The Organization of Primary Healthcare during the COVID-19 Pandemic
A project collection of International Journal of Environmental Research and Public Health (ISSN 1660-4601).
Papers displayed on this page all arise from the same project. Editorial decisions were made independently of project staff and handled by the Editor-in-Chief or qualified Editorial Board members.
Submission Status:
Closed
|
Viewed by 30907
Share This Project Collection
Editors
 Prof. Dr. Sara Willems
Prof. Dr. Sara Willems
 Prof. Dr. Sara Willems
Prof. Dr. Sara Willems
E-Mail
Website
Guest Editor
Department of Public Health and Primary Care, Ghent University, 9000 Gent, Belgium
Interests: primary health care; primary care; social capital, communication; population, quality; self-rated health
 Dr. Andrew D. Pinto
Dr. Andrew D. Pinto
 Dr. Andrew D. Pinto
Dr. Andrew D. Pinto
E-Mail
Website
Guest Editor
Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON M5G 1V7, Canada
Interests: evaluations of interventions that address the social determinants of health, at the individual-, community-, organization- and population-level; applying a population health perspective to health services, including through the application of new tools to “big data” to support health sector transformation
Project Overview
Dear Colleagues,
General practitioners play a crucial role in the fight against the COVID-19 pandemic as the first point of contact for possibly infected patients and are responsible for the short- and long-term follow-up care of the majority of COVID patients. Nonetheless, they experience many barriers to fulfilling this role. The PRICOV-19 study investigates how GP practices in 38 countries are organized during COVID-19 to guarantee high-quality care. Additionally, the shift in roles and tasks and the wellbeing of staff members is researched. Finally, PRICOV-19 aims to study the association with practice and healthcare system characteristics. This Special Issue will comprise a collection of articles on the results of PRICOV-19, which is the largest study ever carried out in Europe and the most comprehensive study examining how GP practices function during COVID-19. Its results can significantly contribute to better preparedness of primary healthcare (PHC) systems across Europe for future major outbreaks of infectious diseases. Potential topics include but are not limited to the wellbeing of care providers, division of tasks and roles, limitations to the infrastructure or buildings, infection control, patient safety incidents, video consultations, health inequities and care for vulnerable population groups, patient education responsiveness, and healthcare system pandemic response and PHC organization.
Prof. Dr. Sara Willems
Dr. Andrew D. Pinto
Guest Editors
Publisher’s Notice
As stated above, the central purpose of this Special Issue is to present research from PRICOV-19 . Given this purpose, the Guest Editors’ contribution to this Special Issue may be greater than outlined in MDPI’s Special Issue guidelines (https://www.mdpi.com/special_issues_guidelines). The Editorial Office and Editor-in-Chief of IJERPH has approved this Topic and MDPI’s standard manuscript editorial processing procedure (https://www.mdpi.com/editorial_process) will be applied to all submissions. As per our standard procedure, Guest Editors are excluded from participating in the editorial process for their submission and/or for submissions from persons with whom a potential conflict of interest may exist. More details on MDPI’s Conflict of Interest policy for reviewers and editors can be found here: https://www.mdpi.com/ethics#_bookmark22.
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. International Journal of Environmental Research and Public Health is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2500 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- primary healthcare
- general practice
- quality of care
- patient safety
- equity
- psychosocial
- infectious diseases
- multicountry COVID-19
- PRICOV-19
Published Papers (8 papers)
Open AccessArticle
Differences between Rural and Urban Practices in the Response to the COVID-19 Pandemic: Outcomes from the PRICOV-19 Study in 38 Countries
by
Ferdinando Petrazzuoli, Claire Collins, Esther Van Poel, Athina Tatsioni, Sven Streit, Gazmend Bojaj, Radost Asenova, Kathryn Hoffmann, Jonila Gabrani, Zalika Klemenc-Ketis, Andrée Rochfort, Limor Adler, Adam Windak, Katarzyna Nessler and Sara Willems
Cited by 10 | Viewed by 4652
Abstract
This paper explores the differences between rural and urban practices in the response to the COVID-19 pandemic, emphasizing aspects such as management of patient flow, infection prevention and control, information processing, communication and collaboration. Using a cross-sectional design, data were collected through the
[...] Read more.
