Effect of a 6-Week Physical Education Intervention on Motor Competence in Pre-School Children with Developmental Coordination Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measurements
2.4. Procedures
2.5. Ethics
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
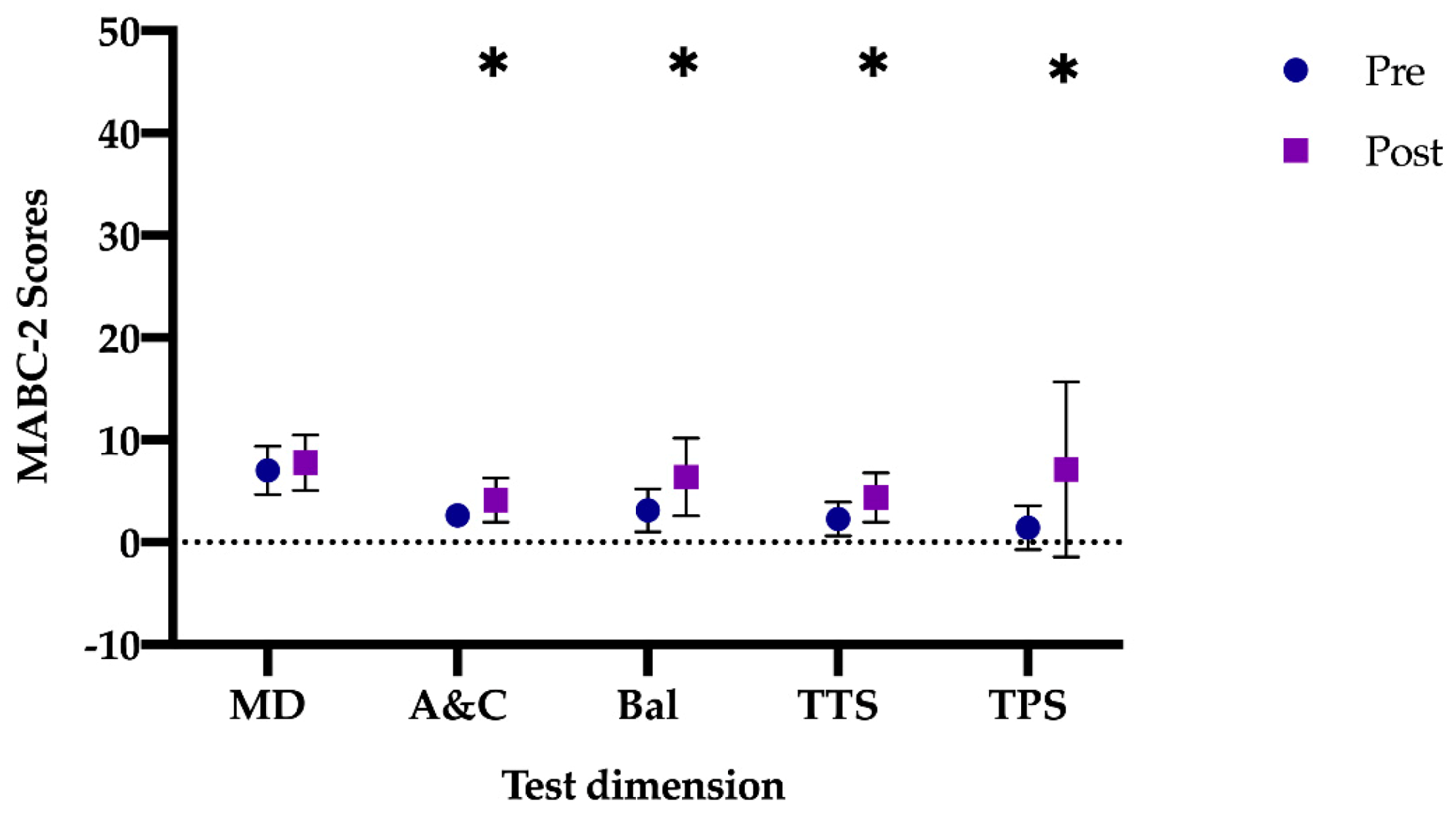
3.2. Control Group Outcomes
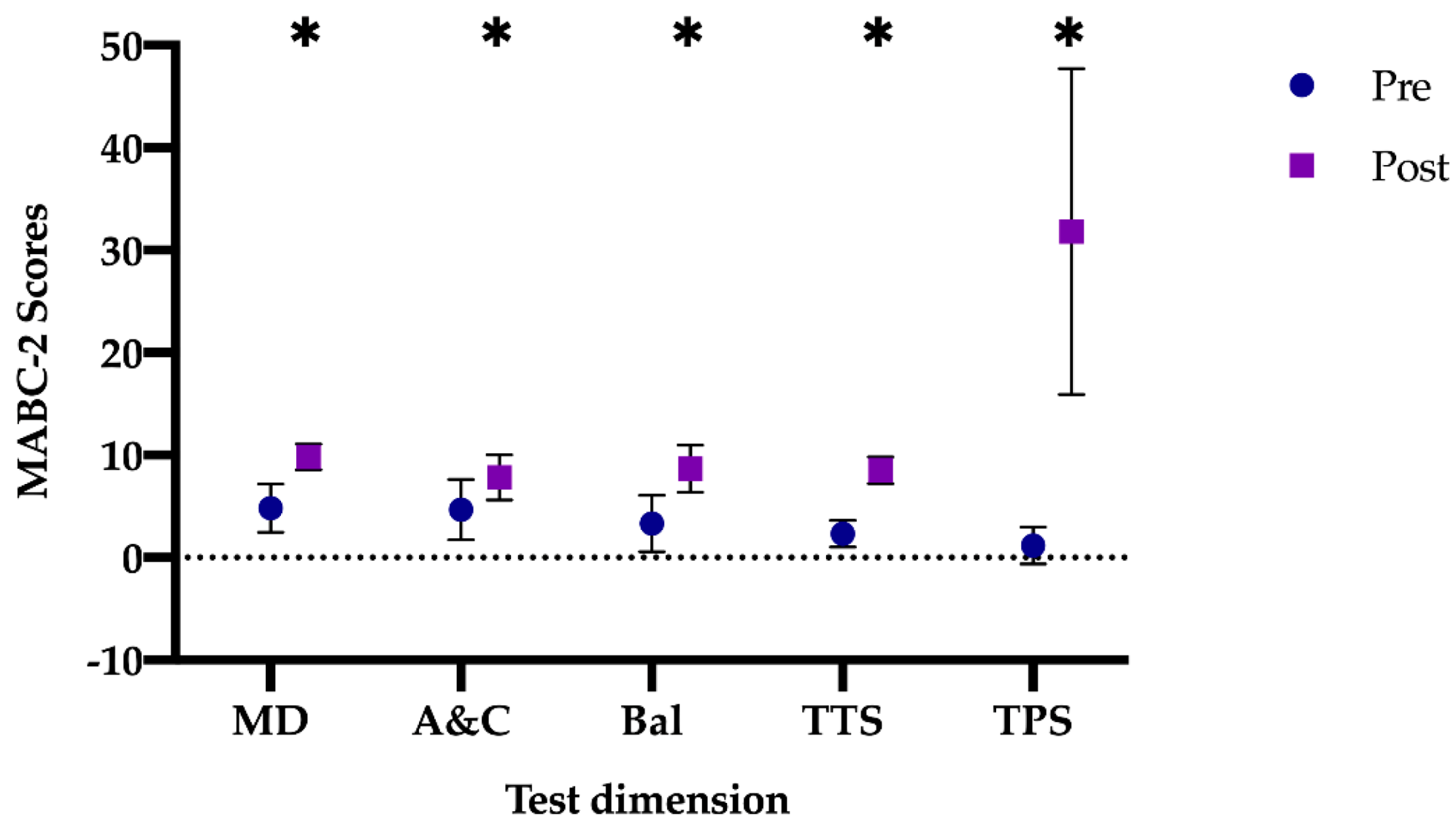
3.3. Intervention Group Outcomes
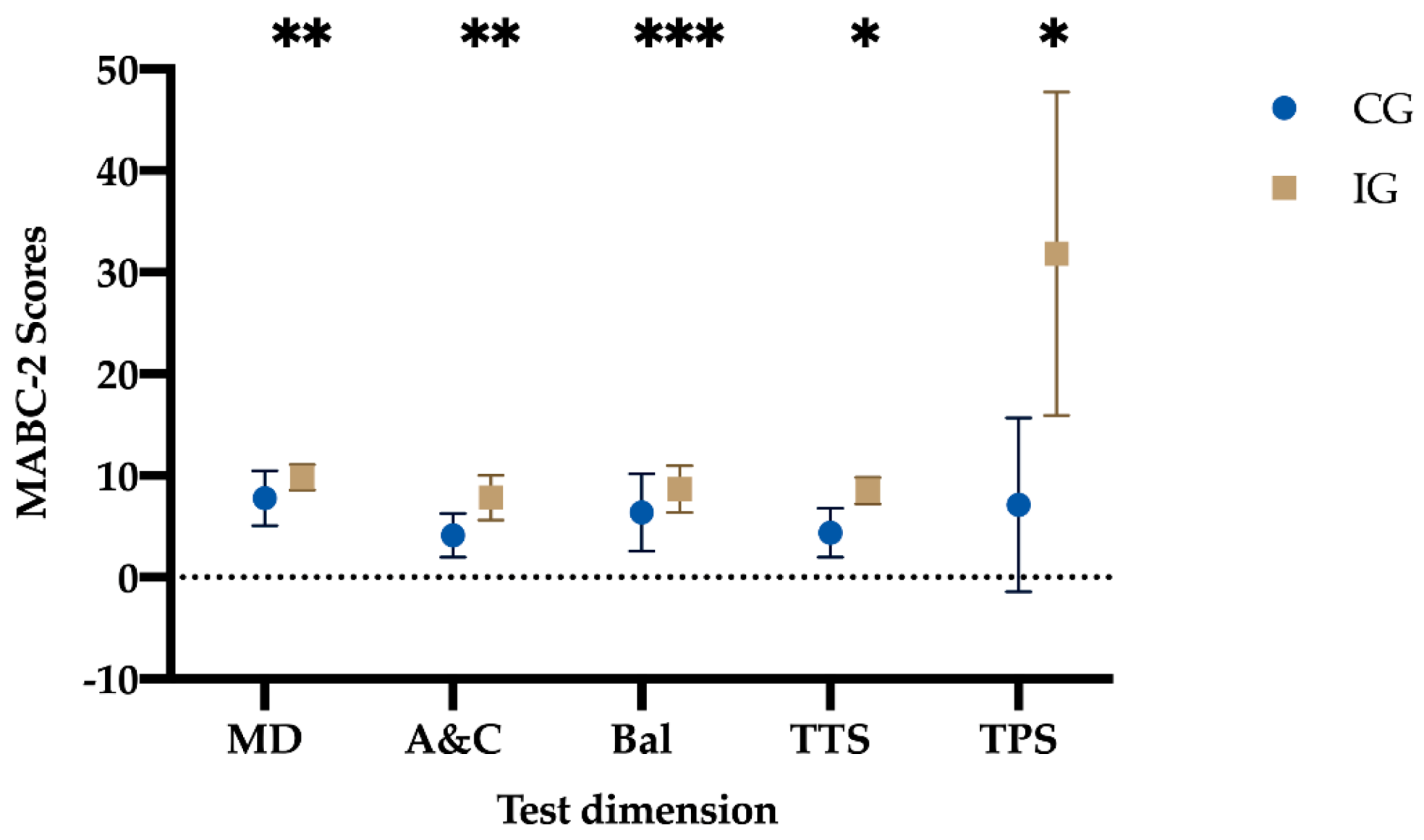
3.4. Intervention Group vs. Control Group Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bornstein, M.H.; Hendricks, C. Screening for developmental disabilities in developing countries. Soc. Sci. Med. 2013, 97, 307–315. [Google Scholar] [CrossRef]
- Hendrix, C.G.; Prins, M.R.; Dekkers, H. Developmental coordination disorder and overweight and obesity in children: A systematic review. Obes. Rev. 2014, 15, 408–423. [Google Scholar] [CrossRef] [PubMed]
- Lingam, R.; Jongmans, M.J.; Ellis, M.; Hunt, L.P.; Golding, J.; Emond, A. Mental Health Difficulties in Children With Developmental Coordination Disorder. Pediatrics 2012, 129, e882–e891. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Sit, C.H.P.; Capio, C.M.; Burnett, A.; Ha, A.S.C.; Huang, W.Y.J. Fundamental movement skills proficiency in children with developmental coordination disorder: Does physical self-concept matter? Disabil. Rehabil. 2016, 38, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.E.; Metcalfe, J.S. The mountain of motor development: A metaphor. In Motor Development: Research and Reviews; Clark, J.E., Humphrey, J., Eds.; NASPE Publications: Reston, VA, USA, 2002; pp. 163–190. [Google Scholar]
- Cobley, S.; Abraham, C.; Baker, J. Relative age effects on physical education attainment and school sport representation. Phys. Educ. Sport Pedagog. 2008, 13, 267–276. [Google Scholar] [CrossRef]
- Almond, L. Serious flaws in an FMS interpretation of physical literacy. Sci. Sports 2014, 29, S60. [Google Scholar] [CrossRef]
- Malina, R.M.; Bouchard, C.; Bar-Or, O. Growth, Maturation, and Physical Activity; Human Kinetics: Champaign, IL, USA, 2004; ISBN 0880118822. [Google Scholar]
- Bardid, F.; Deconinck, F.J.A.; Descamps, S.; Verhoeven, L.; De Pooter, G.; Lenoir, M.; D’Hondt, E. The effectiveness of a fundamental motor skill intervention in pre-schoolers with motor problems depends on gender but not environmental context. Res. Dev. Disabil. 2013, 34, 4571–4581. [Google Scholar] [CrossRef]
