Chemotherapeutic Potential of Epimedium brevicornum Extract: The cGMP-Specific PDE5 Inhibitor as Anti-Infertility Agent Following Long-Term Administration of Tramadol in Male Rats
Abstract
:1. Introduction
2. Materials and Methods
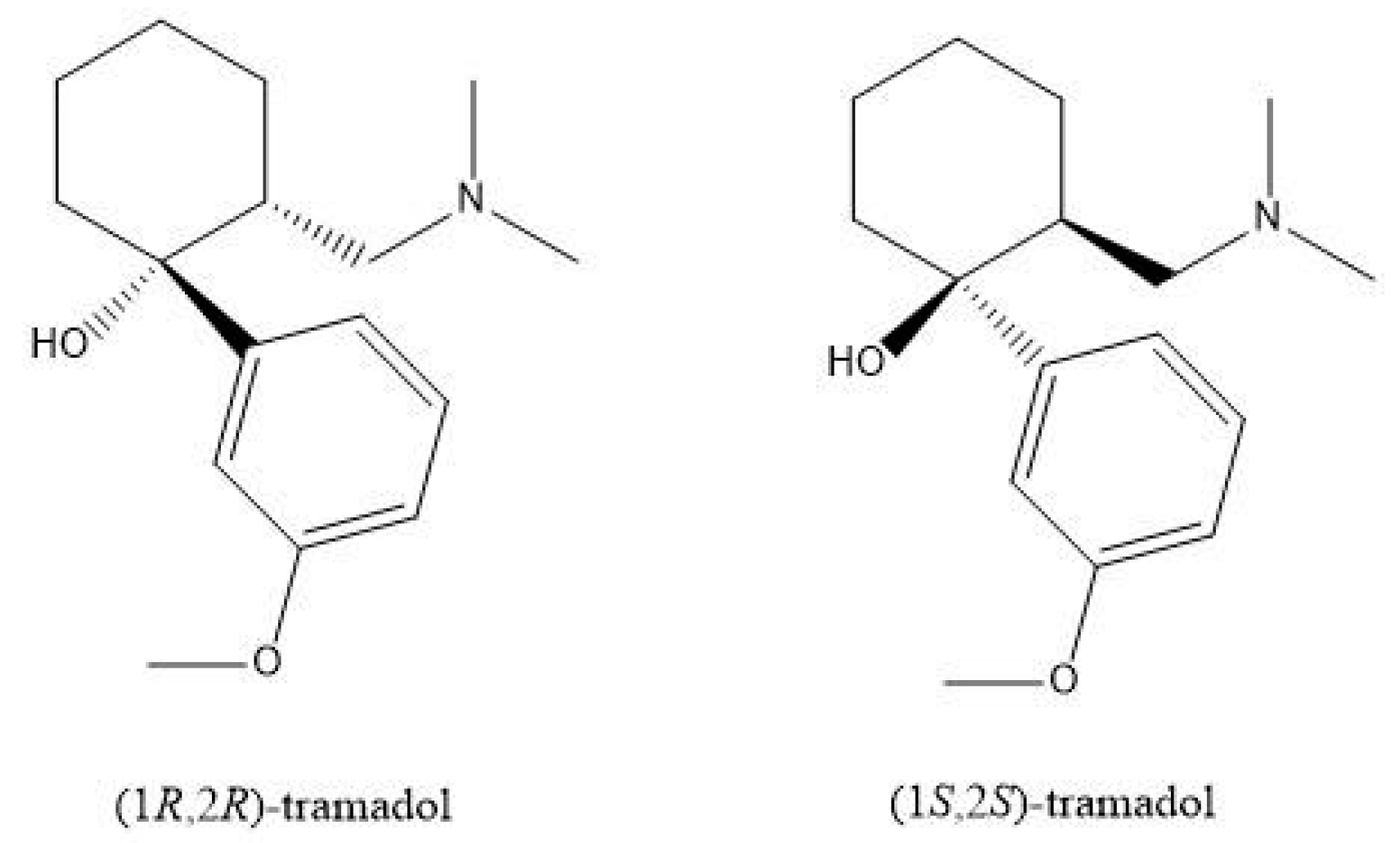
2.1. Chemicals
2.2. Animal Use
2.3. Model Building
2.4. Sample Collection
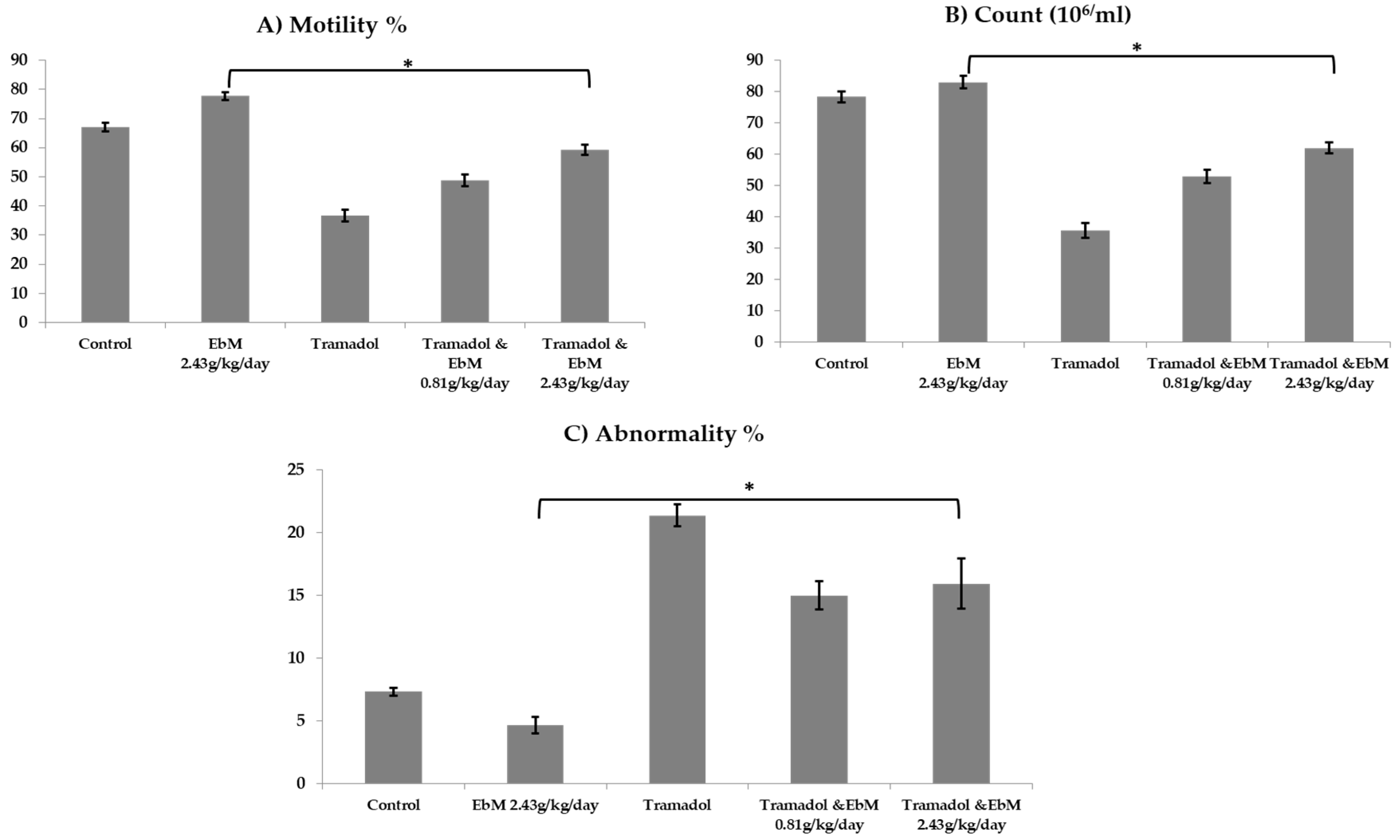
2.5. Semen Assessment and Sperm Parameters
2.6. Hormonal Analysis
2.7. Assessment of NO and Antioxidant Scavenging Capacity
2.8. Relative Quantitative RT-PCR Analysis
2.9. The Testes Morphology
2.10. Statistical Analysis
3. Results
3.1. Efficacy of Oral Administration of E. brevicornum extract and/or Tramadol on Semen Parameters
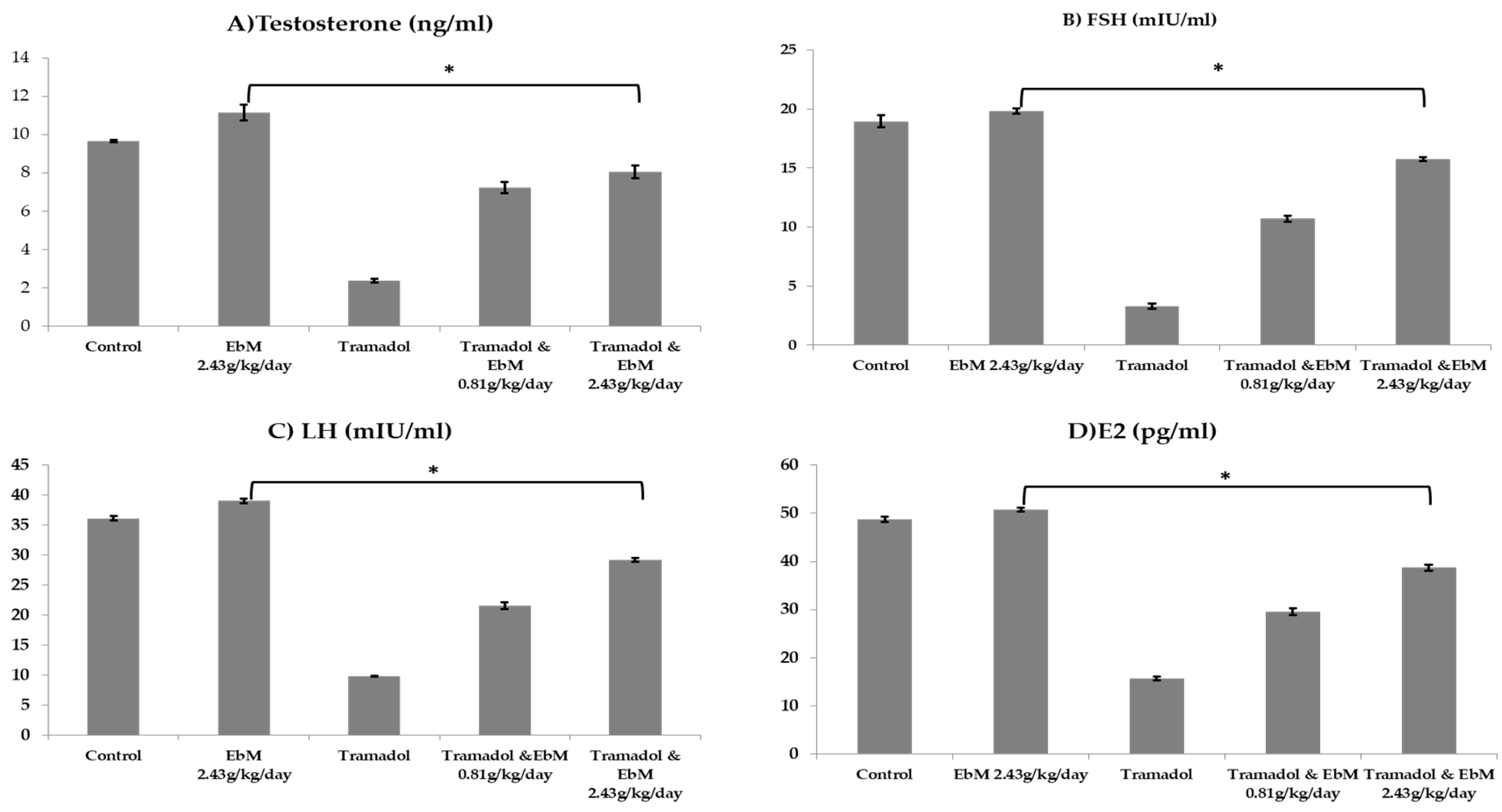
3.2. Effect of E. brevicornum Extract and/or Tramadol Oral Administration on the Hormonal Assay
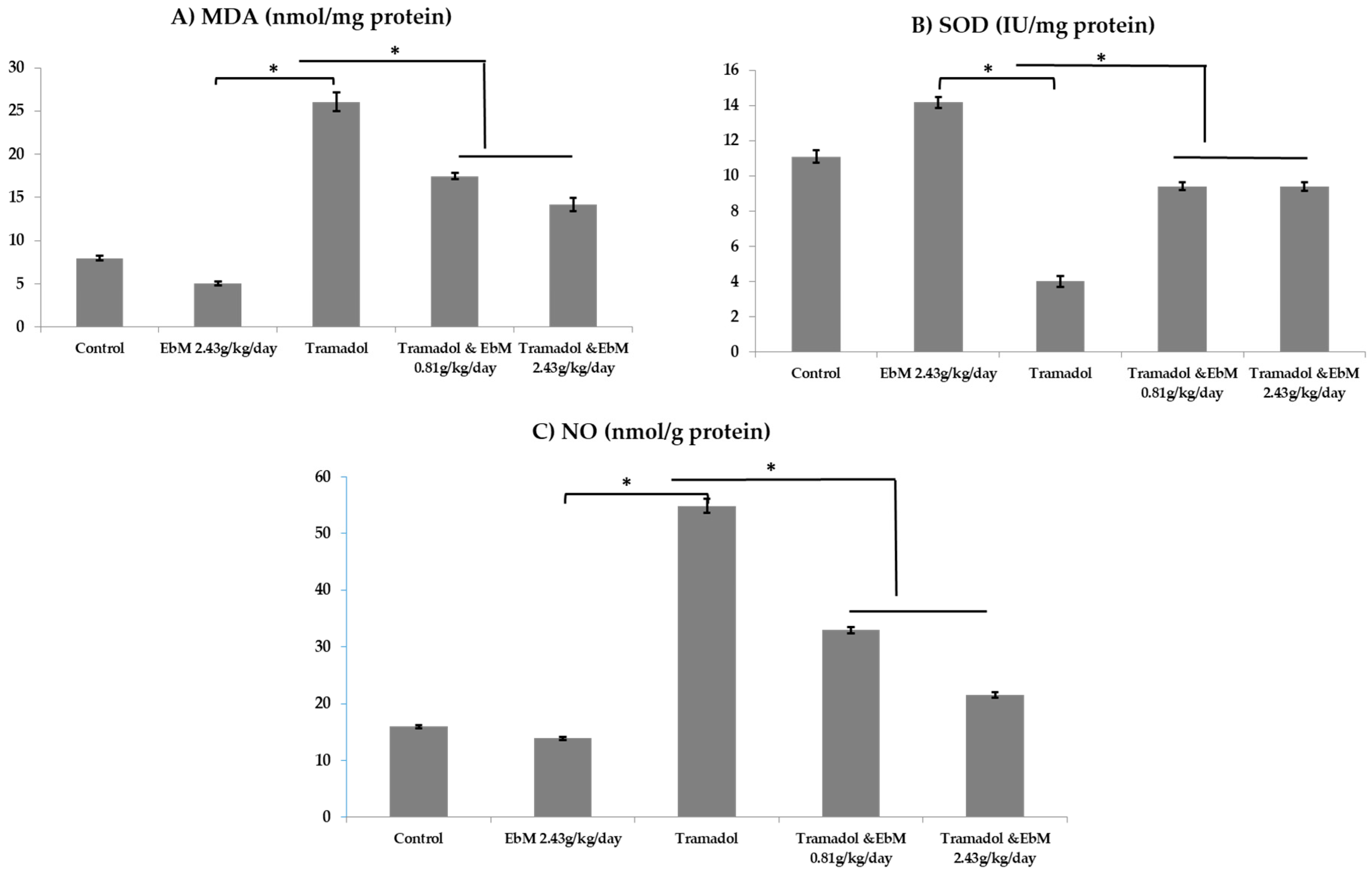
3.3. Effect of E. brevicornum Extract and/or Tramadol Oral Administration on NO and Antioxidant Status
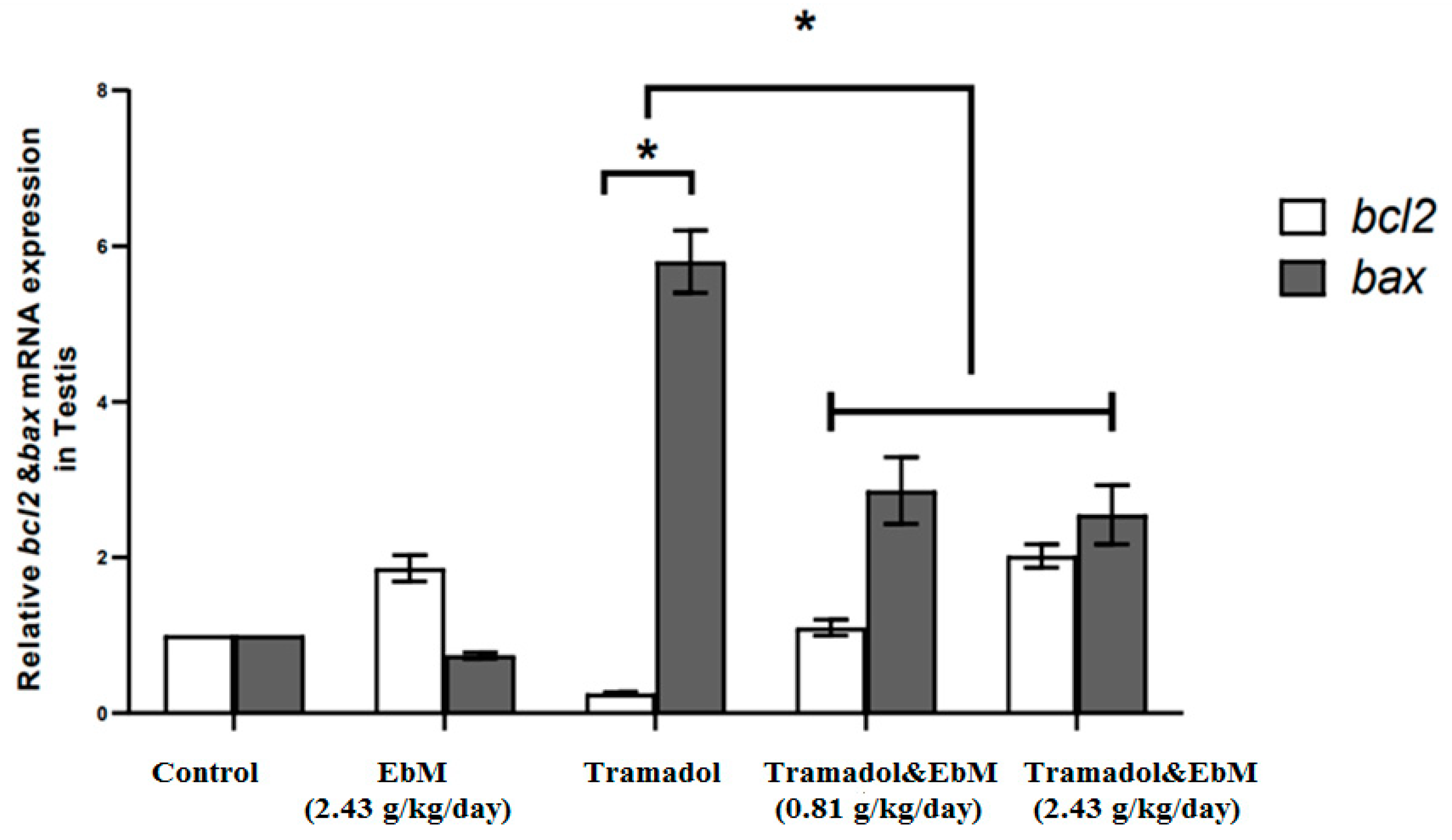
3.4. Expression of Apoptosis-Related Genes in Testicular Tissue
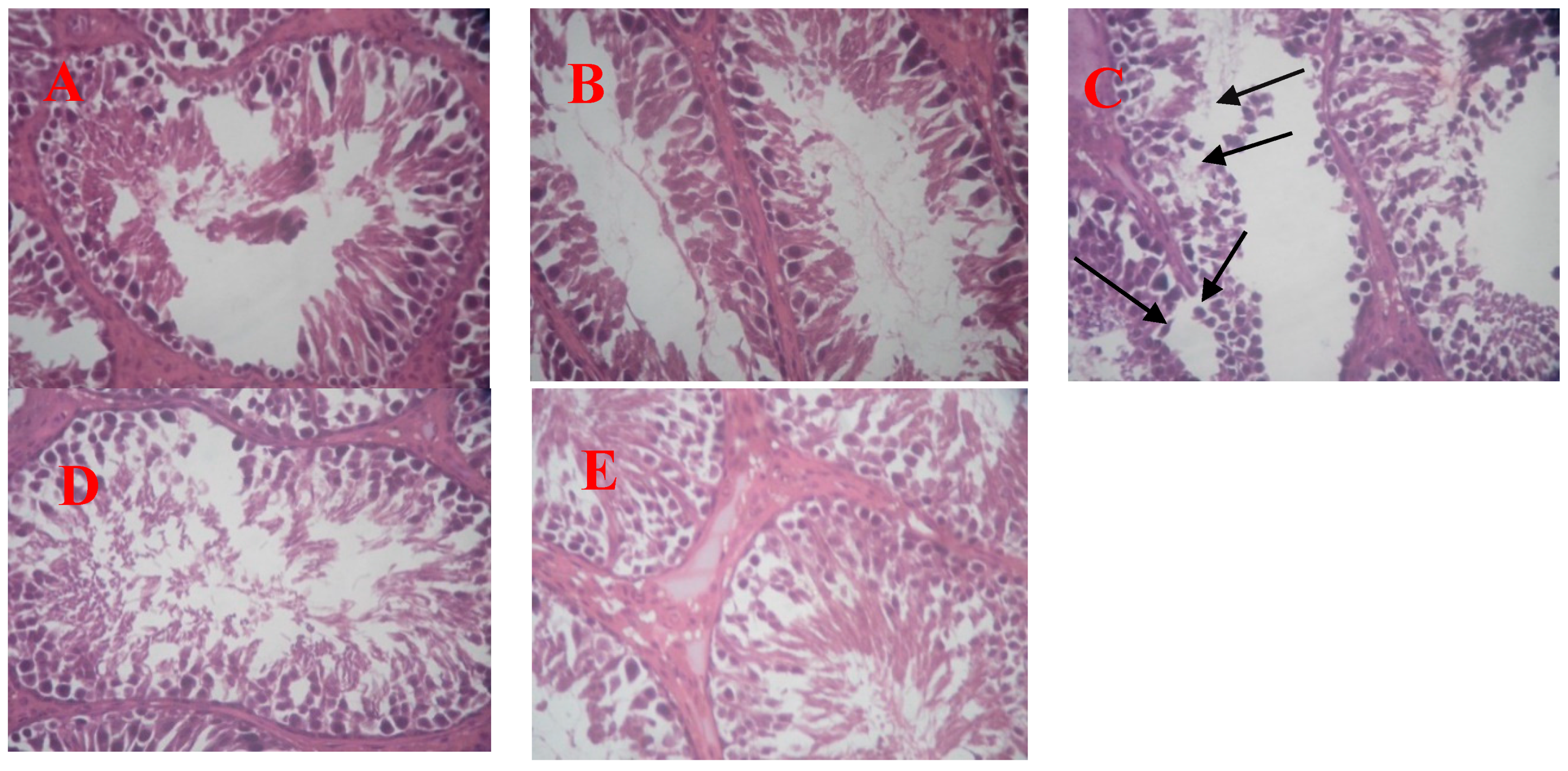
3.5. Effect of Oral E. brevicornum Extract and/or Tramadol Administration on Testicular Histopathology
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- El Fatoh, M.F.A.; Farag, M.R.; Sayed, S.A.; Kamel, M.A.; Abdel-Hamid, N.E.; Hussein, M.A.; Salem, G.A. Some biochemical, neurochemical, pharmacotoxicological and histopathological alterations induced by long-term administration of tramadol in male rats. Int. J. Pharm. Sci. 2014, 4, 2565–2571. [Google Scholar]
- Dayer, P.; Desmeules, J.; Collart, L. Pharmacology of tramadol. Drugs 1997, 53, 18–24. [Google Scholar] [CrossRef]