This paper explores the differences between rural and urban practices in the response to the COVID-19 pandemic, emphasizing aspects such as management of patient flow, infection prevention and control, information processing, communication and collaboration. Using a cross-sectional design, data were collected through the online PRICOV-19 questionnaire sent to general practices in 38 countries. Rural practices in our sample were smaller than urban-based practices. They reported an above-average number of old and multimorbid patients and a below-average number of patients with a migrant background or financial problems. Rural practices were less likely to provide leaflets and information, but were more likely to have ceased using the waiting room or to have made structural changes to their waiting room and to have changed their prescribing practices in terms of patients attending the practices. They were less likely to perform video consultations or use electronic prescription methods. Our findings show the existence of certain issues that could impact patient safety in rural areas more than in urban areas due to the underlying differences in population profile and supports. These could be used to plan the organization of care for similar future pandemic situations.
Full article
►▼
Show Figures
Open AccessArticle
Screening for and Disclosure of Domestic Violence during the COVID-19 Pandemic: Results of the PRICOV-19 Cross-Sectional Study in 33 Countries
by
Elizaveta Fomenko, Ines Keygnaert, Esther Van Poel, Claire Collins, Raquel Gómez Bravo, Päivi Korhonen, Merja K. Laine, Liubove Murauskiene, Athina Tatsioni and Sara Willems
Cited by 3 | Viewed by 2717
Abstract
The COVID-19 pandemic left no one untouched, and reports of domestic violence (DV) increased during the crisis. DV victims rarely seek professional help, yet when they do so, they often disclose it to their general practitioner (GP), with whom they have a trusting
[...] Read more.
The COVID-19 pandemic left no one untouched, and reports of domestic violence (DV) increased during the crisis. DV victims rarely seek professional help, yet when they do so, they often disclose it to their general practitioner (GP), with whom they have a trusting relationship. GPs rarely screen and hence rarely take the initiative to discuss DV with patients, although victims indicate that offering this opportunity would facilitate their disclosure. This paper aims to describe the frequency of screening for DV by GPs and disclosure of DV by patients to the GP during the COVID-19 pandemic, and to identify key elements that could potentially explain differences in screening for and disclosure of DV. The PRICOV-19 data of 4295 GP practices from 33 countries were included in the analyses, with practices nested in countries. Two stepwise forward clustered ordinal logistic regressions were performed. Only 11% of the GPs reported (much) more disclosure of DV by patients during COVID-19, and 12% reported having screened for DV (much). Most significant associations with screening for and disclosure of DV concerned general (pro)active communication. However, (pro)active communication was performed less frequently for DV than for health conditions, which might indicate that GPs are insufficiently aware of the general magnitude of DV and its impact on patients and society, and its approach/management. Thus, professional education and training for GPs about DV seems highly and urgently needed.
Full article
►▼
Show Figures
Open AccessArticle
The Organization of Outreach Work for Vulnerable Patients in General Practice during COVID-19: Results from the Cross-Sectional PRICOV-19 Study in 38 Countries
by
Esther Van Poel, Claire Collins, Peter Groenewegen, Peter Spreeuwenberg, Gazmend Bojaj, Jonila Gabrani, Christian Mallen, Liubove Murauskiene, Milena Šantrić Milićević, Emmily Schaubroeck, Stefanie Stark and Sara Willems
Cited by 9 | Viewed by 4150
Abstract
The COVID-19 pandemic disproportionately affected vulnerable populations’ access to health care. By proactively reaching out to them, general practices attempted to prevent the underutilization of their services. This paper examined the association between practice and country characteristics and the organization of outreach work
[...] Read more.
