapisarda, V. Immunization Status against Measles of Health-Care Workers Operating at Three Sicilian University Hospitals: An Observational Study. Vaccines 2019, 7, 175. [Google Scholar] [CrossRef] [Green Version]
- Rapisarda, V.; Loreto, C.; Vitale, E.; Matera, S.; Ragusa, R.; Coco, G.; Rapisarda, L.; Ledda, C. Incidence of sharp and needle-stick injuries and mucocutaneous blood exposure among healthcare workers. Future Microbiol. 2019, 14, 27–31. [Google Scholar] [CrossRef]
- Rapisarda, V.; Nunnari, G.; Senia, P.; Vella, F.; Vitale, E.; Murabito, P.; Salerno, M.; Ledda, C. Hepatitis B vaccination coverage among medical residents from Catania University Hospital, Italy. Future Microbiol. 2019, 14, 41–44. [Google Scholar] [CrossRef]
- Garozzo, A.; Falzone, L.; Rapisarda, V.; Marconi, A.; Cinà, D.; Fenga, C.; Spandidos, D.A.; Libra, M. The risk of HCV infection among health-care workers and its association with extrahepatic manifestations (Review). Mol. Med. Rep. 2017, 15, 3336–3339. [Google Scholar] [CrossRef] [Green Version]
- Chukwura, C.L.; Santo, T.J.; Waters, C.N.; Andrews, A. ‘Nutrition is out of our control’: Soldiers’ perceptions of their local food environment. Public Health Nutr. 2019, 22, 2766–2776. [Google Scholar] [CrossRef] [Green Version]
- Lindo, J.L.M.; Lagrenade, J.; Eldemire-Shearer, D. The health of office-based workers in kingston, jamaica. Work Health Saf. 2017, 65, 74–82. [Google Scholar] [CrossRef]
- National Cancer Institute. Compendium of Physical Activities. Available online: https://sites/compendiumofphysicalactivities/Activity-Categories (accessed on 25 December 2019).
- International Physical Activity Questionnaire (IPAQ). Guidelines for Data Processing and Analysis of the Short form 2004. Available online: http://www.institutferran.org/documentos/scoring_short_ipaq_april04.pdf (accessed on 30 November 2020).
- National Health and Nutrition Examination Survey (NHANES). Anthropometry Procedures Manual. Available online: https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf (accessed on 27 October 2020).
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [Green Version]
- Gamperiene, M.; Nygård, J.F.; Sandanger, I.; Lau, B.; Bruusgaard, D. Self-reported work ability of norwegian women in relation to physical and mental health, and to the work environment. J. Occup. Med. Toxicol. 2008, 3, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuomi, K.; Ilmarinen, J.; Jahkola, A.; Katajarinne, L.; Tulkki, A. Work Ability Index, 2nd ed.; Institute of Occupational Health: Helsinki, Finland, 2006. [Google Scholar]
- Stunkard, A.J.; Sørensen, T.; Schulsinger, F. Use of the danish adoption register for the study of obesity and thinness. Res. Publ. Assoc. Res. Nerv. Ment. Dis. 1983, 60, 115–120. [Google Scholar]
- Talati, Z.; Pettigrew, S.; Moore, S.; Pratt, I.S. Adults and children prefer a plate food guide relative to a pyramid. Asia Pac. J. Clin. Nutr. 2017, 26, 169–174. [Google Scholar] [PubMed]
- Scapellato, M.L.; Comiati, V.; Buja, A.; Buttignol, G.; Valentini, R.; Burati, V.; La Serra, L.; Maccà, I.; Mason, P.; Scopa, P.; et al. Combined before-and-after workplace intervention to promote healthy lifestyles in healthcare workers (STI-VI study): Short-term assessment. Int. J. Environ. Res. Public Health 2018, 15, 2053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groeneveld, I.F.; Proper, K.I.; van der Beek, A.J.; van Mechelen, W. Sustained body weight reduction by an individual-based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: Results of a randomized controlled trial. Prev. Med. 2010, 51, 240–246. [Google Scholar] [CrossRef]