- Nossaman, V.E.; Ramadhyani, U.; Kadowitz, P.J.; Nossaman, B.D. Advances in perioperative pain management: Use of medications with dual analgesic mechanisms, tramadol & tapentadol. Anaesthesiol. Clin. 2010, 28, 647–666. [Google Scholar]
- Esquivel-Franco, D.C.; Olivier, B.; Waldinger, M.D.; Gutiérrez-Ospina, G.; Olivier, J.D.A. Tramadol’s inhibitory effects on sexual behavior: Pharmacological studies in serotonin transporter knockout rats. Front. Pharmacol. 2018, 9, 676. [Google Scholar] [CrossRef] [PubMed]
- Dhesi, M.; Maani, C.V. Tramadol. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Subedi, M.; Bajaj, S.; Kumar, M.S.; Yc, M. An overview of tramadol and its usage in pain management and future perspective. Biomed. Pharmacother. 2019, 111, 443–451. [Google Scholar] [CrossRef]
- Aea, E.B.; Mm, H. NOS expression in oxidative stress, neurodegeneration and male infertility induced by the abuse of tramadol. Biochem. Pharmacol. 2017, 6. [Google Scholar] [CrossRef]
- Abdel-Hamid, I.A.; Andersson, K.-E.; Waldinger, M.D.; Anis, T.H. Tramadol abuse and sexual function. Sex. Med. Rev. 2016, 4, 235–246. [Google Scholar] [CrossRef]
- Avasthi, A.; Grover, S.; Sathyanarayana Rao, T.S. Clinical practice guidelines for management of sexual dysfunction. Indian J. Psych. 2017, 59, S91–S115. [Google Scholar] [CrossRef]
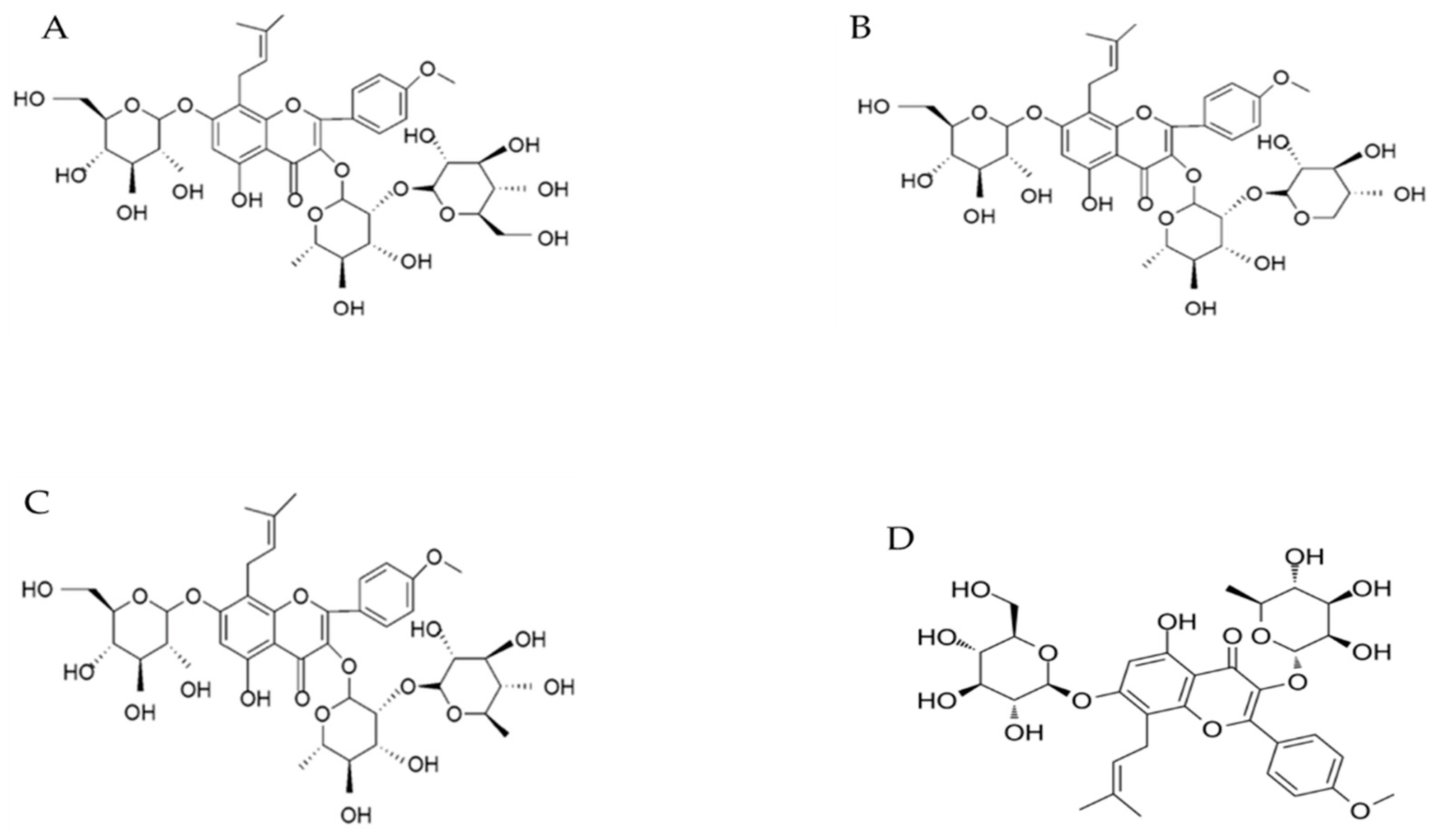
- Ma, H.; He, X.; Yang, Y.; Li, M.; Hao, D.; Jia, Z. The genus Epimedium: An ethnopharmacological and phytochemical review. J. Ethnopharmacol. 2011, 134, 519–541. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-K.; Chiu, J.-H. Effect of Epimedium brevicornum Maxim extract on elicitation of penile erection in the rat. Urology 2006, 67, 631–635. [Google Scholar] [CrossRef]