- Castro Zubizarreta, A.; Ezquerra Muñoz, M.P.; Argos González, J. Fundamentos Teóricos de la Educación Infantil; Universidad de Cantabria: Santander, Spain, 2017; Volume 25, ISBN 978-84-8102-822-5. [Google Scholar]
- Gallahue, D.L.; Ozmun, J.C.; Goodway, J. Understanding Motor Development: Infants, Children, Adolescents, Adults, 7th ed.; McGraw-Hill: New York, NY, USA, 2012; ISBN 9780073376509. [Google Scholar]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Fisher, A.; Reilly, J.J.; Kelly, L.A.; Montgomery, C.; Williamson, A.; Paton, J.Y.; Grant, S. Fundamental Movement Skills and Habitual Physical Activity in Young Children. Med. Sci. Sport. Exerc. 2005, 37, 684–688. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents. Sport. Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.G.; Pfeiffer, K.A.; O’Neill, J.R.; Dowda, M.; McIver, K.L.; Brown, W.H.; Pate, R.R. Motor Skill Performance and Physical Activity in Preschool Children. Obesity 2008, 16, 1421–1426. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- Roth, K.; Ruf, K.; Obinger, M.; Mauer, S.; Ahnert, J.; Schneider, W.; Graf, C.; Hebestreit, H. Is there a secular decline in motor skills in preschool children? Scand. J. Med. Sci. Sports 2010, 20, 670–678. [Google Scholar] [CrossRef]
- Beltrame, T.S.; Capistrano, R.; Alexandre, J.M.; Lisboa, T.; Andrade, R.D.; Felden, É.P.G. Prevalência do Transtorno do Desenvolvimento da Coordenação em uma amostra de crianças brasileiras. Cad. Bras. Ter. Ocup. 2017, 25, 105–113. [Google Scholar] [CrossRef]
- Pulzi, W.; Rodrigues, G.M. Transtorno do Desenvolvimento da Coordenação: Uma Revisão de Literatura. Rev. Bras. Educ. Espec. 2015, 21, 433–444. [Google Scholar] [CrossRef]
- Dos Santos, V.A.P.; Vieira, J.L.L. Prevalência de desordem coordenativa desenvolvimental em crianças com 7 a 10 anos de idade. Rev. Bras. Cineantropometria Desempenho Hum. 2013, 15, 233–242. [Google Scholar] [CrossRef]
- Wilson, P.H.; Ruddock, S.; Smits-Engelsman, B.; Polatajko, H.; Blank, R. Understanding performance deficits in developmental coordination disorder: A meta-analysis of recent research. Dev. Med. Child Neurol. 2013, 55, 217–228. [Google Scholar] [CrossRef]
- Amador-Ruiz, S.; Gutierrez, D.; Martínez-Vizcaíno, V.; Gulías-González, R.; Pardo-Guijarro, M.J.; Sánchez-López, M. Motor Competence Levels and Prevalence of Developmental Coordination Disorder in Spanish Children: The MOVI-KIDS Study. J. Sch. Health 2018, 88, 538–546. [Google Scholar] [CrossRef]