- Christensen, J.R.; Faber, A.; Ekner, D.; Overgaard, K.; Holtermann, A.; Søgaard, K. Diet, physical exercise and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical ability in health care workers A randomized controlled trial. BMC Public Health 2011, 11, 671. [Google Scholar] [CrossRef] [Green Version]
- Barroso, M.; Zomeño, M.D.; Díaz, J.L.; Pérez-Fernández, S.; Martí-Lluch, R.; Cordón, F.; Ramos, R.; Cabezas, C.; Salvador, G.; Castell, C.; et al. Control of cardiovascular risk factors with tailored recommendations: A randomized controlled trial. Prev. Med. 2020, 141, 106302. [Google Scholar] [CrossRef]
- Peng, Y.; Wang, Z. Do the 2017 blood pressure cut-offs improve 10-year cardiovascular disease mortality risk prediction? Nutr. Metab. Cardiovasc. Dis. 2020, 30, 2008–2016. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.; Gans, K.; McCurdy, K.; Risica, P.M.; Jennings, E.; Gorin, A.; Papandonatos, G.D.; Tovar, A. Rationale, design and study protocol of the ‘Strong families start at home’ feasibility trial to improve the diet quality of low-income, ethnically diverse children by helping parents improve their feeding and food preparation practices. Contemp. Clin. Trials. Comm. 2020, 19, 100583. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.W.M.; Choi, K.C.; Yum, R.W.Y.; Yu, D.S.F.; Chair, S.Y. Effectiveness of motivational interviewing on lifestyle modification and health outcomes of clients at risk or diagnosed with cardiovascular diseases: A systematic review. Int. J. Nurs. Stud. 2016, 53, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Mecca, M.S.; Moreto, F.; Burini, F.H.P.; Dalanesi, R.C.; McLellan, K.C.P.; Burini, R.C. Ten-week lifestyle changing program reduces several indicators for metabolic syndrome in overweight adults. Diabetol. Metab. Syndr. 2012, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Koenig, W.; Sund, M.; During, A.; Ernst, E. Leisure-time physical activity but not work-related physical activity is associated with decreased plasma viscosity: Results from a large population sample. Circulation 1997, 95, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Fisac, J.L.; Guallar-Castillón, P.; Díez-Gañán, L.; López García, E.; Banegas Banegas, J.R.; Rodríguez Artalejo, F. Work-related physical activity is not associated with body mass index and obesity. Obes. Res. 2002, 10, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Kouvonen, A.; Kivimäki, M.; Elovainio, M.; Virtanen, M.; Linna, A.; Vahtera, J. Job strain and leisure-time physical activity in female and male public sector employees. Prev. Med. 2005, 41, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Lallukka, T.; Sarlio-Lähteenkorva, S.; Kaila-Kangas, L.; Pitkäniemi, J.; Luukkonen, R.; Leino-Arjas, P. Working conditions and weight gain: A 28-year follow-up study of industrial employees. Eur. J. Epidemiol. 2008, 23, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Trinkoff, A.M.; Geiger-Brown, J. Factors associated with work-related fatigue and recovery in hospital nurses working 12-h shifts. Work 2014, 62, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Pattyn, N.; Cornelissen, V.A.; Toghi Eshghi, S.R.; Vanhees, L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome. Sports Med. 2013, 43, 121–133. [Google Scholar] [CrossRef] [Green Version]
- Blackford, K.; Jancey, J.; Lee, A.H.; James, A.P.; Waddell, T.; Howat, P. Home-based lifestyle intervention for rural adults improves metabolic syndrome parameters and cardiovascular risk factors: A randomised controlled trial. Prev. Med. 2016, 89, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Ahmad, T.; Chasman, D.I.; Buring, J.E.; Lee, I.-; Ridker, P.M.; Everett, B.M. Physical activity modifies the effect of LPL, LIPC, and CETP polymorphisms on HDL-C levels and the risk of myocardial infarction in women of european ancestry. Circ. Cardiovasc. Genet. 2011, 4, 74–80. [Google Scholar] [CrossRef] [Green Version]
