Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sampling and Recruitment
2.3. Data Management and Analysis
2.4. Ethical Approval
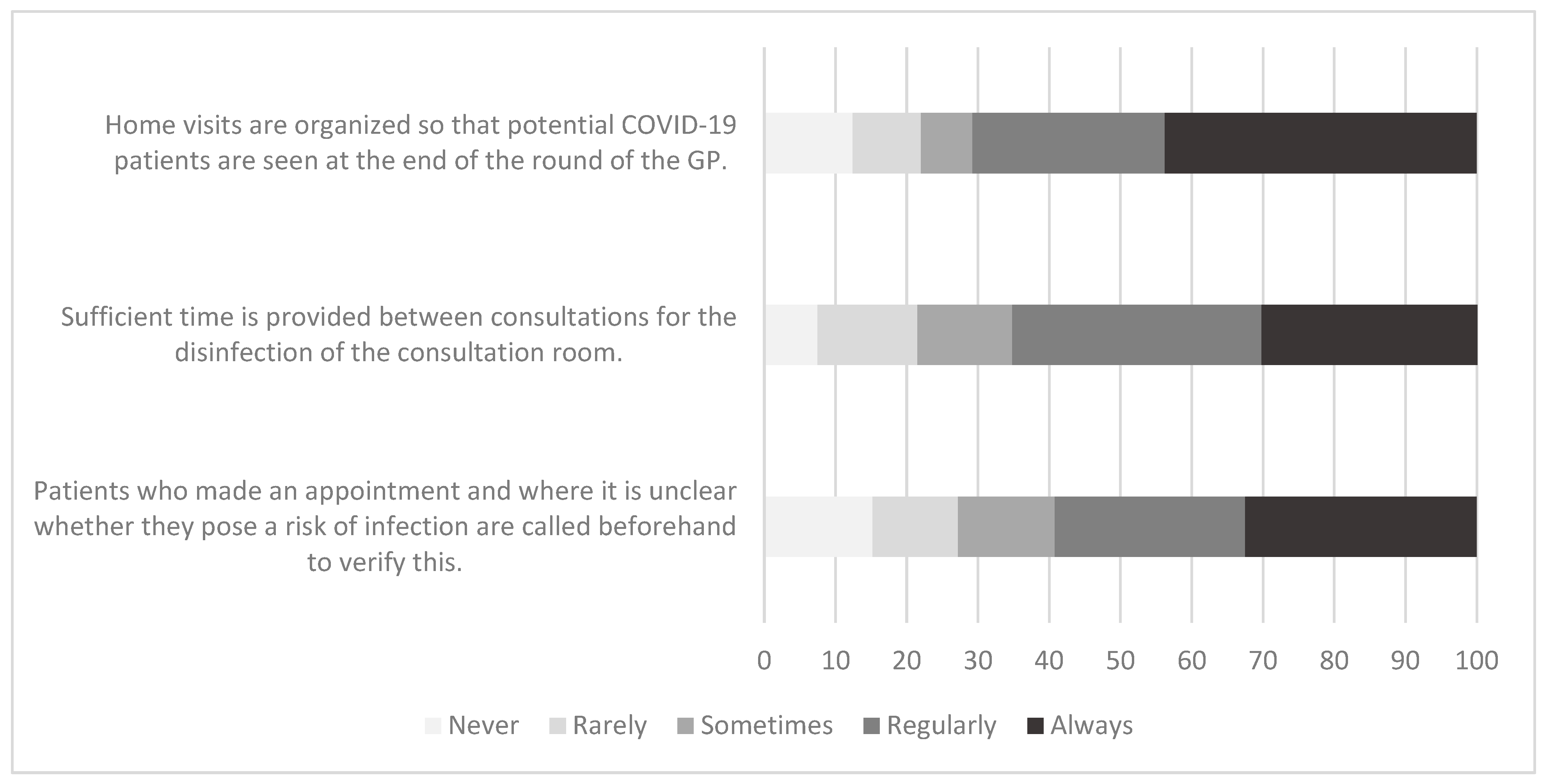
3. Results
4. Discussion
The Limitations and Strengths of the PRICOV-19 Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kearon, J.; Risdon, C. The role of primary care in a pandemic: Reflections during the COVID-19 pandemic in Canada. J. Prim. Care Community Health 2020, 11, 2150132720962871. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Infection Prevention and Control. Available online: https://www.who.int/health-topics/infection-prevention-and-control#tab=tab_1 (accessed on 11 April 2022).
