Explainable AI-Based Identification of Contributing Factors to the Mood State Change in Children and Adolescents with Pre-Existing Psychiatric Disorders in the Context of COVID-19-Related Lockdowns in Greece
Abstract
:1. Introduction
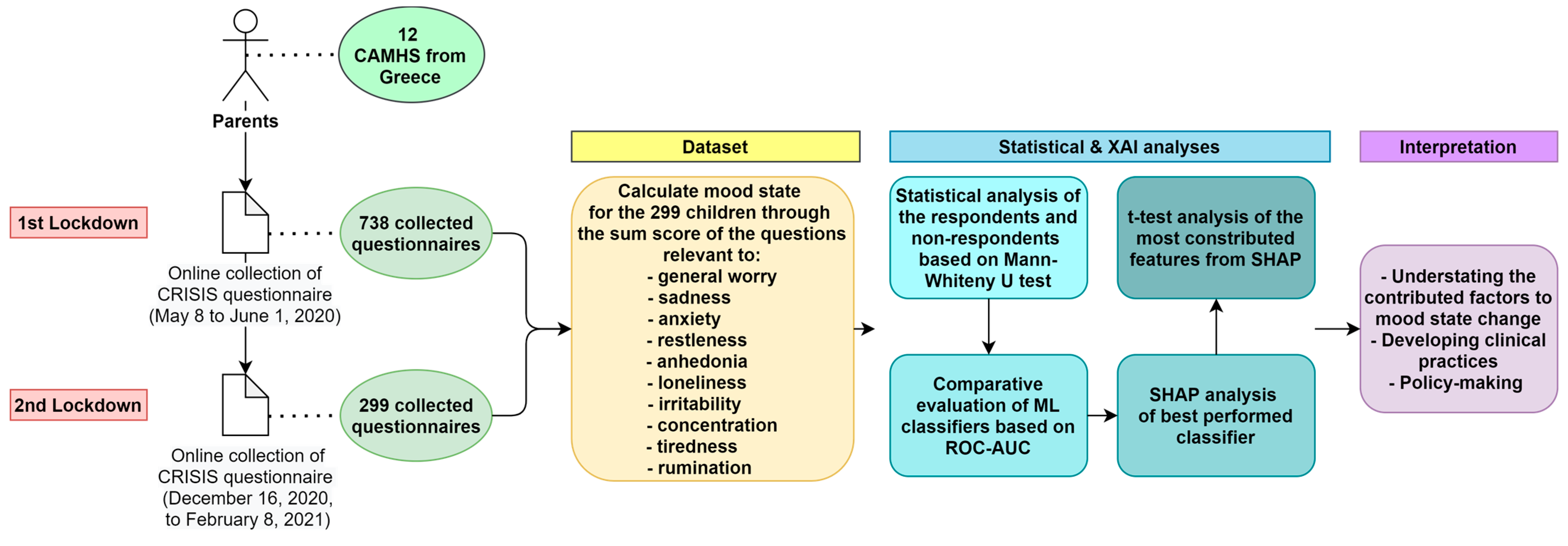
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
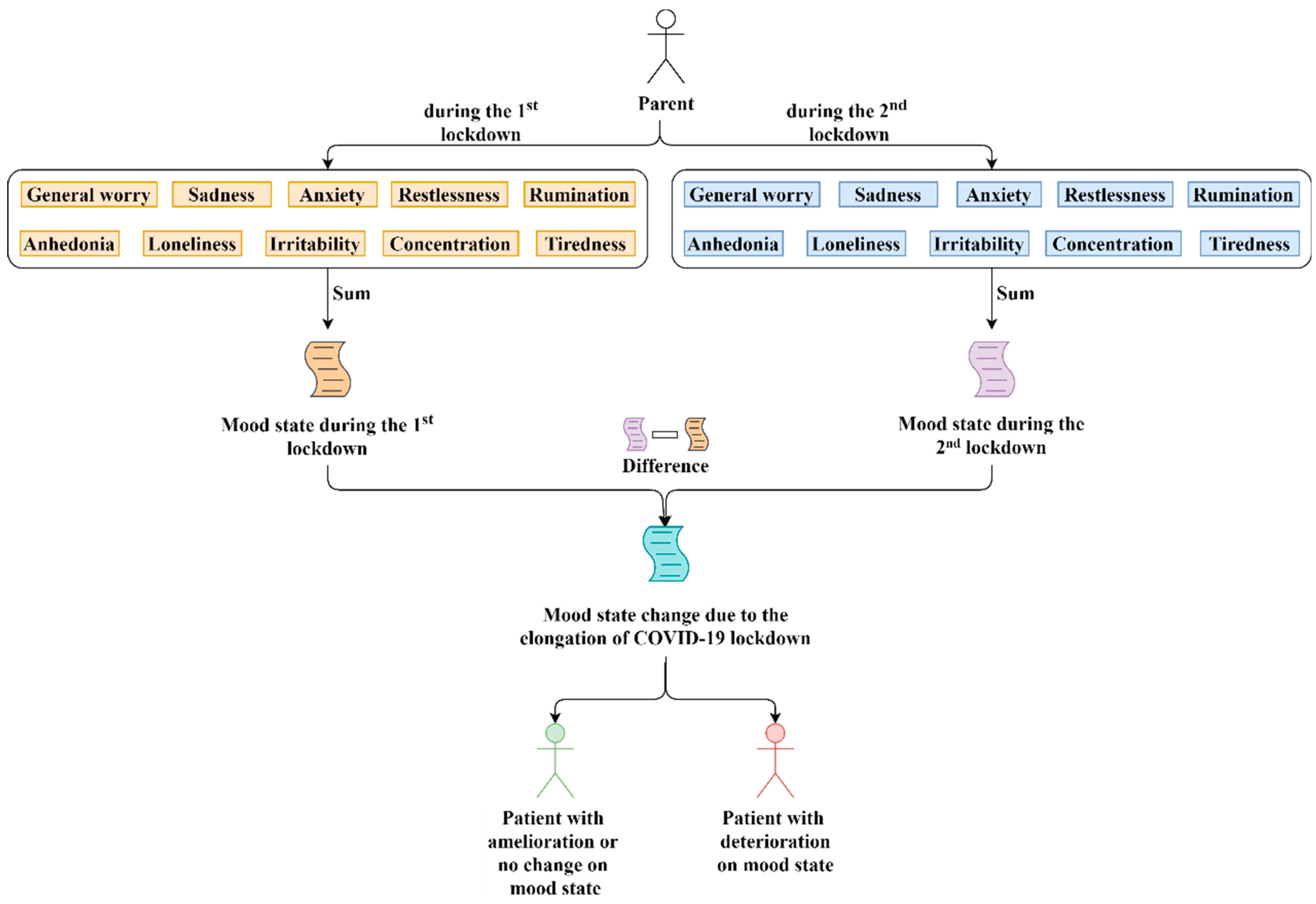
2.3. Mood States