The COVID-19 pandemic disproportionately affected vulnerable populations’ access to health care. By proactively reaching out to them, general practices attempted to prevent the underutilization of their services. This paper examined the association between practice and country characteristics and the organization of outreach work in general practices during COVID-19. Linear mixed model analyses with practices nested in countries were performed on the data of 4982 practices from 38 countries. A 4-item scale on outreach work was constructed as the outcome variable with a reliability of 0.77 and 0.97 at the practice and country level. The results showed that many practices set up outreach work, including extracting at least one list of patients with chronic conditions from their electronic medical record (30.1%); and performing telephone outreach to patients with chronic conditions (62.8%), a psychological vulnerability (35.6%), or possible situation of domestic violence or a child-rearing situation (17.2%). Outreach work was positively related to the availability of an administrative assistant or practice manager (
p < 0.05) or paramedical support staff (
p < 0.01). Other practice and country characteristics were not significantly associated with undertaking outreach work. Policy and financial interventions supporting general practices to organize outreach work should focus on the range of personnel available to support such practice activities.
Full article
►▼
Show Figures
Open AccessArticle
Responding to COVID-19: The Suitability of Primary Care Infrastructure in 33 Countries
by
Adam Windak, Katarzyna Nessler, Esther Van Poel, Claire Collins, Ewa Wójtowicz, Liubove Murauskiene, Kathryn Hoffmann and Sara Willems
Cited by 13 | Viewed by 2672
Abstract
COVID-19 proved that primary care (PC) providers have an important role in managing health emergencies, such as epidemics. Little is known about the preparedness of primary care practice infrastructure to continue providing high quality care during this crisis. The aim of this paper
[...] Read more.
COVID-19 proved that primary care (PC) providers have an important role in managing health emergencies, such as epidemics. Little is known about the preparedness of primary care practice infrastructure to continue providing high quality care during this crisis. The aim of this paper is to describe the perceived limitations to the infrastructure of PC practices during COVID-19 and to determine the factors associated with a higher likelihood of infrastructural barriers in providing high quality care. This paper presents the results of an online survey conducted between November 2020 and November 2021 as a part of PRICOV-19 study. Data from 4974 practices in 33 countries regarding perceived limitations and intentions to make future adjustments to practice infrastructure as a result of the COVID-19 pandemic were collected. Approximately 58% of practices experienced limitations to the building or other practice infrastructure to provide high-quality and safe care during the COVID-19 pandemic, and in 54% making adjustments to the building or the infrastructure was considered. Large variations between the countries were found. The results show that infrastructure constraints were directly proportional to the size of the practice. Better pandemic infection control equipment, governmental support, and a fee-for-service payment system were found to be associated with a lower perceived need for infrastructural changes. The results of the study indicate the need for systematic support for the development of practice infrastructure in order to provide high-quality, safe primary care in the event of future crises similar to the COVID-19 pandemic.
Full article
►▼
Show Figures
Open AccessArticle
Has the COVID-19 Pandemic Led to Changes in the Tasks of the Primary Care Workforce? An International Survey among General Practices in 38 Countries (PRICOV-19)
by
Peter Groenewegen, Esther Van Poel, Peter Spreeuwenberg, Ronald Batenburg, Christian Mallen, Liubove Murauskiene, Antoni Peris, Benoit Pétré, Emmily Schaubroeck, Stefanie Stark, Emil L. Sigurdsson, Athina Tatsioni, Kyriaki Vafeidou and Sara Willems
Cited by 29 | Viewed by 3266
Abstract
The COVID-19 pandemic has had a large and varying impact on primary care. This paper studies changes in the tasks of general practitioners (GPs) and associated staff during the COVID-19 pandemic. Data from the PRICOV-19 study of 5093 GPs in 38 countries were
[...] Read more.
