Abstract
Clinical equipment is essential in a labour unit to assess, monitor, diagnose, and prevent complications during labour. The availability of good working equipment in the labour unit is needed to enhance optimal intrapartum monitoring and delivery for pregnant women. Thus, this paper employed a cross-sectional descriptive design using a quantitative research approach to ascertain how equipment impedes optimal intrapartum monitoring and delivery for pregnant women. A total of 59 midwives were recruited to participate in the study. Data collected using an electronic structured questionnaire were analysed with descriptive statistics using Statistical Package for Social Sciences (SPSS) version 25.0. The study reported that most midwives (68%) in labour units experienced barriers to using equipment when administering care to pregnant women. The barriers were perpetuated by various factors, such as bed capacity, in meeting patient demands, including examination lights, overhead radiant warmers, and examination weighing scales for newborns. Incorporating mandatory computerized maintenance management software is recommended to improve the quality of maternity equipment. In addition, there is a need for regular equipment inspections and maintenance by skilled technicians in selected hospitals of Limpopo Province, South Africa.
Keywords:
clinical; equipment; impediment; optimal; intrapartum; monitoring; delivery; pregnant women; midwives 1. Introduction
Equipment is an essential clinical tool in the labour unit to assess, monitor, diagnose and prevent complications during labour. Labour units must be well equipped with exceptionally functional equipment to monitor and help pregnant women deliver to achieve positive birth outcomes [1]. Childbirth should be a safe and rewarding experience for women and their families [2]. Therefore, it is vital to have available equipment in the labour unit that ensures a physiologically safe birth and a positive childbirth experience [3].
The World Health Organisation reports that it is a requirement that basic essential equipment is always available in sufficient quantities in maternity units for utilisation during labour and childbirth [4]. However, midwives in sub-Saharan Africa experience difficulties providing optimum care to pregnant women and their babies, mainly challenged by increasing deliveries with a lack of essential resources in labour units [5,6,7]. Similarly, in the Philippines, midwives reported that essential routines, monitoring and assessment during labour were not sufficiently conducted due to being compounded by inappropriate infrastructure and supplies [8]. Therefore, the mentioned authors demonstrate that, although the use of equipment is significant during intrapartum monitoring and delivery for a pregnant woman, sufficient allocation and the effective utilisation of equipment by midwives remain barriers to achieving quality care during labour.
Facility midwifery care services need to improve by providing equipment and supplies to increase satisfaction with services received during the intrapartum stage of pregnant women [9]. A study in Sierra Leone indicated that the checklist entries for labour regarding delivery equipment could improve optimum care during intrapartum monitoring and delivery for pregnant women [10]. Significantly, the maintenance of equipment should be prioritised to achieve optimum monitoring and delivery for a pregnant woman effectively [10]. High-quality care is needed during labour. Therefore, improving accessibility to adequately available and functional equipment during labour promotes health and enhances good healthcare services, including quality management for pregnant women and their babies.
A shortage of medical equipment because of either unavailability or non-functioning is a barrier to the ability of the health system to deliver quality health services in South Africa [11]. South African Nursing Council (SANC) Regulation R.2488 (1990 as amended) stipulates conditions under which a registered midwife or accoucheur may carry out her profession. The regulation indicates that a registered midwife or accoucheur shall always have available equipment and the materials required to help pregnant women deliver in the labour unit [12]. This equipment includes the material necessary to perform an episiotomy and suture an episiotomy or a first/second-degree perineum tear. Therefore, there is a need for accessible, functional equipment to ensure the provision of high-quality care during the intrapartum stage to minimize substandard care practices, thereby reducing risks of preventable mortality and morbidity in mothers and newborn babies.
Since 1997, the National Committee on Confidential Enquiries into Maternal Deaths (NCCEMD) has meticulously recorded and analysed all maternal deaths within institutions [13]. They have produced seven comprehensive reports on this issue in South Africa. The reports provide detailed information about the extent of maternal deaths, the types of diseases that cause them and the factors contributing to these deaths, including missed opportunities and inadequate healthcare. Limpopo Province had a maternal mortality rate of 165.16 per 100,000 live births according to the latest NCCEMD report published in January 2018, despite implementing the Saving Mothers and Babies Report 2017–2019 recommendations [14,15].
The current paper aims to ascertain how equipment impedes optimal intrapartum monitoring and delivery for pregnant women in labour units in four selected hospitals in the Sekhukhune District of Limpopo Province, South Africa. The study findings will contribute to the body of knowledge in achieving the objective of the South African Department of Health National Strategy, which aims to improve timeliness, coverage, and quality of antenatal care; manage high-risk pregnancies; and achieve optimal intrapartum monitoring and delivery of pregnant women. In addition, we highlight the status quo of the Sustainable Development Agenda, to be realised by 2030, in terms of Goal 3, which seeks to ensure healthy lives and promote well-being for all ages by reducing the global maternal mortality ratio to less than 70 per 100,000 live births.