2.4. Data Analysis Plan
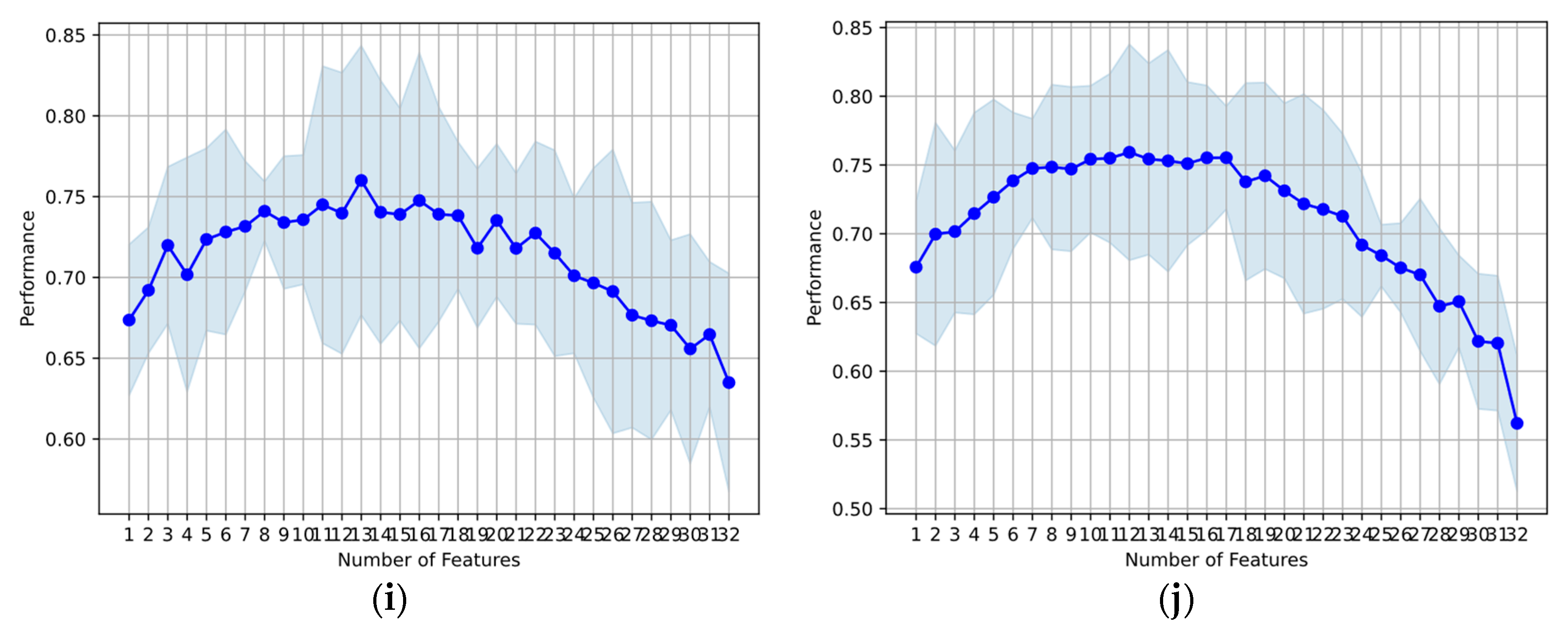
2.5. Evaluation Set-Up
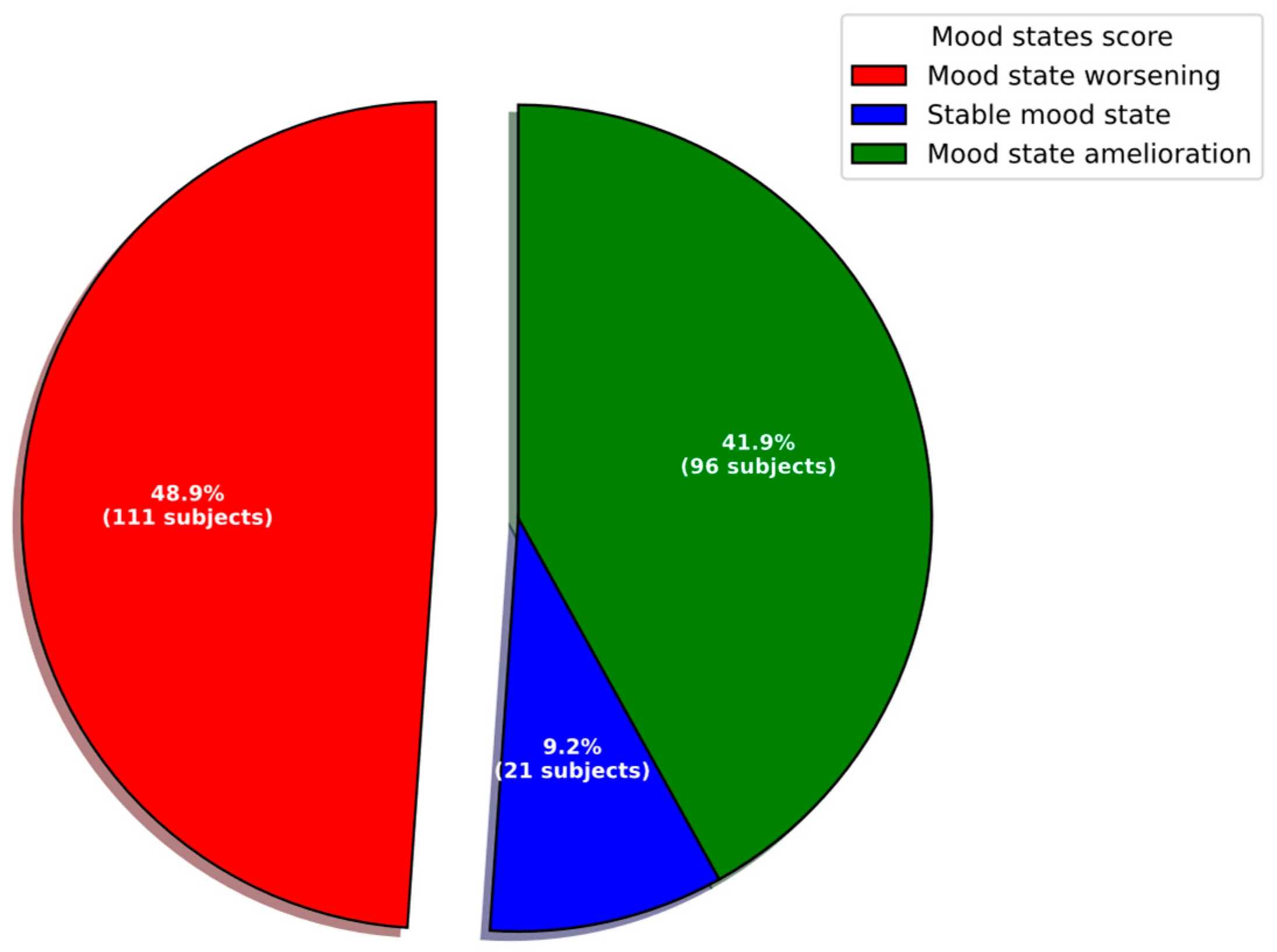
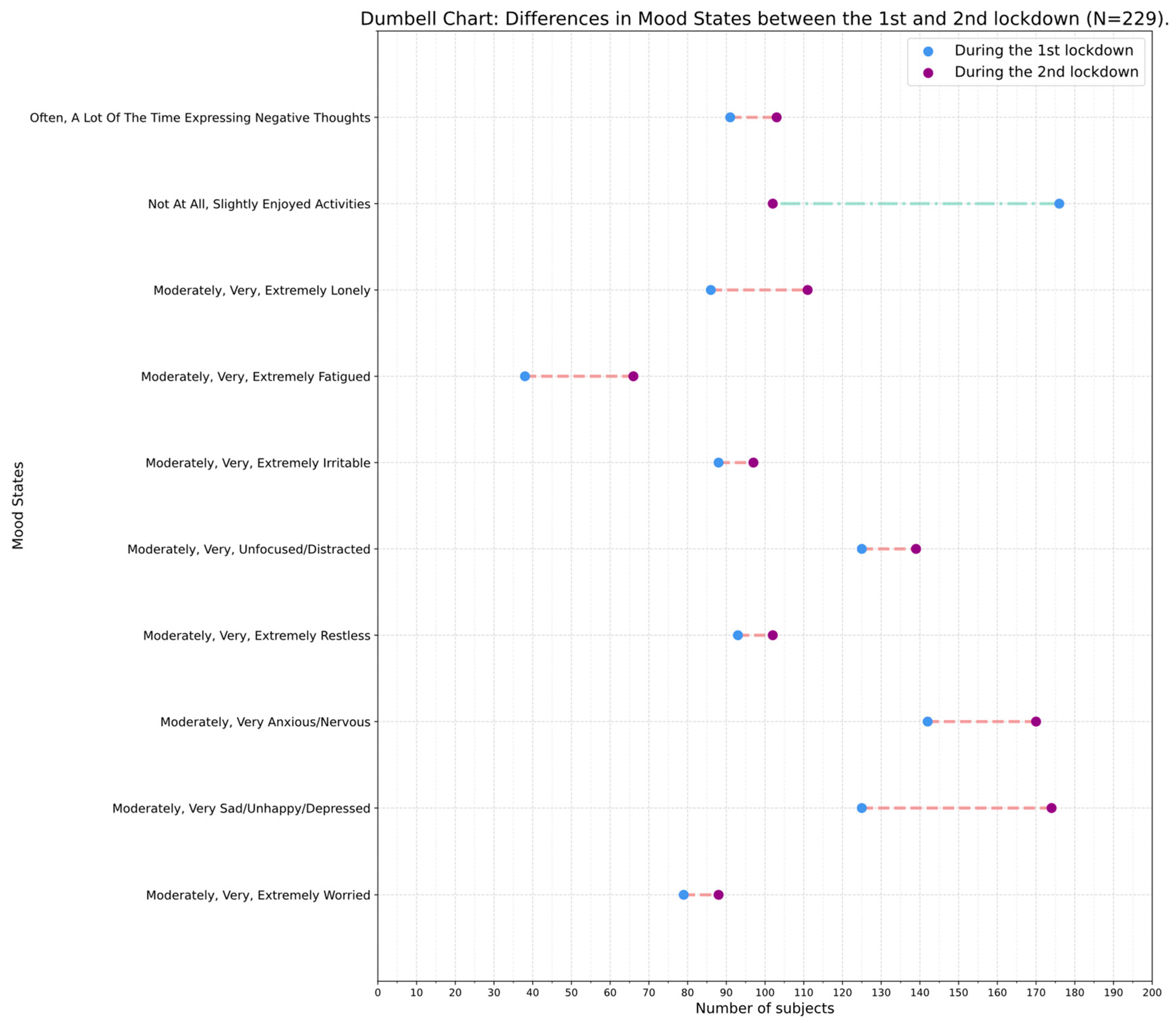
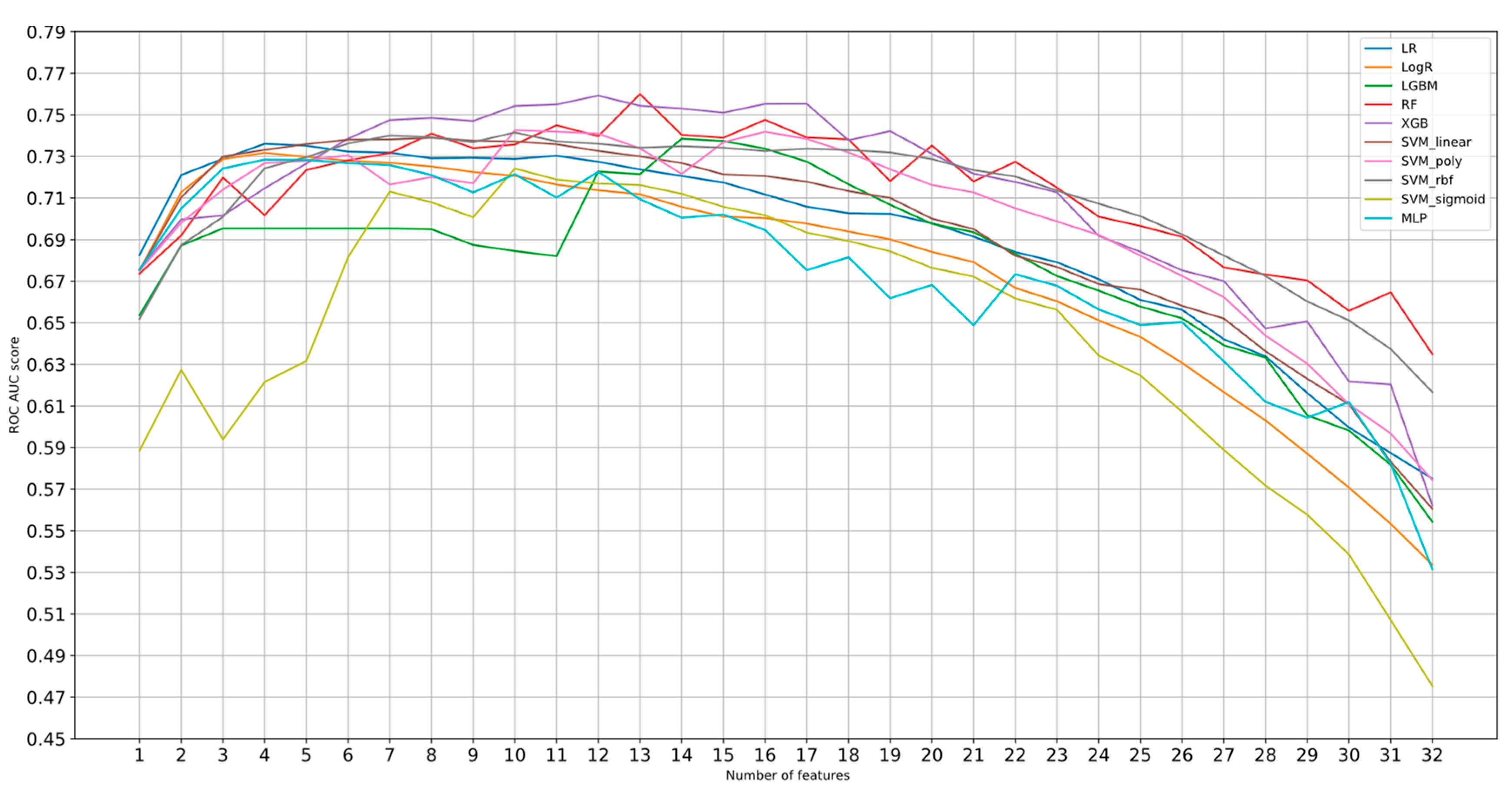
