Validating Capacitive Pressure Sensors for Mobile Gait Assessment
Abstract
1. Introduction
- Presentation of an improved smart sock prototype for measuring kinetic data;
- Validation of the newly developed smart sock prototype as a mobile force-sensing solution.
2. Materials and Methods
2.1. Participants
2.2. Proposed Device/Solution
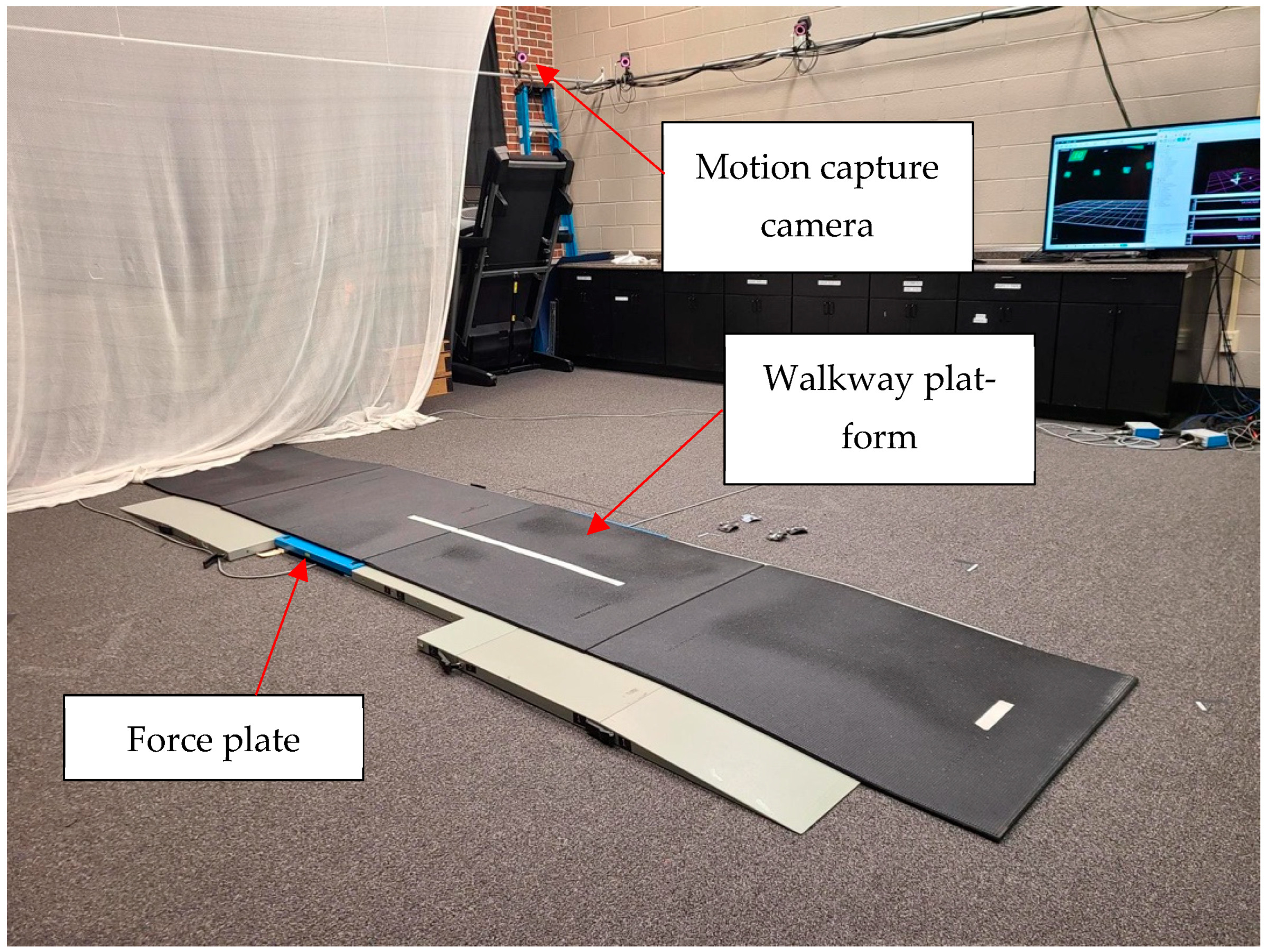
2.3. Experimental Setup and Methodology
2.4. Data Analysis
2.4.1. Preprocessing
2.4.2. Linear Regression and Correlation
2.4.3. Bland–Altman Analysis
3. Results
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 13 September 2023).
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Quantitative Gait Markers and Incident Fall Risk in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64A, 896–901. [Google Scholar] [CrossRef] [PubMed]
- What Is Telehealth?|HRSA. Available online: https://www.hrsa.gov/telehealth/what-is-telehealth (accessed on 13 September 2023).