2. Material and Methods
2.1. Study Site
A quantitative cross-sectional research design was used to identify and ascertain equipment that may impede quality intrapartum monitoring and delivery for pregnant women in the labour unit. The study was conducted in the labour units of four selected hospitals of Limpopo Province in the Sekhukhune Health District. Limpopo is the fifth largest province of nine in South Africa, covering 10.3% of South Africa’s total land area. The province borders neighbouring countries such as Botswana to the west, Zimbabwe to the north, and Mozambique to the east. The province comprises five district hospitals, all rendering intrapartum and delivery care services to pregnant women. Sekhukhune Health District has a capacity of 998 approved beds and 679 actual usable beds, with most labour units having an average bed occupancy of 28–30. These four rural-based hospitals offer maternity health services to pregnant women from rural communities in the Sekhukhune District of Limpopo Province, South Africa.
2.2. Population and Sampling
The study’s target population was midwives working in the labour units of the four selected hospitals in Sekhukhune District, who provide care to pregnant women during the intrapartum stage. These midwives were appropriate for this study because they monitor pregnant women during the intrapartum stage and conduct deliveries for pregnant women. Non-probability total sampling was used in the study to select midwives that were interested in taking part in the study. A total population sample of 59 midwives was used because of the small number of midwives working in the selected hospitals’ labour units.
2.3. Data Collection
Data was collected by the primary researcher using self-developed questionnaires to determine the equipment that may be likely to impede optimal intrapartum care and delivery for pregnant women in labour units. Data collection was conducted after obtaining ethical clearance from the Turfloop Research Ethical Committee (TREC/82/2021: PG). Subsequently, the study sought permission from the Limpopo health department, the Director of Sekhukhune district hospitals, the chief executive officers of the selected hospitals in the Sekhukhune district, and unit managers of labour units. Permission was also obtained from midwives working in labour units who voluntarily participated in the study.
The questionnaires were formulated after reviewing the literature and validated with Cronbach’s alpha (697). The final questionnaires were presented to the supervisor, co-supervisor, and data statistician and were restructured in line with the study objectives. A pilot study was conducted using a sample of seven midwives to assess the readability of the questions, the difficulty, and the time it took to complete the questionnaires. The primary author collected data from February to April 2022 using a self-administered questionnaire. A total of 59 self-administered English-written questionnaires consisting of 4 sections were distributed, with a response rate of 100%. Significantly, the questionnaire used a Likert scale with scores ranging from one to five. The options were Strongly Agree (SA), Agree (A), Strongly Disagree (SD), Disagree (D), and Uncertain (U).
The sections were as follows: Section A: Demographic Data; Section B: The Nurse’s Role in the Use of Equipment; Section C: Equipment availability, effectiveness, and maintenance during the intrapartum stage; Section D: Delivery packs. The researcher approached midwives when they had no patients in labour and during their lunch breaks with their agreement to complete the questionnaire, which took 20–30 min.
2.4. Data Analysis
The completed questionnaires were extracted, coded, and captured using the Microsoft Excel programme (2016) and imported into the IBM Statistical Package for Social Science (SSPS) program, version 25.0, for analysis. Descriptive statistics were used to describe and facilitate the interpretation of the findings. Categorical variables were presented as numbers and percentages. Continued variables were presented as mean standard deviations.
2.5. Reliability and Validity of the Study
Reliability in this study was ensured by conducting a pre-test on 10% (7) of the study population in the labour unit. The pilot or pre-test assessed whether the questionnaires measured what they intended to measure and if the time allocated was adequate. Midwives and accoucheurs in labour units were given instructions before completing the questionnaires. Notably, the hospital used for the pilot study was not one of the selected hospitals. Notably, the small-scale study did not change the primary data collection tool.
The content validity of the questionnaires was ensured by performing an in-depth literature review to evaluate if the content of the questionnaires could achieve the study’s objectives and by providing a questionnaire to a researcher with expertise in quantitative research. The questionnaires were also submitted to the supervisor, co-supervisor, and statistician for review, and changes were made in accordance with biostatistician recommendations.
3. Presentation of the Study Findings
3.1. Section A: Demographic Profile of the Participants
The demographic profile of participants is presented according to age distribution, gender, qualifications, years of working experience, and qualification distribution as depicted in Figure 1 and Figure 2 below. As illustrated in Figure 1, the total number of midwives who participated in this study was 59, with the age distributions of the midwives ranging from 20 to 59 years, and a majority of the respondents in this study were female (91%). Furthermore, in this study, most midwives possessed registered midwifery qualifications (95%). In addition, most midwives had five years or more of working experience (49%), and most midwives were working day duty (74%).