- Wong, S.P.; Shen, P.; Lee, L.; Li, J.; Yong, E.L. Pharmacokinetics of prenylflavonoids and correlations with the dynamics of estrogen action in sera following ingestion of a standardized Epimedium extract. J. Pharmac. Biomed. Anal. 2009, 50, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Xin, Z.C.; Kim, E.K.; Lin, C.S.; Liu, W.J.; Tian, L.; Yuan, Y.M.; Fu, J. Effects of icariin on cGMP-specific PDE5 and cAMP-specific PDE4 activities. Asian J Androl. 2003, 5, 15–18. [Google Scholar] [PubMed]
- Shindel, A.W.; Xin, Z.-C.; Lin, G.; Fandel, T.M.; Huang, Y.-C.; Banie, L.; Breyer, B.N.; Garcia, M.M.; Lin, C.-S.; Lue, T.F. Erectogenic and neurotrophic effects of icariin, a purified extract of horny goat weed (Epimedium spp.) in vitro and in vivo. J. Sex. Med. 2010, 7, 1518–1528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qureshi, M.; Mehjabeen; Noorjahan; Muhammad, S.; Siddiqui, F.A.; Baig, I.; Ahmad, M. Phytochemical and biological assessments on Lipidium meyenii (maca) and Epimidium sagittatum (horny goat weed). Pak. J. Pharm. Sci. 2017, 30, 29–36. [Google Scholar]
- Batiha, G.E.-S.; Beshbishy, A.M.; Adeyemi, O.S.; Nadwa, E.H.; Rashwan, E.K.M.; Alkazmi, L.M.; Elkelish, A.A.; Igarashi, I. Phytochemical screening and antiprotozoal effects of the methanolic Berberis vulgaris and acetonic Rhus coriaria extracts. Molecules. 2020, 25, 550. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Xiong, Y.; Wang, H.; Yang, L.; Wang, C.; Liu, X.; Wu, Z.; Li, X.; Ou, L.; Zhang, R.; et al. Effects of water extract from epimedium on neuropeptide signaling in an ovariectomized osteoporosis rat model. J. Ethnopharmacol. 2018, 221, 126–136. [Google Scholar] [CrossRef]
- Batiha, G.E.-S.; Beshbishy, A.M.; Guswanto, A.; Nugraha, A.; Munkhjargal, T.; Abdel-Daim, M.M.; Mosqueda, J.; Igarashi, I. Phytochemical characterization and chemotherapeutic potential of Cinnamomum verum extracts on the multiplication of protozoan parasites in vitro and in vivo. Molecules 2020, 25, 996. [Google Scholar] [CrossRef] [Green Version]