- Patel, L.N.; Kozikott, S.; Ilboudo, R.; Kamateeka, M.; Lamorde, M.; Subah, M.; Tsiouris, F.; Vorndran, A.; Lee, C.L.; African Primary Health Care IPC Strengthening Community of Practice. Safer primary healthcare facilities are needed to protect healthcare workers and maintain essential services: Lessons learned from a multicountry COVID-19 emergency response initiative. BMJ Global Health 2021, 6, e005833. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/handle/10665/112656 (accessed on 19 June 2022).
- Broussard, I.M.; Kahwaji, C.I. Universal Precautions. StatPearls Publishing, StatPearls [Internet]. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470223/ (accessed on 19 June 2022).
- World Health Organization. Infection Prevention and Control during Health Care When Coronavirus Disease (COVID-19) Is Suspected or Confirmed. Interim Guidance 12 July 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2021.1 (accessed on 11 April 2022).
- Lim, J.; Broughan, J.; Crowley, D.; O’Kelly, B.; Fawsitt, R.; Burke, M.C.; McOmbe, G.; Lambert, J.S.; Cullen, W. COVID-19’s impact on primary care and related mitigation strategies: A scoping review. Eur. J. Gen. Pract. 2021, 27, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Mouallem, R.E.; Moussally, K.; Williams, A.; Repetto, E.; Menassa, M.; Martino, C.; Sittah, G.A. How COVID-19 highlighted the need for infection prevention and control measures to become central to the global conversation: Experience from the conflict settings of the Middle East. Int. J. Infect. Dis. 2021, 111, 55–57. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Rahman, K.M.; Sun, Y.; Qureshi, M.O.; Abdi, I.; Chughtai, A.A.; Seale, H. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: A global analysis. Infect. Control Hosp. Epidemiol. 2020, 41, 1196–1206. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.; Tan, D.H.; Wong, G.J.; Lew, Y.; Chua, Y.; Low, L.; Ho, H.; Kwek, T.; Toh, S.E.; Tan, K. Prepared and highly committed despite the risk of COVID-19 infection: A cross-sectional survey of primary care physicians’ concerns and coping strategies in Singapore. BMC Fam. Pract. 2021, 22, 22. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Weiner-Lastinger, L.; Pattabiraman, V.; Konnor, R.; Patel, P.; Wong, E.; Xu, S.; Smith, B.; Edwards, J.R.; Dudeck, M.A. The impact of coronavirus disease 2019 (COVID-19) on healthcare-associated infections in 2020: A summary of data reported to the National Healthcare Safety Network. Infect. Control. Hosp. Epidemiol. 2022, 43, 12–25. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; United Nations Children’s Fund. Community-Based Health Care, Including Outreach and Campaigns, in the Context of the Covid-19 Pandemic: Interim Guidance; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/331975 (accessed on 11 April 2022).
- World Health Organization. Minimum Requirements for Infection Prevention and Control Programmes; World Health Organization: Geneva, Switzerland, 2019; Available online: https://apps.who.int/iris/handle/10665/330080 (accessed on 11 April 2022).
- World Health Organization. Strengthening Infection Prevention and Control in Primary Care: A Collection of Existing Standards, Measurement and Implementation Resources; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240035249 (accessed on 11 April 2022).
- Lai, X.; Wang, X.; Yang, Q.; Xu, X.; Tang, Y.; Liu, C.; Tan, L.; Lai, R.; Wang, H.; Zhang, X.; et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob. Resist. Infect. Control 2020, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Resource Considerations for Investing in Hand Hygiene Improvement in Health Care Facilities; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- World Health Organization. Hand Hygiene. Technical Reference Manual; World Health Organization: Geneva, Switzerland, 2009; ISBN 9789241598606. Available online: http://apps.who.int/iris/bitstream/handle/10665/44196/9789241598606_eng.pdf?sequence=1 (accessed on 11 April 2022).