- Wang, T.-N.; Tseng, M.-H.; Wilson, B.N.; Hu, F.-C. Functional performance of children with developmental coordination disorder at home and at school. Dev. Med. Child Neurol. 2009, 51, 817–825. [Google Scholar] [CrossRef]
- Deconinck, F.J.A.; Savelsbergh, G.J.P.; De Clercq, D.; Lenoir, M. Balance problems during obstacle crossing in children with Developmental Coordination Disorder. Gait Posture 2010, 32, 327–331. [Google Scholar] [CrossRef]
- Bart, O.; Jarus, T.; Erez, Y.; Rosenberg, L. How do young children with DCD participate and enjoy daily activities? Res. Dev. Disabil. 2011, 32, 1317–1322. [Google Scholar] [CrossRef]
- King-Dowling, S.; Missiuna, C.; Rodriguez, M.C.; Greenway, M.; Cairney, J. Co-occurring motor, language and emotional–behavioral problems in children 3–6years of age. Hum. Mov. Sci. 2015, 39, 101–108. [Google Scholar] [CrossRef]
- Magalhães, L.C.; Cardoso, A.A.; Missiuna, C. Activities and participation in children with developmental coordination disorder: A systematic review. Res. Dev. Disabil. 2011, 32, 1309–1316. [Google Scholar] [CrossRef]
- Prunty, M.M.; Barnett, A.L.; Wilmut, K.; Plumb, M.S. An examination of writing pauses in the handwriting of children with Developmental Coordination Disorder. Res. Dev. Disabil. 2014, 35, 2894–2905. [Google Scholar] [CrossRef] [PubMed]
- Rosa Neto, F.; Dos Santos, A.P.M.; Xavier, R.F.C.; Amaro, K.N. A importância da avaliação motora em escolares: Análise da confiabilidade da escala de desenvolvimento motor. Rev. Bras. Cineantropometria Desempenho Hum. 2010, 12, 422–427. [Google Scholar] [CrossRef]
- Pless, M.; Carlsson, M.; Sundelin, C.; Persson, K. Effects of Group Motor Skill Intervention on Five- to Six-Year-Old Children with Developmental Coordination Disorder. Pediatr. Phys. Ther. 2000, 12, 183–189. [Google Scholar] [CrossRef]
- Graupera, J.L.; Ruiz, L.M. Batería de Evaluación del Movimiento Para Niños-2; Pearson: Madrid, Spain, 2012; Volume 2. [Google Scholar]
- Blank, R.; Smits-Engelsman, B.; Polatajko, H.; Wilson, P. European Academy for Childhood Disability (EACD): Recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Dev. Med. Child Neurol. 2012, 54, 54–93. [Google Scholar] [CrossRef]
- Schoemaker, M.M.; Smits-Engelsman, B.C.M. Is Treating Motor Problems in DCD Just a Matter of Practice and More Practice? Curr. Dev. Disord. Rep. 2015, 2, 150–156. [Google Scholar] [CrossRef]
- Honrubia-Montesinos, C.; Gil-Madrona, P.; Losada-Puente, L. Motor Development among Spanish Preschool Children. Children 2021, 8, 41. [Google Scholar] [CrossRef]
