- Article
Prioritization of Elective Hysterectomies in the Brazilian Unified Health System: Consistency Between Clinical Risk, Waiting Time and Implications for Surgical Equity
- Letícia Calazans Queiroz Cardone,
- Raphael Federicci Haddad and
- Rômulo Negrini
- + 4 authors
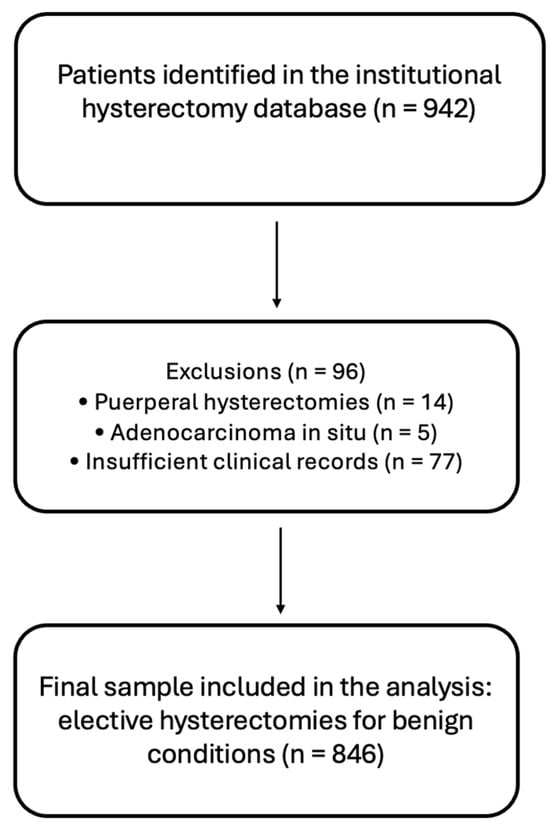
This study examined the consistency between clinical criteria, assigned priority level, and waiting time for elective hysterectomy, assessing whether higher priority translates into faster surgical access. We conducted a retrospective cohort study including 846 women who underwent the procedure between January 2018 and January 2024 at a public hospital in São Paulo, Brazil. The median waiting time was 6 months (IQR: 3–10), with wide variability ranging from 0.5 to 53 months. All components of the clinical score were associated with higher priority levels, demonstrating adequate discriminative ability to identify patients at greater clinical risk. However, assigned priority was not associated with shorter waiting times. Criteria reflecting greater clinical vulnerability, including duration of symptoms (β = +2.50 months), age (β = +1.00), and cardiovascular disease (β = +1.00), were paradoxically associated with longer waiting times, whereas anemia was the only factor associated with reduced waiting time (β = −1.00). These findings reveal a marked discrepancy between formal prioritization and actual surgical scheduling, underscoring the need for more objective and equity-oriented criteria in the management of surgical waiting lists.
25 December 2025