- Kelley, G.A.; Kelley, K.S.; Vu Tran, Z. Aerobic exercise, lipids and lipoproteins in overweight and obese adults: A meta-analysis of randomized controlled trials. Int. J. Obes. 2005, 29, 881–893. [Google Scholar] [CrossRef] [Green Version]
- Radwan, H.; Hasan, H.A.; Ismat, H.; Hakim, H.; Khalid, H.; Al-Fityani, L.; Mohammed, R.; Ayman, A. Body mass index perception, body image dissatisfaction and their relations with weight-related behaviors among university students. Int. J. Environ. Res. Public Health 2019, 16, 1541. [Google Scholar] [CrossRef] [Green Version]
- Agodi, A.; Barchitta, M.; Quattrocchi, A.; Maugeri, A.; Canto, C.; Marchese, A.E.; Vinciguerra, M. Low fruit consumption and folate deficiency are associated with LINE-1 hypomethylation in women of a cancer-free population. Genes Nutr. 2015, 10, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agodi, A.; Barchitta, M.; Valenti, G.; Quattrocchi, A.; Marchese, A.E.; Oliveri Conti, G.; Fallico, R.; Sciacca, S.; Ferrante, M. Dietary folate intake and blood biomarkers reveal high-risk groups in a mediterranean population of healthy women of childbearing potential. Ann. Nutr. Metab. 2013, 63, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Quattrocchi, A.; Maugeri, A.; Barone, G.; Mazzoleni, P.; Catalfo, A.; Guidi, G.D.; Iemmolo, M.; Crimi, N.; Agodi, A. Integrated approach of nutritional and molecular epidemiology, mineralogical and chemical pollutant characterisation: The protocol of a cross-sectional study in women. BMJ Open 2017, 7, e014756. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Quattrocchi, A.; Adornetto, V.; Marchese, A.E.; Agodi, A. Tumor necrosis factor-alpha -308 G>A polymorphism, adherence to mediterranean diet, and risk of overweight/obesity in young women. BioMed. Res. Int. 2014, 2014. [Google Scholar] [CrossRef]
- Maugeri, A.; Barchitta, M.; Fiore, V.; Rosta, G.; Favara, G.; La Mastra, C.; La Rosa, M.C.; San Lio, R.M.; Agodi, A. Determinants of adherence to the mediterranean diet: Findings from a cross-sectional study in women from southern Italy. Int. J. Environ. Res. Public Health 2019, 16, 2963. [Google Scholar] [CrossRef] [Green Version]
- Ledda, C.; Cinà, D.; Matera, S.; Mucci, N.; Bracci, M.; Rapisarda, V. High HOMA-IR index in healthcare shift workers. Medicina 2019, 55, 186. [Google Scholar] [CrossRef] [Green Version]
- Ramaci, T.; Pellerone, M.; Ledda, C.; Rapisarda, V. Health promotion, psychological distress, and disease prevention in the workplace: A cross-sectional study of italian adults. Risk Manag. Healthc. Policy 2017, 10, 167–175. [Google Scholar] [CrossRef] [Green Version]
- Fiore, M.; Ledda, C.; Rapisarda, V.; Sentina, E.; Mauceri, C.; DAgati, P.; Conti, G.O.; Serra-Majem, L.; Ferrante, M. Medical school fails to improve mediterranean diet adherence among medical students. Eur. J. Public Health 2015, 25, 1019–1023. [Google Scholar] [CrossRef] [Green Version]

| Males (n = 17) | Females (n = 21) | Value of p | |
|---|---|---|---|
| Age (years) | 48.5 ± 7.4 | 49.3 ± 7.9 | n.s. |
| Cigarette Packages/year | 5.1 ± 10.6 | 4.8 ± 9.2 | n.s. |
| Medical doctor | 3 (17%) | 4 (19%) | n.s. |
| Technician | 4 (24%) | 3 (14%) | n.s. |
| Nurses | 10 (59%) | 14 (67%) | n.s. |
| Working seniority | 13.4 ± 4.6 | 14.2 ± 4.9 | n.s. |