- Gao, Z.; Zeng, N.; Pope, Z.C.; Wang, R.; Yu, F. Effects of exergaming on motor skill competence, perceived competence, and physical activity in preschool children. J. Sport Heal. Sci. 2019, 8, 106–113. [Google Scholar] [CrossRef]
- Palmer, K.K.; Chinn, K.M.; Robinson, L.E. The effect of the CHAMP intervention on fundamental motor skills and outdoor physical activity in preschoolers. J. Sport Health Sci. 2019, 8, 98–105. [Google Scholar] [CrossRef]
- Hillier, S. Intervention for Children with Developmental Coordination Disorder: A Systematic Review. Internet J. Allied Health Sci. Pract. 2007, 5, 1–11. [Google Scholar]
- Smits-Engelsman, B.C.M.; Blank, R.; Van Der Kaay, A.-C.; Mosterd-Van Der Meijs, R.; Vlugt-Van Den Brand, E.; Polatajko, H.J.; Wilson, P.H. Efficacy of interventions to improve motor performance in children with developmental coordination disorder: A combined systematic review and meta-analysis. Dev. Med. Child Neurol. 2013, 55, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.J.; Burnett, A.F.; Sit, C.H. Motor Skill Interventions in Children With Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 2076–2099. [Google Scholar] [CrossRef] [PubMed]
- Caçola, P.; Romero, M.; Ibana, M.; Chuang, J. Effects of two distinct group motor skill interventions in psychological and motor skills of children with Developmental Coordination Disorder: A pilot study. Disabil. Health J. 2016, 9, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Hung, W.W.Y.; Pang, M.Y.C. Effects of group-based versus individual-based exercise training on motor performance in children with developmental coordination disorder: A randomized controlled pilot study. J. Rehabil. Med. 2010, 42, 122–128. [Google Scholar] [CrossRef]
- Dunford, C. Goal-Orientated Group Intervention for Children with Developmental Coordination Disorder. Phys. Occup. Ther. Pediatr. 2011, 31, 288–300. [Google Scholar] [CrossRef]
- Ato, M.; López, J.J.; Benavente, A. Un sistema de clasificación de los diseños de investigación en psicología. An. Psicol. 2013, 29, 1038–1059. [Google Scholar] [CrossRef]
- Henderson, S.E.; Sudgen, D.A.; Barnett, A. Movement Assessment Battery for Children-2, 2nd ed.; The Psychological Corporation: London, UK, 2007. [Google Scholar]
- Schoemaker, M.M.; Niemeijer, A.S.; Flapper, B.C.T.; Smits-Engelsman, B.C.M. Validity and reliability of the Movement Assessment Battery for Children-2 Checklist for children with and without motor impairments. Dev. Med. Child Neurol. 2012, 54, 368–375. [Google Scholar] [CrossRef]