The COVID-19 pandemic has had a large and varying impact on primary care. This paper studies changes in the tasks of general practitioners (GPs) and associated staff during the COVID-19 pandemic. Data from the PRICOV-19 study of 5093 GPs in 38 countries were used. We constructed a scale for task changes and performed multilevel analyses. The scale was reliable at both GP and country level. Clustering of task changes at country level was considerable (25%). During the pandemic, staff members were more involved in giving information and recommendations to patients contacting the practice by phone, and they were more involved in triage. GPs took on additional responsibilities and were more involved in reaching out to patients. Problems due to staff absence, when dealt with internally, were related to more task changes. Task changes were larger in practices employing a wider range of professional groups. Whilst GPs were happy with the task changes in practices with more changes, they also felt the need for further training. A higher-than-average proportion of elderly people and people with a chronic condition in the practice were related to task changes. The number of infections in a country during the first wave of the pandemic was related to task changes. Other characteristics at country level were not associated with task changes. Future research on the sustainability of task changes after the pandemic is needed.
Full article
Open AccessArticle
Safety Culture and the Positive Association of Being a Primary Care Training Practice during COVID-19: The Results of the Multi-Country European PRICOV-19 Study
by
Bianca Silva, Zlata Ožvačić Adžić, Pierre Vanden Bussche, Esther Van Poel, Bohumil Seifert, Cindy Heaster, Claire Collins, Canan Tuz Yilmaz, Felicity Knights, Maria de la Cruz Gomez Pellin, Maria Pilar Astier Peña, Neophytos Stylianou, Raquel Gomez Bravo, Venija Cerovečki, Zalika Klemenc Ketis and Sara Willems
Cited by 7 | Viewed by 3344
Abstract
The day-to-day work of primary care (PC) was substantially changed by the COVID-19 pandemic. Teaching practices needed to adapt both clinical work and teaching in a way that enabled the teaching process to continue, while maintaining safe and high-quality care. Our study aims
[...] Read more.
The day-to-day work of primary care (PC) was substantially changed by the COVID-19 pandemic. Teaching practices needed to adapt both clinical work and teaching in a way that enabled the teaching process to continue, while maintaining safe and high-quality care. Our study aims to investigate the effect of being a training practice on a number of different outcomes related to the safety culture of PC practices. PRICOV-19 is a multi-country cross-sectional study that researches how PC practices were organized in 38 countries during the pandemic. Data was collected from November 2020 to December 2021. We categorized practices into training and non-training and selected outcomes relating to safety culture: safe practice management, community outreach, professional well-being and adherence to protocols. Mixed-effects regression models were built to analyze the effect of being a training practice for each of the outcomes, while controlling for relevant confounders. Of the participating practices, 2886 (56%) were non-training practices and 2272 (44%) were training practices. Being a training practice was significantly associated with a lower risk for adverse mental health events (OR: 0.83; CI: 0.70–0.99), a higher number of safety measures related to patient flow (Beta: 0.17; CI: 0.07–0.28), a higher number of safety incidents reported (RR: 1.12; CI: 1.06–1.19) and more protected time for meetings (Beta: 0.08; CI: 0.01–0.15). No significant associations were found for outreach initiatives, availability of triage information, use of a phone protocol or infection prevention measures and equipment availability. Training practices were found to have a stronger safety culture than non-training practices. These results have important policy implications, since involving more PC practices in education may be an effective way to improve quality and safety in general practice.
Full article
Open AccessArticle
Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey
by
Claire Collins, Esther Van Poel, Milena Šantrić Milićević, Katica Tripkovic, Limor Adler, Torunn Bjerve Eide, Liubove Murauskiene, Adam Windak, Katarzyna Nessler, Bernard Tahirbegolli and Sara Willems
Cited by 22 | Viewed by 4578
Abstract
Infection prevention and control (IPC) is an evidence-based approach used to reduce the risk of infection transmission within the healthcare environment. Effective IPC practices ensure safe and quality healthcare. The COVID-19 pandemic highlighted the need for enhanced IPC measures and the World Health
[...] Read more.