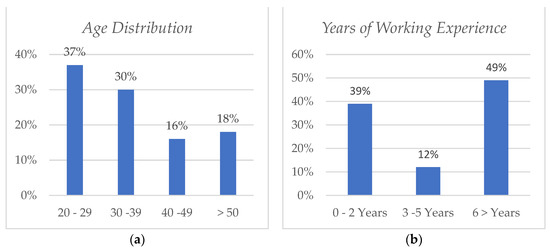
Figure 1.
Age (a) and years of working experience (b).
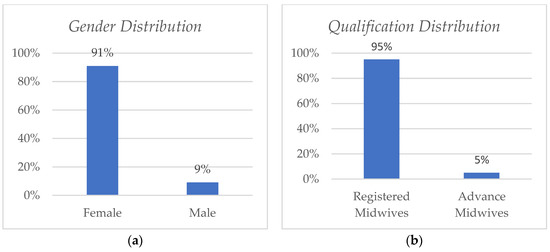
Figure 2.
Gender (a) and qualification distribution (b).
3.2. Section B: Midwives’ Roles Regarding the Use of Equipment
As depicted in Figure 3, 100% of respondents (57) knew their roles regarding the use of equipment in the labour unit, 68% (39) experienced barriers with the use of equipment when administering care to pregnant women, 81% (46) indicated that equipment used in the labour unit needed improvement, and 70% (40) indicated that reported non-functional equipment was not attended to promptly. However, 74% (42) indicated that there were quality care practices for pregnant women with the use of equipment in the labour unit.
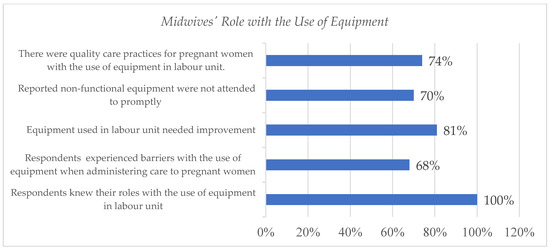
Figure 3.
Midwives’ roles regarding the use of equipment.
3.3. Section C: Equipment Availability, Effectiveness, and Maintenance during the Intrapartum Stage
As depicted in Table 1, 61% of midwives (35) strongly agreed that the blood pressure (BP) machine was available, and 49% (28) indicated that the BP machine was fully functional. However, 37% (21) of respondents strongly disagreed that BP machines in the labour unit adequately monitor all women during the intrapartum stage and labour. In total, 41% (24) midwives strongly agreed that only one BP machine is used for all pregnant women in the labour unit. Shockingly, 32% (18) of respondents strongly disagreed that BP machines undergo routine maintenance or service.

Table 1.
Equipment availability, effectiveness, and maintenance during the intrapartum stage.
About 68% (39) of the respondents indicated that a CTG machine was available. Majority of the respondents agreed that CTG machine was functional. Close to half (45% (31)) of the respondents strongly agreed that CTG paper stripes were always available. In addition to equipment availability, effectiveness, and maintenance during the intrapartum stage, 68% of the midwives (39) indicated that they knew the benefits of using a CTG machine, and 44% (25) of midwives also agreed that they could interpret the CTG results. The study results revealed that 49% (28) indicated that a foetal heart rate (FHR) monitor was available and also that 51% (29) of the respondents agreed that the FHR monitor used in the labour unit provides accurate results. However, 43% of midwives (24) strongly felt that the FHR monitor needed improvement.
According to this study, 35% (20) of the participants disagreed that the capacity of beds is sufficient to cater to the needs of patients. In addition, 32% of the respondents (18) agreed that examination lights were available in each delivery room. However, 32% (18) of the midwives strongly disagreed that the examination lights were functioning well. Furthermore, in this study, 37% (21) of the midwives strongly disagreed that an overhead radiant warmer was available in each delivery room, and the majority, 51% (29), strongly disagreed that the radiant warmer was fully functional in each delivery room. In addition, 44% (25) of respondents indicated that the overhead radiant warmer was inadequate to meet newborn demands. In addition to the equipment used during the intrapartum stage, 31% (18) of respondents strongly disagreed that newborn examination scales are available in each delivery room. Equally, the majority, 54% (31), strongly disagreed that examination scales for newborns were functioning well.
3.4. Section D: Delivery Packs
As depicted in Table 2, most of the respondents, 63% (37), strongly agreed that delivery packs were available, and 35% (20) strongly agreed that delivery packs were always complete inside. In addition, this study’s findings suggest that most of the midwives, 51% (29), agreed that arterial forceps were available in each delivery pack, and 38% of respondents (21) agreed that arterial forceps were functioning well. Regarding the availability of needle holders, 38% of respondents (22) agreed that they were available in all delivery packs. However, 40% (23) of respondents strongly disagreed that needle holders in each delivery pack were functioning well.