- Valentini, N.C.; Ramalho, M.H.; Oliveira, M.A. Movement assessment battery for children-2: Translation, reliability, and validity for Brazilian children. Res. Dev. Disabil. 2014, 35, 733–740. [Google Scholar] [CrossRef]
- Serbetar, I.; Loftesnes, J.M.; Mamen, A. Reliability and Structural Validity of the Movement Assessment Battery for Children-2 in Croatian Preschool Children. Sports 2019, 7, 248. [Google Scholar] [CrossRef]
- Ministerio de Educación y Ciencia. Real Decreto 1630/2006, de 29 de Diciembre, por el que se Establecen las Enseñanzas Mínimas del Segundo ciclo de Educación Infantil; Ministerio de Educación y Ciencia: Madrid, Spain, 2007.
- Logan, S.W.; Robinson, L.E.; Wilson, A.E.; Lucas, W.A. Getting the fundamentals of movement: A meta-analysis of the effectiveness of motor skill interventions in children. Child. Care. Health Dev. 2012, 38, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Thornton, A.; Licari, M.; Reid, S.; Armstrong, J.; Fallows, R.; Elliott, C. Cognitive Orientation to (Daily) Occupational Performance intervention leads to improvements in impairments, activity and participation in children with Developmental Coordination Disorder. Disabil. Rehabil. 2016, 38, 979–986. [Google Scholar] [CrossRef]
- Au, M.K.; Chan, W.M.; Lee, L.; Chen, T.M.K.; Chau, R.M.W.; Pang, M.Y.C. Core stability exercise is as effective as task-oriented motor training in improving motor proficiency in children with developmental coordination disorder: A randomized controlled pilot study. Clin. Rehabil. 2014, 28, 992–1003. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, G.D.; Jelsma, D.; Jelsma, J.; Smits-Engelsman, B.C.M. The efficacy of two task-orientated interventions for children with Developmental Coordination Disorder: Neuromotor Task Training and Nintendo Wii Fit training. Res. Dev. Disabil. 2013, 34, 2449–2461. [Google Scholar] [CrossRef] [PubMed]
- Noordstar, J.J.; van der Net, J.; Voerman, L.; Helders, P.J.M.; Jongmans, M.J. The effect of an integrated perceived competence and motor intervention in children with developmental coordination disorder. Res. Dev. Disabil. 2017, 60, 162–175. [Google Scholar] [CrossRef]
- Wilson, P.H.; Adams, I.L.J.; Caeyenberghs, K.; Thomas, P.; Smits-Engelsman, B.; Steenbergen, B. Motor imagery training enhances motor skill in children with DCD: A replication study. Res. Dev. Disabil. 2016, 57, 54–62. [Google Scholar] [CrossRef]