- Chance, J.; Berube, J.; Vandersmissen, M.; Blanckaert, N. Evaluation of the BD Vacutainer PST II blood collection tube for special chemistry analytes. Clin. Chem. Lab. Med. 2009, 47, 358–361. [Google Scholar] [CrossRef]
- Robb, G.W.; Amann, R.P.; Killian, G.J. Daily sperm production and epididymal sperm reserves of pubertal and adult rats. J. Reprod. Fertil. 1978, 54, 103–107. [Google Scholar] [CrossRef] [Green Version]
- Chapin, R.E.; Heindel, J.J. Male Reproductive Toxicology, 1st ed.; Elsevier: Amsterdam, The Netherlands, 1993; ISBN 978-1-4832-7095-1. [Google Scholar]
- Green, L.C.; Wagner, D.A.; Glogowski, J.; Skipper, P.L.; Wishnok, J.S.; Tannenbaum, S.R. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal. Biochem. 1982, 126, 131–138. [Google Scholar] [CrossRef]
- Nair, V.; Turner, G.A. The thiobarbituric acid test for lipid peroxidation: Structure of the adduct with malondialdehyde. Lipids 1984, 19, 804–805. [Google Scholar] [CrossRef]
- Sinha, A.K. Colorimetric assay of catalase. Anal. Biochem. 1972, 47, 389–394. [Google Scholar] [CrossRef]
- Misra, H.P.; Fridovich, I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [PubMed]
- Arisha, A.H.; Ahmed, M.M.; Kamel, M.A.; Attia, Y.A.; Hussein, M.M.A. Morin ameliorates the testicular apoptosis, oxidative stress, and impact on blood-testis barrier induced by photo-extracellularly synthesized silver nanoparticles. Environ. Sci. Pollut. Res. Int. 2019, 26, 28749–28762. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Semet, M.; Paci, M.; Saïas-Magnan, J.; Metzler-Guillemain, C.; Boissier, R.; Lejeune, H.; Perrin, J. The impact of drugs on male fertility: A review. Andrology 2017, 5, 640–663. [Google Scholar] [CrossRef]