Table 2.
Delivery Packs.
A total of 35% (20) of the respondents agreed that some midwives do not use needle holders but instead use their hands when suturing perineal tears and episiotomy cuts. In total, 49% (27) of the midwives in this study agreed that cord scissors were available in each delivery pack. Despite the availability of cord scissors, 46% of respondents (26) agreed that the umbilical cord scissors were blunt, and 50% (29) respondents agreed that they utilized a razor blade for cutting the umbilical cord in the absence of functional umbilical cord scissors. Most respondents, 51% (29), agreed that episiotomy scissors were available in each delivery pack. However, 57% (33) of respondents strongly agreed that episiotomy scissors were blunt, and 41% (23) agreed that razor blades were utilized in the absence of functional episiotomy scissors.
4. Discussion of Research Results
4.1. Demographic Profile of the Respondents
The study aimed to ascertain how equipment impedes optimal intrapartum monitoring and delivery for pregnant women in selected hospitals of Limpopo Province, South Africa. The respondents’ demographic data provides information about the characteristics of the population who participated in the study.
Most of the respondents in this study were female (91%), compared with male respondents (9%). This discrepancy might be perpetuated for various reasons, such as cultural, religious, and gender stereotypes that men are not allowed to practice midwifery in some African contexts and pregnant women’s beliefs that men are not allowed in maternity units [16]. Furthermore, midwifery care has historically been a female domain, owing to the widely held belief that midwifery is about a female relationship. Of the respondents, 37% were between the age of 20 and 29%, while those aged between 30 and 39% were represented by 30%. Nearly half _49%) of the respondents had six or more years of experience in labour unit. The findings of this study are consistent with those of a study conducted in maternity units at a public hospital in KwaZulu-Natal, where most participants were between 20 and 40 years of age, with an average of 12 years of working experience [17]. Furthermore, in this study, most midwives possessed registered midwifery qualifications (95%), and most midwives (74%) worked the day shift. By contrast, in Western Cape, a study conducted had 93 midwives who participated, and the night shift comprised 57 midwives, while the day shift had only 36 midwives [18].
4.2. Nurse’s Role Regarding the Use of Equipment
A midwife or accoucheur is a person who has met the prescribed education requirements for registration as a midwife or accoucheur and who can assume responsibility and accountability for such practices [19]. In this study, all midwives (100%) knew their roles regarding the use of equipment when attending pregnant women in the selected hospitals in Limpopo Province. However, 68% of the respondents experienced challenges with using equipment when administering care to pregnant women, and that is because the non-functional equipment was not attended to promptly, as reported by most of the respondents (70%) in this study; equally, most of the midwives (81%) indicated that equipment used in the labour unit needed improvement. The literature corroborates the results of this study in that there is a challenge with the use of equipment in maternity units in Limpopo Province. For example, a qualitative study conducted in KwaZulu-Natal revealed that midwives found it challenging to perform their duties because of either faulty or unavailable equipment and materials, especially in public hospitals [20]. This implies that a lack of healthcare equipment impedes optimal intrapartum monitoring and delivery for pregnant women. Therefore, by addressing these challenges, the quality of nursing care provided to pregnant women during intrapartum monitoring and delivery can be improved, ultimately reducing complications that may arise from equipment shortages or malfunctioning.
4.3. Equipment Availability, Effectiveness, and Maintenance during the Intrapartum Stage
The current study looked at the equipment used during the intrapartum stage. More than half (61%) of the respondents agreed that BP machines were available. About 49% of the respondents believed that the BP machines were functional. However, the findings of this study revealed that, in the labour units of the selected hospitals, 37% (21) of respondents strongly disagreed that BP machines were adequate to monitor all pregnant women during the intrapartum period. In addition, a plurality (41%) strongly agreed that only one BP machine was used for all admitted pregnant women in the labour unit. The findings of this study are consistent with those of a quantitative study conducted in Limpopo Province in which most respondents (55%) reported that BP machines were functional in the labour room but were not adequate to cater to admitted pregnant women [6].
Concerning equipment for monitoring FHR in labour units, most respondents (51%) agreed that the FHR monitor in the labour unit provides accurate readings. However, most midwives (43%) strongly agreed that there is a need to improve the equipment used for monitoring FHR in the labour units. Moreover, most of the respondents (68%) in this study reported the availability of the CTG machine and its benefits during the intrapartum stage in the labour unit of the selected hospitals in Limpopo Province. In addition, 44% of the midwives knew how to interpret CTG results. The findings of this study are in contrast with the findings of a quantitative study, which revealed that midwives in KwaZulu-Natal public hospitals were clinically lacking in knowledge of CTG [21]. It is noteworthy to mention that the CTG machine is vital to monitor foetal well-being during the intrapartum stage. Thus, the World Health Organization emphasises that CTG knowledge is necessary for critical decision-making during intrapartum monitoring activities [22].