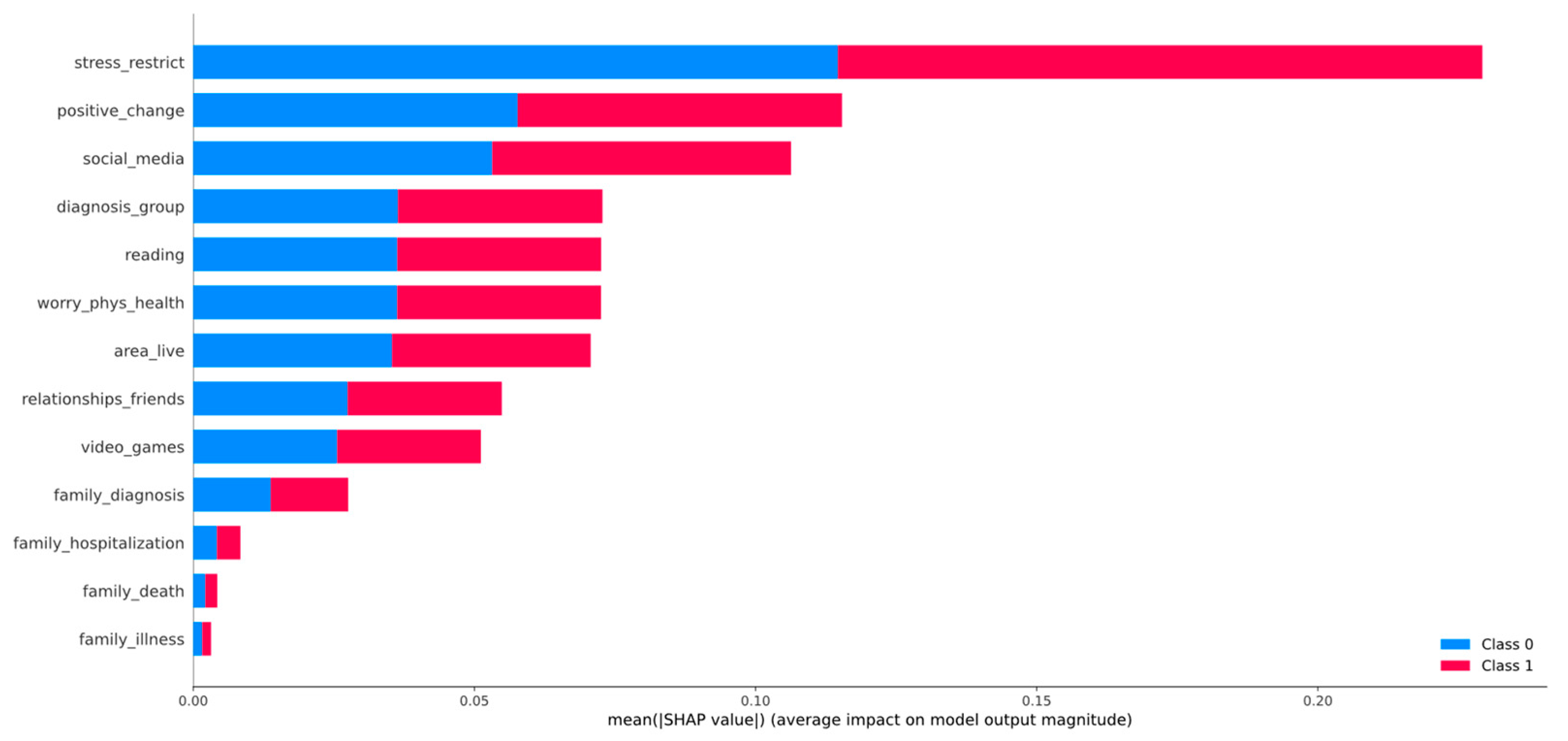
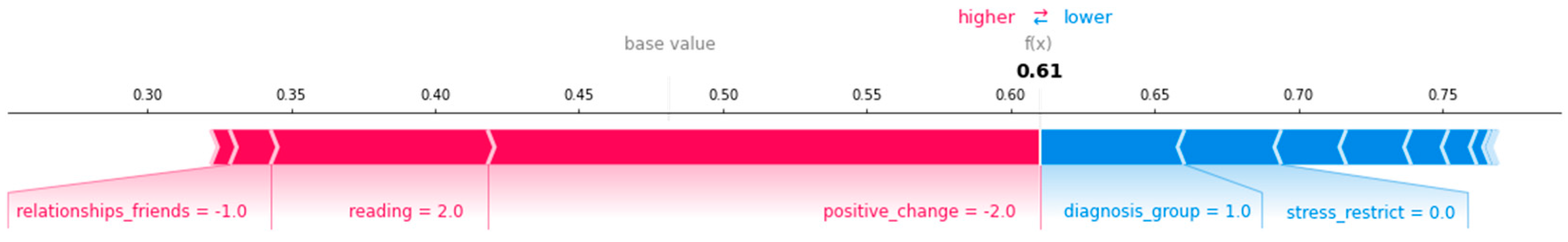
3. Results and Discussion
- A longitudinal survey during two consecutive lockdowns of different duration in Greece.
