Food Addiction Mediates the Relationship between Perceived Stress and Body Mass Index in Taiwan Young Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Demographic Information
2.3. Perceived Stress Scale (PSS-10)
2.4. Yale Food Addiction Scale (YFAS)
2.5. Statistical Analysis
3. Results
3.1. Sample Description
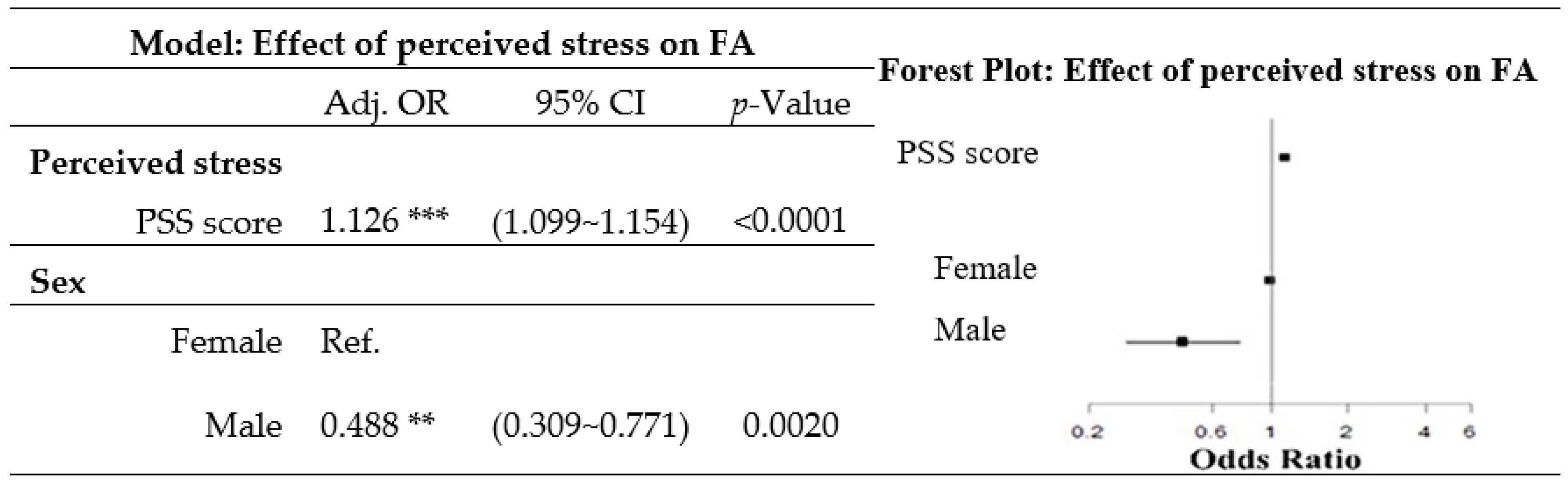
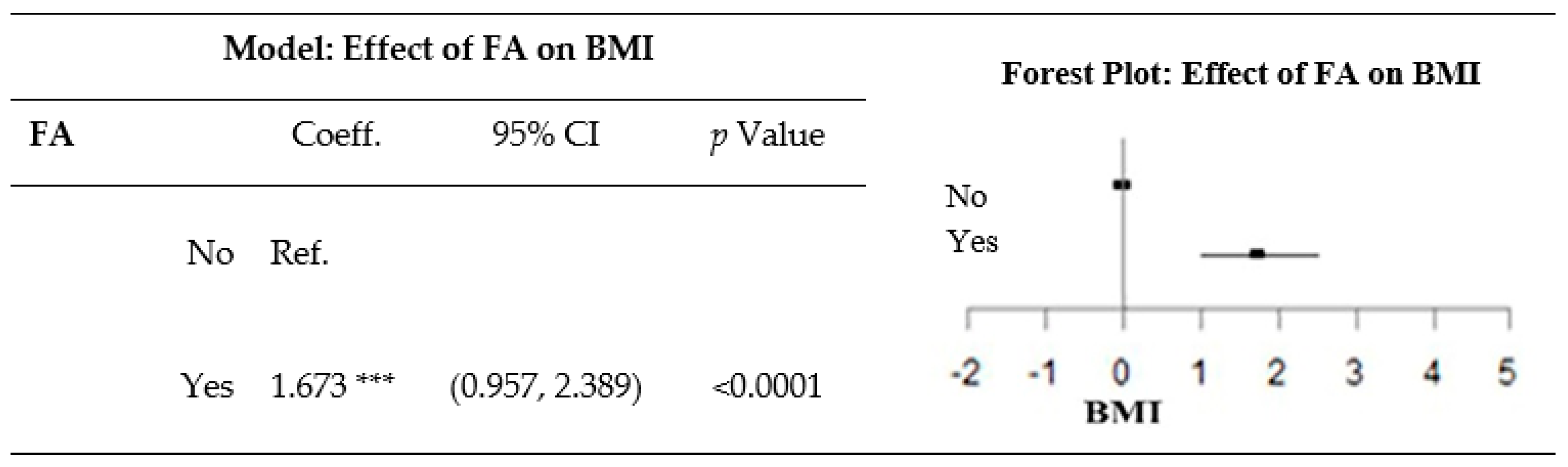