However, in the context of this study, caring for pregnant women during labour following maternity guidelines may not be the case in the selected hospitals in Limpopo Province because of a lack of BP machines. For example, a guideline for maternity care in Guidelines for Maternity Care in South Africa requires midwives to monitor the blood pressure of pregnant women in labour upon admission; every four hours at the latent phase of labour; hourly at the active phase of labour and after the delivery of the placenta; and one post-delivery [23]. Supporting this assertion, a qualitative study conducted in Kenya, which had a similar rural setting background, revealed that a lack of essential equipment and commodities hindered the provision of standard maternity care [24]. Therefore, for midwives to provide quality maternity care, authorities must ensure that essential equipment and commodities are available in public hospitals.
High-quality intrapartum care is critical to the survival of the mother and the newborn [25]. However, the lack of essential equipment in this study was reported to be a potential impediment to the provision of quality care for pregnant women in the labour units of the selected hospitals. In total, 35% of midwives in this study disagreed that bed capacity is enough to meet patient demands. The findings of this study are consistent with those of studies conducted in various African regions. For example, a study in Kenya in Eastern Africa found that maternity units were overcrowded, resulting in some patients being discharged early to make room for others or even having to sleep on the floor because of a shortage of beds [26]. Similar results were observed in other African regions, such as the Southern African Developing Countries. In Gauteng Province, South Africa, midwives had to improvise to provide midwifery care because of a lack of bed capacity for pregnant women [27]. Notably, the lack of bed capacity to care for patients may be because of various reasons, including an influx of migrant and refugee patients from neighbouring countries, such as Zimbabwe and Mozambique [28,29]. Lack of adequate beds in the labour unit affects the quality of care for pregnant women, compromises their comfort, and impedes the quality of management given to pregnant women in labour.
Examination lights are essential during observations, as they provide suitable visibility and authentic images. However, in this study, examination lights were not all functioning well, as 28% of the respondents disagreed that examination lights functioned well in each delivery room. A qualitative study in Uganda found that poor infrastructure at maternity facilities frustrated health workers and made them feel they could not offer quality care to patients [30]. Adequate infrastructure with electricity and lighting is critical to health workers in rural areas such as Limpopo Province in providing quality healthcare. Shockingly, in this study, 37% of respondents agreed that overhead radiant warmers were available in each delivery room. However, 51% of respondents disagreed that overhead radiant were functioning well. In addition, they were not adequate to meet newborn demands, which affected the quality of care. The World Health Organization Practical Guide for the Thermal Control of the Newborn emphasises that the risk of neonatal hypothermia is significantly increased in labour units where policies, procedures, and equipment for maintaining an optimal thermal environment for the newborn are lacking [31]. The findings of this study suggest that there is a lack of implementation of policies that intend to ensure that quality healthcare is provided. As a result, newborns in labour units are exposed to hypothermia, a potentially dangerous drop in body temperature in newborn babies that causes complications [32].
Moreover, 32% of respondents strongly disagreed that examination scales were available in each labour unit. Similar findings were reported in a qualitative study conducted in Tanzania, where midwives reported a lack of sufficient and suitable weighing scales for newborns, which impedes the healthcare services of newborns [33]. Providing infants with holistic and comprehensive healthcare, such as calculating appropriate medication doses, fluids, and the early diagnosis of developmental defects, depends mainly on accurate birth weight [33,34]. Initiatives such as the Ideal Clinic programme are recommended to address the shortage of essential equipment in labour units. The “Ideal Clinic” is a healthcare facility with good infrastructure and adequate staff, medicine, and supplies of crucial health equipment, including partner and stakeholder support, thus ensuring quality healthcare services [35,36]. A lack of and malfunctions in medical equipment during labour can impact nursing care quality, hindering assessment, diagnosis, and the prevention of complications. Addressing issues related to malfunctioning equipment is imperative to achieve the objectives of Sustainable Development Goal 3, especially in rural areas where people have limited access to private healthcare practitioners because of their low socio-economic status.
4.4. The Delivery Packs
Concerning the equipment used during delivery in the selected hospitals in Limpopo Province, most respondents (63%) strongly agreed that delivery packs were available. In total, 35% of midwives strongly agreed that delivery packs are always complete inside. The findings of this study are in contrast with those of a mixed-method study conducted in four labour units in Zanzibar revealed that delivery packs were often incomplete [37]. In our study, most respondents (51%) agreed that arterial forceps were available in each delivery pack. In addition, 38% of respondents agreed that these arterial forceps were functioning well. The findings of this study also revealed that needle holders were available in all prepared delivery packs, as 38% of respondents agreed.