- A focus on children and adolescents with pre-pandemic diagnosed psychiatric and developmental disorders (Table 1).
- The development of a dataset with 52 heterogenous features related to demographics, medical data, social life, personal life, family life, daily stresses, and daily activities (Table 2). The dataset consists of a blend of features that were identified as important through the presented literature review (Section 1).
- The use of an XAI pipeline for the identification of the most contributing factors that helped the examined population to retain their mood state, i.e., searching for possible activities and behaviors that helped children cope with the new daily life during COVID-19 pandemic and related restrictive measures.
- The findings have implications for clinical practice as they highlight both the importance of ongoing monitoring mood states during lockdown periods, and the personal characteristics and daily activities that could contribute positively to mood states during severe events, such as lockdowns.
- The findings have implications for policy-makers’ decisions relevant for child mental health care in Greece, i.e., prioritization, better access to mental health care and psychosocial support services for children and their families, and development of evidence-based interventions to mitigate mental health impact of future pandemic-related lockdowns.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Muehlschlegel, P.A.; Parkinson, E.A.; Chan, R.Y.; Arden, M.A.; Armitage, C.J. Learning from Previous Lockdown Measures and Minimising Harmful Biopsychosocial Consequences as They End: A Systematic Review. J. Glob. Health 2021, 11, 05008. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, M.; Manocha, A.; Ahanger, T.A.; Alqahtani, A. Artificial Intelligence-Inspired Comprehensive Framework for COVID-19 Outbreak Control. Artif. Intell. Med. 2022, 127, 102288. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; Smith, P. Debate: Recognising and Responding to the Mental Health Needs of Young People in the Era of COVID-19. Child Adolesc. Ment. Health 2020, 25, 169–170. [Google Scholar] [CrossRef] [PubMed]
- Giannopoulou, I.; Galinaki, S.; Kollintza, E.; Adamaki, M.; Kympouropoulos, S.; Alevyzakis, E.; Tsamakis, K.; Tsangaris, I.; Spandidos, D.A.; Siafakas, N.; et al. COVID-19 and Post-traumatic Stress Disorder: The Perfect ‘Storm’ for Mental Health (Review). Exp. Ther. Med. 2021, 22, 1162. [Google Scholar] [CrossRef] [PubMed]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent Psychiatric Disorders during the COVID-19 Pandemic and Lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and Lockdown on Mental Health of Children and Adolescents: A Narrative Review with Recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Panchal, U.; Salazar de Pablo, G.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The Impact of COVID-19 Lockdown on Child and Adolescent Mental Health: Systematic Review. Eur. Child Adolesc. Psychiatry 2023, 32, 1151–1177. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Otto, C.; Devine, J.; Löffler, C.; Hurrelmann, K.; Bullinger, M.; Barkmann, C.; Siegel, N.A.; et al. Quality of Life and Mental Health in Children and Adolescents during the First Year of the COVID-19 Pandemic: Results of a Two-Wave Nationwide Population-Based Study. Eur. Child Adolesc. Psychiatry 2023, 32, 575–588. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-Analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef]
- Orgilés, M.; Morales, A.; Delvecchio, E.; Mazzeschi, C.; Espada, J.P. Immediate Psychological Effects of the COVID-19 Quarantine in Youth From Italy and Spain. Front. Psychol. 2020, 11, 579038. [Google Scholar] [CrossRef] [PubMed]
- Cooper, K.; Hards, E.; Moltrecht, B.; Reynolds, S.; Shum, A.; McElroy, E.; Loades, M. Loneliness, Social Relationships, and Mental Health in Adolescents during the COVID-19 Pandemic. J. Affect. Disord 2021, 289, 98–104. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Kauhanen, L.; Wan Mohd Yunus, W.M.A.; Lempinen, L.; Peltonen, K.; Gyllenberg, D.; Mishina, K.; Gilbert, S.; Bastola, K.; Brown, J.S.L.; Sourander, A. A Systematic Review of the Mental Health Changes of Children and Young People before and during the COVID-19 Pandemic. Eur. Child Adolesc. Psychiatry 2023, 32, 995–1013. [Google Scholar] [CrossRef] [PubMed]
- Wolf, K.; Schmitz, J. Scoping Review: Longitudinal Effects of the COVID-19 Pandemic on Child and Adolescent Mental Health. Eur. Child Adolesc. Psychiatry 2023, 1–56. [Google Scholar] [CrossRef]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and Anxiety among Adolescents during COVID-19: A Cross-Sectional Study. Brain Behav. Immun. 2020, 88, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.J.; Barblan, L.P.; Lory, I.; Landolt, M.A. Age-Related Effects of the COVID-19 Pandemic on Mental Health of Children and Adolescents. Eur. J. Psychotraumatol. 2021, 12, 1901407. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic Symptoms and Concern Regarding COVID-19 among Chinese College and Primary School Students: A Cross-Sectional Survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef]
- McKune, S.L.; Acosta, D.; Diaz, N.; Brittain, K.; Beaulieu, D.J.; Maurelli, A.T.; Nelson, E.J. Psychosocial Health of School-Aged Children during the Initial COVID-19 Safer-at-Home School Mandates in Florida: A Cross-Sectional Study. BMC Public Health 2021, 21, 603. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and Socio-Demographic Correlates of Psychological Health Problems in Chinese Adolescents during the Outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and Burden of the Coronavirus 2019 (COVID-19) Pandemic for Child and Adolescent Mental Health: A Narrative Review to Highlight Clinical and Research Needs in the Acute Phase and the Long Return to Normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Bouter, D.C.; Zarchev, M.; de Neve-Enthoven, N.G.M.; Ravensbergen, S.J.; Kamperman, A.M.; Hoogendijk, W.J.G.; Grootendorst-van Mil, N.H. A Longitudinal Study of Mental Health in At-Risk Adolescents before and during the COVID-19 Pandemic. Eur. Child Adolesc. Psychiatry 2023, 32, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Serrano, J.; Díaz-Bóveda, R.; González-Vallespí, L.; Santamarina-Pérez, P.; Bretones-Rodríguez, A.; Calvo, R.; Lera-Miguel, S. Psychological Impact during COVID-19 Lockdown in Children and Adolescents with Previous Mental Health Disorders. Rev. Psiquiatr. Salud Ment. 2023, 16, 32–41. [Google Scholar] [CrossRef]