3.2. Effects of Perceived Stress on BMI
3.3. Effect of FA on BMI
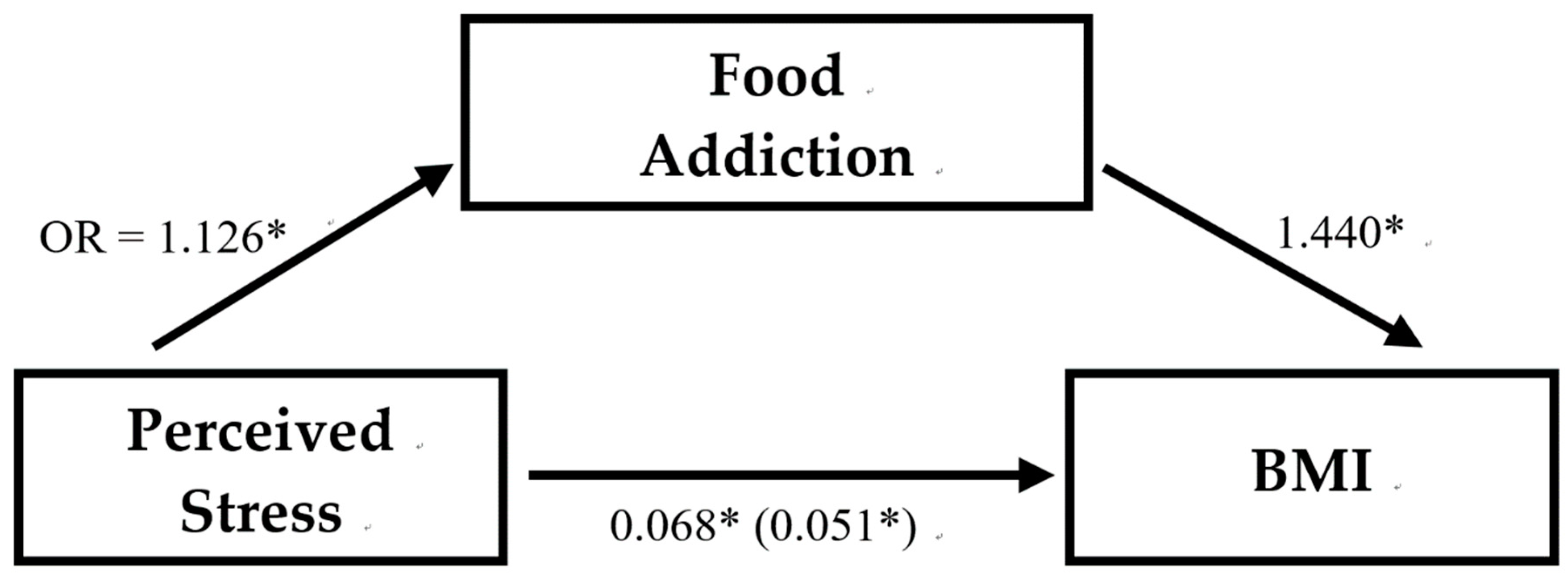
3.4. Effect of Perceived Stress and FA on BMI
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Prevalence of overweight among adults, BMI ≥ 25, age-standardized, 2017. Available online: https://apps.who.int/gho/data/view.main.GLOBAL2461A?lang=en (accessed on 20 April 2020).