- Schally, A.V.; Kastin, A.J.; Arimura, A. FSH-releasing hormone and LH-releasing hormone. Vitam. Horm. 1972, 30, 83–164. [Google Scholar]
- Kalra, S.P.; Kalra, P.S. Neural regulation of luteinizing hormone secretion in the rat. Endocr. Rev. 1983, 4, 311–351. [Google Scholar] [CrossRef]
- Oyeyipo, I.P.; Raji, Y.; Bolarinwa, A.F. Nicotine alters male reproductive hormones in male albino rats: The role of cessation. J. Hum. Reprod. Sci. 2013, 6, 40–44. [Google Scholar] [CrossRef]
- Huhtaniemi, I.; Toppari, J. Endocrine, paracrine and autocrine regulation of testicular steroidogenesis. Adv. Exp. Med. Biol. 1995, 377, 33–54. [Google Scholar] [PubMed]
- Hayes, F.J.; DeCruz, S.; Seminara, S.B.; Boepple, P.A.; Crowley, W.F. Differential regulation of gonadotropin secretion by testosterone in the human male: Absence of a negative feedback effect of testosterone on follicle-stimulating hormone secretion. J. Clin. Endocrinol. Metab. 2001, 86, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Carreau, S.; Lambard, S.; Delalande, C.; Denis-Galeraud, I.; Bilinska, B.; Bourguiba, S. Aromatase expression and role of estrogens in male gonad: A review. Reprod. Biol. Endocrinol. 2003, 1, 35. [Google Scholar] [CrossRef]
- Raven, G.; de Jong, F.H.; Kaufman, J.-M.; de Ronde, W. In men, peripheral estradiol levels directly reflect the action of estrogens at the hypothalamo-pituitary level to inhibit gonadotropin secretion. J. Clin. Endocrinol. Metab. 2006, 91, 3324–3328. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.-B.; Yang, Q.-T. The testosterone mimetic properties of icariin. Asian J. Androl. 2006, 8, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Nna, V.U.; Osim, E.E. Testicular toxicity following separate and combined administration of PDE5 inhibitors and opioid: Assessment of recovery following their withdrawal. Andrologia 2017, 49. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Kurkar, A. Effects of opioid (tramadol) treatment on testicular functions in adult male rats: The role of nitric oxide and oxidative stress. Clin. Exp. Pharmacol. Physiol. 2014, 41, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Nantia, E.A.; Moundipa, P.F.; Monsees, T.K.; Carreau, S. Medicinal plants as potential male anti-infertility agents: A review. Basic Clin. Androl. 2009, 19, 148–158. [Google Scholar] [CrossRef] [Green Version]
- Makarova, M.N.; Pozharitskaya, O.N.; Shikov, A.N.; Tesakova, S.V.; Makarov, V.G.; Tikhonov, V.P. Effect of lipid-based suspension of Epimedium koreanum Nakai extract on sexual behavior in rats. J. Ethnopharmacol. 2007, 114, 412–416. [Google Scholar] [CrossRef]
- Farmer, E.E.; Davoine, C. Reactive electrophile species. Curr. Opin. Plant Biol. 2007, 10, 380–386. [Google Scholar] [CrossRef]
- Costa, C.; Rapisarda, V.; Catania, S.; Di Nola, C.; Ledda, C.; Fenga, C. Cytokine patterns in greenhouse workers occupationally exposed to α-cypermethrin: An observational study. Environ. Toxicol. Pharmacol. 2013, 36, 796–800. [Google Scholar] [CrossRef]
- El-Gaafarawi, I.I. Biochemical toxicity induced by tramadol administration in male rats. Egypt. J. Hosp. Med. 2006, 23, 353–362. [Google Scholar]
- Povsic, T.J.; Zavodni, K.L.; Vainorius, E.; Kherani, J.F.; Goldschmidt-Clermont, P.J.; Peterson, E.D. Common endothelial progenitor cell assays identify discrete endothelial progenitor cell populations. Amer. Heart J. 2009, 157, 335–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atici, S.; Cinel, I.; Cinel, L.; Doruk, N.; Eskandari, G.; Oral, U. Liver and kidney toxicity in chronic use of opioids: An experimental long term treatment model. J. Biosci. 