- Van Poel, E.; Vanden Bussche, P.; Klemenc-Ketis, Z.; Willems, S. How did general practices organize care during the COVID-19 pandemic: The protocol of the cross-sectional PRICOV-19 study in 38 countries. BMC Fam. Pract. 2022, 23, 11. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, J.; Qiao, F.; Feng, B.; Hu, F.; Xi, Z.; Wu, W.; Ni, Z.; Liu, L.; Yuan, Y. Compared hand hygiene compliance among healthcare providers before and after the COVID-19 pandemic: A rapid review and meta-analysis. Am. J. Infect. Control 2022, 50, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Takamatsu, A.; Saito, H.; Okamoto, K. Changes in infection control practice for coronavirus disease 2019 (COVID-19) between 2020 and 2021: A nationwide questionnaire survey in Japan. Antimicrob. Steward. Healthc. Epidemiol. 2021, 1, e12. [Google Scholar] [CrossRef]
- Jeong, G.; Lee, T.R.; Hwang, S.Y.; Cha, W.C.; Shin, T.G.; Sim, M.S.; Jo, I.J.; Song, K.J.; Rhee, J.E.; Jeong, Y.K. Emergency department workers’ perceptions of effectiveness and reported compliance of infection control measures after Middle East respiratory syndrome outbreaks. J. Korean Soc. Emerg. Med. 2016, 27, 328–335. [Google Scholar]
- Loh, L.C.; Chelliah, A.; Ang, T.H.; Ali, A.M. Change in infection control practices and awareness of hospital medical staff in the aftermath of SARS. Med. J. Malays. 2004, 59, 659–664. [Google Scholar] [CrossRef]
- Brooks, S.K.; Greenberg, N.; Wessely, S.; Rubin, G.J. Factors affecting healthcare workers’ compliance with social and behavioural infection control measures during emerging infectious disease outbreaks: Rapid evidence review. BMJ Open 2021, 11, e049857. [Google Scholar] [CrossRef] [PubMed]
- Houghton, C.; Meskell, P.; Delaney, H.; Smalle, M.; Glenton, C.; Booth, A.; Chan, X.H.I.; Devance, D.; Biesty, L.M.l. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020, 4, CD013582. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.; Castro-Sanchez, E.; Charani, E.; Drumright, L.N.; Holmes, A.H. Towards changing healthcare workers’ behaviour: A qualitative study exploring non-compliance through appraisals of infection prevention and control practices. J. Hosp. Infect. 2015, 90, 126–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desborough, J.; Dykgraaf, S.H.; Phillips, C.; Wright, M.; Maddox, R.; Davis, S.; Kidd, M. Lessons for the global primary care response to COVID-19: A rapid review of evidence from past epidemics. Fam. Pract. 2021, 38, 811–825. [Google Scholar] [CrossRef] [PubMed]
- Makhni, S.; Umscheid, C.A.; Soo, J.; Chu, V.; Bartlett, A.; Landon, E.; Marrs, R. Hand hygiene compliance rate during the COVID-19 pandemic. JAMA Intern. Med. 2021, 181, 1006–1008. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.D.; Robbins, G.; Quinn, J.; Arbogast, J.W. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am. J. Infect. Control 2021, 49, 30–33. [Google Scholar] [CrossRef] [PubMed]

| Study Invitation Sent to: | Overall Response Rate | |
|---|---|---|
| Austria | Random National Sample | 28.0% |
| Belgium | Random National Sample with additional convenience sample | 29.7% |
| Bosnia and Herzegovina | Total population | 5.5% |
| Bulgaria | Convenience National Sample | 94.3% |
| Croatia | Convenience National Sample | 11.7% |
| Czechia | Random National Sample from 4 regions and from list of young practitioners | 22.0% |
| Denmark | Total population | 1.5% |
| Estonia | Total population | 13.9% |
| Finland | Convenience National Sample | 15.5% |
| France | Total population | 2.1% |