- Jongmans, M.J.; Linthorst-Bakker, E.; Westenberg, Y.; Smits-Engelsman, B.C.M. Use of a task-oriented self-instruction method to support children in primary school with poor handwriting quality and speed. Hum. Mov. Sci. 2003, 22, 549–566. [Google Scholar] [CrossRef]
- Jongmans, M.J.; Smits-Engelsman, B.C.M.; Schoemaker, M.M. Consequences of Comorbidity of Developmental Coordination Disorders and Learning Disabilities for Severity and Pattern of Perceptual—Motor Dysfunction. J. Learn. Disabil. 2003, 36, 528–537. [Google Scholar] [CrossRef]
- Farhat, F.; Hsairi, I.; Baati, H.; Smits-Engelsman, B.C.M.; Masmoudi, K.; Mchirgui, R.; Triki, C.; Moalla, W. The effect of a motor skills training program in the improvement of practiced and non-practiced tasks performance in children with developmental coordination disorder (DCD). Hum. Mov. Sci. 2016, 46, 10–22. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Vinçon, S.; Blank, R.; Quadrado, V.H.; Polatajko, H.; Wilson, P.H. Evaluating the evidence for motor-based interventions in developmental coordination disorder: A systematic review and meta-analysis. Res. Dev. Disabil. 2018, 74, 72–102. [Google Scholar] [CrossRef]
- Wood, G.; Miles, C.A.L.; Coyles, G.; Alizadehkhaiyat, O.; Vine, S.J.; Vickers, J.N.; Wilson, M.R. A randomized controlled trial of a group-based gaze training intervention for children with Developmental Coordination Disorder. PLoS ONE 2017, 12, e0171782. [Google Scholar] [CrossRef] [PubMed]
- Niemeijer, A.S.; Smits-Engelsman, B.C.M.; Schoemaker, M.M. Neuromotor task training for children with developmental coordination disorder: A controlled trial. Dev. Med. Child Neurol. 2007, 49, 406–411. [Google Scholar] [CrossRef] [PubMed]
| Test Dimension (Range) | Sub-Test |
|---|---|
| Manual dexterity | 1st: Post coins (MD1) |
| 2nd: Threading beads (MD2) | |
| 3rd: Drawing trail (MD3) | |
| Aiming and catching | 4th: Catching bean bag (AC1) |
| 5th: Throwing bean bag onto mat (AC2) | |
| Balance | 6th: One-leg balance (Bal1) |
| 7th: Walking heels raised (Bal2) | |
| 8th: Jumping on mats (Bal3) | |
| Total test score (1–19) | MD1 + MD2 + MD3 + AC1 + AC2 + Bal1 + Bal2 + Bal3 |
| Total percentile score (0.1–99.9) | |
| Session Number | Objectives | Tasks (Skills) |
|---|---|---|