- Fields, C. Supporting the Health Care Workforce: Lessons Following the COVID-19 Pandemic. JAMA 2020, 323, 1439–1440. [Google Scholar] [CrossRef]
- Shaver, J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim. Care 2022, 49, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Martini, E.; Fiumalbi, T.; Dell’agnello, F.; Ivanić, Z.; Munih, M.; Vitiello, N.; Crea, S. Pressure-Sensitive Insoles for Real-Time Gait-Related Applications. Sensors 2020, 20, 1448. [Google Scholar] [CrossRef] [PubMed]
- Parati, M.; Gallotta, M.; Muletti, M.; Pirola, A.; Bellafà, A.; De Maria, B.; Ferrante, S. Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions. Sensors 2022, 22, 6392. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, A.G.; Sevilla, R.R.; Alemán, A.; Durán, C.; Hochsprung, A.; Navarro, G.; Páramo, C.; Venegas, A.; Lladonosa, A.; Ayuso, G.I.; et al. Study for the validation of the FeetMe® integrated sensor insole system compared to GAITRite® system to assess gait characteristics in patients with multiple sclerosis. PLoS ONE 2023, 18, e0272596. [Google Scholar] [CrossRef]
- Jacobs, D.; Farid, L.; Ferré, S.; Herraez, K.; Gracies, J.-M.; Hutin, E. Evaluation of the Validity and Reliability of Connected Insoles to Measure Gait Parameters in Healthy Adults. Sensors 2021, 21, 6543. [Google Scholar] [CrossRef] [PubMed]
- Contini, B.G.; Bergamini, E.; Alvini, M.; Di Stanislao, E.; Di Rosa, G.; Castelli, E.; Vannozzi, G.; Camomilla, V. A wearable gait analysis protocol to support the choice of the appropriate ankle-foot orthosis: A comparative assessment in children with Cerebral Palsy. Clin. Biomech. Bristol. Avon. 2019, 70, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Park, S.; Lee, S.; Seo, S.H.; Kim, H.S.; Cha, Y.; Kim, J.-T.; Kim, J.-W.; Ha, Y.-C.; Yoo, J.-I. Assessing physical abilities of sarcopenia patients using gait analysis and smart insole for development of digital biomarker. Sci. Rep. 2023, 13, 10602. [Google Scholar] [CrossRef] [PubMed]
- Luczak, T.; Saucier, D.; Burch V., R.F.; Ball, J.E.; Chander, H.; Knight, A.; Wei, P.; Iftekhar, T. Closing the Wearable Gap: Mobile Systems for Kinematic Signal Monitoring of the Foot and Ankle. Electronics 2018, 7, 117. [Google Scholar] [CrossRef]
- Luczak, T.; Burch, R.; Lewis, E.; Chander, H.; Ball, J. State-of-the-art review of athletic wearable technology: What 113 strength and conditioning coaches and athletic trainers from the USA said about technology in sports. Int. J. Sports Sci. Coach. 2020, 15, 26–40. [Google Scholar] [CrossRef]
- Carroll, W.; Turner, A.; Talegaonkar, P.; Parker, E.; Middleton, J.C.; Peranich, P.; Saucier, D.; Burch, R.F.; Ball, J.E.; Smith, B.K.; et al. Closing the Wearable Gap–Part IX: Validation of an Improved Ankle Motion Capture Wearable. IEEE Access 2021, 9, 114022–114036. [Google Scholar] [CrossRef]
- Young, F.; Mason, R.; Wall, C.; Morris, R.; Stuart, S.; Godfrey, A. Examination of a foot mounted IMU-based methodology for a running gait assessment. Front. Sports Act. Living 2023, 4, 2022. [Google Scholar] [CrossRef] [PubMed]
- Cramer, L.A.; Wimmer, M.A.; Malloy, P.; O’Keefe, J.A.; Knowlton, C.B.; Ferrigno, C. Validity and Reliability of the Insole3 Instrumented Shoe Insole for Ground Reaction Force Measurement during Walking and Running. Sensors 2022, 22, 2203. [Google Scholar] [CrossRef] [PubMed]
- Samarentsis, A.G.; Makris, G.; Spinthaki, S.; Christodoulakis, G.; Tsiknakis, M.; Pantazis, A.K. A 3D-Printed Capacitive Smart Insole for Plantar Pressure Monitoring. Sensors 2022, 22, 9725. [Google Scholar] [CrossRef] [PubMed]
- Fastier-Wooller, J.W.; Lyons, N.; Vu, T.-H.; Pizzolato, C.; Rybachuk, M.; Itoh, T.; Dao, D.V.; Maharaj, J.; Dau, V.T. Flexible Iron-On Sensor Embedded in Smart Sock for Gait Event Detection. ACS Appl. Mater. Interfaces 2024, 16, 1638–1649. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, Y.L.; Xia, Y.; Wu, X.; Kirk, T.V.; Chen, X.D. A low-cost and highly integrated sensing insole for plantar pressure measurement. Sens. Bio-Sens. Res. 2019, 26, 100298. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Am. J. Ophthalmol. 1986, 148, 4–6. [Google Scholar] [CrossRef]
- Doğan, N.Ö. Bland-Altman analysis: A paradigm to understand correlation and agreement. Turk. J. Emerg. Med. 2018, 18, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Düking, P.; Fuss, F.K.; Holmberg, H.C.; Sperlich, B. Recommendations for Assessment of the Reliability, Sensitivity, and Validity of Data Provided by Wearable Sensors Designed for Monitoring Physical Activity. JMIR mHealth uHealth 2018, 6, e9341. [Google Scholar] [CrossRef] [PubMed]
- Closing the Wearable Gap: Foot–Ankle Kinematic Modeling via Deep Learning Models Based on a Smart Sock Wearable|Wearable Technologies|Cambridge Core. Available online: https://www.cambridge.org/core/journals/wearable-technologies/article/closing-the-wearable-gap-footankle-kinematic-modeling-via-deep-learning-models-based-on-a-smart-sock-wearable/5BF02B4389609465419DFA71149B0D0E (accessed on 17 January 2025).