| Germany | Convenience Sample in 6 areas | 15.5% |
| Greece | Random National Sample | 94.0% |
| Hungary | Convenience National Sample | 23.4% |
| Iceland | Convenience National Sample | 23.8% |
| Ireland | Total population | 12.2% |
| Israel | Convenience National Sample | 21.8% |
| Italy | Convenience National Sample | 25.6% |
| Kosovo * | Convenience Sample in 5 areas | 73.3% |
| Latvia | Total population | 9.2% |
| Lithuania | Convenience National Sample | 22.5% |
| Malta | Total population | 6.5% |
| Moldavia | Convenience Sample from 2 municipalities | 24.2% |
| Netherlands | Random National Sample with additional convenience sample | 18.9% |
| Norway | Total population | 10.5% |
| Poland | Convenience National Sample | 10.4% |
| Portugal | Random National Sample with additional convenience sample | 22.9% |
| Romania | Convenience National Sample | 25.0% |
| Serbia | Convenience National Sample | 90.0% |
| Slovenia | Convenience National Sample | 19.8% |
| Spain | Convenience National Sample | 77.0% |
| Sweden | Convenience National Sample | 7.2% |
| Switzerland | Convenience Sample | 32.0% |
| Turkey | Convenience Sample | 27.9% |
| TOTAL | 27.8% |
| n | % | |
|---|---|---|
| Number of GPs/GP Trainees | ||
| 1 | 1484 | 33.2 |
| 2–3 | 1193 | 26.7 |
| 4–5 | 680 | 15.2 |
| >5 | 1109 | 24.8 |
| Range of disciplines in the practice (Median: 3; IQR: 2–5) | ||
| 1–2 | 1385 | 31.9 |
| 3–4 | 1493 | 34.3 |
| 5+ | 1469 | 33.8 |
| Practice Location | ||
| Big (inner)city | 1455 | 32.7 |
| Suburbs | 450 | 10.1 |
| (Small) town | 827 | 18.6 |
| Mixed urban–rural | 895 | 20.1 |
| Rural | 819 | 18.4 |
| Practice payment system | ||
| Fee for service | 1716 | 39.2 |
| Capitation | 1854 | 42.4 |
| Other and/or mixed | 809 | 18.5 |
| Size of practice population (Median: 2727; IQR: 1550–7000) | ||
| ≤1500 | 1081 | 24.2 |
| >1500–≤3000 | 1381 | 30.9 |
| >3000–≤7000 | 933 | 20.9 |
| >7000 | 1071 | 24.0 |
| Equipment Items | n | % |
|---|---|---|
| Disposable GP coats | 3159 | 70.7 |
| Disposable gloves | 4381 | 98.1 |
| Surface disinfectant | 4378 | 98.0 |
| Paper to cover examination table | 4119 | 92.2 |
| A sink | 4272 | 95.7 |
| A tap operated with the elbow or with a movement detector | 2297 | 51.4 |
| A trash can that can be operated without contact with the hand | 3956 | 88.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collins, C.; Van Poel, E.; Šantrić Milićević, M.; Tripkovic, K.; Adler, L.; Bjerve Eide, T.; Murauskiene, L.; Windak, A.; Nessler, K.; Tahirbegolli, B.; et al. Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2022, 19, 7830. https://doi.org/10.3390/ijerph19137830
Collins C, Van Poel E, Šantrić Milićević M, Tripkovic K, Adler L, Bjerve Eide T, Murauskiene L, Windak A, Nessler K, Tahirbegolli B, et al. Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2022; 19(13):7830. https://doi.org/10.3390/ijerph19137830
Chicago/Turabian StyleCollins, Claire, Esther Van Poel, Milena Šantrić Milićević, Katica Tripkovic, Limor Adler, Torunn Bjerve Eide, Liubove Murauskiene, Adam Windak, Katarzyna Nessler, Bernard Tahirbegolli, and et al. 2022. "Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey" International Journal of Environmental Research and Public Health 19, no. 13: 7830. https://doi.org/10.3390/ijerph19137830
APA StyleCollins, C., Van Poel, E., Šantrić Milićević, M., Tripkovic, K., Adler, L., Bjerve Eide, T., Murauskiene, L., Windak, A., Nessler, K., Tahirbegolli, B., & Willems, S. (2022). Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 19(13), 7830. https://doi.org/10.3390/ijerph19137830