Infection prevention and control (IPC) is an evidence-based approach used to reduce the risk of infection transmission within the healthcare environment. Effective IPC practices ensure safe and quality healthcare. The COVID-19 pandemic highlighted the need for enhanced IPC measures and the World Health Organization (WHO) emphasized the need for strict adherence to the basic principles of IPC. This paper aims to describe the IPC strategies implemented in general practice during the COVID-19 pandemic and to identify the factors that impact their adoption. Data were collected by means of an online self-reported questionnaire among general practices. Data from 4466 practices in 33 countries were included in the analysis. Our results showed a notable improvement in IPC during COVID-19 with more practices reporting that staff members never wore nail polish (increased from 34% to 46.2%); more practices reporting that staff never wear a ring/bracelet (increased from 16.1% to 32.3%); and more practices using a cleaning protocol (increased from 54.9% to 72.7%). Practice population size and the practice payment system were key factors related to adoption of a) range of IPC measures including patient flow arrangements and infrastructural elements. An understanding of the interplay between policy, culture, systemic supports, and behavior are necessary to obtain sustained improvement in IPC measures.
Full article
►▼
Show Figures
Open AccessArticle
Distress and Wellbeing among General Practitioners in 33 Countries during COVID-19: Results from the Cross-Sectional PRICOV-19 Study to Inform Health System Interventions
by
Claire Collins, Els Clays, Esther Van Poel, Joanna Cholewa, Katica Tripkovic, Katarzyna Nessler, Ségolène de Rouffignac, Milena Šantrić Milićević, Zoran Bukumiric, Limor Adler, Cécile Ponsar, Liubove Murauskiene, Zlata Ožvačić Adžić, Adam Windak, Radost Asenova and Sara Willems
Cited by 30 | Viewed by 3922
Abstract
Emerging literature is highlighting the huge toll of the COVID-19 pandemic on frontline health workers. However, prior to the crisis, the wellbeing of this group was already of concern. The aim of this paper is to describe the frequency of distress and wellbeing,
[...] Read more.
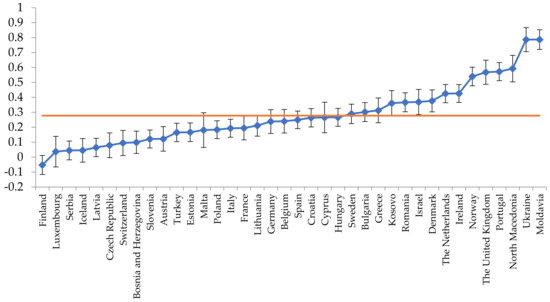
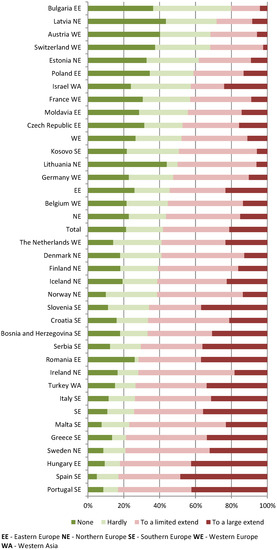
Emerging literature is highlighting the huge toll of the COVID-19 pandemic on frontline health workers. However, prior to the crisis, the wellbeing of this group was already of concern. The aim of this paper is to describe the frequency of distress and wellbeing, measured by the expanded 9-item Mayo Clinic Wellbeing Index (eWBI), among general practitioners/family physicians during the COVID-19 pandemic and to identify levers to mitigate the risk of distress. Data were collected by means of an online self-reported questionnaire among GP practices. Statistical analysis was performed using SPSS software using Version 7 of the database, which consisted of the cleaned data of 33 countries available as of 3 November 2021. Data from 3711 respondents were included. eWBI scores ranged from −2 to 9, with a median of 3. Using a cutoff of ≥2, 64.5% of respondents were considered at risk of distress. GPs with less experience, in smaller practices, and with more vulnerable patient populations were at a higher risk of distress. Significant differences in wellbeing scores were noted between countries. Collaboration from other practices and perception of having adequate governmental support were significant protective factors for distress. It is necessary to address practice- and system-level organizational factors in order to enhance wellbeing and support primary care physicians.
Full article
►▼
Show Figures