Despite the availability, 40% of midwives disagreed that the needle holders in each delivery pack were functioning well. In addition, 35% of respondents disagreed that some midwives do not use needle holders but instead use their hands when suturing tears and episiotomy cuts in delivery. Furthermore, 49% of respondents agreed that umbilical cord scissors are available in each delivery pack. However, 46% of midwives also reported that some umbilical cord scissors were blunt (they cannot cut). In addition, half of the respondents (50%) agreed that they used razor blades to cut umbilical cords when there were no functional scissors. The findings of this study are consistent with those of a quality assurance sampling survey conducted in two states of Nigeria, in which new razor blades were used to cut the newborn umbilical cord in about 75% of the deliveries in Bauchi and over 80% in Sokoto States [38]. Although a razor blade is not recommended to cut a newborn’s umbilical cord, it is essential to mention that, during emergencies, using a sterile razor blade in practice is an appropriate alternative for cutting the umbilical cord.
Most respondents (51%) in this study agreed that episiotomy scissors were available in each delivery pack. However, 57% of respondents strongly agreed that some episiotomy scissors were blunt. TThus, in this study, 41% of midwives reported that razor blades were used for cutting episiotomies in cases where sharp or functional episiotomy scissors were unavailable. This study’s findings contrast with the Guideline for Maternity Care in South Africa, in which episiotomy scissors are listed as essential equipment for maternal healthcare services [22]. Therefore, it is vital to incorporate mandatory computerised maintenance management software to improve the quality of maternity equipment in the labour unit [39]. The study results have significant implications. Using blunt scissors might contribute to serious birth injuries, and, more importantly, it can also increase the risk of perineal tears. Addressing this challenge to mitigate associated risks and enhance the quality of midwifery care provided during labour is highly recommended.
4.5. Limitations of the Study
Even though the study provides insight into equipment as a potential impediment to optimal intrapartum monitoring and delivery for pregnant women, the study results only provide a view of respondents from the selected hospitals in one district of Limpopo Province. Therefore, the study results cannot be generalized to other district hospitals or other hospitals in South Africa. The study was limited to a small population; other researchers can conduct studies that will include more hospitals in South Africa, hence more respondents, to gain more perspectives or views on the study topic, venturing into qualitative research to explore more opinions about the topic.
5. Conclusions
In conclusion, pregnant women face obstacles in receiving optimal intrapartum monitoring and delivery care due to insufficient equipment and inadequate maintenance. High-quality care is needed during labour to enhance positive birth outcomes. Therefore, it is recommended that the employer, the Department of Health, provide the required equipment to labour units and prioritize improving the equipment utilized in labour units with annual budgets by ensuring accessibility to available, adequate, and functional equipment and improving infrastructure. Incorporating mandatory computerized maintenance management software is recommended to improve the quality of maternity equipment. In addition, there is a need for regular equipment inspections and maintenance by skilled technicians in the selected hospitals of Limpopo Province, South Africa.
Author Contributions
Conceptualization, K.M.M., L.M. and M.G.M.; methodology, K.M.M. and M.O.M.; formal analysis, M.O.M. and T.A.P.; investigation, K.M.M.; data curation, K.M.M.; writing—original draft preparation, K.M.M. and T.A.N.; writing—review and editing, K.M.M. and T.A.N.; visualization, T.A.P.; supervision, L.M. and M.G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and ethical clearance was obtained from the University of Turfloop Research Ethics Committee (TREC/82/2021: PG). Permission to conduct the study was obtained from the Limpopo Department of Health.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not shared because of privacy and ethical restrictions.