- Pereira, V.H.; Marques, F.; Lages, V.; Pereira, F.G.; Patchev, A.; Almeida, O.F.; Almeida-Palha, J.; Sousa, N.; Cerqueira, J.J. Glucose intolerance after chronic stress is related with downregulated PPAR-gamma in adipose tissue. Cardiovasc. Diabetol. 2016, 15, 114. [Google Scholar] [CrossRef]
- Berthoud, H.R.; Münzberg, H.; Morrison, C.D. Blaming the brain for obesity: Integration of hedonic and homeostatic mechanisms. Gastroenterology 2017, 152, 1728–1738. [Google Scholar] [CrossRef]
- Masheb, R.M.; Ruser, C.B.; Min, K.M.; Bullock, A.J.; Dorflinger, L.M. Does food addiction contribute to excess weight among clinic patients seeking weight reduction? Examination of the modified yale food addiction survey. Compr. Psychiatry 2018, 84, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: A systematic review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef] [PubMed]
- Imperatori, C.; Fabbricatore, M.; Vumbaca, V.; Innamorati, M.; Contardi, A.; Farina, B. Food addiction: Definition, measurement and prevalence in healthy subjects and in patients with eating disorders. Riv. Psichiatr. 2016, 51, 60–65. [Google Scholar] [PubMed]
- De Vries, S.K.; Meule, A. Food addiction and bulimia nervosa: New data based on the Yale Food Addiction Scale 2.0. Eur. Eat. Disord. Rev. 2016, 24, 518–522. [Google Scholar] [CrossRef]
- Masheb, R.M.; Grilo, C.M. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int. J. Eat. Disord. 2006, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Loxton, N.J.; Levitan, R.D.; Kaplan, A.S.; Carter, J.C.; Kennedy, J.L. ’Food addiction’ and its association with a dopaminergic multilocus genetic profile. Physiol. Behav. 2013, 118, 63–69. [Google Scholar] [CrossRef]
- Davis, C.; Loxton, N.J. A psycho-genetic study of hedonic responsiveness in relation to “food addiction”. Nutrients 2014, 6, 4338–4353. [Google Scholar] [CrossRef]
- Martire, S.I.; Maniam, J.; South, T.; Holmes, N.; Westbrook, R.F.; Morris, M.J. Extended exposure to a palatable cafeteria diet alters gene expression in brain regions implicated in reward, and withdrawal from this diet alters gene expression in brain regions associated with stress. Behav. Brain Res. 2014, 265, 132–141. [Google Scholar] [CrossRef]
- De Ridder, D.; Manning, P.; Leong, S.L.; Ross, S.; Sutherland, W.; Horwath, C.; Vanneste, S. The brain, obesity and addiction: An EEG neuroimaging study. Sci. Rep. 2016, 6, 34122. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Wang, G.J.; Tomasi, D.; Baler, R.D. Obesity and addiction: Neurobiological overlaps. Obes. Rev. 2013, 14, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Koob, G.F. Neurobiology of opioid addiction: Opponent process, hyperkatifeia, and negative reinforcement. Biol. Psychiatry 2020, 87, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Hardy, R.; Fani, N.; Jovanovic, T.; Michopoulos, V. Food addiction and substance addiction in women: Common clinical characteristics. Appetite 2018, 120, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.S.; Wolf, E.J. PTSD, food addiction, and disordered eating in a sample of primarily older veterans: The mediating role of emotion regulation. Psychiatry Res. 2016, 243, 23–29. [Google Scholar] [CrossRef]