| Area of involvement | clinical (n = 7); surgical (n = 7), Services (n = 3) | clinical (n = 6); surgical (n = 10), Services (n = 5) | n.s. |
| T0 | T6 | T12 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Gender Differences | Males | Females | Males T0 vs. T6 | Females T0 vs. T6 | Males | Females | Males T6 vs. T12 | Females T6 vs. T12 | Males T0Vs T12 | Females T0 vs. T12 | |
| SBP (mmHg) | 138.1 ± 13.8 | 132.4 ± 11.7 | n.s. | 131.3 ± 11.6 | 128.5 ± 12.3 | n.s. | n.s. | 128.3 ± 12.4 | 126.1 ± 10.1 | n.s. | n.s. | <0.05 * | n.s. |
| DBP (mmHg) | 88.5 ± 6.9 | 86.2 ± 6.4 | n.s. | 86.4 ± 6.3 | 83.1 ± 5.3 | n.s. | n.s. | 85.7 ± 6.1 | 82.5 ± 4.8 | n.s. | n.s. | n.s. | <0.05 * |
| Waist circumference (cm) | 97.6 ± 7.5 | 88.5 ± 9.3 | <0.05 * | 96.4 ± 6.1 | 86.9 ± 7.8 | n.s. | n.s. | 95.1 ± 4.7 | 86.1 ± 6.7 | n.s. | n.s. | n.s. | n.s. |
| BMI (cm2/kg) | 26.9 ± 3.9 | 26.8 ± 5.1 | n.s. | 25.8 ± 5.2 | 25.4 ± 4.9 | n.s. | n.s. | 24.2 ± 3.7 | 24.1 ± 2.8 | n.s. | n.s. | <0.05 * | <0.05 * |
| WHR index | 0.97 ± 0.09 | 0.91 ± 0.06 | n.s. | 0.92 ± 0.87 | 0.89 ± 0.97 | n.s. | n.s. | 0.90 ± 0.77 | 0.88 ± 0.81 | n.s. | n.s. | n.s. | n.s. |
| Total cholesterol (mg/dL) | 221.8 ± 29.6 | 218.7 ± 24.9 | n.s. | 220.4 ± 27.3 | 211.3 ± 25.4 | n.s. | n.s. | 203.2 ± 20.3 | 204.1 ± 19.6 | <0.05 * | n.s. | <0.05 * | <0.05 * |
| HDL cholesterol (mg/dL) | 56.3 ± 13.2 | 60.1 ± 15.9 | n.s. | 56.4 ± 13.6 | 61.1 ± 14.8 | n.s. | n.s. | 56.9 ± 11.4 | 61.9 ± 14.4 | n.s. | n.s. | n.s. | n.s. |
| LDL cholesterol (mg/dL) | 147.7 ± 21.4 | 146.6 ± 23.5 | n.s. | 143.5 ± 20.2 | 142.2 ± 21.4 | n.s. | n.s. | 140.2 ± 20.3 | 140.7 ± 20.1 | n.s. | n.s. | n.s. | n.s. |
| Triglycerides (mg/dL) | 161.4 ± 75.4 | 155.4 ± 66.5 | n.s. | 152.8 ± 76.2 | 152.1 ± 63.1 | n.s. | n.s. | 148.9 ± 77.1 | 148.3 ± 57.2 | n.s. | n.s. | n.s. | n.s. |
| Blood glucose (mg/dL) | 98.2 ± 11.3 | 96.4 ± 10.9 | n.s. | 96.5 ± 10.4 | 92.1 ± 9.8 | n.s. | n.s. | 93.1 ± 9.4 | 89.3 ± 9.4 | n.s. | n.s. | n.s. | <0.05 * |
| Physical activity (n. sub.) | 4 (24%) | 6 (29%) | n.s. | 15 (88%) | 21 (100%) | <0.05 * | <0.05 * | 17 (100%) | 21 (100%) | n.s. | n.s. | <0.05 * | <0.05 * |
| Physical activity (MET) | 486.9 ±317.5 | 299.9 ±101.3 | <0.05 * | 541.1 ±219.4 | 358.8 ±180.4 | n.s. | n.s. | 615.6 ±345.1 | 417.5 ±234.4 | n.s. | n.s. | n.s. | <0.05 * |
| T0 Males | T12 Males | p -Value | T0 Females | T12 Females | p -Value | |
|---|---|---|---|---|---|---|
| Adherence to diet | 4.6 ± 2.3 | 7.7 ± 1.7 | 0.001 * | 4.8 ± 1.9 | 7.9 ± 1.9 | 0.001 * |
| WAI index | 28.3 ± 7.5 | 38.2 ± 7.9 | 0.001 * | 27.1 ± 7.5 | 37.7 ± 6.3 | 0.001 * |
| BID ≥ 1 | 17 (100%) | 5 (%) | n.s. | 21 (100%) | 8 (%) | n.s. |
| BID < 1 | 0 | 0 | n.s. | 0 | 0 | n.s. |
| BID = 0 | 0 | 12 (71%) | n.s. | 0 | 13 (62%) | n.s. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rapisarda, V.; Cannizzaro, E.; Barchitta, M.; Vitale, E.; Cinà, D.; Minciullo, F.; Matera, S.; Bracci, M.; Agodi, A.; Ledda, C. A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study. J. Clin. Med. 2021, 10, 1512. https://doi.org/10.3390/jcm10071512
Rapisarda V, Cannizzaro E, Barchitta M, Vitale E, Cinà D, Minciullo F, Matera S, Bracci M, Agodi A, Ledda C. A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study. Journal of Clinical Medicine. 2021; 10(7):1512. https://doi.org/10.3390/jcm10071512
Chicago/Turabian StyleRapisarda, Venerando, Emanuele Cannizzaro, Martina Barchitta, Ermanno Vitale, Diana Cinà, Fabrizia Minciullo, Serena Matera, Massimo Bracci, Antonella Agodi, and Caterina Ledda. 2021. "A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study" Journal of Clinical Medicine 10, no. 7: 1512. https://doi.org/10.3390/jcm10071512