Acknowledgments
The authors would like to thank the participants who gave consent to participate for their cooperation during the research process.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Masaba, B.B.; Mmusi-Phetoe, R. A Strategy for Reducing Maternal Mortality in Rural Kenya. Int. J. Women’s Health 2023, 31, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Chandraharan, E.; Arulkumaran, S. Obstetric and Intrapartum Emergencies; Cambridge University Press: New York, NY, USA, 2021. [Google Scholar]
- Cheyne, H.; Duff, M. Anatomy and Physiology of Labour and Associated Behavioural Clues; Squaring the Circle, Pinter & Martin: London, UK, 2019. [Google Scholar]
- World Health Organization. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Bradley, S.; McCourt, C.; Rayment, J.; Parmar, D. Midwives’ perspectives on (dis) respectful intrapartum care during facility-based delivery in sub-Saharan Africa: A qualitative systematic review and meta-synthesis. Reprod. Health 2019, 16, 116. [Google Scholar] [CrossRef] [PubMed]
- Ramavhoya, I.T.; Maputle, M.S.; Ramathuba, D.U.; Lebese, R.T.; Netshikweta, L.M. Managers’ support on implementation of maternal guidelines, Limpopo province, South Africa. Curationis 2020, 43, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Adams, T.; Mason, D.; Gebhardt, G.S. Moderate to severe neonatal encephalopathy with suspected hypoxic-ischaemic encephalopathy in cooled term infants born in Tygerberg Academic Hospital: Characteristics of fetal monitoring and modifiable factors. S. Afr. J. Child Health 2022, 16, 83–88. [Google Scholar] [CrossRef]
- Masuda, C.; Ferolin, S.K.; Masuda, K.; Smith, C.; Matsui, M. Evidence-based intrapartum practice and its associated factors at a tertiary teaching hospital in the Philippines, a descriptive mixed-methods study. BMC Pregnancy Childbirth 2020, 20, 78. [Google Scholar] [CrossRef]
- Sigalla, G.N.; Bakar, R.R.; Manongi, R.N. Experiences of facility-based delivery services among women of reproductive age in Unguja Island, Zanzibar: A Qualitative Study. J. Fam. Med. 2018, 5, 1149. [Google Scholar]
- Koroma, M.M.; Kamara, M.A.; Keita, N.; Lokossou, V.K.; Sundufu, A.J.; Jacobsen, K.H. Access to Essential Medications and Equipment for Obstetric and Neonatal Primary Care in Bombali District, Sierra Leone. World Med. Health Policy 2019, 11, 8–23. [Google Scholar] [CrossRef]
- Moyimane, M.B.; Matlala, S.F.; Kekana, M.P. Experiences of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: A qualitative study. Pan Afr. Med. J. 2017, 28, 157. [Google Scholar] [CrossRef]
- South African Nursing Council. Regulations Relating to the Conditions under Which Registered Midwives and Enrolled Midwives May Carry on Their Profession; Regulation R. 2488; SANC: Pretoria, South Africa, 1990. [Google Scholar]
- National Committee on Confidential Enquiries into Maternal Deaths. Saving Mothers 2014–2016: Seventh Triennial Report on Confidential Enquiries into Maternal Deaths in South Africa; National Department of Health South Africa: Pretoria, South Africa, 2018.
- Bomela, N.J. Maternal mortality by socio-demographic characteristics and cause of death in South Africa: 2007–2015. BMC Public Health 2020, 20, 157. [Google Scholar] [CrossRef]
- Mothapo, K.E.; Maputle, M.S.; Shilubane, H.N.; Netshikweta, L. Challenges Midwives in Limpopo Province Encounter when Implementing Saving Mothers Recommendations. Open Nurs. J. 2020, 14, 292–299. [Google Scholar] [CrossRef]
- Madlala, S.T.; Ngxongo, T.S.; Sibiya, M.N. Perceptions of pregnant women regarding student accoucheurs’ involvement in maternal health care in the Free State Province. Int. J. Afr. Nurs. Sci. 2020, 13, 100255. [Google Scholar] [CrossRef]
- Mhlongo, N.M. Experiences of Midwives Regarding Practice Breakdown in Maternity Units at a Public Hospital in KwaZulu-Natal. Master’s Thesis, Durban University of Technology, Durban, South Africa, 2016. [Google Scholar]
- Phiri, L.P.; Draper, C.E.; Lambert, E.V.; Kolbe-Alexander, T.L. Nurses’ lifestyle behaviours, health priorities and barriers to living a healthy lifestyle: A qualitative descriptive study. BMC Nurs. 2014, 13, 38. [Google Scholar] [CrossRef] [PubMed]
- Martin, S. Quality care during childbirth at a midwife obstetric unit in Cape Town, Western Cape: Women and Midwives’ perceptions. Master’s Thesis, University of Western Cape, Western Cape, South Africa, 2018. [Google Scholar]
- Mhlongo, N.M.; Sibiya, M.N.; Miya, R.M. Experiences of midwives regarding nursing practice breakdown in maternity units at a selected public hospital in KwaZula-Natal. Afr. J. Nurs. Midwifery 2016, 18, 162–178. [Google Scholar] [CrossRef]