- Errisuriz, V.L.; Pasch, K.E.; Perry, C.L. Perceived stress and dietary choices: The moderating role of stress management. Eat. Behav. 2016, 22, 211–216. [Google Scholar] [CrossRef]
- Neseliler, S.; Tannenbaum, B.; Zacchia, M.; Larcher, K.; Coulter, K.; Lamarche, M.; Marliss, E.B.; Pruessner, J.; Dagher, A. Academic stress and personality interact to increase the neural response to high-calorie food cues. Appetite 2017, 116, 306–314. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Burrows, T.; Kay-Lambkin, F.; Pursey, K.; Skinner, J.; Dayas, C. Food addiction and associations with mental health symptoms: A systematic review with meta-analysis. J. Hum. Nutr. Diet. 2018, 31, 544–572. [Google Scholar] [CrossRef]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Chatterji, S.; Lee, S.; Ustün, T.B. The WHO world mental health (WMH) surveys. Psychiatr. Stuttg. 2009, 6, 5–9. [Google Scholar]
- Pan, W.H.; Flegal, K.M.; Chang, H.Y.; Yeh, W.T.; Yeh, C.J.; Lee, W.C. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: Implications for definitions of overweight and obesity for Asians. Am. J. Clin. Nutr. 2004, 79, 31–39. [Google Scholar] [CrossRef]
- Cohen, S. Perceived stress in a probability sample of the United States. In The Social Psychology of Health; Sage Publications, Inc.: New York, NY, USA, 1988; pp. 31–67. [Google Scholar]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Food addiction: An examination of the diagnostic criteria for dependence. J. Addict. Med. 2009, 3, 1–7. [Google Scholar] [CrossRef]
- Isasi, C.R.; Parrinello, C.M.; Jung, M.M.; Carnethon, M.R.; Birnbaum-Weitzman, O.; Espinoza, R.A.; Penedo, F.J.; Perreira, K.M.; Schneiderman, N.; Sotres-Alvarez, D.; et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann. Epidemiol. 2015, 25, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.L.; Backholer, K.; Williams, E.D.; Peeters, A.; Cameron, A.J.; Hare, M.J.; Shaw, J.E.; Magliano, D.J. Psychosocial stress is positively associated with body mass index gain over 5 years: Evidence from the longitudinal AusDiab study. Obesity 2014, 22, 277–286. [Google Scholar] [CrossRef]
- Bourdier, L.; Orri, M.; Carre, A.; Gearhardt, A.N.; Romo, L.; Dantzer, C.; Berthoz, S. Are emotionally driven and addictive-like eating behaviors the missing links between psychological distress and greater body weight? Appetite 2018, 120, 536–546. [Google Scholar] [CrossRef]
- Raymond, K.L.; Kannis-Dymand, L.; Lovell, G.P. A graduated food addiction classifications approach significantly differentiates depression, anxiety and stress among people with type 2 diabetes. Diabetes Res. Clin. Pract. 2017, 132, 95–101. [Google Scholar] [CrossRef]
- Kozak, A.T.; Davis, J.; Brown, R.; Grabowski, M. Are overeating and food addiction related to distress tolerance? An examination of residents with obesity from a, U.S. metropolitan area. Obes. Res. Clin. Pract. 2017, 11, 287–298. [Google Scholar] [CrossRef]
- Mason, S.M.; Flint, A.J.; Roberts, A.L.; Agnew-Blais, J.; Koenen, K.C.; Rich-Edwards, J.W. Posttraumatic stress disorder symptoms and food addiction in women by timing and type of trauma exposure. JAMA Psychiatry 2014, 71, 1271–1278. [Google Scholar] [CrossRef]