- Magklara, K.; Giannopoulou, I.; Kotsis, K.; Tsalamanios, E.; Grigoriadou, A.; Ladopoulou, K.; Koullourou, I.; Serdari, A.; Sadeghi, N.; O’Callaghan, G.; et al. Mental Health of Children and Adolescents with Pre-Existing Psychiatric and Developmental Disorders during the First Pandemic-Related Lockdown: A Cross-Sectional Study in Greece. Psychiatry Res. Commun. 2022, 2, 100034. [Google Scholar] [CrossRef]
- Lavenne-Collot, N.; Ailliot, P.; Badic, S.; Favé, A.; François, G.; Saint-André, S.; Thierry, A.; Bronsard, G. Les enfants suivis en psychiatrie infanto-juvénile ont ils connu la dégradation redoutée pendant la période de confinement liée à la pandémie COVID-19? Neuropsychiatr. L’Enfance L’Adolescence 2021, 69, 121–131. [Google Scholar] [CrossRef]
- Tanir, Y.; Karayagmurlu, A.; Kaya, İ.; Kaynar, T.B.; Türkmen, G.; Dambasan, B.N.; Meral, Y.; Coşkun, M. Exacerbation of Obsessive Compulsive Disorder Symptoms in Children and Adolescents during COVID-19 Pandemic. Psychiatry Res. 2020, 293, 113363. [Google Scholar] [CrossRef]
- Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute Stress, Behavioural Symptoms and Mood States among School-Age Children with Attention-Deficit/Hyperactive Disorder during the COVID-19 Outbreak. Asian J. Psychiatr. 2020, 51, 102077. [Google Scholar] [CrossRef]
- Masi, A.; Mendoza Diaz, A.; Tully, L.; Azim, S.I.; Woolfenden, S.; Efron, D.; Eapen, V. Impact of the COVID-19 Pandemic on the Well-Being of Children with Neurodevelopmental Disabilities and Their Parents. J. Paediatr. Child Health 2021, 57, 631–636. [Google Scholar] [CrossRef]
- Graell, M.; Morón-Nozaleda, M.G.; Camarneiro, R.; Villaseñor, Á.; Yáñez, S.; Muñoz, R.; Martínez-Núñez, B.; Miguélez-Fernández, C.; Muñoz, M.; Faya, M. Children and Adolescents with Eating Disorders during COVID-19 Confinement: Difficulties and Future Challenges. Eur. Eat Disord. Rev. 2020, 28, 864–870. [Google Scholar] [CrossRef]
- Stevanovic, D.; Kabukcu Basay, B.; Basay, O.; Leskauskas, D.; Nussbaum, L.; Zirakashvili, M. COVID-19 Pandemic-Related Aspects and Predictors of Emotional and Behavioural Symptoms in Youth with Pre-Existing Mental Health Conditions: Results from Georgia, Lithuania, Romania, Serbia, and Turkey. Nord. J. Psychiatry 2021, 76, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Monaro, M.; Conversano, C.; Gemignani, A.; Sartori, G. Machine Learning in Psychometrics and Psychological Research. Front. Psychol. 2020, 10, 2970. [Google Scholar] [CrossRef] [PubMed]
- Comito, C.; Pizzuti, C. Artificial Intelligence for Forecasting and Diagnosing COVID-19 Pandemic: A Focused Review. Artif. Intell. Med. 2022, 128, 102286. [Google Scholar] [CrossRef] [PubMed]
- Nikolaidis, A.; DeRosa, J.; Kass, M.; Droney, I.; Alexander, L.; Di Martino, A.; Bromet, E.; Merikangas, K.; Milham, M.P.; Paksarian, D. Heterogeneity in COVID-19 Pandemic-Induced Lifestyle Stressors Predicts Future Mental Health in Adults and Children in the US and UK. J. Psychiatr. Res. 2022, 147, 291–300. [Google Scholar] [CrossRef]
- Ntakolia, C.; Priftis, D.; Charakopoulou-Travlou, M.; Rannou, I.; Magklara, K.; Giannopoulou, I.; Kotsis, K.; Serdari, A.; Tsalamanios, E.; Grigoriadou, A.; et al. An Explainable Machine Learning Approach for COVID-19’s Impact on Mood States of Children and Adolescents during the First Lockdown in Greece. Healthcare 2022, 10, 149. [Google Scholar] [CrossRef]
- National Center for Health Statistics. International Classification of Diseases, Tenth Revision (ICD-10); Centers for Disease Control and Prevention: Herndon, VA, USA, 2023. [Google Scholar]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. A Machine Learning Pipeline for Predicting Joint Space Narrowing in Knee Osteoarthritis Patients. In Proceedings of the 2020 IEEE 20th International Conference on Bioinformatics and Bioengineering (BIBE), Cincinnati, OH, USA, 26–28 October 2020; pp. 934–941. [Google Scholar]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. Identification of Most Important Features Based on a Fuzzy Ensemble Technique: Evaluation on Joint Space Narrowing Progression in Knee Osteoarthritis Patients. Int. J. Med. Inform. 2021, 156, 104614. [Google Scholar] [CrossRef]
- Boateng, E.Y.; Abaye, D.A. A Review of the Logistic Regression Model with Emphasis on Medical Research. J. Data Anal. Inf. Process. 2019, 7, 190–207. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013; ISBN 978-0-470-58247-3. [Google Scholar]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.-Y. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In Advances in Neural Information Processing Systems; Curran Associates, Inc.: New York, NY, USA, 2017; Volume 30. [Google Scholar]
- Wang, D.; Zhang, Y.; Zhao, Y. LightGBM: An Effective MiRNA Classification Method in Breast Cancer Patients. In Proceedings of the 2017 International Conference on Computational Biology and Bioinformatics, Newark, NJ, USA, 18–20 October 2017; Association for Computing Machinery: New York, NY, USA, 2017; pp. 7–11. [Google Scholar]
- Taud, H.; Mas, J.F. Multilayer Perceptron (MLP). In Geomatic Approaches for Modeling Land Change Scenarios; Camacho Olmedo, M.T., Paegelow, M., Mas, J.-F., Escobar, F., Eds.; Lecture Notes in Geoinformation and Cartography; Springer International Publishing: Cham, Switzerland, 2018; pp. 451–455. ISBN 978-3-319-60801-3. [Google Scholar]
- Karlik, B.; Olgac, A.V. Performance Analysis of Various Activation Functions in Generalized MLP Architectures o. J. Artif. Intell. Expert Syst. 2010, 1, 111–122. [Google Scholar]