- James, S.; Maduna, N.E.; Morton, D.G. Knowledge levels of midwives regarding the interpretation of cardiotocographs at labour units in KwaZulu-Natal public hospitals. Curationis 2019, 42, 1–7. [Google Scholar] [CrossRef]
- World Health Organization. WHO Recommendations on Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- National Department of Health, South Africa. Guidelines for Maternity Care in South Africa. In A Manual for Clinics, Community Health Centres and District Hospitals, 4th ed.; NDoH: Pretoria, South Africa, 2015; Volume 172. [Google Scholar]
- Lusambili, A.; Wisofschi, S.; Shumba, C.; Obure, J.; Mulama, K.; Nyaga, L.; Wade, T.J.; Temmerman, M. Health Care Workers’ Perspectives of the Influences of Disrespectful Maternity Care in Rural Kenya. Int. J. Environ. Res. Public Health 2020, 17, 8218. [Google Scholar] [CrossRef] [PubMed]
- Brenner, S.; Madhavan, S.; Nseya, C.K.; Sese, C.; Fink, G.; Shapira, G. Competent and deficient provision of childbirth services: A descriptive observational study assessing the quality of intrapartum care in two provinces of the Democratic Republic of the Congo. BMC Health Serv. Res. 2022, 22, 551. [Google Scholar] [CrossRef]
- Gitobu, C.M.; Gichangi, P.B.; Mwanda, W.O. Satisfaction with delivery services offered under the free maternal healthcare policy in Kenyan public health facilities. J. Environ. Public Health 2018, 2018, 4902864. [Google Scholar] [CrossRef]
- Lumadi, T.G.; Matlala, M.S. Perceptions of midwives on shortage and retention of staff at a public hospital in Tshwane District. Curationis 2019, 42, 1–10. [Google Scholar]
- Mutambara, V.M.; Naidu, M. Probing the Context of Vulnerability: Zimbabwean Migrant Women’s Experiences of Accessing Public Health Care in South Africa. Afr. Hum. Mobil. Rev. 2021, 7, 1. [Google Scholar] [CrossRef]
- Chekero, T.; Ross, F.C. “On paper” and “having papers”: Zimbabwean migrant women’s experiences in accessing healthcare in Giyani, Limpopo province, South Africa. Anthropol. South. Afr. 2018, 41, 41–54. [Google Scholar] [CrossRef]
- Munabi-Babigumira, S.; Glenton, C.; Willcox, M.; Nabudere, H. Ugandan health workers’ and mothers’ views and experiences of the quality of maternity care and the use of informal solutions: A qualitative study. PLoS ONE 2019, 14, e0213511. [Google Scholar] [CrossRef]
- World Health Organization. Thermal Control of the Newborn: A Practical Guide; Maternal Health and Safe Motherhood Programme, Division of Family Health; WHO: Geneva, Switzerland, 1993. [Google Scholar]
- Dey, K.; Deb, U.K. Modeling and simulation of heat transfer phenomenon from infant radiant warmer for a newborn baby. Open J. Model. Simul. 2021, 9, 111. [Google Scholar] [CrossRef]
- Gladstone, M.E.; Salim, N.; Ogillo, K.; Shamba, D.; Gore-Langton, G.R.; Day, L.T.; Blencowe, H.; Lawn, J.E. Birthweight measurement processes and perceived value: Qualitative research in one EN-BIRTH study hospital in Tanzania. BMC Pregnancy Childbirth 2021, 21, 232. [Google Scholar] [CrossRef] [PubMed]
- Weres, A.; Baran, J.; Czenczek-Lewandowska, E.; Leszczak, J.; Mazur, A. Impact of Birth Weight and Length on Primary Hypertension in Children. Int. J. Environ. Res. Public Health 2019, 16, 4649. [Google Scholar] [CrossRef]
- Ideal Clinic Manual. Ideal Clinic Definitions, Components and Checklists. National Department of Health. Version.19. 2020. Available online: https://www.knowledgehub.org.za/elibrary/ideal (accessed on 9 April 2023).
- Muthelo, L.; Moradi, F.; Phukubye, T.A.; Mbombi, M.O.; Malema, R.N.; Mabila, L.N. Implementing the ideal clinic program at selected primary healthcare facilities in South Africa. Int. J. Environ. Res. Public Health 2021, 18, 7762. [Google Scholar] [CrossRef] [PubMed]
- De Barra, M.; Gon, G.; Woodd, S.; Graham, W.J.; de Bruin, M.; Kahabuka, C.; Williams, A.J.; Konate, K.; Ali, S.M.; Said, R.; et al. Understanding infection prevention behaviour in maternity wards: A mixed-methods analysis of hand hygiene in Zanzibar. Soc. Sci. Med. 2021, 272, 113543. [Google Scholar] [CrossRef] [PubMed]
- Abegunde, D.; Orobaton, N.; Beal, K.; Bassi, A.; Bamidele, M.; Akomolafe, T.; Ohanyido, F.; Umar-Farouk, O.; Danladi, S.A. Trends in newborn umbilical cord care practices in Sokoto and Bauchi States of Nigeria: The where, who, how, what and the ubiquitous role of traditional birth attendants: A lot quality assurance sampling survey. BMC Pregnancy Childbirth 2017, 17, 368. [Google Scholar] [CrossRef]
- Mkalaf, K.; Gibson, P.; Flanagan, J. A study of current maintenance strategies and the reliability of critical medical equipment in hospitals in relation to patient outcomes. Int. J. Manag. 2013, 7, 15–28. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).