- Pedram, P.; Wadden, D.; Amini, P.; Gulliver, W.; Randell, E.; Cahill, F.; Vasdev, S.; Goodridge, A.; Carter, J.C.; Zhai, G.; et al. Food Addiction: Its prevalence and significant association with obesity in the general population. PLoS ONE. 2013, 8, e74832. [Google Scholar] [CrossRef] [PubMed]
- Sengor, G.; Gezer, C. Food addiction and its relationship with disordered eating behaviours and obesity. Eat. Weight Disord. 2019, 24, 1031–1039. [Google Scholar] [CrossRef]
- Burrows, T.; Hides, L.; Brown, R.; Dayas, C.V.; Kay-Lambkin, F. Differences in dietary preferences, personality and mental health in Australian adults with and without food addiction. Nutrients 2017, 9, E285. [Google Scholar] [CrossRef]
- Sanlier, N.; Turkozu, D.; Toka, O. Body image, food addiction, depression, and body mass index in university students. Ecol. Food Nutr. 2016, 55, 491–507. [Google Scholar] [CrossRef]
- Beyer, F.; Garcia-Garcia, I.; Heinrich, M.; Schroeter, M.L.; Sacher, J.; Luck, T.; Riedel-Heller, S.G.; Stumvoll, M.; Villringer, A.; Witte, A.V. Neuroanatomical correlates of food addiction symptoms and body mass index in the general population. Hum. Brain Mapp. 2019, 40, 2747–2758. [Google Scholar] [CrossRef] [PubMed]
- Maayan, L.; Hoogendoorn, C.; Sweat, V.; Convit, A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity 2011, 19, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Jeronimus, B.F.; Riese, H.; Sanderman, R.; Ormel, J. Mutual reinforcement between neuroticism and life experiences: A five-wave, 16-year study to test reciprocal causation. J. Pers. Soc. Psychol. 2014, 107, 751–764. [Google Scholar] [CrossRef] [PubMed]
- Benard, M.; Camilleri, G.M.; Etile, F.; Mejean, C.; Bellisle, F.; Reach, G.; Hercberg, S.; Péneau, S. Association between impulsivity and weight status in a general population. Nutrients 2017, 9, 217. [Google Scholar] [CrossRef]
- Escriva-Martinez, T.; Galiana, L.; Rodriguez-Arias, M.; Banos, R.M. The binge eating scale: Structural equation competitive models, invariance measurement between sexes, and relationships with food addiction, impulsivity, binge drinking, and body mass index. Front. Psychol. 2019, 10, 530. [Google Scholar] [CrossRef]
- Murphy, C.M.; Stojek, M.K.; MacKillop, J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite 2014, 73, 45–50. [Google Scholar] [CrossRef]
- Levoy, E.; Lazaridou, A.; Brewer, J.; Fulwiler, C. An exploratory study of mindfulness based stress reduction for emotional eating. Appetite 2017, 109, 124–130. [Google Scholar] [CrossRef]
- Hebebrand, J.; Albayrak, O.; Adan, R.; Antel, J.; Dieguez, C.; de Jong, J.; Leng, G.; Menzies, J.; Mercer, J.G.; Murphy, M.; et al. “Eating addiction”, rather than “food addiction”5, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 2014, 47, 295–306. [Google Scholar] [CrossRef]
- Paterson, C.; Lacroix, E.; von Ranson, K.M. Conceptualizing addictive-like eating: A qualitative analysis. Appetite 2019, 141, 104326. [Google Scholar] [CrossRef] [PubMed]
- Montesi, L.; El Ghoch, M.; Brodosi, L.; Calugi, S.; Marchesini, G.; Dalle Grave, R. Long-term weight loss maintenance for obesity: A multidisciplinary approach. Diabetes Metab. Syndr. Obes. 2016, 9, 37–46. [Google Scholar] [PubMed]
- Heinz, A.; Beck, A.; Halil, M.G.; Pilhatsch, M.; Smolka, M.N.; Liu, S. Addiction as learned behavior patterns. J. Clin. Med. 2019, 8, E1086. [Google Scholar] [CrossRef] [PubMed]