- Awad, M.; Khanna, R. Support Vector Machines for Classification. In Efficient Learning Machines: Theories, Concepts, and Applications for Engineers and System Designers; Awad, M., Khanna, R., Eds.; Apress: Berkeley, CA, USA, 2015; pp. 39–66. ISBN 978-1-4302-5990-9. [Google Scholar]
- Cortes, C.; Vapnik, V. Support-Vector Networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Biau, G.; Scornet, E. A Random Forest Guided Tour. Test 2016, 25, 197–227. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ogunleye, A.; Wang, Q.-G. XGBoost Model for Chronic Kidney Disease Diagnosis. IEEE/ACM Trans. Comput. Biol. Bioinform. 2020, 17, 2131–2140. [Google Scholar] [CrossRef]
- Prabha, A.; Yadav, J.; Rani, A.; Singh, V. Design of Intelligent Diabetes Mellitus Detection System Using Hybrid Feature Selection Based XGBoost Classifier. Comput. Biol. Med. 2021, 136, 104664. [Google Scholar] [CrossRef]
- Ntakolia, C.; Kokkotis, C.; Moustakidis, S.; Tsaopoulos, D. Prediction of Joint Space Narrowing Progression in Knee Osteoarthritis Patients. Diagnostics 2021, 11, 285. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A Unified Approach to Interpreting Model Predictions. In Advances in Neural Information Processing Systems; Curran Associates, Inc.: New York, NY, USA, 2017; Volume 30. [Google Scholar]
- Bai, M.-S.; Miao, C.-Y.; Zhang, Y.; Xue, Y.; Jia, F.-Y.; Du, L. COVID-19 and Mental Health Disorders in Children and Adolescents (Review). Psychiatry Res. 2022, 317, 114881. [Google Scholar] [CrossRef]
- Patel, K. Mental Health Implications of COVID-19 on Children with Disabilities. Asian J. Psychiatr. 2020, 54, 102273. [Google Scholar] [CrossRef]
- Aebi, M.; Kuhn, C.; Banaschewski, T.; Grimmer, Y.; Poustka, L.; Steinhausen, H.-C.; Goodman, R. The Contribution of Parent and Youth Information to Identify Mental Health Disorders or Problems in Adolescents. Child Adolesc. Psychiatry Ment. Health 2017, 11, 23. [Google Scholar] [CrossRef]
- Fischer, K.; Tieskens, J.M.; Luijten, M.A.J.; Zijlmans, J.; van Oers, H.A.; de Groot, R.; van der Doelen, D.; van Ewijk, H.; Klip, H.; van der Lans, R.M.; et al. Internalizing Problems before and during the COVID-19 Pandemic in Independent Samples of Dutch Children and Adolescents with and without Pre-Existing Mental Health Problems. Eur. Child Adolesc. Psychiatry 2022, 32, 1873–1883. [Google Scholar] [CrossRef]



| Sociodemographic Characteristics | Population (%) |
|---|---|
| Age, mean ± standard deviation | 9.97 ± 3.77 |
| Sex | |
| Male | 154 (67.25%) |
| Female | 75 (32.75%) |
| Residential area | |
| City | 135 (58.95%) |
| Suburbs of a city | 64 (27.95%) |
| Town | 22 (9.61%) |
| Rural area | 6 (2.62%) |
| Island | 2 (0.87%) |
| Disorders | |
| Developmental disorders 1 | 105 (45.85%) |
| Psychiatric disorders 2 | 124 (54.15%) |
| Category | Features | Description |
|---|---|---|
| Demographics | age_group | Age group of the children |
| gender_child | Gender of the children | |
| area_live | Area of residence | |
| Social life | recommendations | Change in the difficulty to follow recommendations regarding social distancing between the 1st and 2nd lockdown |
| relationships_friends | Change in the quality of the child’s relationships with his/her friends between the 1st and 2nd lockdown | |
| soc_media | Change in the time spent using social media (e.g., Facetime, Facebook, Instagram, Snapchat, Twitter, Tiktok) between the 1st and 2nd lockdown | |
| Personal life | positive_change | Change in the positive changes in the child’s life due to the coronavirus/COVID-19 crisis between the 1st and 2nd lockdown |
| Family life | family_impact | If any event that affected the family occurred due to COVID-19 in the 1st and 2nd lockdown |
| finance | Change in the financial problems faced by the family due to the coronavirus/COVID-19 crisis between the 1st and 2nd lockdown | |
| relationships_family | Changes in the quality of relationships between the child and members of his/her family between the 1st and 2nd lockdown | |
| family_lost_job | Whether the child’s family members lost their job due to coronavirus/COVID-19 in the 1st or/and 2nd lockdown | |
| economical_impact | Whether the child’s family members lost earnings due to coronavirus/COVID-19 in the 1st or/and 2nd lockdown | |
| Daily activities | exercise | Change in the frequency the child engaged in exercise (e.g., increased heart rate, breathing) for at least 30 min between the 1st and 2nd lockdown |
| video_games | Change in the time spent playing video games between the 1st and 2nd lockdown | |
| tv | Change in the time spent watching TV or digital means (e.g., Netflix, Youtube, or web surfing) between the 1st and 2nd lockdown | |
| reading | Change in the frequency the child asked questions, read, or talked about coronavirus/COVID-19 between the 1st and 2nd lockdown | |
| Health concerns | worry_self_infected | Change in the child’s worry about becoming infected between the 1st and 2nd lockdown |
| worry_family_infected | Change in the child’s worry about family members or friends becoming infected between the 1st and 2nd lockdown | |
| worry_phys_health | Change in worry that physical health will be affected by coronavirus/COVID-19 | |
| worry_mental_health | Change in worry that the child’s mental/emotional health will be affected by coronavirus/COVID-19 between the 1st and 2nd lockdown | |
| Daily stresses | stress_restrict | Change in stress caused by the curfew between the 1st and 2nd lockdown |
| stress_family | Change in stress caused to the child by changes in family contacts between the 1st and 2nd lockdown | |
| worry_living_stability | Change in the child’s concern about the stability of the family’s living situation between the 1st and 2nd lockdown | |
| hopeful_end | Change in how hopeful the child is that the coronavirus/COVID-19 crisis will end between the 1st and 2nd lockdown | |
| Medical diagnosis and care | diagnosis_group | Diagnosis defined by the medical expert |
| symptoms | Change in symptoms the child had between the 1st and 2nd lockdown | |