2005, 30, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Hou, Y.; Tang, G.; Cai, E.; Liu, S.; Yang, H.; Zhang, L.; Wang, S. Optimization of ultrasonic extraction of phenolic compounds from Epimedium brevicornum maxim using response surface methodology and evaluation of its antioxidant activities in vitro. J. Anal. Methods Chem. 2014, 2014, 864654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.-D.; Hou, J.-G.; Yang, G.; Jiang, S.; Chen, C.; Wang, Z.; Liu, Y.-Y.; Ren, S.; Li, W. Icariin ameliorates cisplatin-induced cytotoxicity in human embryonic kidney 293 cells by suppressing ROS-mediated PI3K/Akt pathway. Biomed. Pharmacother. 2019, 109, 2309–2317. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C.F.; Hibbs, J.B. Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr. Opin. Immunol. 1991, 3, 65–70. [Google Scholar] [CrossRef]
- Ch, E. Nitric oxide: What role does it play in inflammation and tissue destruction? Agents Actions Suppl. 1995, 47, 107–116. [Google Scholar]
- Yuk, S.-S.; Lim, E.-M.; Lee, J.Y.; Lee, Y.-J.; Kim, Y.-S.; Lee, T.H.; Park, S.K.; Bae, H.; Kim, H.M.; Ko, S.-G.; et al. Antiinflammatory effects of Epimedium brevicornum water extract on lipopolysaccharide-activated RAW264.7 macrophages. Phytother. Res. 2010, 24, 1781–1787. [Google Scholar] [CrossRef]
- Elnaga, A.A.A.; Kassab, A.A.; Soliman, G.M.; Shal, A.O.E. Histological and immunohistochemical study of the effect of tramadol on the seminiferous tubules of adult albino rat and the effect of its withdrawal. Tanta Med. J. 2018, 46, 38. [Google Scholar] [CrossRef]
- Ghoneim, F.M.; Khalaf, H.A.; Elsamanoudy, A.Z.; Helaly, A.N. Effect of chronic usage of tramadol on motor cerebral cortex and testicular tissues of adult male albino rats and the effect of its withdrawal: Histological, immunohistochemical and biochemical study. Int. J. Clin. Exp. Pathol. 2014, 7, 7323–7341. [Google Scholar]