| Entire Cohort | Non-Food Addiction | Food Addiction | p-Value | p for Trend | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Sex | <0.0001 # | |||||||
| Female | 1387 | 77.92% | 1180 | 85.08% | 207 | 14.92% | ||
| Male | 393 | 22.08% | 369 | 93.89% | 24 | 6.11% | ||
| Age group (year) | 0.0216 # | |||||||
| 20~29 | 1312 | 73.71% | 1093 | 88.43% | 143 | 11.57% | ||
| 30~39 | 429 | 24.10% | 403 | 83.44% | 80 | 16.56% | ||
| ≥40 | 39 | 2.19% | 53 | 86.89% | 8 | 13.11% | ||
| Mean (standard deviation (SD)) | 26.96 | (5.56) | 26.89 | (5.57) | 27.38 | (5.51) | 0.2132 † | |
| Body mass index (BMI) (kg/m2) | 0.0011 # | 0.0001 | ||||||
| <18.5 | 156 | 8.76% | 141 | 90.38% | 15 | 9.62% | ||
| 18.5~24 | 916 | 51.46% | 819 | 89.41% | 97 | 10.59% | ||
| 24~27 | 314 | 17.64% | 265 | 84.39% | 49 | 15.61% | ||
| ≥27 | 394 | 23.13% | 324 | 82.23% | 70 | 17.77% | ||
| Mean (SD) | 23.98 | (5.36) | 23.76 | (5.15) | 25.47 | (6.39) | <0.0001 † | |
| Educational attainment | 0.0533 # | |||||||
| Less than high school | 46 | 2.58% | 39 | 84.78% | 7 | 15.22% | ||
| College/University | 1314 | 73.82% | 1130 | 86.00% | 184 | 14.00% | ||
| Master’s or more | 420 | 23.60% | 380 | 90.48% | 40 | 9.52% | ||
| Employment status | 0.8223 # | |||||||
| Full time | 961 | 53.99% | 833 | 86.68% | 128 | 13.32% | ||
| Part time | 129 | 7.25% | 111 | 86.05% | 18 | 13.95% | ||
| Unemployed | 182 | 10.22% | 157 | 86.26% | 25 | 13.74% | ||
| Student | 508 | 28.54% | 448 | 88.19% | 60 | 11.81% | ||
| PSS score group | <0.0001 # | <0.0001 | ||||||
| 0~10 | 133 | 7.47% | 130 | 97.74% | 3 | 2.26% | ||
| 11~20 | 791 | 44.44% | 736 | 93.05% | 55 | 6.95% | ||
| 21~30 | 770 | 43.26% | 626 | 81.30% | 144 | 18.70% | ||
| 31~40 | 86 | 4.83% | 57 | 66.28% | 29 | 33.72% | ||
| Mean (SD) | 19.87 | (6.71) | 19.23 | (6.55) | 24.12 | (6.20) | <0.0001 † | |
| PSS Score 0~10 | PSS Score 11~20 | PSS Score 21~30 | PSS Score 31~40 | PSS Score Mean (SD) | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Sex | |||||||||
| Female | 77 | 57.89% | 571 | 72.19% | 661 | 85.84% | 78 | 90.70% | 20.63 (6.49) |
| Male | 56 | 42.11% | 220 | 27.81% | 109 | 14.16% | 8 | 9.30% | 17.17 (6.78) |
| p-Value | <0.0001 # p for trend <0.0001 | <0.0001 † | |||||||
| Ratio of F:M | 1.4 | 2.6 | 6.1 | 9.8 | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.-S.; Tung, Y.-T.; Yen, Y.-C.; Chien, Y.-W. Food Addiction Mediates the Relationship between Perceived Stress and Body Mass Index in Taiwan Young Adults. Nutrients 2020, 12, 1951. https://doi.org/10.3390/nu12071951
Lin Y-S, Tung Y-T, Yen Y-C, Chien Y-W. Food Addiction Mediates the Relationship between Perceived Stress and Body Mass Index in Taiwan Young Adults. Nutrients. 2020; 12(7):1951. https://doi.org/10.3390/nu12071951
Chicago/Turabian StyleLin, Yi-Syuan, Yu-Tang Tung, Yu-Chun Yen, and Yi-Wen Chien. 2020. "Food Addiction Mediates the Relationship between Perceived Stress and Body Mass Index in Taiwan Young Adults" Nutrients 12, no. 7: 1951. https://doi.org/10.3390/nu12071951
APA StyleLin, Y.-S., Tung, Y.-T., Yen, Y.-C., & Chien, Y.-W. (2020). Food Addiction Mediates the Relationship between Perceived Stress and Body Mass Index in Taiwan Young Adults. Nutrients, 12(7), 1951. https://doi.org/10.3390/nu12071951