| exposure | Child exposed to someone likely to have coronavirus/COVID-19 in the 1st and/or 2nd lockdown | |
| support_activities support_medical | Support activities, physical or medical, respectively, which were in place for the child and have been disrupted in the 1st and/or 2nd lockdown | |
| family_diagnosis | Whether any members of the child’s family have been diagnosed with COVID-19 in the 1st and/or 2nd lockdown | |
| family_hospitilization family_quarantine family_death family_illness | Whether any of the following have happened to the child’s family members because of Coronavirus/COVID-19: hospitalization, self-quarantine, death, and physical illness in the 1st and/or 2nd lockdown | |
| Mood state | l1_general_worry l2_general_worry | How worried the child generally was, in the 1st and 2nd lockdown, respectively |
| l1_sadness l2_sadness | How happy versus sad the child was, in the 1st and 2nd lockdown, respectively | |
| l1_anxiety l2_anxiety | How relaxed versus anxious the child was, in the 1st and 2nd lockdown, respectively | |
| l1_restlessness l2_restlessness | How fidgety or restless the child was, in the 1st and 2nd lockdown, respectively | |
| l1_anhedonia l2_anhedonia | Ability of the child to enjoy his/her usual activities, in the 1st and 2nd lockdown, respectively | |
| l1_loneliness l2_loneliness | How lonely the child was, in the 1st and 2nd lockdown, respectively | |
| l1_irritability l2_irritability | How irritable or easily angered the child was, in the 1st and 2nd lockdown, respectively | |
| l1_concentration l2_concentration | How well the child was able to concentrate or focus, in the 1st and 2nd lockdown, respectively | |
| l1_tiredness l2_tiredness | How fatigued or tired the child was, in the 1st and 2nd lockdown, respectively | |
| l1_rumination l2_rumination | How often the child was expressing negative thoughts, in the 1st and 2nd lockdown, respectively |
| Classifier | Hyperparameters |
|---|---|
| LR | - |
| LogR | penalty = [11, 12], C: [0, 1, 2, 4, 6, 8, 10] |
| MLP | hidden layer sizes: [(2, 5, 10), (5, 10, 20), (10, 20, 50)], activation: [tanh, relu], solve: [sgd, adam], alpha: [0.0001, 0.05], learning rate: [constant, adaptive] |
| LightGBM | n estimators: range (200, 600, 80), num leaves: range (20, 60, 10) |
| SVM | C: [0.001, 0.01, 0.1, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15], kernel: [linear,sigmoid,rbf,poly] |
| RF | criterion: [gini, entropy], n estimators: [10, 15, 20, 25, 27, 30], min samples leaf: [1, 2, 3, 4, 5], min samples split: [2, 3, 4, 5, 6, 7] |
| XG Boost | max depth: [1, 2, 3, 4, 5, 6, 7, 8, 9, 10], min child weight: [1, 2, 3, 4, 5, 6, 8, 10], gamma: [0, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9, 1] |
| Mann–Whitney U Test | ||
|---|---|---|
| Variable | U | p-Value |
| Age | 49,181.5 | 0.00033 |
| Gender | 54,811.5 | 0.06065 |
| Mood state score | 53,129.5 | 0.02715 |
| Diagnosis | 54,927.0 | 0.09506 |
| Living area | 50,203.0 | 0.00050 |
| Positive changes | 55,271.5 | 0.09720 |
| Daily behaviors | 54,586.0 | 0.08347 |
| Prediction Model | Best AUC-ROC Score | Number of Features |
|---|---|---|
| Linear Regression | 73.61% | 4 |
| Logistic Regression | 73.17% | 4 |
| LightGBM | 73.85% | 14 |
| Random Forest | 76% | 13 |
| XGBoost | 75.93% | 12 |
| SVM linear | 73.90% | 8 |
| SVM poly | 74.26% | 10 |
| SVM rbf | 74.15% | 10 |
| SVM sigmoid | 72.42% | 10 |
| MLP | 72.85% | 4 |
| Features | Deterioration vs. Amelioration/Stability of Mood State |
|---|---|
| stress_restrict | p = 0.001 |
| positive_change | p = 0.000 |
| social_media | p = 0.002 |
| diagnosis_group | p = 0.000 |
| reading | p = 0.001 |
| worry_phys_health | p = 0.057 |
| area_live | p = 0.061 |
| Most Important Features | |
|---|---|
| RF with ROC_AUC | RF with SHAP |
| stress_restrict | stress_restrict |
| positive_change | positive_change |
| social_media | social_media |
| worry_phys_health | diagnosis_group |
| relationships_friends | reading |
| diagnosis_group | worry_phys_health |
| reading | area_live |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ntakolia, C.; Priftis, D.; Kotsis, K.; Magklara, K.; Charakopoulou-Travlou, M.; Rannou, I.; Ladopoulou, K.; Koullourou, I.; Tsalamanios, E.; Lazaratou, E.; et al. Explainable AI-Based Identification of Contributing Factors to the Mood State Change in Children and Adolescents with Pre-Existing Psychiatric Disorders in the Context of COVID-19-Related Lockdowns in Greece. BioMedInformatics 2023, 3, 1040-1059. https://doi.org/10.3390/biomedinformatics3040062
Ntakolia C, Priftis D, Kotsis K, Magklara K, Charakopoulou-Travlou M, Rannou I, Ladopoulou K, Koullourou I, Tsalamanios E, Lazaratou E, et al. Explainable AI-Based Identification of Contributing Factors to the Mood State Change in Children and Adolescents with Pre-Existing Psychiatric Disorders in the Context of COVID-19-Related Lockdowns in Greece. BioMedInformatics. 2023; 3(4):1040-1059. https://doi.org/10.3390/biomedinformatics3040062
Chicago/Turabian StyleNtakolia, Charis, Dimitrios Priftis, Konstantinos Kotsis, Konstantina Magklara, Mariana Charakopoulou-Travlou, Ioanna Rannou, Konstantina Ladopoulou, Iouliani Koullourou, Emmanouil Tsalamanios, Eleni Lazaratou, and et al. 2023. "Explainable AI-Based Identification of Contributing Factors to the Mood State Change in Children and Adolescents with Pre-Existing Psychiatric Disorders in the Context of COVID-19-Related Lockdowns in Greece" BioMedInformatics 3, no. 4: 1040-1059. https://doi.org/10.3390/biomedinformatics3040062
APA StyleNtakolia, C., Priftis, D., Kotsis, K., Magklara, K., Charakopoulou-Travlou, M., Rannou, I., Ladopoulou, K., Koullourou, I., Tsalamanios, E., Lazaratou, E., Serdari, A., Grigoriadou, A., Sadeghi, N., Chiu, K., & Giannopoulou, I. (2023). Explainable AI-Based Identification of Contributing Factors to the Mood State Change in Children and Adolescents with Pre-Existing Psychiatric Disorders in the Context of COVID-19-Related Lockdowns in Greece. BioMedInformatics, 3(4), 1040-1059. https://doi.org/10.3390/biomedinformatics3040062