| Session 1 “I explore my body” | Introduce manual dexterity, balance and global throwing and catching skills through games | “We play with the tweezers” (manual dexterity) “Balance chase game” (balance) “Do not fall!” (aiming and catching) “Manual golf” (aiming and catching) “The jumping kangaroos” (balance) |
| Session 2 “I develop my motor skills” | Improve fine motor and manual dexterity, jot down tasks, grasp and balance | “Wrap the giraffe” (manual dexterity) “Shooting into the tunnel” (aiming and catching) “Balance circuit” (balance) |
| Session 3 “The art of catching” | Develop manual dexterity with both hands and practice the tasks of catching and receiving various objects | “Chinese carriers” (manual dexterity) “Catch practice” (catching) “Catch and win” (catching) “Molded animals” (manual dexterity) |
| Session 4 “Sharpen your aim” | Improve fine motor skills in both hands. Develop aim and precision when throwing objects | “The coin catcher” (manual dexterity) “Aim for the bullseye” (aiming) “Double throw” (aiming and catching) “The labyrinth” (manual dexterity) |
| Session 5: “Circus tightrope walkers” | Work on manual dexterity and fine motor skills, develop static and dynamic balance | “Paste-stickers” (manual dexterity) “The stilts” (balance) “The rescue” (balance and aiming and catching) “The endless line” (balance) “To pick up!” |
| Session 6: “Motor circuits” | Remember through the motor circuit, tasks and games performed in previous sessions. Work with manual dexterity, aiming, grip and balancing | “The circuit” (manual dexterity; aiming and catching; balance) “Circuit 1” (manual dexterity; aiming and catching; balance) “Circuit 2” (manual dexterity; aiming and catching; balance) |
| Total Sample | Control Group | Intervention Group | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Manual dexterity | Boys | 6.27 | 2.69 | 4.00 | 0.00 | 4.20 | 2.04 |
| Girls | 5.33 | 2.06 | 8.00 | 1.89 | 8.00 | 2.04 | |
| Total | 6.07 | 2.56 | 7.00 | 2.36 | 4.83 | 2.36 | |
| Aiming and catching | Boys | 3.81 | 2.46 | 2.83 | 1.11 | 5.00 | 3.12 |
| Girls | 2.33 | 0.51 | 2.00 | 0.00 | 3.00 | 0.00 | |
| Total | 3.50 | 2.26 | 2.62 | 1.02 | 4.66 | 2.93 | |
| Balance | Boys | 3.00 | 2.46 | 2.50 | 1.97 | 3.60 | 2.95 |
| Girls | 4.00 | 1.78 | 5.00 | 1.15 | 2.00 | 0.00 | |
| Total | 3.21 | 2.34 | 3.12 | 2.09 | 3.33 | 2.74 | |
| Total test score | Boys | 2.45 | 1.65 | 2.50 | 1.88 | 2.40 | 1.42 |
| Girls | 1.66 | 0.51 | 1.50 | 0.57 | 2.00 | 0.00 | |
| Total | 2.28 | 1.51 | 2.25 | 1.69 | 2.33 | 1.30 | |
| Total percentile score | Boys | 1.58 | 2.14 | 1.80 | 2.36 | 1.32 | 1.94 |