- Armitage, M.; Beato, M.; McErlain-Naylor, S.A. Inter-unit reliability of IMU Step metrics using IMeasureU Blue Trident inertial measurement units for running-based team sport tasks. J. Sports Sci. 2021, 39, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Andò, B.; Baglio, S.; Graziani, S.; Marletta, V.; Dibilio, V.; Mostile, G.; Zappia, M. A Comparison among Different Strategies to Detect Potential Unstable Behaviors in Postural Sway. Sensors 2022, 22, 7106. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.G.; Wolf, A. Body weight unloading modifications on frontal plane joint moments, impulses and Center of Pressure during overground gait. Clin. Biomech. 2016, 39, 77–83. [Google Scholar] [CrossRef] [PubMed]



| Gender | Total | Mean Height | Mean Weight | Mean Foot Size |
|---|---|---|---|---|
| Male | 9 | 185 cm | 98 kg | 11 [US] |
| Female | 10 | 163 cm | 84 kg | 8 [US] |
| Shoe | Foot | Correlation Mean | Correlation Std | R2 Mean | R2 Std | R2 Mean | R2 Std | |
|---|---|---|---|---|---|---|---|---|
| 0 | All | All | 0.81 | 0.13 | 0.83 | 0.12 | 0.86 | 0.10 |
| 1 | All | L | 0.80 | 0.14 | 0.83 | 0.11 | 0.86 | 0.09 |
| 2 | All | R | 0.83 | 0.13 | 0.83 | 0.12 | 0.86 | 0.10 |
| 3 | Shoes | All | 0.81 | 0.09 | 0.83 | 0.10 | 0.87 | 0.08 |
| 4 | Shoes | L | 0.82 | 0.17 | 0.82 | 0.13 | 0.86 | 0.11 |
| 5 | Shoes | R | 0.81 | 0.09 | 0.85 | 0.09 | 0.88 | 0.07 |
| 6 | No shoe | All | 0.80 | 0.09 | 0.82 | 0.11 | 0.86 | 0.08 |
| 7 | No shoe | L | 0.78 | 0.17 | 0.80 | 0.13 | 0.85 | 0.11 |
| 8 | No shoe | R | 0.85 | 0.16 | 0.84 | 0.13 | 0.87 | 0.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Middleton, J.C.; Saucier, D.; Davarzani, S.; Parker, E.; Sellers, T.; Chalmers, J.; Burch, R.F.; Ball, J.E.; Freeman, C.E.; Smith, B.; et al. Validating Capacitive Pressure Sensors for Mobile Gait Assessment. Biomechanics 2025, 5, 54. https://doi.org/10.3390/biomechanics5030054
Middleton JC, Saucier D, Davarzani S, Parker E, Sellers T, Chalmers J, Burch RF, Ball JE, Freeman CE, Smith B, et al. Validating Capacitive Pressure Sensors for Mobile Gait Assessment. Biomechanics. 2025; 5(3):54. https://doi.org/10.3390/biomechanics5030054
Chicago/Turabian StyleMiddleton, John Carver, David Saucier, Samaneh Davarzani, Erin Parker, Tristen Sellers, James Chalmers, Reuben F. Burch, John E. Ball, Charles Edward Freeman, Brian Smith, and et al. 2025. "Validating Capacitive Pressure Sensors for Mobile Gait Assessment" Biomechanics 5, no. 3: 54. https://doi.org/10.3390/biomechanics5030054
APA StyleMiddleton, J. C., Saucier, D., Davarzani, S., Parker, E., Sellers, T., Chalmers, J., Burch, R. F., Ball, J. E., Freeman, C. E., Smith, B., & Chander, H. (2025). Validating Capacitive Pressure Sensors for Mobile Gait Assessment. Biomechanics, 5(3), 54. https://doi.org/10.3390/biomechanics5030054