| Gene | Forward Primer (5′–3′) | Reverse Primer (5′–3′) | Accession No | Product Size | Ref. |
|---|---|---|---|---|---|
| Bax | CGAATTGGCGATGAACTGGA | CAAACATGTCAGCTGCCACAC | NM_017059.2 | 109 | [25] |
| Bcl2 | GACTGAGTACCTGAACCGGCATC | CTGAGCAGCGTCTTCAGAGACA | NM_016993.1 | 135 | [25] |
| GAPDH | GGCACAGTCAAGGCTGAGAATG | ATGGTGGTGAAGACGCCAGTA | NM_017008.4 | 143 | [25] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelaziz, A.S.; Kamel, M.A.; Ahmed, A.I.; Shalaby, S.I.; El-darier, S.M.; Magdy Beshbishy, A.; Batiha, G.E.-S.; Alomar, S.Y.; Khodeer, D.M. Chemotherapeutic Potential of Epimedium brevicornum Extract: The cGMP-Specific PDE5 Inhibitor as Anti-Infertility Agent Following Long-Term Administration of Tramadol in Male Rats. Antibiotics 2020, 9, 318. https://doi.org/10.3390/antibiotics9060318
Abdelaziz AS, Kamel MA, Ahmed AI, Shalaby SI, El-darier SM, Magdy Beshbishy A, Batiha GE-S, Alomar SY, Khodeer DM. Chemotherapeutic Potential of Epimedium brevicornum Extract: The cGMP-Specific PDE5 Inhibitor as Anti-Infertility Agent Following Long-Term Administration of Tramadol in Male Rats. Antibiotics. 2020; 9(6):318. https://doi.org/10.3390/antibiotics9060318
Chicago/Turabian StyleAbdelaziz, Ahmed S., Mohamed A. Kamel, Amany I. Ahmed, Shimaa I. Shalaby, Salama M. El-darier, Amany Magdy Beshbishy, Gaber El-Saber Batiha, Suliman Y. Alomar, and Dina M. Khodeer. 2020. "Chemotherapeutic Potential of Epimedium brevicornum Extract: The cGMP-Specific PDE5 Inhibitor as Anti-Infertility Agent Following Long-Term Administration of Tramadol in Male Rats" Antibiotics 9, no. 6: 318. https://doi.org/10.3390/antibiotics9060318