| Girls | 0.36 | 0.20 | 0.30 | 0.23 | 0.50 | 0.00 | |
| Total | 1.32 | 1.96 | 1.42 | 2.13 | 1.18 | 1.78 | |
| Total Sample | Control Group | Intervention Group | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Manual dexterity | Boys | 9.00 | 1.69 | 8.33 | 1.66 | 9.80 | 1.39 |
| Girls | 7.33 | 4.13 | 6.00 | 4.61 | 10.00 | 0.00 | |
| Total | 8.64 | 2.42 | 7.75 | 2.72 | 9.83 | 1.26 | |
| Aiming and catching | Boys | 6.36 | 2.80 | 4.66 | 2.22 | 8.40 | 1.95 |
| Girls | 3.33 | 1.36 | 2.50 | 0.57 | 5.00 | 0.00 | |
| Total | 5.71 | 2.83 | 4.12 | 2.15 | 7.83 | 2.20 | |
| Balance | Boys | 6.81 | 3.40 | 5.83 | 4.10 | 8.00 | 1.88 |
| Girls | 9.33 | 2.73 | 8.00 | 2.30 | 12.00 | 0.00 | |
| Total | 7.35 | 3.39 | 6.37 | 3.79 | 8.66 | 2.30 | |
| Total test Score | Boys | 6.36 | 2.83 | 4.66 | 2.60 | 8.40 | 1.42 |
| Girls | 5.33 | 3.14 | 3.50 | 1.73 | 9.00 | 0.00 | |
| Total | 6.14 | 2.87 | 4.37 | 2.41 | 8.50 | 1.31 | |
| Total Percentile Score | Boys | 18.69 | 17.42 | 8.60 | 9.41 | 30.80 | 17.36 |
| Girls | 14.16 | 17.82 | 2.75 | 2.59 | 37.00 | 0.00 | |
| Total | 17.72 | 17.27 | 7.13 | 8.55 | 31.83 | 15.89 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro-Patón, R.; Martín-Ayala, J.L.; Martí González, M.; Hernández, A.; Mecías-Calvo, M. Effect of a 6-Week Physical Education Intervention on Motor Competence in Pre-School Children with Developmental Coordination Disorder. J. Clin. Med. 2021, 10, 1936. https://doi.org/10.3390/jcm10091936
Navarro-Patón R, Martín-Ayala JL, Martí González M, Hernández A, Mecías-Calvo M. Effect of a 6-Week Physical Education Intervention on Motor Competence in Pre-School Children with Developmental Coordination Disorder. Journal of Clinical Medicine. 2021; 10(9):1936. https://doi.org/10.3390/jcm10091936
Chicago/Turabian StyleNavarro-Patón, Rubén, Juan Luis Martín-Ayala, Mariacarla Martí González, Alba Hernández, and Marcos Mecías-Calvo. 2021. "Effect of a 6-Week Physical Education Intervention on Motor Competence in Pre-School Children with Developmental Coordination Disorder" Journal of Clinical Medicine 10, no. 9: 1936. https://doi.org/10.3390/jcm10091936
APA StyleNavarro-Patón, R., Martín-Ayala, J. L., Martí González, M., Hernández, A., & Mecías-Calvo, M. (2021). Effect of a 6-Week Physical Education Intervention on Motor Competence in Pre-School Children with Developmental Coordination Disorder. Journal of Clinical Medicine, 10(9), 1936. https://doi.org/10.3390/jcm10091936








